Abstract
Background:
There is a paucity of studies addressing the elevation of C-reactive protein (CRP) among psoriatic patients and the role of this marker in assessment of disease severity and association with cardiovascular diseases (CVDs).
Objective:
To assess the difference in CRP levels between psoriatic patients and healthy population and to determine their role in disease severity. Also to compare CRP levels in psoriatic patients with and without the metabolic syndrome.
Materials and Methods:
A total of hundred patients with chronic plaque psoriasis and an equal number of age- and gender-matched healthy controls were enrolled in the study over a period of one year. Serum CRP levels of both cases and controls were estimated. Metabolic syndrome was identified among psoriasis patients using National Cholesterol Education Program's Adult Panel III (ATP III) guidelines. Clinical activity of psoriasis was evaluated using Psoriasis Area and Severity Index Score.
Results:
Patients with psoriasis reported significantly higher levels of CRP than healthy controls (P value 0.001). Patients with severe disease had significantly higher levels of CRP (P value < 0.003). Elevated level of CRP was observed among psoriatic patients with the metabolic syndrome than patients without the metabolic syndrome and the difference was statistically significant (P value = 0.001).
Conclusion:
CRP may be considered as a useful marker of psoriasis severity that could be used to monitor psoriasis and its treatment. Elevated levels of CRP may be an independent risk factor for CVD in patients with psoriasis.
Keywords: Cardiovascular risk factor, C-reactive protein, PASI score, psoriasis
INTRODUCTION
Psoriasis is a common chronic immune-mediated disease that affects 1%-3% of population and is characterized by inflammatory cell infiltration and hyperproliferation of epidermal cells.[1,2] In recent years, psoriasis has been recognized as a systemic disease associated with the metabolic syndrome or its components such as obesity, insulin resistance, hypertension, and atherogenic dyslipidemia.[3] The association of psoriasis with enhanced atherosclerosis and risk of cardiovascular disease (CVD) may account for higher morbidity and mortality rates in psoriatic patients. The intensity of inflammation and skin changes in psoriasis may not only indicate the severity of psoriasis but also that of other systemic pathologies.[4] C-reactive protein, although nonspecific, is known to be the most sensitive indicator of inflammation, the magnitude of its increase correlating with the extent of tissue injury and inflammation severity.[5] It has a short half-life of 6-8 h making it an appropriate tool for following disease course.[6] Many studies have demonstrated an association between increased blood CRP levels, neutrophil activation, and CVD, thus suggesting CRP to be an independent risk factor for CVD.
There is a paucity of studies addressing whether and to what extent the CRP levels are raised among psoriatic patients and if the marker can play a role in assessment of disease severity. Our aim was to evaluate the role of CRP as a marker of disease severity and cardiovascular risk factor in patients with psoriasis.
MATERIALS AND METHODS
This study was conducted in the Department of Dermatology of a tertiary care institution in South India, between September 2012 and December 2013, after being approved by the institutional ethics committee. It was a hospital-based, case–control study. The study group included 100 patients of chronic plaque psoriasis and an equal number of age- and gender-matched healthy controls. All consecutive clinically diagnosed cases of chronic plaque psoriasis (excluding psoriatic arthritis and other inflammatory disorders) above the age of 18 years not receiving any systemic treatment for psoriasis and not on any other medications affecting carbohydrate and lipid metabolism (beta-blockers, thiazides, corticosteroids, and lipid-lowering agents) for at least one month prior to enrolment were included in the study. Controls were age- and gender-matched normal healthy individuals (attendants of patients and staff members of the hospital).
