Abstract
Background
It is now debated whether the screening of heavy smokers for lung cancer with low dose computed tomography (low dose CT) might lower their mortality due to lung cancer. We use data from the National Lung Screening Trial (NLST) in the USA to predict the likely effects of such screening in Germany.
Methods
The number of heavy smokers aged 55–74 in Germany was extrapolated from survey data obtained by the Robert Koch Institute. Published data from the NLST were then used to estimate the likely effects of low dose CT screening of heavy smokers in Germany.
Results
If low dose CT screening were performed on 50% of the heavy smokers in Germany aged 55–74, an estimated 1 329 506 persons would undergo such screening. If the screening were repeated annually, then, over three years, 916 918 screening CTs would reveal suspect lesions, and the diagnosis of lung cancer would be confirmed thereafter in 32 826 persons. At least one positive test result in three years would be obtained in 39.1% of the participants (519 837 persons). 4155 deaths from lung cancer would be prevented over 6.5 years, and the number of persons aged 55–74 who die of lung cancer in Germany would fall by 2.6%. 12 449 persons would have at least one complication, and 1074 persons would die in the 60 days following screening.
Conclusion
The screening of heavy smokers for lung cancer can lower their risk of dying of lung cancer by 20% in relative terms, corresponding to an absolute risk reduction of 0.3 percentage points. These figures can provide the background for a critical discussion of the putative utility of this type of screening in Germany.
The National Lung Screening Trial (NLST), completed in 2011, provided a new evidential basis for the use of low dose computed tomography (low dose CT) to screen for lung cancer (1). Altogether, this randomized study included 53 454 heavy smokers in the age group 55 to 74 years. The participants underwent either conventional radiographic examination or low dose thoracic CT (average effective dose 1.4 mSv; estimated organ dose for the lungs 4.5 mGy [2]) annually for a period of 3 years. The median observation period thereafter was 6.5 years.
Lung cancer mortality was 1.3% in the low dose CT group and 1.6% in the conventional radiography group. The number needed to screen (NNS) in order for low dose CT to prevent one additional lung cancer death among persons who had already undergone at least one screening was 320. Overall mortality was also lower for low dose CT (7.0%) than for conventional radiography (7.5%).
A Cochrane Review of screening for lung cancer revealed that yearly low dose CT screening is associated with reduced lung cancer mortality in high-risk smokers. The authors remarked, however, that further data on cost effectiveness and the relationship between benefit and harm in various risk groups and settings are required (3).
The authors of the NLST drew attention to the following limitations of the study:
Healthier smokers may have been particularly attracted to participate.
CT scanning technology has advanced since the end of the study period (August 2002 to September 2007).
The study was carried out in specialized lung cancer centers.
The effect of screening for longer than 3 years could not be estimated.
Together with a high rate of false-positive findings, the rate of overdiagnosis could not be estimated.
The risk of radiation-induced cancer remains to be analyzed.
The last two points have since been addressed with the aid of statistical models. Other authors have also raised a number of questions that need to be answered before a position can be elaborated with regard to population-related low dose CT screening (4, 5).
Even with these limitations/problems, and although a meta-analysis of European studies is being planned (6), public debate of the benefits and risks of screening for lung cancer is inevitable. The discussion has recently been fueled by the decision of the US Centers for Medicare and Medicaid Services to cover the cost of low dose CT screening for those insured by Medicare (7).
Elaboration of a position for low dose CT screening in Germany requires consideration of issues with a bearing on the willingness of the population to undergo screening: the examination should be brief, universally available, minimally invasive, and free of charge for the participant and should involve low levels of pain and risk. The screening should be of high quality, and suspect findings should have clear consequences (8).
Our aim in writing this article is to extrapolate the results of low dose CT screening in the NLST to a population-wide lung cancer screening program in Germany and thus to provide a basis for critical discussion of such screening for lung cancer in this country. It is expressly not the aim of this article to criticize, express opinions, or take a position with regard to low dose CT screening.
Material and methods
The number of heavy smokers in the age group 55 to 74 years (reflecting the NLST participants) in the German population was estimated with the aid of data from the Robert Koch Institute (eBox 1). The key data of the NLST were extracted from the original publication (1). The low dose CT imaging findings were divided into positive, i.e., suspicious of lung cancer (non-calcified nodes at least 4 mm in diameter), other lesions (e.g., adenopathy or similar), and slight or no changes. The NLST definitions of minor, intermediate, and major complications are shown in eBox 2. The authors of the original NLST publication did not present a number needed to harm (NNH), so this was calculated from the published data (eBox 3).
eBox 1. Calculation of the number of heavy smokers in Germany, based on the data of the German Health Interview and Examination Survey for Adults.
Eligible for the National Lung Screening Trial (NLST) were persons in the age group 55–74 years with a smoking history of at least 30 pack-years (e1). Ex-smokers were eligible if they had stopped smoking no more than 15 years before inclusion in the study. To estimate how many men and women in Germany would fulfill the NLST criteria for participation in a low dose CT screening program, we used data from the German Health Interview and Examination Survey for Adults (DEGS) (e2). Out of the total of 7115 probands, 428 (6.0%) were excluded from estimation of the prevalence of heavy smoking owing to the absence of data on smoking status, time since giving up smoking, or number of pack-years.
The NLST excluded probands with a history of lung cancer. The estimated 10-year prevalence of lung cancer for men/women in the age groups 50–59, 60–69, and 70–79 years in Germany was, respectively, 0.17%/0.09%, 0.40%/0.14%, and 0.63%/0.16% (e3). The number of persons in Germany eligible for lung cancer screening according to the NLST inclusion criteria was corrected on the basis of these figures.
Further, study-related reasons for exclusion such as thoracic CT in the 18 months immediately preceding recruitment (e1), hemoptysis (e2), or unexplained weight loss exceeding 6.8 kg in the previous 12 months (e3) were not considered, because there are no population-based prevalence data for these factors in heavy smokers. The prevalences calculated per 5-year age band for men and women in Germany who fulfilled the inclusion criteria were statistically weighted by a factor calculated according to the disproportionate sampling design (e4).
eBox 3. Derivation of the number needed to harm (NNH).
