Abstract
The aim of this study was to survey veterinary practitioners’ selection of diagnostic tests for horses with clinical signs of abdominal pain. A questionnaire was distributed to veterinary surgeons involved in the primary evaluation of horses with abdominal pain, including the respondent's demographics, selection of diagnostic tests and factors affecting decision-making. Data analysis included descriptive analysis, categorisation of free text and simple univariable correlations to explore the relationships between independent variables and the relative self-estimated frequency that diagnostic tests were performed. A total of 228 responses were analysed. Participants worked in mixed practice (55.7 per cent), first opinion equine (22.8 per cent), first and second opinion equine (17.9 per cent) and referral practice (3.1 per cent). The majority (48.2 per cent, 105/218) were very confident managing a colic case (confidence level 4/5). The most frequently used diagnostic tests were ‘response to analgesia’ (87.2±24.0 per cent cases), rectal examination (75.9±21.2 per cent) and nasogastric intubation (43.8±27.6 per cent). Approach varied between practitioners, and for all diagnostic tests with frequency of use ranging from 0 to 100 per cent of cases. ‘Risk to personal safety’ was the most common reason for not using rectal examination. Practitioner's opinion of their confidence level in managing a colic case was associated with how frequently they used different diagnostic tests. There was marked variation in practitioners’ approaches, highlighting the need for further evidence to support decision-making.
Keywords: Colic, Diagnostics, Horses, Veterinary profession
Introduction
Colic is of high welfare and economic concern (Traub-Dargatz and others 2001, Egenvall and others 2008), and has been ranked as the most important emergency problem by both owners and veterinary surgeons (Traub-Dargatz and others 1991, Bowden and others 2014). ‘Colic’ refers to the clinical signs of abdominal pain; this has many different aetiologies, and therefore, assessment of the nature of the disease can be extremely challenging (Dukti and White 2009). Clinical signs usually relate to abdominal pain, but other conditions such as thoracic pain can have similarities in presentation (false colic). An early and accurate diagnosis is particularly important for critical cases, where the degree, duration and severity of pathology will impact upon outcome.
Many diagnostic tests can be used to evaluate horses with abdominal pain, and these vary in their cost and the facilities and level of expertise required to perform the techniques and interpreting outcomes. The current research evaluating diagnostic tests for horses with clinical signs of abdominal pain is focused on referral hospital populations. There is limited evidence relating to diagnostic approach at the first evaluation of cases; most information is only available from reviews and textbooks (Greatorex 1972, Wilson and Gordon 1987, Archer 2004, Southwood and Fehr 2012). The primary evaluation of horses with abdominal pain is usually an emergency consultation in the field environment, often with limited facilities and financial restrictions. Factors such as temperament of the horse and availability and cost of diagnostic equipment may have a significant impact on the diagnostic tests employed and decisions made.
The aim of this study was to survey veterinary practitioners’ selection of diagnostic tests for horses with clinical signs of abdominal pain.
The objectives of the study were:
to survey veterinary practitioners’ selection of diagnostic tests for the primary evaluation of horses presenting with clinical signs of abdominal pain;
to identify which factors influence veterinary practitioners’ decision-making in choosing diagnostic tests for horses with clinical signs of abdominal pain;
to determine whether there is an association between veterinary practitioners’ background and experience and their choice of diagnostic tests.
Materials and methods
Survey distribution
A survey of UK equine practitioners was carried out using a mixed methods questionnaire. Online and paper-based versions of the questionnaire were distributed to all UK practitioners with an equine client base, identified from the Royal College of Veterinary Surgeons (RCVS) database, and to all practitioners participating in a survey of the primary evaluation of colic cases (Curtis and others 2014). Veterinary practitioners were asked to complete the questionnaire if they saw any cases of equine colic as part of their veterinary work. The questionnaire could be completed and returned in either paper-based format or in an online format (Adobe Forms Central, Adobe Systems, California, USA). The online version of the survey was open from October 17 to November 15, 2013. Postal questionnaires were distributed on October 28–30, 2013. A follow-up email was sent out two weeks prior to the study's closure to veterinary surgeons and veterinary practices, reminding them to complete the questionnaire.
