Abstract
AKI requiring RRT is associated with high mortality, morbidity, and long-term consequences, including CKD and ESRD. Many patients never recover kidney function; in others, kidney function improves over a period of many weeks or months. Methodologic constraints of the available literature limit our understanding of the recovery process and hamper adequate intervention. Current management strategies have focused on acute care and short-term mortality, but new data indicate that long-term consequences of AKI requiring RRT are substantial. Promotion of kidney function recovery is a neglected focus of research and intervention. This lack of emphasis on recovery is illustrated by the relative paucity of research in this area and by the lack of demonstrated effective management strategies. In this article the epidemiologic implications of kidney recovery after AKI requiring RRT are discussed, the available literature and its methodologic constraints are reviewed, and strategies to improve the understanding of factors that affect kidney function recovery are proposed. Measures to promote kidney function recovery are a serious unmet need, with a great potential to improve short- and long-term patient outcomes.
Keywords: AKI, kidney function recovery, survival, RRT, progression of renal failure
Introduction
AKI requiring RRT (commonly designated AKI-D) is a common and serious condition with substantial morbidity, mortality, and associated CKD (1,2). The incidence of AKI-D in the United States is increasing; between 2000 and 2009, the number of new patients of AKI-D rose by 10% per year (3). Overall, AKI-D occurs in approximately 1%–2% of hospitalized patients and in 6%–7% of critically ill patients (4).
The mortality associated with AKI-D is high and is greater than other serious illnesses such as acute respiratory distress syndrome (5) or myocardial infarction (MI) (6). Overall in-hospital mortality of patients with AKI-D is 33% (7) and between 50% and 60% in the intensive care unit (ICU) (8, 9). Survivors of AKI-D are at risk for long-term complications, including CKD (10–13), ESRD (2,14), bone fractures (15), upper gastrointestinal bleeding (16), stroke (17), and cardiovascular events, including MI and congestive heart failure (6,12). Because observational studies suggest that adverse outcomes are mitigated when the severity and duration of AKI is reduced (18,19), it is hypothesized that targeted measures to facilitate kidney function recovery might improve both kidney- and nonkidney-related outcomes. However, despite these potential benefits, clinical management guidelines focusing on kidney function recovery are scarce, and therapies to accelerate kidney function recovery are practically nonexistent. Investigation to identify effective management strategies and therapies that accelerate kidney function recovery in AKI is sorely needed.
In this review, we discuss the magnitude of the problem of kidney function recovery in patients with AKI-D (Figure 1); the known clinical factors and potential management strategies that may facilitate recovery; the priority areas of research on AKI-D management; and the effect of kidney function recovery on patient survival, quality of life, and cost. We submit that efforts to improve kidney function recovery in patients with AKI-D are a serious unmet need, with great potential to benefit patients.
Figure 1.
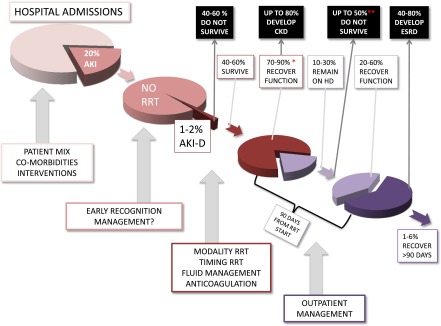
On average, 20% of hospitalized patients develop AKI; of those, 1%–2% develop AKI requiring RRT. Among patients with AKI-D, 40%–60% die and 40%–50% survive. *Depending on the degree of preexisting CKD, 70%–90% of the survivors recover function, whereas 10%–30% remain on dialysis at hospital discharge. Importantly, up to 80% of those who recover may develop CKD in the future. **Because of cardiovascular disease, up to 50% of those patients never reach ESRD. During the next 90 days, 20%–60% of those patients potentially recover while on outpatient dialysis, and 40%–80% are called ESRD at 90 days. Recent evidence suggests that with appropriate care, up to 75% may experience recovery. Of the remaining patients with ESRD, 1%–6% may still experience recovery after 90 days, as late as up to 1 year after discharge. The fraction of patients who develop AKI depends on multiple factors, including patient mix, comorbidities, and interventions during the hospitalization (cardiovascular procedures, sepsis), but the reasons for the overall increasing incidence of AKI are not completely understood. During the acute phase of AKI, early recognition and intervention may decrease severity. For those who develop AKI-D, some observational evidence suggests that RRT modality, timing, and fluid management may influence recovery. Those who are discharged on RRT will likely benefit from especial care designed to promote recovery. Even among those called ESRD at >90 days, 1%–6% may still recover function as late as 1 year after starting HD. AKI-D, AKI requiring RRT; HD, hemodialysis.
Patients with AKI-D are particularly vulnerable to a lack of adequate outpatient dialysis options and an absence of well-defined clinical management strategies. Our accompanying article (20) discusses the policy implications of this problem and suggests practical management strategies for these patients.
Kidney Function Recovery and Long-Term Outcomes of Patients with AKI-D
Kidney function recovery of AKI-D has been best studied in the context of the short-term ICU stay. Dialysis independence at the time of hospital discharge is the most commonly reported outcome. Studies suggest that 10%–30% of survivors with AKI-D remain dialysis dependent at the time of hospital discharge (8,21–27). The largest epidemiologic study regarding outcomes of patients with AKI-D is the Beginning and Ending Supportive Therapy for the Kidney cohort (N=1006) (8). In this study, reporting the outcomes of critically ill patients treated with AKI requiring continuous RRT (CRRT) in 54 ICUs in 23 countries, 15% of survivors were dialysis dependent at hospital discharge. Continued dialysis dependence after hospital discharge and up to 90 days is variably reported, ranging from 16% to 29% (27,28). By arbitrary convention, 90 days is an important time point because it is the defined time when many patients are considered to have reached ESRD.
Studies specifically examining the outcomes of outpatients who still require dialysis at hospital discharge are lacking. Better epidemiologic data are essential to inform patients and providers regarding the potential for kidney function recovery and to help determine when kidney function loss might reasonably be considered irreversible.
Baseline kidney function is the most consistently identified factor affecting kidney function recovery in patients with AKI-D (27,29–32). Other factors shown to adversely affect kidney function recovery include increasing age, diabetes mellitus, heart failure, and increased number of comorbidities (27,33,34).
To our knowledge, only one study has specifically examined the outcome of hospitalized patients with AKI-D who were transferred to an outpatient dialysis facility (34). At 6 months, the cumulative recovery rate was 21%. Within 6 months, whereas 50% of patients with AKI-D with baseline eGFR>60 ml/min per 1.73 m2 recovered, only 17% of AKI-on-CKD 3–4 patients (baseline eGFR 15–60 ml/min per 1.73 m2) and zero CKD 5 patients (baseline eGFR<15 ml/min per 1.73 m2) recovered function. In multivariable analysis, higher baseline eGFR, acute tubular necrosis (ATN) from sepsis or surgery, and absence of heart failure were independent predictors of survival. Among those who recovered, 73% of the recovery occurred within the first 3 months of dialysis initiation; thereafter, 21% recovered between 3 and 6 months and only 6% beyond 6 months.