The authors of the National Lung Screening Trial (NLST) (1) reported the number needed to screen (NNS), but did not discuss NNH. According to a recent Cochrane Review, screening using chest radiography yields no benefit for the patient (e5); this means that the NNS for the NLST can be applied to Germany although no systematic screening by means of chest radiography has yet taken place in this country.
With regard to the NNH for Germany, however, it is unclear whether the situation here is better described by the difference in risk from the chest radiography group or from no chest radiography screening. Therefore we report a range of NNH with a lower limit of 0% relative frequency and an upper limit defined by the observed relative frequency of complications in the chest radiography group of the NLST. The denominator of relative frequency of complications was 26 722 persons in the low dose CT group and 26 732 in the chest radiography group.
Table - eBox 3. Derivation of the number needed to harm (NNH).
| Complications | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Low dose CT | Chest radiography | Persons | Risk | NNH | |||||
| Lung cancer | Confirmed | Not confirmed | Confirmed | Not confirmed | CT | Chest radiography | CT | Chest radiography | |
| NNH derivation with chest radiography screening | |||||||||
| Major | 75 | 12 | 24 | 4 | 26722 | 26732 | 0.00325574 | 0.00104743 | 453 |
| Intermediate | 95 | 44 | 35 | 9 | 26722 | 26732 | 0.00520171 | 0.00164597 | 281 |
| Minor | 14 | 5 | 6 | 3 | 26722 | 26732 | 0.00071102 | 0.00033668 | 2671 |
| At least one complication | 184 | 61 | 65 | 16 | 26722 | 26732 | 0.00916848 | 0.00303008 | 163 |
| Death | 10 | 11 | 11 | 3 | 26722 | 26732 | 0.00078587 | 0.00052372 | 3815 |
| NNH derivation without chest radiography screening | |||||||||
| Major | 75 | 12 | 24 | 4 | 26722 | 26732 | 0.00325574 | 0 | 307 |
| Intermediate | 95 | 44 | 35 | 9 | 26722 | 26732 | 0.00520171 | 0 | 192 |
| Minor | 14 | 5 | 6 | 3 | 26722 | 26732 | 0.00071102 | 0 | 1406 |
| At least one complication | 184 | 61 | 65 | 16 | 26722 | 26732 | 0.00916848 | 0 | 109 |
| Death | 10 | 11 | 11 | 3 | 26722 | 26732 | 0.00078587 | 0 | 1272 |
CT, computed tomography
The relative frequencies of events and adverse effects in the NLST were applied to the portion of the German population that fulfilled the smoking history criteria of the original publication (1). It was assumed that only 50% of these persons would take part in low dose CT screening.
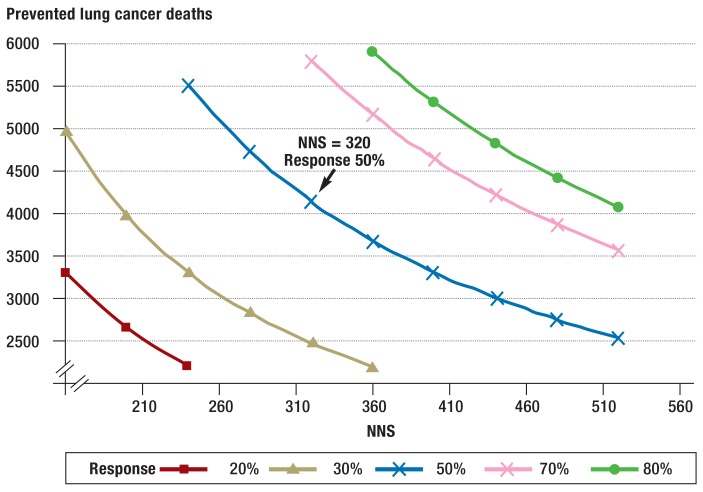
The influence of the NNS and willingness to participate on the number of avoidable lung cancer deaths (Np) was investigated in a sensitivity analysis. Npis calculated from the number of eligible persons Ne, the willingness to participate R, and the NNS: Np= Ne×R/NNS.
The estimated rate of overdiagnosis was taken from the work of Patz et al. (9). All existing official pronouncements by organizations and professional bodies were identified by a systematic survey of the published literature (search term: “lung cancer screening” [title], N = 643 publications; 10 May 2015) (eTable 1).
eTable 1. Recommendations of organizations and professional bodies on the topic of lung cancer screening, in chronological order.
