Abstract
Introduction Acute suppurative neck infections associated with third or fourth branchial arch fistulas are frequently recurrent. Third and fourth branchial arch anomalies are much less common and usually present with recurrent left thyroid lobe abscesses.
Objectives The authors present their experience in treating such cases that were observed exclusively in children.
Methods The study involved performing a retrospective review of five cases in PSG Institute of Medical Sciences & Research. All cases were evaluated radiologically and with Direct Rigid hypopharyngoscopy. Definitive surgery was performed, including hemithyroidectomy.
Results The patients consisted of five children, two boys and three girls. All of them presented with recurrent episodes of neck infection. Investigations performed included computed tomography (CT) fistulography, rigid hypopharyngoscopy and ultrasound, which were useful in preoperatively delineating pyriform sinus fistulous tract. All patients underwent neck exploration with excision of the fistulous tract and hemithyroidectomy. Upon follow-up, all patients are asymptomatic.
Conclusions Recurrent neck abscesses in a child should alert the clinician to the possibility of a fourth branchial arch anomaly; therefore, children with this condition require a complete evaluation so the anomaly can be ruled out.
Keywords: pyriform sinus, abscess, thyroiditis
Introduction
Children presenting with recurrent neck abscesses or thyroiditis present a diagnostic dilemma. They are often treated symptomatically, which involves frequent incision and drainage (I&D) procedures, adding to the child's fear psychosis and parents' anxiety. An entity called congenital branchial pouch anomaly of the fourth arch has only been recently described as an underlying pathology in these children.1 2 3 An inflammatory infiltration or abscess between the pyriform fossa and the thyroid bed in the lower left part of the neck may indicate an infected third or fourth branchial fistula.1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 Acute suppurative thyroiditis and thyroid abscess are extremely rare disorders. In this context, it is imperative to commence early diagnosis and treatment of the fourth pouch fistula. This article presents the author's experience in treating patients with this rare anomaly.
Materials and Methods
A retrospective review and prospective follow-up of five cases of congenital fourth branchial pouch anomaly was done in our hospital, a tertiary care center. The study period included the years 2008–2013. The study was performed upon approval from the Institutional Human Ethics Committee (ref no.13/339). All the patients had presented to the pediatric surgery OPD with a history of recurrent neck abscesses with a past history of multiple I&D procedures. One patient had presented with an acute suppurative inflammation in the neck.
Once all the patients were admitted, they underwent a thorough evaluation, including complete blood counts with peripheral smear evaluation to document infection and to rule out neutrophil anomalies. The patients that had presented with suppuration underwent a preliminary ultrasonography of the neck to document the abscess. These patients were also started with broad spectrum antibiotics (Inj.Ceftriaxone + Inj.Flagyl). Pus was sent for culture and antibiotic sensitivity while an I&D was done to relieve the acute symptoms.
Once all the symptoms of acute inflammation had subsided, the children underwent a computerized tomography (CT) of the neck using contrast. Two children also underwent a magnetic resonance imaging (MRI) of the neck. The Otorhinolaryngologist performed a diagnostic hypopharyngoscopy/endoscopy under general anesthesia on all the children. A fistulous opening in the apex of the pyriform sinus was documented for all five patients. There was no barium study done on any of the patients. The children were then planned for definitive management, which included an external approach to delineate the fistulous tract and direct hypopharyngoscopy to cauterize the internal opening in the pyriform sinus (Figs. 1 2 3 4 5).
Fig. 1.