The design and performance of quality epidemiologic studies of patients with AKI-D are challenging. Studies assessing kidney function outcomes must address two key factors: (1) the effect of hospital survival on the interpretation of kidney function recovery, and (2) the definition of kidney function recovery.
Hospital Survival of Patients with AKI-D
Because the mortality rate of patients with AKI-D is high, reporting outcomes only among survivors can be misleading. Patients discharged after an episode of AKI have a 40% risk of dying in the 2 years after the initial hospitalization (35). As shown in Table 1, in-hospital mortality rates are 45%–79%, and dialysis dependence at hospital discharge occurs in 5%–13% when all patients (survivors and nonsurvivors) are considered. Therefore, comparing outcomes of epidemiologic studies and clinical trials of AKI-D requires that kidney function outcomes be considered for all patients (survivors and nonsurvivors). Studies with apparent benefit on function recovery may be less convincing when the entire cohort of patients with AKI-D is considered.
Table 1.
Mortality, survival, and dialysis dependence at hospital discharge among patients with AKI requiring RRT in selected studies
| References | Total No. of Patients | ICU Versus Non-ICU Patients | Cause of AKI | Prevalence of CKD (%) | No. of Patients Who Died in the Hospital (% In-hospital Mortality) | No. of Patients Who Survived to Hospital Discharge | No. of Dialysis-Dependent Patients at Hospital Discharge (% Survivors, % Total) | No. of Patients Alive and Dialysis Independent at Hospital Discharge, n (% Total) |
|---|---|---|---|---|---|---|---|---|
| Chertow, 1995 (21) | 132 | 100% ICU | Critical disease, MOF | N/A | 92 (70) | 40 (30) | 13 (33, 10) | 27 (20) |
| Manns, 2003 (22) | 261 | 100% ICU all AKI-D | Critical disease, MOF | 50 | 163 (63) | 98 (38) | 28 (29, 11) | 70 (27) |
| Korkeila, 2000 (22) | 62 | 100% ICU all AKI-D | Critical disease, MOF | 8 | 28 (45) | 34 (55) | 6 (18, 10) | 28 (45) |
| Cole, 2000 (24) | 116 | 100% ICU | Critical disease, MOF | 36.7 | 57 (49) | 59 (51) | 11 (10, 9) | 48 (41) |
| Silvester, 2001 (25) | 299 | 100% ICU | Critical disease, MOF | 34.1 | 140 (47) | 159 (53) | 25 (16, 8) | 134 (45) |
| Cosentino, 1994 (26) | 363 | 100% ICU | Critical disease, MOF | N/A | 287 (79) | 76 (21) | 26 (34, 7) | 50 (14) |
| Uchino, 2007 (8) | 1006 | 100% ICU | Critical disease, MOF | 28.1 | 642 (64) | 364 (36) | 52 (15, 5) | 312 (31) |
| Bagshaw, 2005 (27) | 240 | 100% ICU | Critical disease, MOF | 18.8 | 143 (60) | 97 (40) | 31 (32, 13) | 66 (28) |
| Totals (mean±SD) | 2479 (309±299) | 100% | 100% Critical disease, MOF | (29.3±15) | (60±12) | (41±12) | (23±10, 9±3) | (31±12) |
ICU, intensive care unit; AKI-D, AKI requiring RRT; MOF, multiple organ failure; N/A, not applicable.
Definition of Kidney Function Recovery
Recovery has traditionally been defined by dialysis independence at hospital discharge. Recent clinical trials have also examined long-term outcomes at 60 and 90 days after initiation of dialysis (9,36). Indeed, alive and dialysis free at 90 days is likely to become a relevant clinical end point in future trials. Although dialysis independence is clearly important, merely assessing dialysis independence ignores the significant proportion of patients that may develop CKD. Defining kidney function recovery independent of dialysis status is not without challenges, however. Definitions that rely on a return to baseline kidney function are problematic because baseline kidney function is often unknown. Moreover, recent studies highlight the inadequacies of serum creatinine as a marker of GFR and recovery in the critically ill, whereby the use of eGFR and serum creatinine overestimated kidney function recovery compared with measured creatinine clearance (37,38). The discrepancy may be explained by the effect of muscle mass loss associated with prolonged critical illness (27,28,38). Efforts to standardize definitions of kidney function recovery in AKI-D are ongoing and are a key consideration in future clinical trial design.
Long-Term Outcomes of Patients with AKI-D Who Become Dialysis Independent within 90 Days
Although alive and dialysis free at 90 days is clearly an important milestone, AKI-D survivors remain at risk for serious complications within the next 1–5 years (6,12,15–17,32). The risk of ESRD after AKI-D after early dialysis independence is substantial, ranging from 8% to 21% of survivors (12,39). A large cohort of 4383 patients with AKI-D who were dialysis free for >90 days was analyzed for risk of subsequent ESRD (defined as dialysis requirement for at least 90 days). Of these, 8% (n=356) developed ESRD after a median follow-up of 2.4 years; of note, 34% (n=1475) of the cohort died during the follow-up period. Risk factors for return to dialysis included preexisting CKD, hypertension, and comorbidities (39). In another large matched cohort study, 4869 patients with AKI-D who were alive and dialysis free at 30 days had a 2.4 higher adjusted risk of developing ESRD at a mean follow-up of 3 years compared with 4869 matched controls (12). In a third study, the risk for ESRD in 3769 survivors of AKI-D who were dialysis free for at least 30 days was compared with the risk of ESRD in 13,598 well-matched hospital controls (40). Median follow-up was 3 years. ESRD occurred in 8.5% of AKI-D (n=322) and 3% of controls (n=403), with an adjusted hazard ratio (HR) of 3.23. Although it has been suggested that patients with AKI-D are more likely to develop ESRD if they have underlying CKD, in the same study (40), the adjusted risk for ESRD was highest (at 15.5) among patients with AKI-D without preexisting CKD.
The increased risk of ESRD after episodes of AKI-D is not surprising: many patients with AKI-D develop new CKD (10,13) or have worsening of preexisting CKD (10–13). Therefore, in a single-center study of patients with normal baseline kidney function (serum creatinine 1.3 mg/dl) after 54 months of follow-up, approximately 80% of AKI-D survivors developed CKD stage 3 or higher (10).
The long-term consequences of AKI-D extend beyond the risk of CKD and ESRD (41). Two large studies have examined survival, cardiovascular events, and stroke after AKI-D using data from the Taiwan National Healthcare System. In the first study, a total of 17,106 patients with AKI-D were identified; 4869 AKI-D survivors who were alive and dialysis free at 30 days were matched with 4869 controls (12). After a mean follow-up of 3 years, the risk of mortality and coronary events, including MI, were significantly greater in AKI-D. Mortality was 57.4% versus 34.6% in those with and without AKI-D (adjusted HR, 1.67), and 6.1% of AKI-D survivors experienced coronary events compared with 3.6% of controls (adjusted HR, 1.42). In the second study, 4315 AKI-D survivors who were alive and dialysis free at 30 days were matched with controls. After a mean follow-up of 3 years, patients with AKI-D had a higher risk of stroke (adjusted HR, 1.25) and a higher severity of stroke events (17). Remarkably, AKI-D conferred a future risk of coronary events (12) or stroke (17) that was similar to the risk conferred by diabetes.