| Organization | Year | Reference | Tendency* | Statement |
| American Association for Thoracic Surgery (AATS) | 2012 | (e6) | + | Screening according to the NLST – Also for patients aged 50 years or more with at least criteria recommended 20 pack-years |
| French multidisciplinary expert panel; Groupe d’Oncologie de Langue Francaise (GOLF) | 2013 | (e7) | (+) | Individual screening based on the NLST criteria recommended |
| Austrian Society of Radiology and Austrian Society of Pneumology | 2013 | (e8) | + | Screening based on the NLST criteria recommended;detailed patient information and standardized investigation of positive findings required |
| American Cancer Society | 2013 | (e9) | + | Screening analogous to the NLST criteria recommended |
| International Association for the Study of Lung Cancer (IASLC) and Strategic Screening Advisory Committee (SSAC) | 2014 | (e10) | (+) | Screening analogous to the NLST criteria recommended, but only at specialized centers
|
| Multidisciplinary expert panel of the Swiss university hospitals | 2014 | (e11) | – | Screening exclusively in the context of a national observational study recommended |
| American Lung Association | 2014 | (e12) | + | Screening analogous to the NLST criteria recommended, but only at specialized centers |
| American Academy of Family Physicians | 2014 | (e12) | – | Screening cannot be recommended on the basis of a single study |
| German Respiratory Society, German Thoracic Surgery Society, and German Röntgen Society | 2014 | (e13) | – | Lung cancer screening currently not recommended |
| United States Preventive Services Task Force | 2015 | (e14) | + | Screening analogous to the NLST criteria recommended
|
| European Society of Radiology (ESR) and European Respiratory Society (ERS) | 2015 | (e15) | (+) | Lung cancer screening recommended in clinical studies or at certified multidisciplinary centers |
| American College of Radiology | 2015 | (e16) | + | Screening analogous to the NLST criteria recommended, but only at specialized centers |
| American College of Chest Physicians and American Thoracic Society | 2015 | (e17) | + | Screening recommended |
| National Comprehensive Cancer Network (NCCN) | 2015 | (e18) | + | Screening analogous to the NLST criteria recommended |
*This rating sums up the respective authors’ current recommendation regarding introduction of lung cancer screening: + = in favor of screening;
(+) = tendency towards endorsement of screening under certain conditions; – = rejection of screening at the current time.NLST, National Lung Screening Trial
Results
Table 1 summarizes the results of the NLST. The rate of positive findings, i.e., suspicion of tumor, was much higher in the low dose CT group, although the proportion of false-positive results was almost identical between the two groups. Thirty-nine percent of those in the low dose CT group and 16% in the conventional radiography group had at least one positive screening result. While the incidence of lung cancer was higher in the low dose CT group (645 per 100 000 person-years) than in the radiography group (572 per 100 000 person-years; relative effect size 1.13, 95% confidence interval [95% CI] 1.03 to 1.23), lung cancer mortality and overall mortality were lower for the low dose CT group than for the radiography group (lung cancer mortality: 247 versus 309 per 100 000 person-years; overall mortality: 1877 versus 2000, rate not reported). The absolute reduction in risk of lung cancer mortality (median duration of follow-up 6.5 years) was 0.3 percentage points (from 1.6 to 1.3%), corresponding to a relative risk reduction of 20% (mortality ratio 0.80; 95% CI 0.73 to 0.93).
Table 1. Results of the National Lung Screening Trial (1).
| Low dose CT | Conventional chest radiography | Relative effect size | 95% CI | |||
|---|---|---|---|---|---|---|
| N | % | N | % | |||
| Participants | 26722 | 26732 | ||||
| Compliance | 95.0 | 93.0 | ||||
| Screening examinations | 75126 | 73470 | ||||
| Positive results | 18146 | 24.2 | 5043 | 6.9 | ||
|
17 497 | 96.4 | 4764 | 94.5 | ||
|
649 | 3.6 | 279 | 5.5 | ||
| Conspicuous result without suspicion of malignancy | 5622 | 7.5 | 1575 | 2.1 | ||
| At least one positive result (proportion of participants) | 39.1 | 16.0 | ||||
| Lung cancer diagnosed | 1060 | 941 | ||||
|
649 | 279 | ||||
|
44 | 137 | ||||
|
367 | 525 | ||||
| Program sensitivity*2 | 94.1 | 67.9 | ||||
| Incidence of lung cancer (per 100000 person years) | 645 | 572 | 1.13 | 1.03–1.23 | ||
| Deaths (from any cause) | 1877 | 2000 | ||||
| Relative reduction in overall mortality (%) | 6.7 | 1.2–13.6 | ||||
| Unknown cause of death | 12 | 9 | ||||
| Known cause of death | 1865 | 1991 | ||||
|
427 | 22.9 | 503 | 25.3 | ||
|
416 | 22.3 | 442 | 22.2 | ||
|
486 | 26.1 | 470 | 23.6 | ||
|
175 | 9.4 | 226 | 11.4 | ||
|
12 | 0.6 | 7 | 0.4 | ||
|
349 | 18.7 | 343 | 17.2 | ||
| Lung cancer deaths, without DCO | 356 | 443 | ||||
| Lung cancer mortality (per 100000), without DCO | 247 | 309 | 0.80 | 0.73–0.93 | ||
| Relative risk reduction (%) | 20.0 | 6.8–26.7 | ||||
| Participants with at least one screening | 26455 | 26232 | ||||
|
346 | 1.3 | 425 | 1.6 | ||
| Number needed to screen | 320 | |||||
| Number needed to harm*3 | ||||||
|
307–453 | |||||
|
192–281 | |||||
|
1406–2671 | |||||
|
109–163 | |||||
|
1272–3815 | |||||
*1Altogether there were 3875 death certificates, 1877 in the low dose CT group and 1998 in the conventional radiography group; the cause of death was unknown in 12 and 7 persons respectively; the denominators for the percentages of causes of death relate to all deaths for which the cause was known, i.e., 1865 and 1991 deaths respectively; overall (low dose CT and conventional radiography) lung cancer was diagnosed 892 times, n=35 in participants who were not screened at all, n=802 in screened participants but after the end of the screening phase, and n=55 in persons who were The program scheduled for but had not yet undergone screening
*2sensitivity for the first 3 years was calculated from the data of Patz et al. See (9).
*3 eBox 3
CT, computed tomography; N, number; 95% CI, 95% confidence interval; DCO, death certificate only (deaths for which the death certificate is the only source of information); for definitions of major, intermediate, and minor complications, see eBox 2
Applying the inclusion criteria of the NLST, 2 659 012 persons in Germany would be eligible for low dose CT screening. This group comprises 13.6% of all 55 to 74-year-olds in the country (eTable 2). If 50% were willing to participate, 1 329 506 persons would be screened. Application of the NLST parameters to this population would necessitate 3 796 404 low dose CT investigations over a 3-year period, 916 918 of which would arouse suspicion of a tumor. Alongside clinical examination, clarification would involve 530 712 diagnostic imaging procedures (including thoracic CT in 456 167 cases). Invasive procedures such as bronchoscopy or exploratory surgery would take place in 71 703 cases. The suspicion of lung cancer would be confirmed in 32 826 persons (Table 2). The rate of true-positive screening results is therefore 6.3% in relation to all 519 837 persons with at least one positive screening result and 3.6% for all 916 918 of screenings arousing suspicion of a tumor.
eTable 2. Estimated number of persons in the age group 55 to 74 years in Germany in 2010 fulfilling the criteria of the National Lung Screening Trial (NLST) for low dose CT screening.