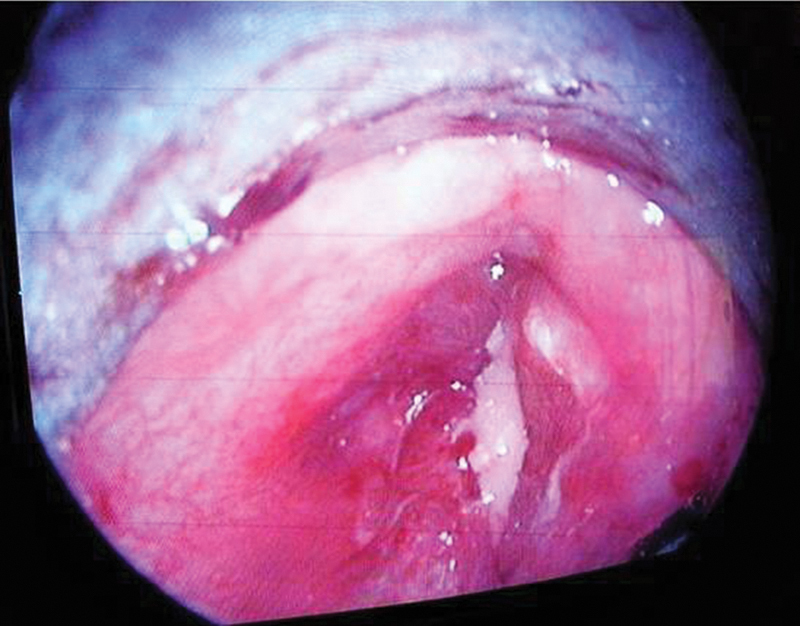
Pus seen during hypopharyngoscopy at the internal opening in the pyriform sinus.
Fig. 2.
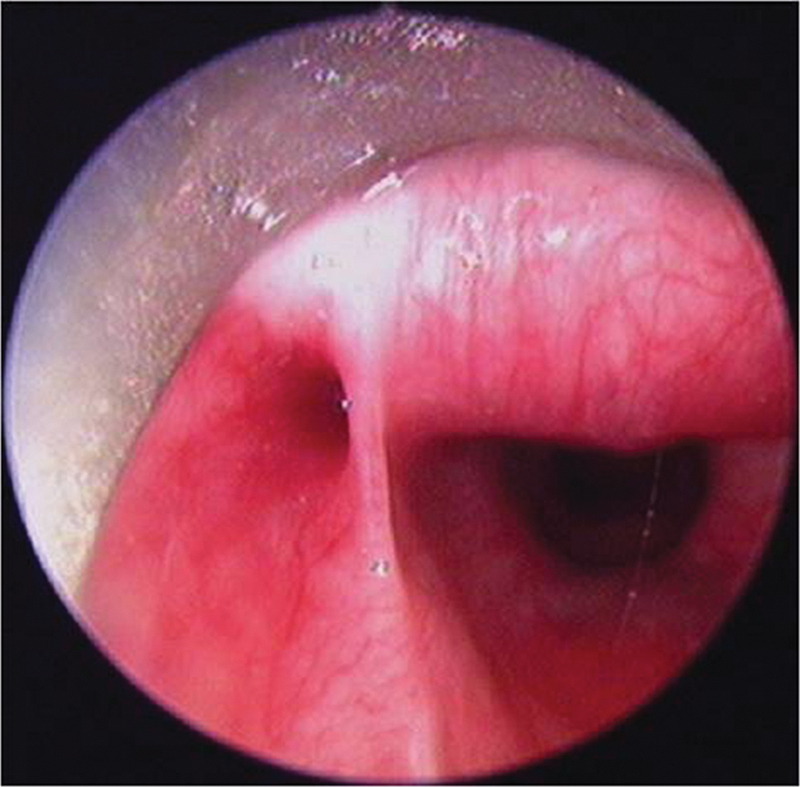
Endoscopic view of the internal opening in the apex of left pyriform sinus.
Fig. 3.