Questionnaire design
All participants were asked to complete a consent form at the start of the questionnaire, consistent with current guidelines (1998 Data Protection Act, BERA Ethical Guidelines 2011, and Statement for Ethical Practice for the BSA 2002). The questionnaire consisted of both open and closed questions. The first questions related to the demographics of the veterinary practitioner. This included the year the respondent graduated, the type of practice where they worked (categorised into mixed (any combination of species), equine first opinion, equine first and second opinion, equine referral and other) and the estimated number of colic cases the respondents examined each month. Colic was defined as clinical signs of abdominal pain, and the study specified that this survey only related to gastrointestinal causes of abdominal pain.
The next section related to practitioners’ diagnostic approach. This included how frequently they estimated that they used six different diagnostic tests (estimated percentage of cases in which they used rectal examination, abdominal paracentesis, nasogastric intubation, haematology and biochemistry, ultrasound examination and response to analgesia/treatment on the primary assessment of horses with clinical signs of abdominal pain), the scenarios in which they would use each test and the reasons for not using diagnostic tests (including the main primary reason and up to two other reasons why they would not use a diagnostic test). The scenarios in which they would use each test were open free text questions. The reasons why they would not use each diagnostic test were available as list of possible options, based on current and published literature (Gough and Munroe 1998, Archer 2004, Everitt 2011), but also included a free text option for practitioners to identify and describe ‘other’ reasons of their choice. Participants were also given a free text option to identify and describe other diagnostic tests they would use. A copy of the questionnaire is available in online supplementary file 1.
Data analysis
Data were exported from the online response portal (Adobe Forms Central) or input manually for postal forms into a spreadsheet (Excel 2010, Microsoft Corporation, Washington, USA). Descriptive data analyses, including mean, median, mode and range values, were displayed in graphs and tables. Data were tested for normality using QQ plots. Free text responses for a total of 26 open questions within the questionnaire were reviewed, categorised and ranked into order of frequency for each category. The reasons why practitioners did not use each diagnostic test were analysed to determine both the primary reason for not using the test (how frequently each reason was ranked first by respondents) and the total frequency for each reason (total number of times each reason was given, irrespective of ranking; respondents could list up to three reasons for each test). Spearman's rank correlation (ordinal data) and Pearson's correlation coefficient (continuous data) (SPSS V.21 or 22; IBM, New York, USA) were used to evaluate statistical associations between the participants’ demographics (number of years qualified, confidence of practitioner, type of employment) and how frequently they estimated that they used each diagnostic test. Evidence of association was accepted if P<0.05.
Results
An email containing the link to the questionnaire was sent to 943 veterinary surgeons, and paper-based copies of the questionnaire were posted to 985 practitioners/practices (which included some of the practitioners who were emailed directly). In total, 112 questionnaires were returned online (response rate of 11.9 per cent) and 136 paper-based responses were returned by post (response rate of 13.8 per cent), producing an overall total of 248 responses. A percentage response rate was not calculated due to the overlap between contacting practices and practitioners, which meant the total number of vets contacted could not be calculated. Fifteen postal respondents did not complete the ethics statement section, and five respondents were not based in the UK. These responses were excluded; therefore, 228 responses were used for the final data analysis. Some participants did not complete all sections; therefore, the total number of responses is given for each question.
The majority (55.7 per cent) of veterinary surgeons worked in mixed practice (127/228 responses), 22.8 per cent worked in first opinion equine practice (52/228), 17.9 per cent in first and second opinion equine practice (41/228), 3.1 per cent in referral only (7/228) and 0.44 per cent (1/228) in ‘other’ employment (equine charity work).
The number of years since graduation for each participant ranged from 0 to 47, with a median of nine years and a mean value of 14.0±12.0 years (n=226 responses).
The mean number of colic cases that participants stated that they saw was 5.00±4.36 (mean±SD) cases per month, with a range of 0–30 (n=216 responses).
When asked to rate their confidence when assessing a case of colic (0—not confident to 5—very confident), 48.2 per cent (105/218 of participants) rated their confidence level as 4 and 99.5 per cent of respondents rated their confidence level between 2 and 5 (217/218). A number of respondents who had recently qualified rated their confidence level highly (Figure 1).