| History of at least 30 pack-years*1 | Eligible persons (n) | |||||||
|---|---|---|---|---|---|---|---|---|
| Age (years) | Population*2 (n) | Lung cancer prevalence | Adjusted population (n) | Current smokers (%) | Previous smokers (%) | Current smokers | Previous smokers | Total |
| Men | ||||||||
| 55–59 | 2812652 | 0.0017 | 2807870 | 11.67 | 8.75 | 327678 | 245689 | 573367 |
| 60–64 | 2478851 | 0.0040 | 2468936 | 8.98 | 11.34 | 221710 | 279977 | 501687 |
| 65–69 | 1922351 | 0.0040 | 1914662 | 4.93 | 13.30 | 94393 | 254650 | 349043 |
| 70–74 | 2269990 | 0.0063 | 2255689 | 3.68 | 5.45 | 83009 | 122935 | 205944 |
| Total | 9483844 | 9447157 | 726790 | 903251 | 1630041 | |||
| Women | ||||||||
| 55–59 | 2835731 | 0.0009 | 2833179 | 10.64 | 5.51 | 301450 | 156108 | 457558 |
| 60–64 | 2581663 | 0.0014 | 2578049 | 8.01 | 4.56 | 206502 | 117559 | 324 061 |
| 65–69 | 2070891 | 0.0014 | 2067992 | 4.78 | 2.18 | 98850 | 45082 | 143932 |
| 70–74 | 2609224 | 0.0016 | 2605049 | 1.45 | 2.52 | 37773 | 65 647 | 103420 |
| Total | 10097509 | 10084269 | 644575 | 384396 | 1028971 | |||
| Men and women together | 2659012 | |||||||
*1 Estimates from the German Health Interview and Examination Survey for Adults (DEGS). No correction was made for the higher prevalence of lung cancer in heavy smokers than in the general population.
*2German population on 31 December 2012, minus the proportion of persons with known lung cancer; weighted prevalences of current and past smokers (cessation of smoking at least 15 years previously) with at least 30 pack-years from the DEGS. CT, computed tomography
Table 2. Hypothetical calculation of key data on diagnostic follow-up of screening participants in Germany who had one positive result (i.e., tumor suspected) in three rounds of low dose CT screening.
| Variable | Number of personsn | Proportion of positive results | Number of positive results |
|---|---|---|---|
| Positive result (tumor suspected) | |||
| T0 (100%) | 1329506 | 0.2733 | 363354 |
| T1 (93.94%) | 1248938 | 0.2792 | 348703 |
| T2 (91.61%) | 1217960 | 0.1682 | 204861 |
| Total positive results | 916918 | ||
| Lung cancer confirmed | 0.0358 | 32826 | |
| Lung cancer not confirmed | 0.9642 | 884092 | |
| Full information on diagnostic follow-up* | 916918 | ||
| At least one diagnostic follow-up examination | 0.7207 | 660823 | |
| Clinical examination | 0.5892 | 540248 | |
| Imaging procedures | 0.5788 | 530712 | |
|
0.1439 | 131945 | |
|
0.4975 | 456167 | |
|
0.0831 | 76196 | |
| Percutaneous cytology | 0.0182 | 16688 | |
|
0.0143 | 13112 | |
|
0.0045 | 4126 | |
| Bronchoscopy | 0.0379 | 34751 | |
|
0.0181 | 16596 | |
|
0.0221 | 20264 | |
| Operation | 0.0403 | 36952 | |
|
0.0066 | 6052 | |
|
0.0132 | 12103 | |
|
0.0288 | 26407 | |
| Other procedures | 0.0185 | 16963 | |
T0, T1, T2: first, second, and third annual screening; participation of 50% of the 2659014 heavy smokers in Germany who fulfilled the study criteria in the first screening was assumed. The relative decrease in cohort size from T0 to T1 and T2 is identical with the relative decrease in size of the low dose CT arm of the National Lung Screening Trial (NLST). In the NLST information on diagnostic follow-up in 2.4% of the persons with a positive result was missing. For our calculation we assumed that no data were missing.
*In contrast to the NLST, we assume availability of complete diagnostic work-up on all participants with a positive screening result. CT, computed tomography; n, number; FDG PET, fluorodeoxyglucose positron emission tomography
According to Patz et al., 6073 (18.5%) of the 32 826 lung cancer diagnoses would represent overdiagnosis (9). Over the 3 years of screening there would be at least one positive screening result in 519 837 participants (39.1%), in 487 011 of whom further investigation would reveal no lung cancer. For the 1 329 506 persons screened, an NNS of 320 would mean prevention of 4155 lung cancer deaths (without “death certificate only” [DCO] cases) in the 6.5 years of follow-up. The sensitivity analyses show that the number of preventable lung cancer deaths is strongly dependent both on the readiness of heavy smokers to participate and on the NNS. For example, with a participation rate of only 30% and a higher NNS (e.g., 360) the number of preventable lung cancer deaths would be 2216 (Figure).
Figure.
Prevented deaths from lung cancer in Germany by participation rate and number needed to screen (NNS)
The extrapolation of prevented lung cancer deaths from the National Lung Screening Trial (NLST) data relates to the number of 2 659 012 heavy smokers in the age group 55 to 74 years. The principal analysis (arrow) was based on the assumption that 50% of persons in this age bracket would be willing to participate in a screening program, with an NNS of 320 (as in the NLST). In this scenario, 4155 lung cancer deaths would be prevented in Germany in the 6.5 years of follow-up. The individual curves show the impact of participation rate (20–80%) and NNS on the number of lung cancer deaths prevented
A 3-year screening program in Germany would be associated with at least one complication in the course of further investigation in 12 449 persons. According to the definition of the NLST there would be 4363 major complications, including death, and 1074 deaths (505 with and 569 without confirmation of lung cancer) would occur within 60 days of screening following highly invasive interventions. These deaths include mortality associated with confirmatory procedures and all other causes. Of the 884 092 participants with a positive screening result in whom lung cancer was suspected but not verified, 569 (0.06%) would suffer a major complication.