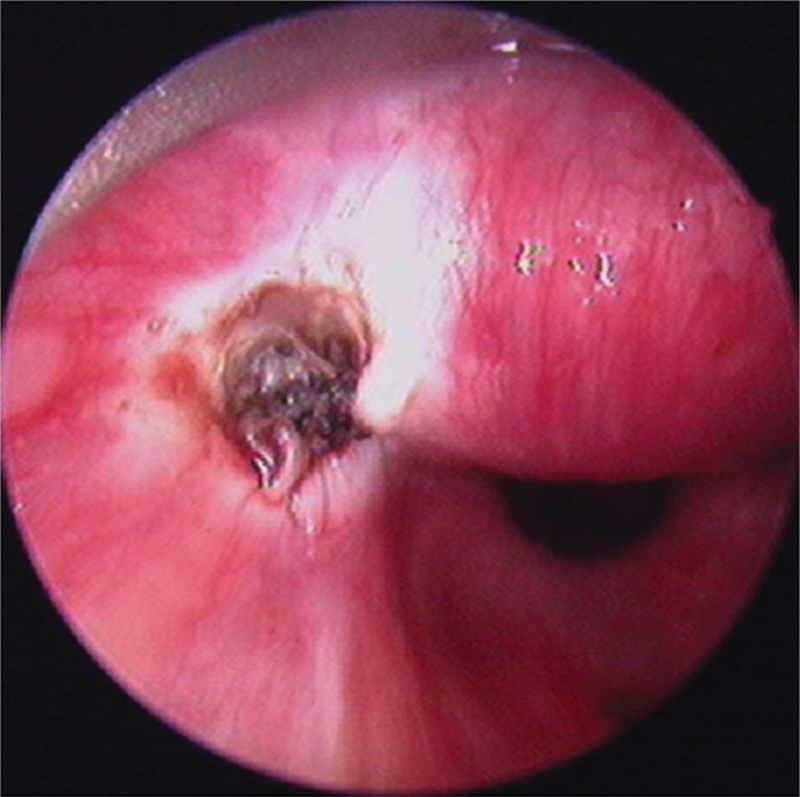
The internal opening following cauterization.
Fig. 4.

CT scan of the neck showing the sinus communicating with the left pyriform sinus.
Fig. 5.

MRI showing a neck abscess.
Procedure
External Approach
Only one patient had an external opening due to a previous failed drainage procedure. The remaining four patients had sinuses. A horizontal skin crease incision was done and a subplatysmal flap was raised. The authors identified the fistulous tract and dissected it until it was free from other tissue. Surrounding fibrosis due to previous drainage procedures made these steps a challenge. The fibrous tract was traced to the thyroid in all patients, although, on one patient, it only involved the left thyroid lobe. This patient underwent a left hemithyroidectomy. The tract was traced to the apex of the pyriform sinus in all patients, thus, proving that it was of fourth pouch origin. It was ligated at this level.
Endoscopic Approach
A direct hypopharyngoscopy is done and the internal opening was visualized. A 0° Hopkins rod endoscope with a camera is inserted into the hypopharyngoscope. This provided a magnified image of the finding, which enabled photographic documentation and was also used for teaching purposes. The opening is then cannulated by a guide wire from CV catheter and was cauterized using monopolar cautery.
The patients were extubated and shifted to the general ward. Oral feeds resumed 4 hours after surgery. Sutures were removed 5 days after surgery. The patients were subsequently on follow-up.
Results
All patients were children. There were 3 girls and 2 boys. The youngest was 3 years old while the oldest was 16. The lesions occurred on the left side of the neck for all patients. In all cases, the internal opening of the sinus tract was confirmed by hypopharyngoscopy, and originated from the apex of the pyriform sinus, posterior to the fold made by the internal laryngeal nerve. In one case, surgical excision of the entire sinus tract was performed. In this patient, the sinus tract originated from the apex of the pyriform sinus, passed through the thyroid gland, and terminated in perithyroid tissue. This patient underwent a Left hemithyroidectomy with excision of the sinus tract.
The CT scans (n = 5) showed disease extending from the pyriform sinus apex through the strap muscle layer to the thyroid or perithyroid tissue in all patients. In all patients, abnormal soft-tissue swelling and enhancement along the course of the disease were evident on the CT scans. In two patients, the lesions ended at the perithyroid level. There were no cases involving the mediastinums below the sternal notch. The involved pyriform sinus fossae were deformed by adjacent soft-tissue inflammation in all patients. One patient had cutaneous opening in the left anterior portion of the neck. One patient had thyroid gland involvement, including swelling of the thyroid gland, poor definition of the thyroid margin, and loss of high attenuation of the affected lobe on CT scans after contrast enhancement. MR images, obtained from two patients, showed the same disease course as did the CT scans.