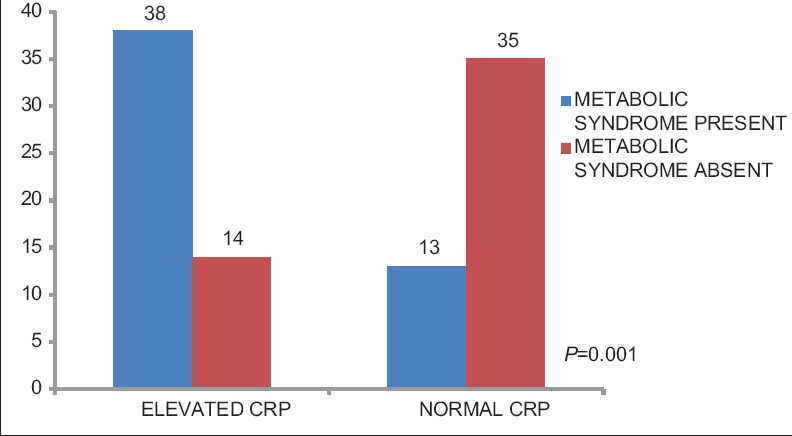
Relevant data included age, gender, weight, height, body mass index, waist circumference, blood pressure, smoking, alcohol abuse, age of onset, and duration of psoriasis. Severity of psoriasis was assessed according to Psoriasis Area and Severity Index (PASI) score, determined by the same investigator in all 100 cases. PASI < 10 was considered mild and PASI > 10 was considered severe disease.[7] Investigations carried out included fasting lipid profile, fasting and postprandial blood glucose, and C-reactive protein (immunoturbidimetry). Metabolic syndrome was diagnosed by the presence of three or more criteria of the National Cholesterol Education Program's Adult Panel III (ATP III) criteria [Table 1].[8]
Table 1.
Criteria of the National Cholesterol Education Program's Adult Panel III for diagnosis of metabolic syndrome
RESULTS
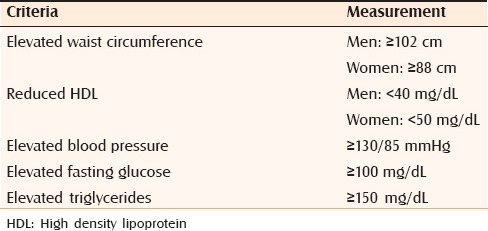
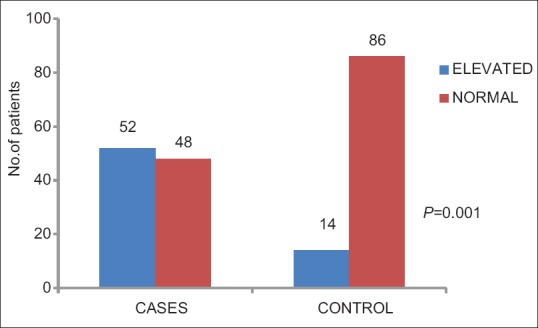
The study included 100 patients with chronic plaque psoriasis and an equal number of age- and gender-matched healthy controls. The mean age of the patients with psoriasis was 44.71 ± 10.84 (mean ± SD). Maximum number of patients were in the age group 41-50 years. PASI score ranged from 2 to 54, mean PASI being 18.15 ± 12.208. We found a higher prevalence of the metabolic syndrome in cases than controls (51% vs 29%, P = 0.005). CRP was significantly elevated (>5 mg/L) in psoriatic patients when compared with controls (52% vs 14%) (P = 0.001). Psoriatic patients with severe disease (PASI > 10) showed significantly higher levels of CRP than those with mild disease (PASI < 10) (44% vs 25%, P value = 0.003). Elevated levels of CRP was seen more in psoriatic patients with the metabolic syndrome when compared with patients without the metabolic syndrome and the difference was statistically highly significant (P value = 0.001) [Figures 1–3].
Figure 1.
C-reactive protein among cases and controls
Figure 3.
C-reactive protein in psoriatic patients with and without metabolic syndrome
Figure 2.