Discussion
Extrapolation from the NLST data reveals that 13.6% of all 55 to 74-year-olds in Germany—i.e., 2.7 million people—would be eligible for low dose CT lung cancer screening, should it be introduced. In heavy smokers, the anticipated reduction in relative and absolute risk, respectively, of death from lung cancer after three rounds of screening and a median observation time of 6.5 years would be 20% (relative risk reduction [RRR]) and 0.3 percentage points (absolute risk reduction [ARR]). An overview of the current recommendations issued by organizations and professional bodies can be found in eTable 1.
It can be calculated that low dose CT screening of heavy smokers in the age bracket 55 to 74 years would prevent 4155 deaths from lung cancer nationwide within 6.5 years. In 2013, 24 361 members of this age group died of lung cancer in Germany (www.gbe-bund.de, accessed on 5 January 2015). Assuming constant mortality over a 6.5-year period, a total of 158 347 persons aged 55 to 74 years would die of lung cancer. Screening of heavy smokers with a participation rate of 50% would prevent 2.6% of lung cancer deaths (4155/158 347) in this age group in the general population.
Implementation of a low dose CT screening program in Germany
In contrast to organized screening programs in which invitations are sent to all members of the population in the target group, use of residential registry data to invite all 55 to 74-year-olds to take part in low dose CT screening for lung cancer seems impractical, given that only 13.6% of those in this age bracket are current or previous heavy smokers. Planning is hampered by the lack of an organized system for invitation.
In the NLST, screened persons with suspected cancer were often investigated and, when necessary, treated at specialized lung centers. However, no standardized procedure for confirmatory investigation was defined. The NLST authors report that surgical resection in their study was associated with mortality of 1% (1). In a representative population study from the USA the mortality was 4% and the survival rate was related to the number of operations performed (10). Assuming that this connection between surgeon’s experience and patient survival also applies to Germany, if screening were introduced it would have to be decided to which institutions participants with suspected tumor should be referred. Germany currently has 43 lung centers certified by the German Cancer Society (DKG) (www.oncomap.de/index.php, accessed on 25 February 2015).
Cumulative effective radiation dose and damage
The expected number of radiation-related lung cancer deaths was calculated taking account of not only the low dose CT screening but also the follow-up CT examinations to clarify the nature of suspect lesions (11). Statistical models calibrated to the individual data from the NLST were used to this end. The extrapolations were made on the basis of a simulated cohort of 100 000 persons followed up from 45 to 90 years of age. In such a cohort, annual low dose CT screening of 55 to 74-year-old heavy smokers would prevent 459 deaths from lung cancer. However, 24 of those screened would die of lung cancer caused by the radiation received.
In contrast to the NLST, in which annual low dose CT screening was limited to 3 years, we simulated 20 low dose CT examinations plus the potential follow-up CT. This simulation in a group of 100 000 participants revealed that 141 lung cancers would be overdiagnosed (2.7% of all lung cancers and 8.7% of lung cancers detected by screening) (11). A further extrapolation—assuming yearly low dose CT screening (2 mSv) from 55 to 74 years of age and the necessary confirmatory investigations (follow-up CT; 8 mSv)—yielded a cumulative effective radiation dose (lungs) of up to 280 mSv (12).
The effective radiation dose from low dose CT scanners can be expected to fall further in future, resulting in fewer radiation-induced deaths from lung cancer. The existing sensitivity analyses suggest that, with the current models, the impact on prevented lung cancer deaths of a decreased radiation dose from modern CT scanners would be much lower than that of, for example, a change of 10% in either the participation rate or the NNS.
Possible measures to reduce false-positive results
In the NLST 64% of confirmatory examinations revealed nodes of no more than 7 mm in diameter. Repeated volumetric measurements of lesions, as practiced in the NELSON Trial (13) and the UK Lung Screen Pilot Trial (14), could further reduce the rate of false-positive results. Predictably, raising the minimum diameter of nodes to be referred for clarification lowers the rate of false positives. A minimum diameter of 8 mm (instead of 4 mm) in the NLST would have avoided 66% of the false-positive results and 10.5% of the lung cancers found on screening would have been diagnosed later or remained undetected (15).
In a follow-up publication the NLST collective was divided on the basis of various factors estimated from multivariate regression models into quintiles (Q) of 5-year lung cancer mortality risk (Q1: 0.15–0.55%; Q2: 0.56–0.84%; Q3: 0.85–1.23%; Q4: 1.24–2.00%; Q5: >2%) (eBox 4). From Q1 to Q5 the NNS went down from 5276 to 161. If screening were restricted to quintiles Q3 to Q5 (i.e., from an estimated 5-year lung cancer mortality risk of 0.85%), the NNS would be 208. The proportion of false positives would fall from 97% (Q1) to 88% (Q5). The ratio of the number of persons with false-positive results to the number of prevented lung cancer deaths would fall sharply from 1648 (Q1) to 65 (Q5). Eighty-eight percent of all lung cancer deaths preventable by screening would fall among the 60% of the total collective contained in the three highest quintiles (risk ≥ 0.85%) (16).
eBox 4. Determination of quintiles of 5-year lung cancer mortality risk.
The participants’ absolute risk of dying from lung cancer and their life expectancy were estimated using Cox proportional hazards regressions, taking account of competing risks. Individual characteristics (age, sex, ethnicity, body mass index, cigarette consumption in pack-years, years since end of smoking, emphysema, and lung cancer in first-degree relatives) were also considered. The risk model was validated using data from the radiography arm of the PCLO Trial (16).
Consequences for mental health
If around 520 000 persons in Germany have at least one screening result arousing suspicion of tumor over a 3-year period but cancer is confirmed in “only” approximately 33 000 persons in the following 6.5 years, that means some 487 000 men and women have a false-positive result with ensuing investigations and psychic stress. The NLST does not report the psychic consequences of false-positive findings. The NELSON Trial showed that after a second screening, anxiety and stress in persons whose first screening aroused suspicion of tumor or indicated another, non-oncological lesion decrease to the initial levels (17). In participants whose first screening revealed no abnormal findings, anxiety and stress sank to levels lower than before screening (18). A false-positive result was associated with a higher likelihood of giving up smoking. In the context of the NELSON Trial, it was observed that the rate of giving up smoking in the CT group was higher than the expected rate in the general population (14.5% versus 3–7%) (18). However, repeated negative screening could lead some participants to start smoking again.