The patients continue to be under follow-up even after two years. There has been no evidence of recurrence in any of the patients (Table 1).
Table 1. Summary of patients.
| No. | Age | Year presented | Sex | Clinical presentation | Radiology |
|---|---|---|---|---|---|
| 1 | 3 | 2010 | F | Recurrent left-sided neck swelling I & D x 2 |
CT - Abscess extending from pyriform apex to supraclavicular fossa |
| 2 | 4 | 2011 | F | Recurrent left sided neck swelling I & D x 1 |
MRI - tract delineated to pyriform sinus |
| 3 | 16 | 2011 | M | Recurrent neck left sided abscess × 7 years I & D x 6 |
CT- Left thyroid lobe abscess +, |
| 4 | 8 | 2010 | F | Recurrent left sided neck abscess I & D x 3 Exploration for lymphangioma done elsewhere |
MRI- sinus tract seen communicating with Left pyriform sinus |
| 5 | 7 | 2009 | M | Recurrent left sided neck abscess I & D x 4 |
CT- abscess in high cervical region with possible communication with left pyriform sinus |
| No. | Age | Year presented | Sex | Hypophayngoscopy | Treatment | Status |
|---|---|---|---|---|---|---|
| 1 | 3 | 2010 | F | Internal opening in apex of pyriform sinus with pus | External excision of tract with endoscopic diathermy of internal opening | No recurrence |
| 2 | 4 | 2011 | F | Positive | Neck exploration with endoscopic diathermy | No recurrence |
| 3 | 16 | 2011 | M | Positive | Neck exploration, left hemithyroidectomy, endoscopic diathermy | No recurrence |
| 4 | 8 | 2010 | F | Positive | Neck exploration with endoscopic diathermy | No recurrence |
| 5 | 7 | 2009 | M | Positive | Neck exploration with endoscopic diathermy | No recurrence |
Abbreviations: CT, computerized tomography; I&D. incision and drainage; MRI, magnetic resonance imaging.
Discussion
Fourth branchial pouch anomalies are rare, representing only 1–4% of branchial apparatus anomalies.6 They commonly occur as recurrent abscesses involving the neck and thyroid glands.1 2 3 12 13 An anomaly can present as a sinus, a cyst or a fistula. A sinus has an opening either in the pyriform sinus or the skin but not both; a cyst does not have an opening; a fistula has an internal opening in the pyriform sinus and external opening in the skin, which makes it an epithelized tract.8 Sinuses and be converted into fistulae by repeated I&D procedures.
The third and fourth branchial pouches are connected to the developing pharynx by the pharyngobranchial duct, which degenerates by the 7th week of intrauterine life. Failure to degenerate results in a 3rd or 4th branchial pouch anomaly.4 5 The course of the anomalies involving 3rd and 4th branchial pouches is well described in literature. It is difficult to differentiate clinically between the two anomalies, though a definitive diagnosis can be established by radiological means and direct hypopharyngoscopy.
The fistulous tract of a fourth branchial pouch originates at the apex of the pyriform sinus and descends to exit the pharynx inferior to the superior laryngeal nerve, cricothyroid muscle, and thyroid cartilage. The tract continues to descend lateral to the trachea and recurrent laryngeal nerve. On the left side, the tract curves forward, under the arch of the aorta, and then courses upward posterior to the internal carotid artery. On the right side, although rare, the tract circles forward underneath the subclavian artery before ascending. The tract proceeds superiorly, coursing over the hypoglossal nerve and, possibly, open externally in the neck at the lower anterior portion of the sternocleidomastoid muscle.4 5 There have only been a handful of cases in the literature claiming a true fourth pouch fistula10; none of our patients had a true fourth pouch fistula. All of them had blind sinuses which terminated in the neck and thyroid gland. The single patient with an external opening had it as a result of an I&D procedure.