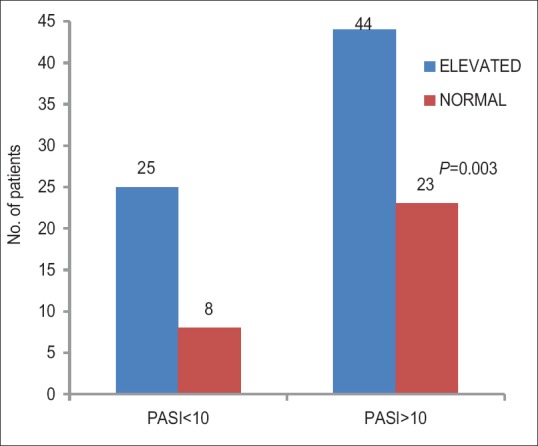
C-reactive protein and disease severity
DISCUSSION
Unlike the earlier rejection of CRP as an empirical test because of its perceived lack of specificity, the current stress over CRP is widely characterized by failure to recognize appropriately the nonspecific nature of the acute phase response.[9] The plasma half-life of CRP is constant under all conditions of health and disease, so that the sole determinant of circulating levels of CRP is the synthesis rate, which thus directly reflects the intensity of pathological process stimulating CRP production.[9,10]
Several studies have investigated the role of CRP in psoriasis. Two studies by Vanizor et al. have shown that patients with psoriasis have significantly high baseline levels of CRP compared with healthy controls (P < 0.004 and P < 0.001).[11,12,13] Malbris et al. noted that patients with psoriasis had higher levels of CRP compared with controls, with a positive correlation between CRP and total plasma cholesterol.[14] In our study, CRP was elevated (>5 mg/L) in 52% of psoriatic patients when compared with 14% of control population and the difference was statistically highly significant (P value 0.001). Similar results were observed by Rocha-Periera et al.[15] in a study evaluating inflammatory markers in patients with mild or severe psoriasis. In a study by Kimbell et al.,[11] CRP levels correlated with the presence and severity of disease, with the lowest levels seen in the control group and progressively higher CRP levels observed in patients with increasing disease severity. Compared with controls, patients with mild and severe psoriasis had significantly higher levels of CRP (mean ± standard deviation; 0.31 ± 0.02 mg/dL vs 0.90 ± 0.27 mg/dL; P < 0.001). Further comparison indicated that patients with severe psoriasis had significantly higher levels of CRP than those with only mild disease (mean ± standard deviation; 0.63 ± 0.03 mg/dL vs 1.16 ± 0.07 mg/dL; P < 0.001). In our study, we found a significant association between disease severity and elevated CRP levels. Psoriatic patients with severe disease (PASI > 10) had significantly higher levels of CRP than those with mild disease (PASI < 10) (44% vs 25%) (P value = 0.003). Thus, these results are consistent with the characterization of psoriasis as an inflammatory response that worsens with increasing disease severity. Several other studies have also reported a correlation between increased levels of CRP and PASI.[3,5,16] Thus, CRP can be considered as a useful marker of disease severity that could be used to monitor the disease course and its treatment.