AKI exposure portends severe kidney and cardiovascular outcomes. Patients who experience a simultaneous acute MI and AKI are twice as likely to experience subsequent admissions for congestive heart failure compared with patients with MI alone (6). The potentiation is bidirectional: AKI and MI increase the chances of subsequent kidney dysfunction and cardiovascular disease, and when AKI complicates and MI occurs, there is significantly increased risk of later development of cardio renal syndrome (42). Measured in terms of mortality and major adverse cardiovascular events, AKI exposure is potentially worse than an isolated ST-elevation acute MI (6).
In summary, data from large cohorts suggest that approximately one of every 12 survivors of AKI-D who become dialysis independent will require long-term dialysis within 3–5 years (39,40). Increased risk of ESRD occurs regardless of baseline CKD status. Nephrology care within 90 days of dialysis independence is associated with improved long-term survival (43). Although definitive evidence of benefit is still lacking, we recommend that nephrology follow-up occur within at least 90 days of dialysis discontinuation (ideally, within a month). We also suggest that, in this high-risk population, nephrology care be continued to mitigate progression to CKD or ESRD; to properly prepare for long-term dialysis if necessary; and to anticipate preventive care for other long-term complications, such as cardiovascular events, including heart failure and stroke (6).
Management Factors Affecting Kidney Function Recovery
Although RRT is the mainstay of supportive care in AKI-D, its application can have untoward effects and contribute to prolongation of kidney failure or impede recovery (44). No single management strategy has been proven to promote kidney function recovery in patients with AKI-D. Evidence-based clinical guidelines are currently lacking. The lack of quality data in this area is concerning, and research inquiry in this area is urgently needed.
In the absence of data, current management strategies focus on avoidance of additional kidney injury by maintaining kidney perfusion, avoiding hypotension, and avoiding nephrotoxins and technique-related infection (44). There is great interest to determine if modifications in RRT modality, fluid management, timing, RRT dose, anticoagulation strategies, and dialysis membranes effect recovery.
Renal Replacement Modality
By far, the RRT modality has received the most attention as a potential modifier of kidney function recovery. CRRT is considered by some to be superior to intermittent hemodialysis (IHD). It is hypothesized that hypotensive episodes during dialysis contribute to decreased kidney perfusion and compromise recovery. CRRT might be associated with better recovery because it affords better hemodynamic stability and less risk of intradialytic hypotension than IHD (45). Several animal models have demonstrated loss of renal blood flow autoregulation in AKI (46–48) that exposes the kidneys to additional injury, and the hemodynamic changes induced by IHD (9,49,50) are clinically important (51–59) and could adversely affect recovery.
However, available data are inadequate to definitively recommend one modality over another. Studies suggest that patients treated with CRRT versus IHD may experience better kidney function recovery (22,44,60–65). In a recent cohort study (66) of critically ill patients, 2004 patients treated with CRRT were matched with 2004 patients treated with IHD. At 3 years, the risk of chronic dialysis (dialysis >90 days) was significantly lower among patients initially treated with CRRT. A recent systematic review (45) analyzed several modality trials. The pooled analysis of observational studies indicated that among survivors of AKI-D, initial treatment with IHD was associated with a higher rate of dialysis dependence. However, the pooled analysis of the randomized controlled trials showed no difference in the rate of dialysis dependence between the two modalities among survivors. The large imbalances in underlying risk and competing risk for mortality in observational trials make it impossible to conclude at this time whether any modality is able to provide a better kidney functional outcome (67,68). Clinical trials are needed to demonstrate clear benefit.
Fluid Overload
Initiation of dialysis to avoid fluid overload might have a beneficial effect on recovery. In a single-center, retrospective cohort study (69), initiation of dialysis before the development of fluid overload was associated with improved recovery (fluid overload defined as ≥10% increase in baseline weight; recovery defined as dialysis independence at 1 year). In another study, dialysis initiation at >20% fluid overload was associated with prolonged time to kidney function recovery (70). Fluid overload might delay recovery because of (1) increased kidney edema and altered kidney architecture, (2) reduced kidney perfusion from increased intra-abdominal pressure, and (3) more aggressive fluid removal at dialysis initiation resulting in more intradialytic hypotension (69). Fluid overload at dialysis initiation is also associated with increased mortality (71–74). These studies are all observational and potentially affected by confounding; a causal link has not been established. Prospective interventional studies are needed to determine if fluid overload is merely a marker of severity of illness causing poor outcomes or whether preventing fluid overload (e.g., by early dialysis initiation) might improve outcomes.
Dialysis Timing
The optimal timing and indication of dialysis that confers kidney function benefit are unknown. Two systematic reviews on timing of dialysis initiation noted nonsignificant trends toward lower dialysis dependence with earlier initiation of dialysis (75,76). However, these systematic reviews pooled studies that defined timing of initiation on the basis of variable criteria, including levels of BUN and creatinine and duration of ICU stay; therefore, the results should be interpreted with caution.
Dialysis Dose
Increasing the dose of dialysis does not seem to affect kidney function recovery (77). In the ATN (78) and Intensity of continuous Renal Replacement Therapy in Critically Ill Patients (36) trials, there was no correlation between the intensity of dialysis and kidney function recovery. Furthermore, a meta-analysis on the effects of intensity of dialysis in eight trials including 3841 patients demonstrated no benefit of increased dialysis dose on kidney function recovery (79).
Dialysis Membrane
Aside from solute clearance, the interactions between blood and the dialysis membrane have been referred to as biocompatibility. A number of experimental studies in animal models suggested that complement and granulocyte activation during IHD could contribute to prolongation of AKI. Subsequent human prospective randomized trials in the 1990s suggested faster kidney function recovery and lower morbidity and mortality using biocompatible membranes (80–83), but more recent systematic reviews (44,84) showed no clinical benefit of biocompatible compared with less biocompatible membranes on kidney function recovery in patients with AKI-D receiving IHD. No published studies on the effects of membrane characteristics on recovery have been performed in patients receiving CRRT.
Anticoagulation
Although most of the studies on citrate anticoagulation are too small to evaluate patient outcome (85), the largest single-center trial (86) showed an increase in 3-month patient survival and a trend toward better kidney recovery, a benefit not explained by lesser bleeding. Anti-inflammatory effects of citrate may play a role in these preliminary results (87). These findings will require confirmation in larger multicenter trials.