FIG 1:
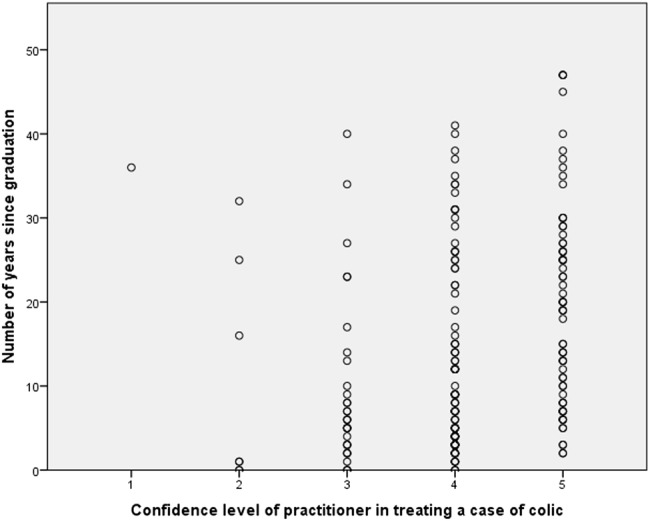
Comparison between number of years and qualified and veterinary practitioners confidence in horses presented with clinical signs of abdominal pain (colic), from a mixed methods questionnaire of 228 UK veterinary surgeons
The next section related to how practitioners used six different diagnostic tests. Participants indicated that they used response to analgesia/treatment most frequently in colic cases (mean ± SD 87.2±24.0 per cent), followed by rectal examination (75.9±21.2 per cent), nasogastric intubation (43.9±27.6 per cent), haematology and biochemistry (15.2±20.6 per cent), abdominal paracentesis (13.5±17.8 per cent) and ultrasound (8.0±18.1 per cent) (Table 1). Individual practitioners’ use of different diagnostic tests varied markedly; for all six tests, there were individual respondents who indicated that they used these tests in 0 per cent and 100 per cent of cases (Table 1). Categorisation of free text responses for reasons for using diagnostic tests indicated that the most commonly identified reason practitioners would use rectal examination was to identify lesion or case type. Abdominal paracentesis was considered most useful to differentiate ‘medical versus surgical’ or to determine prognosis, nasogastric intubation most useful for suspected ‘proximal’ intestinal lesions, ultrasound was also considered most useful for identifying lesion or case type, haematology/biochemistry most useful for recurrent/chronic cases and response to analgesia was considered most useful in most cases (Table 1). When asked for the reasons they would not use specific diagnostic tests, practitioners identified ‘test not required to contribute to diagnosis/treatment’ as the main primary reason for all six diagnostic tests (Table 1). When the total frequency of all the reasons was analysed (primary reason and up to two other reasons from each respondent), the most commonly identified reason varied between the diagnostic tests. ‘Test not required to contribute to diagnosis/treatment’ remained the most frequently identified reason for abdominal paracentesis, nasogastric intubation, haematology and biochemistry, and response to analgesia, but ‘risk to personal safety’ was the most commonly identified reason for not using rectal examination, and ‘lack of facilities/resources’ was the most commonly identified reason for not using ultrasound (Table 1). ‘Other’ reasons for not performing rectal examination were identified in 47/478 reasons identified (each respondent could identify up to three reasons) and included horses that were too small to permit rectal examination. Lack of personal experience in the technique was identified as a reason for not performing ultrasound in 18.0 per cent (76/423) of reasons identified.
TABLE 1:
Practitioners’ selection of different diagnostic tests in horses with colic, and the reasons they would not use specific tests, from a mixed methods survey of UK practitioners
| Diagnostic test | Estimated % of colic cases in which test is used (mean+/SD (range: min–max)) | Scenario in which test is considered to be most useful (most common category identified) | Primary reason for not performing diagnostic test (% frequency of responses) | Top 3 reasons for not performing diagnostic test (% of summed responses) |
|---|---|---|---|---|
| Response to analgesia/treatment | 87.2±24.0 (range 0–100) |
All/most scenarios | Test not required to contribute to diagnosis/treatment (49.5%, 50/161) |
|
| Rectal examination | 75.92±21.2 (range 0–100) |
Identification of specific lesion or case type (including differentiating medical v surgical) | Test not required to contribute to diagnosis/treatment (32.9%, 56/270) |
|
| Nasogastric intubation | 43.85±27.6 (range 0–100) |
Diagnosis of cases with suspected proximal lesion (oesophageal/gastric or small intestinal) | Test not required to contribute to diagnosis/treatment (69.9%, 121/173) |
|
| Haematology and biochemistry | 15.23±20.6 (range 0–100) |
Diagnosis of recurrent colic/ongoing cases | Test not required to contribute to diagnosis/treatment (63.6%, 110/173) |
|
| Abdominocentesis | 13.45±17.8 (range 0–100) |
Determination of diagnosis/prognosis of medical v surgical/severe cases of colic/decision for euthanasia | Test not required to contribute to diagnosis/treatment (65.9%, 116/176) |
|
| Ultrasound | 8.04±18.1 (range: 0–100) |
Identification of specific lesion or case type (including differentiating medical v surgical) | Test not required to contribute to diagnosis/treatment (44.0%, 74/168) |
|
In total, 196 respondents gave free text information that they used other diagnostic tests more frequently than the six listed in the questionnaire. Also, 52 different descriptions were listed by 42 respondents, and the main tests identified were clinical examination (63.5 per cent) and faecal analysis (13.5 per cent).