CRP is an independent risk factor for CVD.[6,17] The greater than expected incidence of coronary artery disease in psoriatic patients might be attributable to the high levels of this marker.[18] Several studies have reported a link between the levels of CRP and CVD, hypertriglyceridemia, abnormal blood pressure, and insulin resistance.[9,19,20] In our study, when we compared the CRP levels in psoriatic patients with and without the metabolic syndrome, CRP was significantly elevated in patients with the metabolic syndrome (38% vs 13%, P = 0.001). Possible specific associations of CRP with CVD include binding of CRP selectively to LDL, especially “damaged” LDL, deposition of CRP in most atherosclerotic plaques, and co-deposition of CRP with activated complement in acute myocardial infarction lesions.[9] Raised baseline CRP values are also associated with many features of insulin resistance and the metabolic syndrome. It has been suggested that the inflammatory process in psoriasis, which is characterized by elevated levels of CRP, is connected to increased arterial stiffness and premature development of atherosclerosis. These findings provide further evidence of a link between inflammation and CVD in patients with psoriasis.[3]
There is a recent emphasis on the “high-sensitivity” CRP, abbreviated as hs CRP. The “high sensitivity” refers to the lower detection limit of the assay procedure being used. The actual CRP analyte, the plasma protein that is being measured, is the same regardless of the assay range.[9] Various studies have demonstrated that hs CRP independently predicts vascular risk and has additive prognostic value at all levels of the metabolic syndrome or in the prediction of type 2 diabetes mellitus.[21]
CONCLUSION
There has been no accurate laboratory tool to assess the psoriasis severity and progress. PASI is currently the preferred method for the evaluation of disease severity. However, the subjective nature and limited utility for non–plaque-type disease limits its use. CRP estimation is inexpensive, widely available, and can be easily carried out in an outpatient clinical setting. CRP along with PASI could be used as a powerful and sensitive blood marker to evaluate psoriasis disease severity, as it is not based on visual evaluation of the lesions. It can be used to monitor the disease course and treatment. As there is evidence supporting the link between inflammation and CVD in patients with psoriasis, elevation of CRP may be considered as a risk factor for CVD in patients with psoriasis. However, further research especially using highly sensitive techniques for CRP determination is required to confirm this observation.
Footnotes
Source of Support: Shiraz University of Medical Sciences
Conflict of Interest: None declared.
REFERENCES
- 1.Takahashi H, Iizuka H. Psoriasis and metabolic syndrome. J Dermatol. 2012;39:212–8. doi: 10.1111/j.1346-8138.2011.01408.x. [DOI] [PubMed] [Google Scholar]
- 2.Neimann AL, Shin DB, Margolis DJ, Wang X, Troxel AB. Prevalence of cardiovascular risk factors in patients with psoriasis. J Am Acad Dermatol. 2006;55:829–35. doi: 10.1016/j.jaad.2006.08.040. [DOI] [PubMed] [Google Scholar]
- 3.Gerkowicz A, Pietrzak A, Szepietowski JC, Radej S, Chodorowska G. Biochemical markers of psoriasis as a metabolic disease. Folia Histochem Cytobiol. 2012;50:155–70. doi: 10.5603/fhc.2012.0025. [DOI] [PubMed] [Google Scholar]
- 4.Pietrzak A, Bartosińska J, Chodorowska G, Szepietowski JC, Paluszkiewicz P, Schwartz RA. Cardiovascular aspects of psoriasis: An updated review. Int J Dermatol. 2013;52:153–62. doi: 10.1111/j.1365-4632.2012.05584.x. [DOI] [PubMed] [Google Scholar]
- 5.Coimbra S, Oliveira H, Reis F, Belo L, Rocha S, Quintanilha A, et al. C-reactive protein and leucocyte activation in psoriasis vulgaris according to severity and therapy. J Eur Acad Dermatol Venereol. 2010;24:789–96. doi: 10.1111/j.1468-3083.2009.03527.x. [DOI] [PubMed] [Google Scholar]