Kidney Function and Long-Term Outcomes of Patients with AKI-D Who Remain Dialysis Dependent beyond 90 Days
Data suggest that dialysis dependence beyond 90 days is not uncommon in AKI-D: those patients are generally considered to have ESRD. In a cohort of 240 ICU patients with AKI-D, 22% of survivors (n=19) were RRT-dependent at 1 year; notably, at 1 year, only 28% of the cohort (n=68) were alive and free of dialysis (27). In another report of 1095 patients with AKI-D and normal baseline kidney function followed for 5 years, at 90 days 60% of patients survived and 17% of survivors (n=107) still required dialysis and were considered ESRD. Of these, only six patients were eventually able to discontinue dialysis. Overall, the 5-year survival was significantly worse for patients with ESRD from AKI (41%) versus patients with nondiabetic kidney diseases as the cause of ESRD (61%); the cause of death was related to the cause of AKI in most patients (28).
In patients with AKI-D who are considered to have ESRD, kidney function recovery has been reported to occur in approximately 1%–2% of patients (88). Recently, however, among the 194,007 patients in the Medicare ESRD program identified via submission of Centers for Medicare and Medicare Services 2728 forms between 2008 and 2009 (89), function recovery (defined as dialysis independence >1 year) occurred in 5.6% and 5.9% of patients in 2008 and 2009, respectively. Among these patients ATN alone accounted for 19.9% of all patients of renal recovery and 22% of those with sustained recovery. Among patients who were able to discontinue dialysis, most did so within the first 3 months: 69% for the entire cohort, and 81% for patients with a diagnosis of ATN. Although AKI (acute interstitial nephritis and ATN in particular) was the most common diagnosis associated with dialysis independence, dialysis independence was still higher than previous reports when diagnoses associated with AKI were excluded (i.e., 4.2% for 2008, 4.4% for 2009). Renal recovery was most likely to occur in the first month after incident hemodialysis; more than half of the patients of recovery occurred within the first 2 months, and more than two thirds occurred in the first 3 months of ESRD registration. Rate of recovery was fastest for patients with ATN as the primary cause of failure (89).
Because patients with AKI as the cause of ESRD have the highest rate of recovery of all patients with ESRD, we recommend that these patients be systematically monitored for kidney recovery during the first year of dialysis therapy. Indeed, methods to assess function recovery could reasonably be put in place for all patients initiating dialysis, as has been suggested by others (88), because approximately one in 20 of all patients with ESRD (AKI or non-AKI related) will achieve dialysis independence during the first year of dialysis initiation. Because most patients with ESRD who recover kidney function do so within the first 3 months of dialysis initiation, attention to recovery is especially important during this time period.
The most appropriate method to monitor kidney function recovery in the outpatient dialysis setting is still uncertain. Studies suggest that in hospitalized patients, increased urine output is the most reliable early indicator of recovery (90). Falling serum creatinine is another well-recognized indicator of recovery; however, declining serum creatinine values might reflect catabolism, declining muscle mass, and malnutrition. Normalization of serum electrolytes, such as potassium and phosphorus, may also occur. In the ATN trial (9), dialysis was discontinued when the 6-hour creatinine clearance was >20 ml/min, but the most appropriate threshold for discontinuation is still uncertain (88). In the outpatient setting, a 24-hour urine collection for urea and creatinine is commonly used to calculate residual GFR. This method has been examined in intermittent hemodialysis patients and shown to be as accurate as inulin clearance (91). Unfortunately, symptoms and signs of recovery are nonspecific (Table 2), but they should still be assessed and considered for their potential value as early indicators. Those symptoms of recovery may also be conflicting; although some patients may develop an improved sense of well-being, other patients may begin to feel worse because of unnecessary fluid removal after gaining true body weight (88).
Table 2.
Potential indicators of kidney function recovery in patients with AKI requiring dialysis
| Indicators |
|---|
| Spontaneous decline in serum creatinine |
| Increase in urine output |
| Decrease in interdialytic weight gain |
| Increase in calculated GFR (using urea and creatinine clearance derived form a timed urine collection) |
There are no guidelines on the proper methods to taper or discontinue dialysis in patients with AKI-D. Tapering of the dialysis by reducing time and frequency (88) or temporary discontinuation of dialysis with close monitoring may be appropriate. Whether dialysis is weaned or a trial of discontinuation is attempted, careful attention to medication dosing is warranted: some medications will need a higher dose (to account for recovering kidney function), but some will need a dose decrease (to account for the lack of dialysis removal). Phosphorus binders may also need adjustment to avoid hypophosphatemia in the face of recovering kidney function.
In addition to monitoring recovery, we propose measures to promote recovery, especially during the first 3 months postdialysis initiation. Specifically, intradialytic hypotension should be avoided, and for patients without symptomatic fluid overload, it may be advisable to delay establishing a dry weight until the patient has been deemed to have irreversible ESRD. Predialysis and home BP measurements must be carefully monitored, and BP medications must be carefully titrated to avoid hypotension. Readers are referred to extensive recent reviews on the subject of intradialytic hypotension and its management (92–96). Nephrotoxic medications and intravenous radiocontrast media should be avoided if possible.
Because most patients with ESRD will not recover function, we suggest that other management aspects of ESRD care be used as usual, regarding bone mineral management, anemia management, and permanent hemo- or peritoneal dialysis access creation. Patients with nonrecovering AKI must be offered the opportunity to explore all dialytic options as afforded to patients with progressive CKD. Although observational studies have suggested better preservation of residual function with peritoneal dialysis, other studies have failed to demonstrate a relationship (97) or are affected by confounding (88), and prospective randomized trials are not available.
For patients with AKI-D, the benefits of recognition and promotion of recovery in the outpatient setting cannot be overstated. Achievement of dialysis independence has substantial benefit in terms of improved quality of life and reduced morbidity. Measures to improve recovery will also reduce incident ESRD and its multiple, severe, long-term complications. Moreover, minimizing incident ESRD will have a substantial cost benefit, given the heavy health care expenditures associated with long-term care of patients with ESRD and their related complications.
Development of new measures able to predict recovery in patients with AKI-D would be greatly beneficial. Clinical prediction markers (e.g., baseline CKD, chronic heart failure, age, AKI phenotype) or novel biomarkers (68,98–102) may soon help identify individuals likely to recover and enable appropriate clinical trial enrollment and intensive monitoring of recovery.
Conclusions
AKI-D has traditionally been considered a problem of acute care management focused on hospital survival, but minimal attention has been paid to measures to promote kidney function recovery. We suggest that measures to recognize and promote recovery will potentially benefit both the increasingly incident patients with AKI-D and the overall health care system. Further, we suggest that the strategies with the most potential effect include the following: (1) implementation of improvements in the transition-of-care process after hospital discharge (as discussed in the accompanying Heung et al. [20]); (2) research in nondialytic interventions that promote recovery; (3) research in RRT innovations that promote recovery and avoid further kidney damage; (4) systematic monitoring of recovery in the outpatient setting for patients with persistent AKI-, and for patients declared ESRD after AKI; and (5) research to identify clinical and biomarker predictors of recovery. Such measures will have significant benefits by reducing the very high morbidity and mortality currently associated with ESRD and providing a meaningful improvement in overall quality of life to patients with severe AKI.