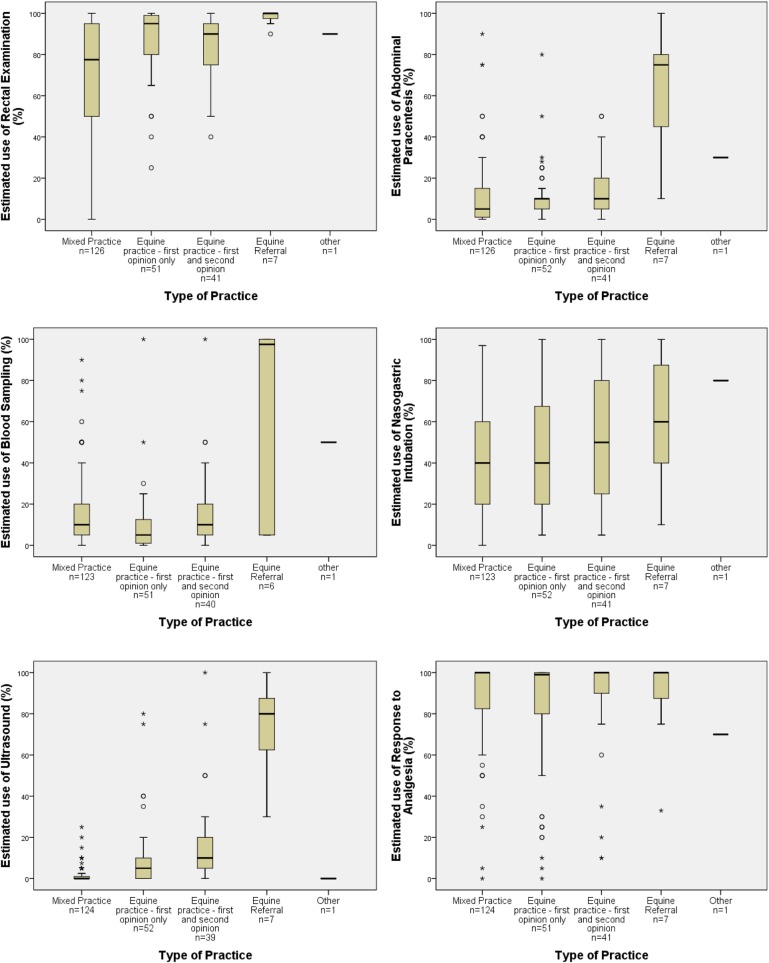
Practitioner's estimates of how frequently they use diagnostic tests in colic (rectal examination, abdominal paracentesis, blood sampling, nasogastric intubation, ultrasound and response to analgesia) were analysed according to their employment (Figure 2). Practitioners employed in mixed practice estimated that they used rectal examination less frequently (mean use 75.8 per cent, range 0–100 per cent) compared with those employed in equine only practice (first opinion equine (mean 95.0 per cent range, 65.0–100 per cent), first and second opinion equine practice (mean 90.1 per cent, range 49.8–100 per cent) and equine referral practice (mean 100 per cent, range 95.0–100 per cent)). There was also a higher mean estimated frequency of usage of abdominal paracentesis blood sampling and ultrasound in equine referral practice than other types of practice (Figure 2). There was moderate variation in the estimated use of nasogastric intubation (39.7–79.9 per cent) and response to analgesia across the different types of practice (70.0–100 per cent).