Cost effectiveness of low dose CT screening
A detailed cost effectiveness analysis of the NLST data showed additional costs of US$ 1631 per screened person, associated with a gain of 0.0316 years of life and 0.0201 quality-adjusted life years (QALYs). The corresponding incremental cost–effectiveness ratio (ICER) was US$ 52 000 per extra year of life and US$ 81 000 per additional QALY (eBox 5). However, the results of this analysis were heavily dependent on the assumptions made (19).
eBox 5. Cost effectiveness of low dose computed tomography screening.
The incremental cost–effectiveness ratio (ICER) sums up the cost effectiveness of an action. The ICER is calculated by dividing the difference between the costs of two possible courses of action by the difference between their effects. Thus, it expresses the average additional cost per unit of difference. Black et al. (19) determined the incremental costs per year of life gained. An ICER of $ 52 000 per life year therefore means that $ 52 000 must be invested in low dose screening to gain one year of life.
For calculation of quality-adjusted life years (QALYs), the prolongation of life achieved by an action is multiplied by an estimation of life quality (utility value) that varies between 0 (worst conceivable quality of life) and 1 (best conceivable quality of life). If the low dose CT screening achieved on average 0.0316 additional years of life per person screened and the utility value were 0.636, the gain in QALY would be 0.0316 × 0.636 = 0.0201. According to the data of the NLST, therefore, one QALY is associated with costs of $ 81 000.
Summary
The data presented here for lung cancer screening by low dose CT provide a basis for critical discussion of the potential value of such screening in the German population. The extrapolations for Germany were made under the assumption that the results of the NLST are both internally valid and transferable to the population of this country.
Table 3. Hypothetical calculation of complications following the most invasive procedures for clarification of a positive result (tumor suspected) among participants in low dose CT screening in Germany.
| Thoracotomy, thoracoscopy, or mediastinoscopy | Bronchoscopy | Needle biopsy | Non-invasive procedure | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | Proportion | N | Proportion | N | Proportion | N | Proportion | N | Proportion | |
| Lung cancer confirmed | 25745 | 3844 | 1668 | 1569 | 32826 | |||||
| No complications | 17398 | 0.6758 | 3490 | 0.9079 | 1314 | 0.7879 | 1316 | 0.8387 | 23519 | 0.7165 |
| At least one complication | 8347 | 0.3242 | 354 | 0.0921 | 354 | 0.2121 | 253 | 0.1613 | 9307 | 0.2835 |
|
3591 | 0.1395 | 101 | 0.0263 | 0 | 0 | 101 | 0.0645 | 3794 | 0.1156 |
|
4096 | 0.1591 | 253 | 0.0658 | 354 | 0.2121 | 101 | 0.0645 | 4804 | 0.1463 |
|
656 | 0.0255 | 0 | 0 | 0 | 0 | 51 | 0.0323 | 707 | 0.0215 |
| Death within 60 days of the most invasive procedure | 252 | 0.0098 | 202 | 0.0526 | 51 | 0.0303 | 0 | 0 | 505 | 0.0154 |
| Lung cancer not confirmed | 8487 | 11 758 | 3448 | 860 398 | 884 092 | |||||
| No complications | 7142 | 0.8415 | 11 188 | 0.9515 | 3082 | 0.8939 | 859 538 | 0.9990 | 880 949 | 0.9964 |
| At least one complication | 1345 | 0,1585 | 570 | 0.0485 | 366 | 0.1061 | 860 | 0.0010 | 3142 | 0.0036 |
|
466 | 0.0549 | 103 | 0.0088 | 0 | 0.0000 | 0 | 0.0000 | 569 | 0.0006 |
|
673 | 0.0793 | 466 | 0.0396 | 313 | 0.0909 | 860 | 0.0010 | 2312 | 0.0026 |
|
207 | 0.0244 | 0 | 0.0000 | 52 | 0.0152 | 0 | 0.0000 | 259 | 0.0003 |
| Death within 60 days of the most invasive procedure | 104 | 0.0122 | 207 | 0.0176 | 0 | 0.0000 | 258 | 0.0003 | 569 | 0.0006 |
| All procedures for clarification of a positive result | 34232 | 15602 | 5116 | 861967 | 916918 | |||||
| No complications | 24540 | 0,7169 | 14678 | 0,9408 | 4396 | 0.8593 | 860854 | 0.9987 | 904468 | 0.9864 |
| At least one complication | 9692 | 0.2831 | 924 | 0.0592 | 720 | 0.1407 | 1113 | 0.0013 | 12449 | 0.0136 |
|
4057 | 0.1185 | 205 | 0.0131 | 0 | 0.0000 | 101 | 0.0001 | 4363 | 0.0048 |
|
4769 | 0.1393 | 719 | 0.0461 | 667 | 0.1304 | 962 | 0.0011 | 7116 | 0.0078 |
|
864 | 0.0252 | 0 | 0.0000 | 52 | 0.0102 | 51 | 0.0001 | 967 | 0.0011 |
| Death within 60 days of the most invasive procedure | 356 | 0.0104 | 409 | 0.0262 | 51 | 0.0099 | 258 | 0.0003 | 1074 | 0.0012 |
If a given diagnostic procedure was repeated in the same patient, the first procedure was counted; complications arising before the most invasive procedure were not included in analysis; each participant could have up to three positive screening results and thus be counted up to three times in each row of figures. Proportions were calculated for each column
Key Messages.
With a participation rate of 50%, annual screening of heavy smokers in the age group 55 to 74 years in Germany for a period of 3 years would result in detection of a suspected tumor in 916 918 examinations and confirmation of lung cancer in 32 826 persons.
There would be at least one positive screening result in 519 837 persons over the 3 years of screening, 487 011 of whom would be found not to have lung cancer on further investigation.
A total of 4155 deaths from lung cancer would be prevented over a period of 6.5 years, and the number of lung cancer deaths in the age group 55 to 74 years would decrease by 2.6%.