Disclosures
None.
Acknowledgments
The members of the Acute Kidney Injury Advisory Board are as follows: Sarah Faubel (Chair), David J. Askenazi (2016), Azra Bihorac, FASN (2017), Jorge Cerdá FASN (2017), Lakhmir S. Chawla (2015), Alan J. Davidson (2016), Mark P. De Caestecker, MBBS (2017), William Henry Fissell (2016), Michael Heung (2017), Benjamin D. Humphreys, FASN (2017), Jay L. Koyner (2015), Kathleen D. Liu (2016), Girish K. Mour (2017), Thomas D. Nolin, FASN (2015), Anitha Vijayan, FASN (2017), Council Liaison Mark D. Okusa, FASN, and Staff Liaison Mark Lukaszewski.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.Cerdá J, Lameire N, Eggers P, Pannu N, Uchino S, Wang H, Bagga A, Levin A: Epidemiology of acute kidney injury. Clin J Am Soc Nephrol 3: 881–886, 2008 [DOI] [PubMed] [Google Scholar]
- 2.Chawla LS: Acute kidney injury leading to chronic kidney disease and long-term outcomes of acute kidney injury: The best opportunity to mitigate acute kidney injury? Contrib Nephrol 174: 182–190, 2011 [DOI] [PubMed] [Google Scholar]
- 3.Hsu RK, McCulloch CE, Dudley RA, Lo LJ, Hsu CY: Temporal changes in incidence of dialysis-requiring AKI. J Am Soc Nephrol 24: 37–42, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Prescott GJ, Metcalfe W, Baharani J, Khan IH, Simpson K, Smith WC, MacLeod AM: A prospective national study of acute renal failure treated with RRT: Incidence, aetiology and outcomes. Nephrol Dial Transplant 22: 2513–2519, 2007 [DOI] [PubMed] [Google Scholar]
- 5.The Acute Respiratory Distress Syndrome Network: Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 342: 1301–1308, 2000 [DOI] [PubMed] [Google Scholar]
- 6.Chawla LS, Amdur RL, Shaw AD, Faselis C, Palant CE, Kimmel PL: Association between AKI and long-term renal and cardiovascular outcomes in United States veterans. Clin J Am Soc Nephrol 9: 448–456, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xue JL, Daniels F, Star RA, Kimmel PL, Eggers PW, Molitoris BA, Himmelfarb J, Collins AJ: Incidence and mortality of acute renal failure in Medicare beneficiaries, 1992 to 2001. J Am Soc Nephrol 17: 1135–1142, 2006 [DOI] [PubMed] [Google Scholar]
- 8.Uchino S, Bellomo R, Morimatsu H, Morgera S, Schetz M, Tan I, Bouman C, Macedo E, Gibney N, Tolwani A, Oudemans-van Straaten H, Ronco C, Kellum JA: Continuous renal replacement therapy: A worldwide practice survey. The beginning and ending supportive therapy for the kidney (B.E.S.T. kidney) investigators. Intensive Care Med 33: 1563–1570, 2007 [DOI] [PubMed] [Google Scholar]
- 9.Palevsky PM, Zhang JH, O’Connor TZ, Chertow GM, Crowley ST, Choudhury D, Finkel K, Kellum JA, Paganini E, Schein RM, Smith MW, Swanson KM, Thompson BT, Vijayan A, Watnick S, Star RA, Peduzzi P; VA/NIH Acute Renal Failure Trial Network: Intensity of renal support in critically ill patients with acute kidney injury. N Engl J Med 359: 7–20, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Duran PA, Concepcion LA: Survival after acute kidney injury requiring dialysis: Long-term follow up. Hemodial Int 18[Suppl 1]: S1–S6, 2014 [DOI] [PubMed] [Google Scholar]
- 11.Lo LJ, Go AS, Chertow GM, McCulloch CE, Fan D, Ordoñez JD, Hsu CY: Dialysis-requiring acute renal failure increases the risk of progressive chronic kidney disease. Kidney Int 76: 893–899, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wu VC, Wu CH, Huang TM, Wang CY, Lai CF, Shiao CC, Chang CH, Lin SL, Chen YY, Chen YM, Chu TS, Chiang WC, Wu KD, Tsai PR, Chen L, Ko WJ; NSARF Group: Long-term risk of coronary events after AKI. J Am Soc Nephrol 25: 595–605, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schiffl H, Fischer R: Five-year outcomes of severe acute kidney injury requiring renal replacement therapy. Nephrol Dial Transplant 23: 2235–2241, 2008 [DOI] [PubMed] [Google Scholar]
- 14.Goldstein SL, Jaber BL, Faubel S, Chawla LS; Acute Kidney Injury Advisory Group of American Society of Nephrology: AKI transition of care: A potential opportunity to detect and prevent CKD. Clin J Am Soc Nephrol 8: 476–483, 2013 [DOI] [PubMed] [Google Scholar]
- 15.Wang WJ, Chao CT, Huang YC, Wang CY, Chang CH, Huang TM, Lai CF, Huang HY, Shiao CC, Chu TS, Chen YM, Wu VC, Ko WJ, Wu KD; National Taiwan University Study Group on Acute Renal Failure: The impact of acute kidney injury with temporary dialysis on the risk of fracture. J Bone Miner Res 29: 676–684, 2014 [DOI] [PubMed] [Google Scholar]
- 16.Wu PC, Wu CJ, Lin CJ, Wu VC; National Taiwan University Study Group on Acute Renal Failure Group: Long-term risk of upper gastrointestinal hemorrhage after advanced AKI. Clin J Am Soc Nephrol 10: 353–362, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu VC, Wu PC, Wu CH, Huang TM, Chang CH, Tsai PR, Ko WJ, Chen L, Wang CY, Chu TS, Wu KD; National Taiwan University Study Group on Acute Renal Failure (NSARF) Group: The impact of acute kidney injury on the long-term risk of stroke. J Am Heart Assoc 3: 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Coca SG, King JT, Jr, Rosenthal RA, Perkal MF, Parikh CR: The duration of postoperative acute kidney injury is an additional parameter predicting long-term survival in diabetic veterans. Kidney Int 78: 926–933, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Coca SG, Yusuf B, Shlipak MG, Garg AX, Parikh CR: Long-term risk of mortality and other adverse outcomes after acute kidney injury: A systematic review and meta-analysis. Am J Kidney Dis 53: 961–973, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Heung, et al. reference CJASN 02290215 when published, XXX [Google Scholar]
- 21.Chertow GM, Christiansen CL, Cleary PD, Munro C, Lazarus JM: Prognostic stratification in critically ill patients with acute renal failure requiring dialysis. Arch Intern Med 155: 1505–1511, 1995 [PubMed] [Google Scholar]
- 22.Manns B, Doig CJ, Lee H, Dean S, Tonelli M, Johnson D, Donaldson C: Cost of acute renal failure requiring dialysis in the intensive care unit: Clinical and resource implications of renal recovery. Crit Care Med 31: 449–455, 2003 [DOI] [PubMed] [Google Scholar]