FIG 2:
Box and whisker plots showing the estimated frequency of use of rectal examination, abdominal paracentesis, blood sampling, nasogastric intubation, ultrasound and response to analgesia in horses presented with clinical signs of abdominal pain (colic) by veterinary practitioners working in different types of practice, from a mixed methods questionnaire of 228 UK veterinary surgeons
There was evidence of an association between the self-assessed confidence level of the practitioner and the estimated frequency of use of diagnostic tests, with increased confidence level significantly associated with an increased use of rectal examination (P<0.001), ultrasound examination (P<0.001) and abdominal paracentesis (P<0.05). The numbers of years a practitioner had been qualified were not significantly associated with the frequency of use of diagnostic tests, except for nasogastric intubation, which was used less frequently with increased years since qualification (P>0.001) (Table 2).
TABLE 2:
Association between the frequency of use of different diagnostic tests in the primary evaluation of equine colic and the demographics of the veterinary practitioners, from a mixed methods questionnaire of 228 UK practitioners
| Diagnostic test used in primary evaluation of equine colic | No. of years graduated | Confidence level of practitioner |
|---|---|---|
| Rectal examination | Pearson 0.02 P=0.82 (n=224) |
Coeff. 0.29** P<0.01 (n=216) |
| Abdominal paracentesis | Pearson 0.06 P=0.36 (n=225) |
Coeff. 0.17* P=0.02 (n=227) |
| Nasogastric intubation | Pearson −0.18** P=0.01 (n=222) |
Coeff.0 .010 P=0.88 (n=214) |
| Haematology and biochemistry | Pearson −0.01 P=0.93 (n=219) |
Coeff. 0.03 P=0.62 (n=211) |
| Ultrasound examination | Pearson 0.01 P=0.87 (n=221) |
Coeff. 0.34** P<0.01 (n=213) |
| Response to analgesia/treatment | Pearson −0.12 P=0.07 (n=223) |
Coeff. −0.06 P=0.37 (n=214) |
Evidence of association was accepted if P<0.05
n, number of valid responses; Pearson, Pearson's correlation coefficient; Coeff., Spearman's rank correlation coefficient
*P<0.05, **P<0.005
Discussion
There are many factors that influence clinical decision-making. Everitt (2011) studied decision-making by veterinary practitioners, in a range of different scenarios, predominantly based in small animal practice, but including equine and types of other practice. She identified a large degree of variation in the decisions made between clinicians (Everitt 2011). Factors identified in previous studies are the age and experience of the veterinary practitioner, actual and perceived value of the test, risks to the animal and veterinary practitioner, cost of the test and owner preference (Kassirer 1976, Gough and Munroe 1998, Lucas and others 2009, Vandeweerd and others 2012). The current survey highlighted that in the majority of primary assessments of horses with clinical signs of abdominal pain practitioners use a small number of key tests (predominantly response to analgesia, rectal examination), and other diagnostic tests are used infrequently. The primary reason not to use a diagnostic test, for all six tests investigated, was that practitioners did not consider that the tests were required to contribute to a diagnosis. A number of other reasons were identified that are particularly relevant to the primary assessment of patients. These included lack of facilities and resources, financial constraints and risk to the veterinary surgeon; these were most frequently mentioned for rectal examination, nasogastric intubation and abdominal paracentesis. The current survey also highlighted that the main factors influencing use of diagnostic tests were confidence levels of the practitioner and the type of practice they worked in.
The current study had a relatively low response rate. Response rates for surveys of veterinary surgeons can be variable, with published rates varying between 20 and 50 per cent (Nielsen and others 2006, Roberts and Murray 2013). The RCVS manpower survey of 2014 had a response rate of 27 per cent (Robinson and others 2014), and the British Equine Veterinary Association (BEVA) member survey 2014 had 471 members responding (percentage response rate unknown), with 377 participants completing the questionnaire (Anon 2014). The total response rate was not calculated for this study as the postal questionnaires were circulated to practices as well as individuals, and therefore, the total population is unknown. A low response rate reduces the validity and may introduce bias into a study, and the outcomes of this survey should be interpreted with this in mind. Potential biases are increased participation by practitioners with an interest in clinical research or evidence-based medicine or by those who are outliers within the target population. Outliers may include both ranges of the spectrum, from practitioners who see many cases and consider themselves to have a high level of expertise to those who are inexperienced, have low confidence levels or who have had a negative experience. Practitioners are more likely to remember difficult or unsuccessful cases and their responses may be biased or influenced by these. An ideal study design would follow-up on non-responders to improve response rates and to determine whether their demographics and selections were similar to the respondents. The effect of a low response rate on validity is reduced if the responders are representative of the study population.
