Abstract
Ecthyma gangrenosum is a rare skin infection caused by Pseudomonas aeruginosa. It is usually seen in immunocompromised and critically ill patients. We report one such case in a previously healthy 20-year old male. Ecthyma gangrenosum can occur in healthy patients without bacteremia.
Keywords: Ecthyma, ecthyma gangrenosum, Pseudomonas aeruginosa
INTRODUCTION
Ecthyma gangrenosum (EG) is a rare skin infection caused by Pseudomonas aeruginosa. EG is usually seen in immunocompromised and critically ill patients.[1,2] Almost all EG lesions occur in patients with pseudomonas sepsis.[3,4,5] It has rarely been reported in the absence of sepsis or among healthy subjects.[6,7] The characteristic lesions of EG are hemorrhagic vesicles and pustules that evolve into necrotic ulcers surrounded by a tender erythematous border.[3,6] We herein present a case of EG in a previously healthy young male.
CASE REPORT
A previously healthy 20-year old male soldier was admitted with fever and painful wounds over his sternum, right leg and left arm since three days. He also had swelling, redness and pain over his left eye. Four days prior he underwent a dental filling procedure after which flurbiprofen was prescribed. One day later he had fever along with reddish skin lesions and painful swelling around his left eye. Within 24 hours, the reddish lesions progressively developed a central black hue without suppuration. He had no history of immunosuppressive disease in the past or any drug intake other than flurbiprofen. On admission he was febrile and physical examination revealed oral aphthous ulcers, left periorbital swelling and redness, and multiple, tender, necrotic lesions surrounded by erythema over the chest, right leg, and right arm. The largest lesion was 5 × 4 cm in diameter. The skin lesions were accompanied by fever till the fourth day of admission [Figures 1 and 2]. Investigations revealed leukopenia (910/µL; normal range, 3700 to 9700/µL) with severe neutropenia (neutrophil count, 50/µL; normal range, 2000 to 6700/µL). The hemoglobin level was 13.8 g/dL and the platelet count was 228000/mm3. His inflammatory markers were elevated: C-reactive protein 135 mg/dL (normal range, 0 to 3.5 mg/L) and erythrocyte sedimentation rate 83 mm/hr (normal range, 0 to 10 mm/hr). All other biochemical parameters were in the normal range. Blood and urine cultures, wound aspiration culture and skin biopsy were performed. While the results of cultures were pending antibiotic therapy with piperacillin tazobactam (4.5 g every 8 hours) was initiated. Chest radiography was normal. Transthoracic echocardiographic examination was normal, hence the formation of septic emboli due to endocardial vegetations was ruled out. Orbital magnetic resonance imaging revealed increased diffuse contrast enhancement in the left periorbital soft tissues. Bone marrow biopsy revealed hypocellularity of the marrow without blast cells. Serology for HIV was negative by ELISA. Skin biopsy revealed inflammatory cell infiltration, vascular proliferation and extensive keratinocyte necrosis. Repeated blood and urine cultures remained sterile but wound aspiration cultures yielded P.aeruginosa, sensitive to all antibiotics. Based on the clinical and laboratory inputs, a diagnosis of EG associated with P.aeruginosa was made [Figure 3]. Fever resolved completely after 72 hours of initiation of therapy. Neutropenia resolved by the seventh day of therapy. Two weeks later, skin lesions and periorbital cellulitis healed completely.
Figure 1.

Necrotic skin lesions due to Pseudomonas aeruginosa
Figure 2.

Multiple Ecthyma gangrenosum lesions
Figure 3.
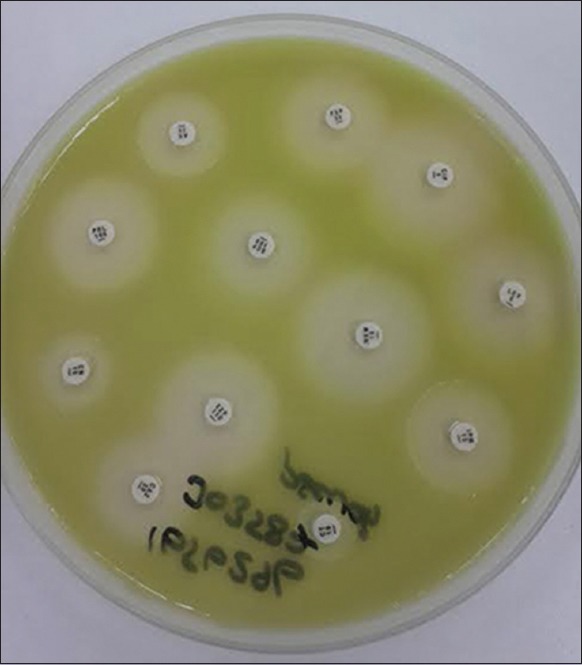
Antibiotic susceptibility of Pseudomonas aeruginosa
DISCUSSION
EG is a characteristic necrotic skin lesion generally associated with P.aeruginosa sepsis and bacteremia in immunocompromised patients. It may also occur in patients without underlying immunodeficiencies.[3,4,5,6,7] Our previously healthy patient presented with multiple EG lesions in the absence of bacteremia. EG sometimes may be the initial manifestation of primary immunodeficiency and also P. aeruginosa sepsis in previously well patients.[4,5] However, repeated blood cultures of our patient were sterile. It has been recommended in the literature that such patients with EG should be investigated for previously undetected immunodeficiencies or transient risk factors.[7]