- 23.Korkeila M, Ruokonen E, Takala J: Costs of care, long-term prognosis and quality of life in patients requiring renal replacement therapy during intensive care. Intensive Care Med 26: 1824–1831, 2000 [DOI] [PubMed] [Google Scholar]
- 24.Cole L, Bellomo R, Silvester W, Reeves JH: A prospective, multicenter study of the epidemiology, management, and outcome of severe acute renal failure in a “closed” ICU system. Am J Respir Crit Care Med 162: 191–196, 2000 [DOI] [PubMed] [Google Scholar]
- 25.Silvester W: Outcome studies of continuous renal replacement therapy in the intensive care unit. Kidney Int Suppl 66: S138–S141, 1998 [PubMed] [Google Scholar]
- 26.Cosentino F, Chaff C, Piedmonte M: Risk factors influencing survival in ICU acute renal failure. Nephrol Dial Transplant 9[Suppl 4]: 179–182, 1994 [PubMed] [Google Scholar]
- 27.Bagshaw SM, Laupland KB, Doig CJ, Mortis G, Fick GH, Mucenski M, Godinez-Luna T, Svenson LW, Rosenal T: Prognosis for long-term survival and renal recovery in critically ill patients with severe acute renal failure: A population-based study. Crit Care 9: R700–R709, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bhandari S, Turney JH: Survivors of acute renal failure who do not recover renal function. QJM 89: 415–421, 1996 [DOI] [PubMed] [Google Scholar]
- 29.Schiffl H: Renal recovery after severe acute renal injury. Eur J Med Res 13: 552–556, 2008 [PubMed] [Google Scholar]
- 30.Triverio PA, Martin PY, Romand J, Pugin J, Perneger T, Saudan P: Long-term prognosis after acute kidney injury requiring renal replacement therapy. Nephrol Dial Transplant 24: 2186–2189, 2009 [DOI] [PubMed] [Google Scholar]
- 31.Lins RL, Elseviers MM, Daelemans R: Severity scoring and mortality 1 year after acute renal failure. Nephrol Dial Transplant 21: 1066–1068, 2006 [DOI] [PubMed] [Google Scholar]
- 32.Amdur RL, Chawla LS, Amodeo S, Kimmel PL, Palant CE: Outcomes following diagnosis of acute renal failure in U.S. veterans: Focus on acute tubular necrosis. Kidney Int 76: 1089–1097, 2009 [DOI] [PubMed] [Google Scholar]
- 33.Craven AM, Hawley CM, McDonald SP, Rosman JB, Brown FG, Johnson DW: Predictors of renal recovery in Australian and New Zealand end-stage renal failure patients treated with peritoneal dialysis. Perit Dial Int 27: 184–191, 2007 [PubMed] [Google Scholar]
- 34.Hickson LJ, Chaudhary S, Williams AW, Dillon JJ, Norby SM, Gregoire JR, Albright RC, Jr, McCarthy JT, Thorsteinsdottir B, Rule AD: Predictors of outpatient kidney function recovery among patients who initiate hemodialysis in the hospital. Am J Kidney Dis 65: 592–602, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lafrance JP, Miller DR: Acute kidney injury associates with increased long-term mortality. J Am Soc Nephrol 21: 345–352, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bellomo R, Cass A, Cole L, Finfer S, Gallagher M, Lo S, McArthur C, McGuinness S, Myburgh J, Norton R, Scheinkestel C, Su S; RENAL Replacement Therapy Study Investigators: Intensity of continuous renal-replacement therapy in critically ill patients. N Engl J Med 361: 1627–1638, 2009 [DOI] [PubMed] [Google Scholar]
- 37.Schetz M, Gunst J, Van den Berghe G: The impact of using estimated GFR versus creatinine clearance on the evaluation of recovery from acute kidney injury in the ICU. Intensive Care Med 40: 1709–1717, 2014 [DOI] [PubMed] [Google Scholar]
- 38.Prowle JR, Kolic I, Purdell-Lewis J, Taylor R, Pearse RM, Kirwan CJ: Serum creatinine changes associated with critical illness and detection of persistent renal dysfunction after AKI. Clin J Am Soc Nephrol 9: 1015–1023, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Harel Z, Bell CM, Dixon SN, McArthur E, James MT, Garg AX, Harel S, Silver S, Wald R: Predictors of progression to chronic dialysis in survivors of severe acute kidney injury: A competing risk study. BMC Nephrol 15: 114, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wald R, Quinn RR, Luo J, Li P, Scales DC, Mamdani MM, Ray JG; University of Toronto Acute Kidney Injury Research Group: Chronic dialysis and death among survivors of acute kidney injury requiring dialysis. JAMA 302: 1179–1185, 2009 [DOI] [PubMed] [Google Scholar]
- 41.Hsu CY, Liu KD: Cardiovascular events after AKI: A new dimension. J Am Soc Nephrol 25: 425–427, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cruz DN, Gheorghiade M, Palazzuoli A, Ronco C, Bagshaw SM: Epidemiology and outcome of the cardio-renal syndrome. Heart Fail Rev 16: 531–542, 2011 [DOI] [PubMed] [Google Scholar]
- 43.Harel Z, Wald R, Bargman JM, Mamdani M, Etchells E, Garg AX, Ray JG, Luo J, Li P, Quinn RR, Forster A, Perl J, Bell CM: Nephrologist follow-up improves all-cause mortality of severe acute kidney injury survivors. Kidney Int 83: 901–908, 2013 [DOI] [PubMed] [Google Scholar]
- 44.Palevsky PM, Baldwin I, Davenport A, Goldstein S, Paganini E: Renal replacement therapy and the kidney: Minimizing the impact of renal replacement therapy on recovery of acute renal failure. Curr Opin Crit Care 11: 548–554, 2005 [DOI] [PubMed] [Google Scholar]
- 45.Schneider AG, Bellomo R, Bagshaw SM, Glassford NJ, Lo S, Jun M, Cass A, Gallagher M: Choice of renal replacement therapy modality and dialysis dependence after acute kidney injury: A systematic review and meta-analysis. Intensive Care Med 39: 987–997, 2013 [DOI] [PubMed] [Google Scholar]
- 46.Matthys E, Patton MK, Osgood RW, Venkatachalam MA, Stein JH: Alterations in vascular function and morphology in acute ischemic renal failure. Kidney Int 23: 717–724, 1983 [DOI] [PubMed] [Google Scholar]
- 47.Kelleher SP, Robinette JB, Miller F, Conger JD: Effect of hemorrhagic reduction in blood pressure on recovery from acute renal failure. Kidney Int 31: 725–730, 1987 [DOI] [PubMed] [Google Scholar]
- 48.Adams PL, Adams FF, Bell PD, Navar LG: Impaired renal blood flow autoregulation in ischemic acute renal failure. Kidney Int 18: 68–76, 1980 [DOI] [PubMed] [Google Scholar]
- 49.Davenport A: Intradialytic complications during hemodialysis. Hemodial Int 10: 162–167, 2006 [DOI] [PubMed] [Google Scholar]