A fistulous tract of a third branchial apparatus abnormality has a similar course to a fourth arch anomaly, albeit it exits the pharynx superior to the superior laryngeal nerve. The internal opening in the pyriform sinus is also located higher up in the lateral wall rather than at the apex.4 5 9
The common symptoms of a fourth branchial pouch anomaly include recurring deep neck infections or abscesses, as well as soft fluctuant masses.2 11 14 Third and fourth branchial arch anomalies may also lead to acute suppurative thyroiditis. For this reason, some authors recommend investigating the presence of a branchial arch anomaly in all cases of thyroiditis.1 2 3 12 13 It is important to run diagnostic tests to demonstrate a sinus or fistula originating in the pyriform sinus. A barium esophagogram can detect these findings but this procedure should only be done after the acute infection has resolved.12 15 CT and magnetic resonance imaging (MRI) are the modalities of choice for displaying both location and extent of pyriform sinus anomalies, as well as thyroid involvement.11 14 We performed direct hypopharyngoscopies in all our patients prior to open surgery to confirm our diagnosis and to cauterize the internal opening so as to abolish recurrence.17
All patients had been referred to the authors and had undergone multiple external drainage procedures. It was imperative to consider a diagnosis of fourth branchial pouch anomaly for these patients. The recommended treatment for fourth branchial anomalies is a complete surgical excision of the tract.8 11 14 15 16 The most commonly used approach is the external one, which involves complete exposure of the thyroid ala and carotid sheath on the affected side to expose the fistulous tract. The use of endoscopic cauterization limited to the sinus tract origin as a less-invasive procedure has been noted. Recently, use of sclerotherapy with OK-432 has been expanded to treat branchial cleft cysts.17 18 The authors formulated a combined treatment modality for all our patients involving the pediatric surgeon and Otorhinolaryngologist. All the patients underwent external surgery with a concomitant therapeutic hypopharyngoscopy to ensure complete excision of the anomalous tract. We did not use any chemical agents to cauterize the internal opening. The use of electro cautery was adequate. Due to the high incidence of secondary infection of these anomalies, early excision is recommended. A thorough examination is critical, and cannulation of the tract under direct visualization with a small catheter is very helpful in aiding a complete and safe dissection. Due to the intimacy of tracheal structures and fibrosis, it is often ideal to remove a portion of the thyroid gland as well.
Conclusion
Fourth branchial pouch anomalies present a challenge to the clinician due to their rarity and ambiguous presentation. A detailed clinical history and examination should arouse suspicion. Radiology and diagnostic hypopharyngoscopy will confirm the diagnosis. Once diagnosed, early treatment is critical due to the high incidence of complications. The authors advocate a combined treatment involving external surgery with internal cauterization of the mucosal communication to eradicate the disease process.
Key Points
Fourth branchial pouch anomaly is rare
Presents as recurrent neck abscess and thyroiditis mostly in children
MRI and Direct hypopharyngoscopy are confirmatory tools
Surgical exploration and excision of the tract is the treatment
Hemithyroidectomy may be needed if the thyroid lobe is involved
Cauterization of the internal opening prevents recurrence in all patients
Financial Disclosures
None.
Footnotes
Conflict of Interest None.