Over 50 per cent of the respondents in this survey worked in mixed practice, with only a small percentage (3.1 per cent) in referral hospital situations. There are no directly comparable studies or databases of the numbers and distribution of veterinary surgeons who are involved in equine veterinary work in the UK. The RCVS 2014 manpower survey of 6988 respondents reported that 15.8 per cent of practitioners worked in mixed practice, 5.5 per cent in equine and 8.1 per cent in referral (but referral included all species) (Robinson and others 2014). The BEVA member survey 2014 of 471 respondents reported that 14.73 per cent of participants worked in mixed practice, 48.2 per cent in general practices and 19.6 per cent in referral practice although this survey was of members of the BEVA only; therefore, mixed practitioners were likely to be under-represented as they may be members of other professional organisations. The current study included a range of experiences from new graduates to practitioners who had been qualified for many years (maximum 47 years). The estimated number of colic cases seen per month also showed a significant range from 0 to 30, but as highlighted earlier, this will be subject to recall bias. Practitioners may overestimate the number of cases seen if they consider themselves very experienced or if the cases have been difficult or stressful. Despite this, the confidence levels of the practitioners were high, with the majority (48.2 per cent) rating their confidence as 4/5. Factors that affect confidence level may include the duration of time since qualifying (Vandeweerd and others 2012), gender of participants (Lundeberg and others 1994) and the number of cases seen. Confidence and clinical experience generated an expected connection; however, high confidence scores were not restricted to older practitioners, and a number of recently qualified veterinary surgeons also placed themselves at the higher end of the confidence scale.
This study focused on six diagnostic tests: rectal examination, abdominal paracentesis, nasogastric intubation, haematology and biochemistry, ultrasound and response to analgesia/treatment. These six tests were selected based on review of the current literature and the results of a survey of practitioners’ data from clinical cases (Curtis and others 2014). Rectal examination was used in approximately three-quarters of cases (75.9 per cent), but there was a wide variation in its use (range 0–100 per cent of cases). This variation between different individuals may be due to concerns over personal safety, but could also reflect the variation between different practitioners and their approach to a colic case. Risk to personal safety and poor cooperation of the horse were commonly identified as reasons for not performing a rectal examination. This probably reflects the challenges of the field setting for the examination of most cases and the greater risk of injury to practitioners working in equine practice (Reijula and others 2003, BEVA 2014). Everitt (2011) also found that the cooperation and temperament of the animal can influence the decision-making process. Poor cooperation from the horse was among the three main reasons deterring practitioners from the use of a rectal examination, abdominal paracentesis and nasogastric intubation in this study, highlighting the practical challenges and risks to practitioners. Confidence level was significantly associated with the use of three of the six diagnostic tests, and this may reflect a concern over potential welfare and litigation associated risks, such as rectal tearing, in addition to the risks of injury to the practitioner (Southwood and Fehr 2012), both of which may impact confidence levels. There was, however, no significant association between duration of time since qualifying and use of diagnostic tests with the exception of nasogastric intubation, suggesting that this is not a main factor in decision-making for most diagnostic tests for colic.
Ultrasound examination was ranked as the least important test when evaluating a case of colic. The main reason for using it was identified as to help determine the type of lesion, which suggests that it is used mainly in more difficult/critical cases. There is evidence within the literature on the value of ultrasound as a diagnostic tool and its increased sensitivity for detecting specific conditions compared with rectal palpation (Klohnen and others 1996, Slack 2012). Lack of facilities/resources and finance of the owner were identified as two of the three main limiting factors that prevent vets from performing ultrasound. In addition, 18 per cent of responses identified lack of personal experience as a limiting factor, and 16 participants (data not shown) identified ultrasound examination as the test they would like to perform but currently do not because of a lack of facilities and/or sufficient knowledge. There was a significant association between practitioner confidence and ultrasound usage, with increased use associated with higher confidence scores, and in referral practice. This demonstrates that there are issues around availability, cost and training that may currently limit the practical use of ultrasound in colic cases.