- 50.Manns M, Sigler MH, Teehan BP: Intradialytic renal haemodynamics--potential consequences for the management of the patient with acute renal failure. Nephrol Dial Transplant 12: 870–872, 1997 [DOI] [PubMed] [Google Scholar]
- 51.Bagshaw SM, Berthiaume LR, Delaney A, Bellomo R: Continuous versus intermittent renal replacement therapy for critically ill patients with acute kidney injury: A meta-analysis. Crit Care Med 36: 610–617, 2008 [DOI] [PubMed] [Google Scholar]
- 52.Burton JO, Jefferies HJ, Selby NM, McIntyre CW: Hemodialysis-induced repetitive myocardial injury results in global and segmental reduction in systolic cardiac function. Clin J Am Soc Nephrol 4: 1925–1931, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lameire N, Van Biesen W, Vanholder R, Colardijn F: The place of intermittent hemodialysis in the treatment of acute renal failure in the ICU patient. Kidney Int Suppl 66: S110–S119, 1998 [PubMed] [Google Scholar]
- 54.Selby NM, Lambie SH, Camici PG, Baker CS, McIntyre CW: Occurrence of regional left ventricular dysfunction in patients undergoing standard and biofeedback dialysis. Am J Kidney Dis 47: 830–841, 2006 [DOI] [PubMed] [Google Scholar]
- 55.Van der Schueren G, Diltoer M, Laureys M, Huyghens L: Intermittent hemodialysis in critically ill patients with multiple organ dysfunction syndrome is associated with intestinal intramucosal acidosis. Intensive Care Med 22: 747–751, 1996 [DOI] [PubMed] [Google Scholar]
- 56.Abdeen O, Mehta RL: Dialysis modalities in the intensive care unit. Crit Care Clin 18: 223–247, 2002 [DOI] [PubMed] [Google Scholar]
- 57.Davenport A, Will EJ, Davidson AM: Improved cardiovascular stability during continuous modes of renal replacement therapy in critically ill patients with acute hepatic and renal failure. Crit Care Med 21: 328–338, 1993 [DOI] [PubMed] [Google Scholar]
- 58.Cerdá J, Ronco C: Modalities of continuous renal replacement therapy: Technical and clinical considerations. Semin Dial 22: 114–122, 2009 [DOI] [PubMed] [Google Scholar]
- 59.Conger JD: Does hemodialysis delay recovery from acute renal failure? Semin Dial 3 (3): 146–148, 1990 [Google Scholar]
- 60.Mehta RL, McDonald B, Gabbai FB, Pahl M, Pascual MT, Farkas A, Kaplan RM; Collaborative Group for Treatment of ARF in the ICU: A randomized clinical trial of continuous versus intermittent dialysis for acute renal failure. Kidney Int 60: 1154–1163, 2001 [DOI] [PubMed] [Google Scholar]
- 61.Jacka MJ, Ivancinova X, Gibney RT: Continuous renal replacement therapy improves renal recovery from acute renal failure. Can J Anaesth 52: 327–332, 2005 [DOI] [PubMed] [Google Scholar]
- 62.Uchino S, Bellomo R, Kellum JA, Morimatsu H, Morgera S, Schetz MR, Tan I, Bouman C, Macedo E, Gibney N, Tolwani A, Oudemans-Van Straaten HM, Ronco C; Beginning and Ending Supportive Therapy for the Kidney (B.E.S.T. Kidney) Investigators Writing Committee: Patient and kidney survival by dialysis modality in critically ill patients with acute kidney injury. Int J Artif Organs 30: 281–292, 2007 [DOI] [PubMed] [Google Scholar]
- 63.Bell M, Granath F, Schön S, Ekbom A, Martling CR; SWING: Continuous renal replacement therapy is associated with less chronic renal failure than intermittent haemodialysis after acute renal failure. Intensive Care Med 33: 773–780, 2007 [DOI] [PubMed] [Google Scholar]
- 64.Augustine JJ, Sandy D, Seifert TH, Paganini EP: A randomized controlled trial comparing intermittent with continuous dialysis in patients with ARF. Am J Kidney Dis 44: 1000–1007, 2004 [DOI] [PubMed] [Google Scholar]
- 65.Lins RL, Elseviers MM, Van der Niepen P, Hoste E, Malbrain ML, Damas P, Devriendt J; SHARF investigators: Intermittent versus continuous renal replacement therapy for acute kidney injury patients admitted to the intensive care unit: Results of a randomized clinical trial. Nephrol Dial Transplant 24: 512–518, 2009 [DOI] [PubMed] [Google Scholar]
- 66.Wald R, Shariff SZ, Adhikari NK, Bagshaw SM, Burns KE, Friedrich JO, Garg AX, Harel Z, Kitchlu A, Ray JG: The association between renal replacement therapy modality and long-term outcomes among critically ill adults with acute kidney injury: A retrospective cohort study*. Crit Care Med 42: 868–877, 2014 [DOI] [PubMed] [Google Scholar]
- 67.Schneider AG, Bagshaw SM: Effects of renal replacement therapy on renal recovery after acute kidney injury. Nephron Clin Pract 127: 35–41, 2014 [DOI] [PubMed] [Google Scholar]
- 68.Goldstein SL, Chawla L, Ronco C, Kellum JA: Renal recovery. Crit Care 18: 301, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Heung M, Wolfgram DF, Kommareddi M, Hu Y, Song PX, Ojo AO: Fluid overload at initiation of renal replacement therapy is associated with lack of renal recovery in patients with acute kidney injury. Nephrol Dial Transplant 27: 956–961, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hayes LW, Oster RA, Tofil NM, Tolwani AJ: Outcomes of critically ill children requiring continuous renal replacement therapy. J Crit Care 24: 394–400, 2009 [DOI] [PubMed] [Google Scholar]
- 71.Payen D, de Pont AC, Sakr Y, Spies C, Reinhart K, Vincent JL; Sepsis Occurrence in Acutely Ill Patients (SOAP) Investigators: A positive fluid balance is associated with a worse outcome in patients with acute renal failure. Crit Care 12: R74, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bagshaw SM, Brophy PD, Cruz D, Ronco C: Fluid balance as a biomarker: Impact of fluid overload on outcome in critically ill patients with acute kidney injury. Crit Care 12: 169, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Goldstein SL, Somers MJ, Baum MA, Symons JM, Brophy PD, Blowey D, Bunchman TE, Baker C, Mottes T, McAfee N, Barnett J, Morrison G, Rogers K, Fortenberry JD: Pediatric patients with multi-organ dysfunction syndrome receiving continuous renal replacement therapy. Kidney Int 67: 653–658, 2005 [DOI] [PubMed] [Google Scholar]
- 74.Bouchard J, Soroko SB, Chertow GM, Himmelfarb J, Ikizler TA, Paganini EP, Mehta RL; Program to Improve Care in Acute Renal Disease (PICARD) Study Group: Fluid accumulation, survival and recovery of kidney function in critically ill patients with acute kidney injury. Kidney Int 76: 422–427, 2009 [DOI] [PubMed] [Google Scholar]