Definite resolution of neutropenia was achieved in our patient without the use of granulocyte colony sitimulating factor. Evaluation of bone marrow biopsy and serological assay revealed no evidence of any immunosupressive condition. Although there was no prior history or signs of viral infection in our patient at presentation, EG associated with transient severe neutropenia caused by influenza B infection has been reported.[6]
We were unable to pinpoint the exact cause of transient neutropenia. However, NSAIDs in some rare instances may cause bone marrow suppression.[8] The prior use of NSAID in our case could be the possible cause of neutropenia. One case of EG due to diclofenac-induced neutropenia has been reported in the literature.[9]
EG results from perivascular bacterial invasion of skin blood vessels and resultant ischemic skin necrosis. Though EG is commonly caused by P. aeruginosa infection, it has been observed in patients infected with other agents.[10] The lesions of ecthyma gangrenosum commonly begin as painless red macules that develop into pustules, bullae, or crusted ulcers surrounded by a raised erythematous margin that become gangrenous ulcers within 12 to 18 hours. Lesions may be single or multiple and they may be in different stages of development as in our case [Figures 1 and 2]. The presence of the typical lesions of EG usually indicates P. aeruginosa infection however many different organisms can cause EG.[8] Cultures of blood, tissue and exudates from the lesion could identify the causative pathogen. The absence of growth on blood and wound exudate cultures does not rule out the diagnosis of ecthyma. When both cultures are negative histopathological examinaton should be performed.
CONCLUSION
Lesions of EG should be rapidly diagnosed by their characteristic morphology so as to avoid complications. Empiric antimicrobial therapy for EG should include an agent with activity against pseudomonas.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Fink M, Conrad D, Matthews M, Browning JC. Primary ecthyma gangrenosum as a presenting sign of leukemia in a child. Dermatol Online J. 2012;18:3. [PubMed] [Google Scholar]
- 2.Kryeziu E, Kryeziu K, Bajraktari G, Abazi M, Zylfiu B, Rudhani I, et al. Ecthyma gangrenosum in a patient with acute leukemia. Med Arh. 2010;64:373–4. [PubMed] [Google Scholar]
- 3.Koo SH, Lee JH, Shin H, Lee JI. Ecthyma gangrenosum in a previously healthy infant. Arch Plast Surg. 2012;39:673–5. doi: 10.5999/aps.2012.39.6.673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yan W, Li W, Mu C, Wang L. Ecthyma gangrenosum and multiple nodules: Cutaneous manifestations of Pseudomonas aeruginosa sepsis in a previously healthy infant. Pediatr Dermatol. 2011;28:204–5. doi: 10.1111/j.1525-1470.2011.01386.x. [DOI] [PubMed] [Google Scholar]
- 5.Baro M, Marín EM, Ruiz-Contreras J, de Miguel SF, Sánchez-Díaz I. Pseudomonas aeruginosa sepsis and ecthyma gangrenosum as initial manifestations of primary immunodeficiency. Eur J Pediatr. 2004;163:173–4. doi: 10.1007/s00431-003-1381-x. [DOI] [PubMed] [Google Scholar]
- 6.Goolamali SI, Fogo A, Killian L, Shaikh H, Brathwaite N, Ford-Adams M, et al. Ecthyma gangrenosum: An important feature of pseudomonal sepsis in a previously well child. Clin Exp Dermatol. 2009;34:e180–2. doi: 10.1111/j.1365-2230.2008.03020.x. [DOI] [PubMed] [Google Scholar]
- 7.Mull CC, Scarfone RJ, Conway D. Ecthyma gangrenosum as a manifestation of Pseudomonas sepsis in a previously healthy child. Ann Emerg Med. 2000;36:383–7. doi: 10.1067/mem.2000.110013. [DOI] [PubMed] [Google Scholar]
- 8.Cramer RL, Aboko-Cole VC, Gualtieri RJ. Agranulocytosis associated with etodolac. Ann Pharmacother. 1994;28:458–60. doi: 10.1177/106002809402800406. [DOI] [PubMed] [Google Scholar]
- 9.Fairhurst DA, Pollock B. Ecthyma gangrenosum presenting in diclofenac induced neutropenia. J Eur Acad Dermatol Venereol. 2006;20:868–9. doi: 10.1111/j.1468-3083.2006.01544.x. [DOI] [PubMed] [Google Scholar]
- 10.Reich HL, Williams Fadeyi D, Naik NS, Honig PJ, Yan AC. Nonpseudomonal ecthma gangrenosum. J Am Acad Dermatol. 2004;50(Suppl):S114–7. doi: 10.1016/j.jaad.2003.09.019. [DOI] [PubMed] [Google Scholar]