The financial situation of the owner was considered an important factor when deciding whether to use haematology and biochemistry, ultrasound examination and response to analgesia/treatment. Again, this finding was also reported by Everitt (2011), who considered it to be a fundamental factor that influences the decision-making process. There are concerns within the equine veterinary profession about the impact of the current financial climate on owner decision-making and treatment options for equine colic (Blikslager and Mair 2014).
This study has highlighted veterinary practitioners’ selection of different diagnostic tests and identified some factors that are significantly associated with the use of different tests. There may be other confounding factors affecting these associations that could not be determined within the scope of this project and the nature of univariable analysis. More detailed qualitative investigation, such as interviews and focus groups, is warranted to understand the demotivators for the use of diagnostic tests such as rectal examination and explore some of the wide variations in approach. Further evidence is also required on how history and clinical findings influence decision-making, the value of diagnostic tests for horses presenting with colic and the incidence of complications associated with different tests, to enable practitioners to make an evidence-based decision on the benefits and risks of different procedures.
This study describes veterinary practitioners’ selection of the diagnostic tests used in the primary assessment of horses with clinical signs of abdominal pain. Practitioners use a relatively small number of tests in the majority of cases (predominantly response to analgesia and rectal examination); risk to personal safety and poor cooperation of the horse were key reasons practitioners did not perform rectal examinations. This study identified significant variation between individual practitioners’ approaches. The practitioner's level of confidence was associated with frequency of use of diagnostic tests. Further research in this area would help develop strategies to assist veterinary surgeons with the decision-making process.
Acknowledgments
The authors would like to thank the participating veterinary surgeons.
Footnotes
Contributors: LC and IT were the main researchers, with the major roles in data collection, data analysis and manuscript preparation. GCWE, JHB and SLF contributed to study design, data collection and study execution, and preparation of the final manuscript.
Funding: LC was funded by the School of Veterinary Medicine and Science, University of Nottingham. The survey was supported by a grant from Petplan Charitable Trust.
Competing interests: None declared.
Ethics approval: The study was reviewed and approved by the Ethics Committee, School of Veterinary Medicine and Science, University of Nottingham.
Provenance and peer review: Not commissioned; internally peer reviewed.
Data sharing statement: A copy of the study questionnaire and an anonymised version of raw data set are available from the authors on request.
References
- Anon (2014) BEVA Member Survey 2014. http://www.beva.org.uk/membership/membershipsurvey2012. (accessed 17 Jul 2015)
- Archer D. C. (2004) Decision making in the management of the colicky horse. In Practice 26, 378–385 doi:10.1136/inpract.26.7.378 [Google Scholar]
- BEVA (2014) Survey reveals high risk of injury to equine vets. Veterinary Record 175, 263 doi:10.1136/vr.g5714 [DOI] [PubMed] [Google Scholar]
- Blikslager A. & Mair T. (2014) Trends in management of horses referred for evaluation of colic: 2004–2013. Eleventh International Colic Research Symposium, Dublin, Ireland [Google Scholar]
- Bowden A., Burford J. H. & Freeman S. L. (2014) Equine emergencies: opinions of yard owners. The Eleventh Equine Colic Research Symposium, Dublin [Google Scholar]
- Curtis L., Curran M. L., Bayes T. C., England G. C. W., Burford J. H. & Freeman S. L. (2014) Prospective study of primary assessment of equine colic. Part 1: study population and case presentation. Eleventh International Colic Research Symposium. Dublin, Ireland [Google Scholar]