A total of 12 449 persons would suffer at least one complication, and 1074 persons would die within 60 days after the most invasive procedures.
eBox 2. Definition of complications in the National Lung Screening Trial.
-
Major complications:
Acute respiratory failure, anaphylaxia, bronchopulmonary fistula, cardiac arrest, cerebrovascular event (cerebral insult), heart failure, death, hemothorax requiring drainage, myocardial infarction, respiratory arrest, wound dehiscence, bronchial stump insufficiency requiring thoracostomy or drainage for more than 4 days, empyema, injury of vital organs or vessels, mechanical ventilation for more than 48 h after operation, thromboembolic events requiring intervention, chylus fistula, brachial plexopathy, collapsed lung, infarction of the sigmoid colon
-
Intermediate complications:
Blood loss requiring transfusion, cardiac arrhythmia requiring treatment, fever requiring administration of antibiotics, hospitalization after procedure, pain requiring referral to a pain specialist, pneumothorax requiring drainage, rib fracture(s), vocal cord immobility or paresis, infection requiring administration of antibiotics, cardiac ischemia (ST-segment elevation), bronchitis, pneumonia, pleural effusion, sepsis, respiratory distress, splenomegaly with splenic infarcts, mucous plug requiring bronchoscopy, steroid-induced diabetes
-
Minor complications:
Allergic reaction, bronchospasm, vasovagal reaction/hypotonia, subcutaneous emphysema, atelectases, pneumothorax not requiring treatment by drainage, ileus, seroma, paresthesias/hyperesthesias, others
Acknowledgments
Translated from the original German by David Roseveare.
Footnotes
Conflict of interest statement
Prof. Schuler has received payments for consulting (advisory board) from AstraZeneca, Boehringer Ingelheim, Novartis, and Celgene. He has received honoraria for expert advice in legal proceedings. He has received reimbursement of conference fees from Boehringer Ingelheim and Lilly. He has received financial support for studies (third-party funding) from AstraZeneca, Boehringer Ingelheim, BMS, Lilly, and Novartis. He is a member of the scientific advisory board of the Institute for Quality and Efficiency in Health Care (IQWIG).
The remaining authors declare that no conflict of interest exist.
References
- 1.Aberle DR, Adams AM, Berg CD, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365:395–409. doi: 10.1056/NEJMoa1102873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Larke FJ, Kruger RL, Cagnon CH, et al. Estimated radiation dose associated with low-dose chest CT of average-size participants in the National Lung Screening Trial. Am J Roentgenol. 2011;197:1165–1169. doi: 10.2214/AJR.11.6533. [DOI] [PubMed] [Google Scholar]
- 3.Manser R, Lethaby A, Irving LB, et al. Screening for lung cancer. Cochrane Database Syst Rev. 2013;6 doi: 10.1002/14651858.CD001991.pub3. CD001991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bach PB, Mirkin JN, Oliver TK, et al. Benefits and harms of CT screening for lung cancer: a systematic review. JAMA. 2012;307:2418–2429. doi: 10.1001/jama.2012.5521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Prokop M. Lung cancer screening: the radiologist’s perspective. Semin Respir Crit Care Med. 2014;35:91–98. doi: 10.1055/s-0033-1363455. [DOI] [PubMed] [Google Scholar]
- 6.Field JK, van KR, Pedersen JH, et al. European randomized lung cancer screening trials. Post NLST J Surg Oncol. 2013;108:280–286. doi: 10.1002/jso.23383. [DOI] [PubMed] [Google Scholar]
- 7.Schmidt C. Lung cancer screening poised to expand. J Natl Cancer Inst. 2015;107:6–7. doi: 10.1093/jnci/djv114. [DOI] [PubMed] [Google Scholar]
- 8.Giersiepen K, Hense HW, Klug SJ, Antes G, Zeeb H. [Planning, implementation and evaluation of cancer screening programs] Z Arztl Fortbild Qualitatssich. 2007;101:43–49. doi: 10.1016/j.zgesun.2006.12.027. [DOI] [PubMed] [Google Scholar]
- 9.Patz EF, Jr., Pinsky P, Gatsonis C, et al. Overdiagnosis in low-dose computed tomography screening for lung cancer. JAMA Intern Med. 2014;174:269–274. doi: 10.1001/jamainternmed.2013.12738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bach PB, Cramer LD, Schrag D, Downey RJ, Gelfand SE, Begg CB. The influence of hospital volume on survival after resection for lung cancer. N Engl J Med. 2001;345:181–188. doi: 10.1056/NEJM200107193450306. [DOI] [PubMed] [Google Scholar]
- 11.de Koning HJ, Meza R, Plevritis SK, et al. Benefits and harms of computed tomography lung cancer screening strategies: a comparative modeling study for the U.S. Preventive Services Task Force. Ann Intern Med. 2014;160:311–320. doi: 10.7326/M13-2316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McCunney RJ, Li J. Radiation risks in lung cancer screening programs: a comparison with nuclear industry workers and atomic bomb survivors. Chest. 2014;145:618–624. doi: 10.1378/chest.13-1420. [DOI] [PubMed] [Google Scholar]
- 13.van Klaveren RJ, Oudkerk M, Prokop M, et al. Management of lung nodules detected by volume CT scanning. N Engl J Med. 2009;361:2221–2229. doi: 10.1056/NEJMoa0906085. [DOI] [PubMed] [Google Scholar]