- 75.Karvellas CJ, Farhat MR, Sajjad I, Mogensen SS, Leung AA, Wald R, Bagshaw SM: A comparison of early versus late initiation of renal replacement therapy in critically ill patients with acute kidney injury: A systematic review and meta-analysis. Crit Care 15: R72, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Seabra VF, Balk EM, Liangos O, Sosa MA, Cendoroglo M, Jaber BL: Timing of renal replacement therapy initiation in acute renal failure: A meta-analysis. Am J Kidney Dis 52: 272–284, 2008 [DOI] [PubMed] [Google Scholar]
- 77.Ronco C, Bellomo R, Homel P, Brendolan A, Dan M, Piccinni P, La Greca G: Effects of different doses in continuous veno-venous haemofiltration on outcomes of acute renal failure: A prospective randomised trial. Lancet 356: 26–30, 2000 [DOI] [PubMed] [Google Scholar]
- 78.Palevsky PM, O’Connor TZ, Chertow GM, Crowley ST, Zhang JH, Kellum JA; US Department of Veterans Affairs/National Institutes of Health Acute Renal Failure Trial Network: Intensity of renal replacement therapy in acute kidney injury: Perspective from within the Acute Renal Failure Trial Network Study. Crit Care 13: 310, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Jun M, Heerspink HJ, Ninomiya T, Gallagher M, Bellomo R, Myburgh J, Finfer S, Palevsky PM, Kellum JA, Perkovic V, Cass A: Intensities of renal replacement therapy in acute kidney injury: A systematic review and meta-analysis. Clin J Am Soc Nephrol 5: 956–963, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Hakim RM: Recent advances in the biocompatibility of haemodialysis membranes. Nephrol Dial Transplant 10[Suppl 10]: 7–11, 1995 [PubMed] [Google Scholar]
- 81.Hakim RM: Clinical implications of biocompatibility in blood purification membranes. Nephrol Dial Transplant 15[Suppl 2]: 16–20, 2000 [DOI] [PubMed] [Google Scholar]
- 82.Himmelfarb J, Hakim RM: The use of biocompatible dialysis membranes in acute renal failure. Adv Ren Replace Ther 4[Suppl 1]: 72–80, 1997 [PubMed] [Google Scholar]
- 83.Schulman G, Hakim RM: Recent advances in the biocompatibility of haemodialysis membranes. Nephrol Dial Transplant 6[Suppl 2]: 10–13, 1991 [PubMed] [Google Scholar]
- 84.Alonso A, Lau J, Jaber BL: Biocompatible hemodialysis membranes for acute renal failure. Cochrane Database Syst Rev (1): CD005283, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Oudemans-van Straaten HM, Wester JP, de Pont AC, Schetz MR: Anticoagulation strategies in continuous renal replacement therapy: Can the choice be evidence based? Intensive Care Med 32: 188–202, 2006 [DOI] [PubMed] [Google Scholar]
- 86.Oudemans-van Straaten HM, Bosman RJ, Koopmans M, van der Voort PH, Wester JP, van der Spoel JI, Dijksman LM, Zandstra DF: Citrate anticoagulation for continuous venovenous hemofiltration. Crit Care Med 37: 545–552, 2009 [DOI] [PubMed] [Google Scholar]
- 87.Oudemans-van Straaten HM, Ostermann M: Bench-to-bedside review: Citrate for continuous renal replacement therapy, from science to practice. Crit Care 16: 249, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Chu JK, Folkert VW: Renal function recovery in chronic dialysis patients. Semin Dial 23: 606–613, 2010 [DOI] [PubMed] [Google Scholar]
- 89.Mohan S, Huff E, Wish J, Lilly M, Chen SC, McClellan WM; Fistula First Breakthrough Initiative Data Committee: Recovery of renal function among ESRD patients in the US medicare program. PLoS One 8: e83447, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kidney Disease Improving Global Outcomes. KDIGO clinical practice guideline for acute kidney injury. Kidney Int 2 (supplement 1): 1–138, 2012 [Google Scholar]
- 91.Milutinovic J, Cutler RE, Hoover P, Meijsen B, Scribner BH: Measurement of residual glomerular filtration rate in the patient receiving repetitive hemodialysis. Kidney Int 8: 185–190, 1975 [DOI] [PubMed] [Google Scholar]
- 92.Chan CT, Covic A, Craig JC, Davenport A, Kasiske BL, Kuhlmann MK, Levin NW, Li PK, Locatelli F, Rocco MV, Wheeler DC: Novel techniques and innovation in blood purification: A clinical update from Kidney Disease: Improving Global Outcomes. Kidney Int 83: 359–371, 2013 [DOI] [PubMed] [Google Scholar]
- 93.Agarwal R: How can we prevent intradialytic hypotension? Curr Opin Nephrol Hypertens 21: 593–599, 2012 [DOI] [PubMed] [Google Scholar]
- 94.Chao CT, Huang JW, Yen CJ: Intradialytic hypotension and cardiac remodeling: a vicious cycle. Biomed Res Int 2015: 724147, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Davenport A: Using dialysis machine technology to reduce intradialytic hypotension. Hemodial Int 15[Suppl 1]: S37–S42, 2011 [DOI] [PubMed] [Google Scholar]
- 96.Doshi M, Murray PT: Approach to intradialytic hypotension in intensive care unit patients with acute renal failure. Artif Organs 27: 772–780, 2003 [DOI] [PubMed] [Google Scholar]
- 97.Macdonald JA, McDonald SP, Hawley CM, Rosman J, Brown F, Wiggins KJ, Bannister K, Johnson DW: Recovery of renal function in end-stage renal failure--comparison between peritoneal dialysis and haemodialysis. Nephrol Dial Transplant 24: 2825–2831, 2009 [DOI] [PubMed] [Google Scholar]
- 98.Canaud G, Bonventre JV: Cell cycle arrest and the evolution of chronic kidney disease from acute kidney injury. Nephrol Dial Transplant 30: 575–583, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Kashani K, Kellum JA: Novel biomarkers indicating repair or progression after acute kidney injury. Curr Opin Nephrol Hypertens 24: 21–27, 2015 [DOI] [PubMed] [Google Scholar]
- 100.Koraishy FM, Coca SG: Can we predict recovery from severe acute kidney injury with biomarkers? Semin Dial 27: 236–239, 2014 [DOI] [PubMed] [Google Scholar]
- 101.Srisawat N, Murugan R, Kellum JA: Repair or progression after AKI: A role for biomarkers? Nephron Clin Pract 127: 185–189, 2014 [DOI] [PubMed] [Google Scholar]
- 102.Heung M, Chawla LS: Predicting progression to chronic kidney disease after recovery from acute kidney injury. Curr Opin Nephrol Hypertens 21: 628–634, 2012 [DOI] [PubMed] [Google Scholar]