References
- 1.Takai S I, Miyauchi A, Matsuzuka F, Kuma K, Kosaki G. Internal fistula as a route of infection in acute suppurative thyroiditis. Lancet. 1979;1(8119):751–752. doi: 10.1016/s0140-6736(79)91208-x. [DOI] [PubMed] [Google Scholar]
- 2.Lucaya J, Berdon W E, Enriquez G, Regas J, Carreno J C. Congenital pyriform sinus fistula: a cause of acute left-sided suppurative thyroiditis and neck abscess in children. Pediatr Radiol. 1990;21(1):27–29. doi: 10.1007/BF02010809. [DOI] [PubMed] [Google Scholar]
- 3.Tovi F, Gatot A, Bar-Ziv J, Yanay I. Recurrent suppurative thyroiditis due to fourth branchial pouch sinus. Int J Pediatr Otorhinolaryngol. 1985;9(1):89–96. doi: 10.1016/s0165-5876(85)80007-0. [DOI] [PubMed] [Google Scholar]
- 4.Williams P L. New York, NY: Churchill Livingstone; 1995. Gray's Anatomy (38th ed.) [Google Scholar]
- 5.Benson M T, Dalen K, Mancuso A A. et al. Congenital anomalies of the branchial apparatus: embryology and pathologic. Radiographics. 1992;12:943–960. doi: 10.1148/radiographics.12.5.1529135. [DOI] [PubMed] [Google Scholar]
- 6.Shrime M, Kacker A, Bent J, Ward R F. Fourth branchial complex anomalies: a case series. Int J Pediatr Otorhinolaryngol. 2003;67(11):1227–1233. doi: 10.1016/j.ijporl.2003.07.015. [DOI] [PubMed] [Google Scholar]
- 7.Tucker H M, Skolnick M L. Fourth branchial cleft (pharyngeal pouch) remnant. Trans Am Acad Ophthalmol Otolaryngol. 1973;77(5):ORL368–ORL371. [PubMed] [Google Scholar]
- 8.Godin M S Kearns D B Pransky S M Seid A B Wilson D B Fourth branchial pouch sinus: principles of diagnosis and management Laryngoscope 1990100(2 Pt 1):174–178. [DOI] [PubMed] [Google Scholar]
- 9.Nicoucar K, Giger R, Jaecklin T, Pope H G Jr, Dulguerov P. Management of congenital third branchial arch anomalies: a systematic review. Otolaryngol Head Neck Surg. 2010;142(1):21–2800. doi: 10.1016/j.otohns.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 10.Patel A B, Hinni M L. The fourth branchial complex anomaly: a rare clinical entity. Case Rep Otolaryngol. 2011;2011:958652. doi: 10.1155/2011/958652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yang C, Cohen J, Everts E, Smith J, Caro J, Andersen P. Fourth branchial arch sinus: clinical presentation, diagnostic workup, and surgical treatment. Laryngoscope. 1999;109(3):442–446. doi: 10.1097/00005537-199903000-00019. [DOI] [PubMed] [Google Scholar]
- 12.Cases J A, Wenig B M, Silver C E, Surks M I. Recurrent acute suppurative thyroiditis in an adult due to a fourth branchial pouch fistula. J Clin Endocrinol Metab . 2000;85(3):953–956. doi: 10.1210/jcem.85.3.6481. [DOI] [PubMed] [Google Scholar]
- 13.Tovi F, Gatot A, Bar-Ziv J, Yanay I. Recurrent suppurative thyroiditis due to fourth branchial pouch sinus. Int J Pediatr Otorhinolaryngol. 1985;9(1):89–96. doi: 10.1016/s0165-5876(85)80007-0. [DOI] [PubMed] [Google Scholar]
- 14.Liberman M, Kay S, Emil S. et al. Ten years of experience with third and fourth branchial remnants. J Pediatr Surg. 2002;37(5):685–690. doi: 10.1053/jpsu.2002.32253. [DOI] [PubMed] [Google Scholar]
- 15.Nonomura N, Ikarashi F, Fujisaki T, Nakano Y. Surgical approach to pyriform sinus fistula. Am J Otolaryngol. 1993;14(2):111–115. doi: 10.1016/0196-0709(93)90049-d. [DOI] [PubMed] [Google Scholar]
- 16.Kubota M, Suita S, Kamimura T, Zaizen Y. Surgical strategy for the treatment of pyriform sinus fistula. J Pediatr Surg. 1997;32(1):34–37. doi: 10.1016/s0022-3468(97)90087-7. [DOI] [PubMed] [Google Scholar]
- 17.Kim M G, Lee N H, Ban J H, Lee K C, Jin S M, Lee S H. Sclerotherapy of branchial cleft cysts using OK-432. Otolaryngol Head Neck Surg. 2009;141(3):329–334. doi: 10.1016/j.otohns.2009.05.022. [DOI] [PubMed] [Google Scholar]
- 18.Kim K H, Sung M W, Koh T Y, Oh S H, Kim I S. Pyriform sinus fistula: management with chemocauterization of the internal opening. Ann Otol Rhinol Laryngol. 2000;109(5):452–456. doi: 10.1177/000348940010900503. [DOI] [PubMed] [Google Scholar]