- 14.Baldwin DR, Duffy SW, Wald NJ, Page R, Hansell DM, Field JK. UK Lung Screen (UKLS) nodule management protocol: modelling of a single screen randomised controlled trial of low-dose CT screening for lung cancer. Thorax. 2011;66:308–313. doi: 10.1136/thx.2010.152066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gierada DS, Pinsky P, Nath H, Chiles C, Duan F, Aberle DR. Projected outcomes using different nodule sizes to define a positive CT lung cancer screening examination. J Natl Cancer Inst. 2014 106 doi: 10.1093/jnci/dju284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kovalchik SA, Tammemagi M, Berg CD, et al. Targeting of low-dose CT screening according to the risk of lung-cancer death. N Engl J Med. 2013;369:245–254. doi: 10.1056/NEJMoa1301851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.van den Bergh KA, Essink-Bot ML, Borsboom GJ, Scholten ET, van Klaveren RJ, de Koning HJ. Long-term effects of lung cancer computed tomography screening on health-related quality of life: the NELSON trial. Eur Respir J. 2011;38:154–161. doi: 10.1183/09031936.00123410. [DOI] [PubMed] [Google Scholar]
- 18.van der Aalst CM, van den Bergh KA, Willemsen MC, de Koning HJ, van Klaveren RJ. Lung cancer screening and smoking abstinence: 2 year follow-up data from the Dutch-Belgian randomised controlled lung cancer screening trial. Thorax. 2010;65:600–605. doi: 10.1136/thx.2009.133751. [DOI] [PubMed] [Google Scholar]
- 19.Black WC, Gareen IF, Soneji SS, et al. Cost-effectiveness of CT screening in the National Lung Screening Trial. N Engl J Med. 2014;371:1793–1802. doi: 10.1056/NEJMoa1312547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e1.Aberle DR, Adams AM, Berg CD, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365:395–409. doi: 10.1056/NEJMoa1102873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e2.Gößwald A, Lange M, Dölle R, Hölling H. [The first wave of the German Health Interview and Examination Survey for Adults (DEGS1): participant recruitment, fieldwork, and quality management] Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2013;56:611–619. doi: 10.1007/s00103-013-1671-z. [DOI] [PubMed] [Google Scholar]
- e3.Robert Koch-Institut. Entwicklungen der Prävalenzen zwischen 1990 und 2010. Berlin: 2010. Verbreitung von Krebserkrankungen in Deutschland. [Google Scholar]
- e4.Kamtsiuris P, Lange M, Hoffmann R, et al. [The first wave of the German Health Interview and Examination Survey for Adults (DEGS1): sample design, response, weighting and representativeness] Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2013;56:620–630. doi: 10.1007/s00103-012-1650-9. [DOI] [PubMed] [Google Scholar]
- e5.Manser R, Lethaby A, Irving LB, et al. Screening for lung cancer. Cochrane Database Syst Rev. 2013;6 doi: 10.1002/14651858.CD001991.pub3. CD001991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e6.Jaklitsch MT, Jacobson FL, Austin JH, et al. The American Association for Thoracic Surgery guidelines for lung cancer screening using low-dose computed tomography scans for lung cancer survivors and other high-risk groups. J Thorac Cardiovasc Surg. 2012;144:33–38. doi: 10.1016/j.jtcvs.2012.05.060. [DOI] [PubMed] [Google Scholar]
- e7.Couraud S, Cortot AB, Greillier L, et al. From randomized trials to the clinic: is it time to implement individual lung-cancer screening in clinical practice? A multidisciplinary statement from French experts on behalf of the French intergroup (IFCT) and the groupe d’Oncologie de langue francaise (GOLF) Ann Oncol. 2013;24:586–597. doi: 10.1093/annonc/mds476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e8.Prosch H, Studnicka M, Eisenhuber E, et al. [Opinion of the Austrian Society of Radiology and the Austrian Society of Pneumology] Wien Klin Wochenschr. 2013;125:339–345. doi: 10.1007/s00508-013-0356-9. [DOI] [PubMed] [Google Scholar]
- e9.Wender R, Fontham ET, Barrera E, Jr., et al. American Cancer Society lung cancer screening guidelines. CA Cancer J Clin. 2013;63:107–117. doi: 10.3322/caac.21172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e10.Field JK, Aberle DR, Altorki N, et al. The International Association Study Lung Cancer (IASLC) Strategic Screening Advisory Committee (SSAC) response to the USPSTF recommendations. J Thorac Oncol. 2014;9:141–143. doi: 10.1097/JTO.0000000000000060. [DOI] [PubMed] [Google Scholar]
- e11.Frauenfelder T, Puhan MA, Lazor R, et al. Early detection of lung cancer: a statement from an expert panel of the Swiss university hospitals on lung cancer screening. Respiration. 2014;87:254–264. doi: 10.1159/000357049. [DOI] [PubMed] [Google Scholar]
- e12.Gould MK. Clinical practice. Lung-cancer screening with low-dose computed tomography. N Engl J Med. 2014;371:1813–1820. doi: 10.1056/NEJMcp1404071. [DOI] [PubMed] [Google Scholar]
- e13.Herth FJ, Hoffmann H, Heussel CP, Biederer J, Groschel A. [Lung cancer screening-update 2014] Pneumologie. 2014;68:781–783. doi: 10.1055/s-0034-1390899. [DOI] [PubMed] [Google Scholar]
- e14.Blackmon SH, Feinglass SR. The United States preventive services task force recommendations for lung cancer screening. Thorac Surg Clin. 2015;25:199–203. doi: 10.1016/j.thorsurg.2014.12.004. [DOI] [PubMed] [Google Scholar]
- e15.Kauczor HU, Bonomo L, Gaga M, et al. ESR/ERS white paper on lung cancer screening. Eur Respir J. 2015;46:28–39. doi: 10.1183/09031936.00033015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e16.Kazerooni EA, Armstrong MR, Amorosa JK, et al. ACR CT accreditation program and the lung cancer screening program designation. J Am Coll Radiol. 2015;12:38–42. doi: 10.1016/j.jacr.2014.10.002. [DOI] [PubMed] [Google Scholar]
- e17.Mazzone P, Powell CA, Arenberg D, et al. Components necessary for high-quality lung cancer screening: American College of Chest Physicians and American Thoracic Society Policy Statement. Chest. 2015;147:295–303. doi: 10.1378/chest.14-2500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e18.Wood DE, Kazerooni E, Baum SL, et al. Lung cancer screening, version 12. 015: featured updates to the NCCN guidelines. J Natl Compr Canc Netw. 2015;13:23–34. doi: 10.6004/jnccn.2015.0006. [DOI] [PubMed] [Google Scholar]