- 6.Beygi S, Lajevardi V, Abedini R. C-reactive protein in psoriasis: A review of the literature. J Eur Acad Dermatol Venereol. 2014;28:700–11. doi: 10.1111/jdv.12257. [DOI] [PubMed] [Google Scholar]
- 7.Feldman SR. The design of Clinical trials in psoriasis: Lessons for clinical practice. J Am Acad Dermatol. 2003;49:S62–5. doi: 10.1016/s0190-9622(03)01137-x. [DOI] [PubMed] [Google Scholar]
- 8.Pereira RR, Amladi ST, Varthakavi PK. A study of the prevalence of diabetes, insulin resistance, lipid abnormalities and cardiovascular risk factors in patients with chronic plaque psoriasis. Indian J Dermatol. 2011;56:520–6. doi: 10.4103/0019-5154.87144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pepys MB, Hirschfield GM. C-reactive protein: A critical update. J Clin Invest. 2003;111:1805–12. doi: 10.1172/JCI18921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vigushin DM, Pepys MB, Hawkins PN. Metabolic and scintigraphic studies of radioiodinated human C-reactive protein in health and disease. J Clin Invest. 1993;91:1351–7. doi: 10.1172/JCI116336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kimball AB, Wu Y. Cardiovascular disease and classic cardiovascular risk factors in patients with psoriasis. Int J Dermatol. 2009;48:1147–56. doi: 10.1111/j.1365-4632.2009.04075.x. [DOI] [PubMed] [Google Scholar]
- 12.Vanizor Kural B, Orem A, Cimşit G, Yandi YE, Calapoglu M. Evaluation of the atherogenic tendency of lipids and lipoprotein content and their relationships with oxidant-antioxidant system in patients with psoriasis. Clin Chim Acta. 2003;328:71–82. doi: 10.1016/s0009-8981(02)00373-x. [DOI] [PubMed] [Google Scholar]
- 13.Vanizor Kural B, Orem A, Cimşit G, Uydu HA, Yandi YE, Alver A. Plasma homocysteine and its relationships with atherothrombotic markers in psoriatic patients. Clin Chim Acta. 2003;332:23–30. doi: 10.1016/s0009-8981(03)00082-2. [DOI] [PubMed] [Google Scholar]
- 14.Mallbris L, Granath F, Hamsten A, Ståhle M. Psoriasis is associated with lipid abnormalities at the onset of skin disease. J Am Acad Dermatol. 2006;54:614–21. doi: 10.1016/j.jaad.2005.11.1079. [DOI] [PubMed] [Google Scholar]
- 15.Rocha-Pereira P, Santos-Silva A, Rebelo I, Figueiredo A, Quintanilha A, Teixeira F. The inflammatory response in mild and in severe psoriasis. Br J Dermatol. 2004;150:917–28. doi: 10.1111/j.1365-2133.2004.05984.x. [DOI] [PubMed] [Google Scholar]
- 16.Coimbra S, Oliveira H, Reis F, Belo L, Rocha S, Quintanilha A, et al. Circulating adipokine levels in portugese patients with psoriasis vulgaris according to body mass index, severity and therapy. J Eur Acad Dermatol Venereol. 2010;24:1386–94. doi: 10.1111/j.1468-3083.2010.03647.x. [DOI] [PubMed] [Google Scholar]
- 17.Ridker PM, Buring JE, Shih J, Matias M, Hennekens CH. Prospective study of C-reactive protein and the risk of future cardiovascular events among apparently healthy women. Circulation. 1998;98:731–3. doi: 10.1161/01.cir.98.8.731. [DOI] [PubMed] [Google Scholar]
- 18.Siegel D, Devaraj S, Mitra A, Raychaudhuri SP, Raychaudhuri SK, Jialal I. Inflammation, atherosclerosis, and psoriasis. Clin Rev Allergy Immunol. 2013;44:194–204. doi: 10.1007/s12016-012-8308-0. [DOI] [PubMed] [Google Scholar]
- 19.Ridker PM. C-reactive protein: Eighty years from discovery to emergence as a major risk marker for cardiovascular disease. Clin Chem. 2009;55:209–15. doi: 10.1373/clinchem.2008.119214. [DOI] [PubMed] [Google Scholar]
- 20.Yeh ET, Palusinski RP. C-reactive protein: The pawn has been promoted to queen. Curr Atheroscler Rep. 2003;5:101–5. doi: 10.1007/s11883-003-0080-4. [DOI] [PubMed] [Google Scholar]
- 21.Ridker PM, Wilson PW, Grundy SM. Should C-reactive protein be added to metabolic syndrome and to assessment of global cardiovascular risk? Circulation. 2004;109:2818–25. doi: 10.1161/01.CIR.0000132467.45278.59. [DOI] [PubMed] [Google Scholar]