- Dukti S. & White N. (2009) Prognosticating Equine Colic. Veterinary Clinics of North America Equine Practice 25, 543–544 doi:10.1016/j.cveq.2009.08.004 [DOI] [PubMed] [Google Scholar]
- Egenvall A., Penell J., Bonnett B. N., Blix J. & Pringle J. (2008) Demographics and costs of colic in Swedish horses. Journal of Veterinary Internal Medicine 22, 1029–1037 doi:10.1111/j.1939-1676.2008.0136.x [DOI] [PubMed] [Google Scholar]
- Everitt S. (2011) Clinical Decision Making in Veterinary Practice. University of Nottingham [Google Scholar]
- Gough M. & Munroe G. (1998) Decision making in the diagnosis and management of bone spavin horses. In Practice 20, 252–259 doi:10.1136/inpract.20.5.252 [Google Scholar]
- Greatorex J. C. (1972) The clinical diagnosis of colic in the horse. Equine Veterinary Journal 4, 182–187 doi:10.1111/j.2042-3306.1972.tb03906.x [Google Scholar]
- Kassirer J. P. (1976) The principles of clinical decision making: an introduction to decision analysis. Yale Journal of Biology and Medicine 49, 149–164 [PMC free article] [PubMed] [Google Scholar]
- Klohnen A., Vachon A. M. & Fischer A. T. Jr (1996) Use of diagnostic ultrasonography in horses with signs of acute abdominal pain. Journal of the American Veterinary Medical Association 209, 1597–1601 [PubMed] [Google Scholar]
- Lucas M., Day L. & Fritschi L. (2009) Injuries to Australian veterinarians working with horses. The Veterinary Record 164, 207–209 doi:10.1136/vr.164.7.207 [DOI] [PubMed] [Google Scholar]
- Lundeberg M. A., Fox P. W. & Puncochar J. (1994) Highly confident but wrong - gender differences and similarities in confidence judgements. Journal of Educational Psychology 86, 114–121 doi:10.1037/0022-0663.86.1.114 [Google Scholar]
- Nielsen M. K., Monrad J. & Olsen S. N. (2006) Prescription-only anthelmintics—a questionnaire survey of strategies for surveillance and control of equine strongyles in Denmark. Veterinary Parasitology 135, 47–55 doi:10.1016/j.vetpar.2005.10.020 [DOI] [PubMed] [Google Scholar]
- Reijula K., Räsänen K., Hämäläinen M., Juntunen K., Lindbohm M., Taskinen H., Bergbom B. & Rinta-Jouppi M. (2003) Work environment and occupational health of Finnish veterinarians. American Journal of Industrial Medicine 44, 46–57 doi:10.1002/ajim.10228 [DOI] [PubMed] [Google Scholar]
- Roberts J. L. & Murray J. (2013) Survey of equine nutrition: perceptions and practices of veterinarians in Georgia, USA. Journal of Equine Veterinary Science 33, 454–459 doi:10.1016/j.jevs.2012.08.001 [Google Scholar]
- Robinson D., Williams M. & Buzzeo J. (2014) RCVS Survey of the Veterinary Professions 2014 Synthesis Report. https://www.rcvs.org.uk/publications/rcvs-survey-of-the-veterinary-profession-2014/. (accessed 17 Jul 2015)
- Slack J. (2012) Abdominal sonographic evaluation. In: Southwood L. L., Ed. Practical Guide to Equine Colic. John Wiley & Sons, Inc., pp. 116–148 [Google Scholar]
- Southwood L. L. & Fehr J. E. (2012) Abdominal palpation per rectum. In: Southwood L. L., Ed. Practical Guide to Equine Colic. John Wiley & Sons, Inc., pp. 22–37 [Google Scholar]
- Traub-Dargatz J., Salman M. & Voss J. (1991) Medical problems of adult horses, as ranked by equine practitioners. Journal of the American Veterinary Medical Association 198, 1745–1747 [PubMed] [Google Scholar]
- Traub-Dargatz J. L., Kopral C. A., Seitzinger A. H., Garber L. P., Forde K. & White N. A. (2001) Estimate of the national incidence of and operation-level risk factors for colic among horses in the United States, spring 1998 to spring 1999. Journal of the American Veterinary Medicine Association 219, 67–71 doi:10.2460/javma.2001.219.67 [DOI] [PubMed] [Google Scholar]
- Vandeweerd J. M., Vandeweerd S., Gustin C., Keesemaecker G., Cambier C., Clegg P., Saegerman C., Reda A., Perrenoud P. & Gustin P. (2012) Understanding veterinary practitioners’ decision-making process: implications for veterinary medical education. Journal of Veterinary Medicine Education 39, 142–151 doi:10.3138/jvme.0911.098R1 [DOI] [PubMed] [Google Scholar]
- Wilson J. & Gordon B. (1987) Equine colic - interpreting the diagnostic tests. Veterinary Medicine 82, 629–645 [Google Scholar]