Sir,
Phaeohyphomycosis (PH) are a rare group of heterogenous dematiaceous (phaeoid) brown pigment producing fungi, which cause superficial, cutaneous, and subcutaneous infections in the immunocompetent and systemic illness, especially brain abscesses in the immunosuppressed.[1,2] A myriad of fungal species causes this unique infection, which includes Exophiala, Phialophora, Cladosporium, Wangiella, Fonsacaea, Alternaria, Bipolaris, and Curvularia species.[3] The usual source of infection is usually exogenous, following pricks with thorns or wood splinters. A 27-year-old man, a renal transplant recipient two years ago and currently on prednisolone and mycophenolate mofetil presented with a nodulocystic lesion on right forearm of five months duration. The lesion first started as a small, tender, erythematous papule on the right forearm and gradually over a period of five months attained the present size. The patient denied prior trauma at the site of the lesion. On examination, the patient had an ill-defined skin-colored nontender nodulocystic lesion of about 3 × 4 cm on the right forearm [Figure 1]. The lesion was more prominent on palpation and had a soft cystic consistency.
Figure 1.
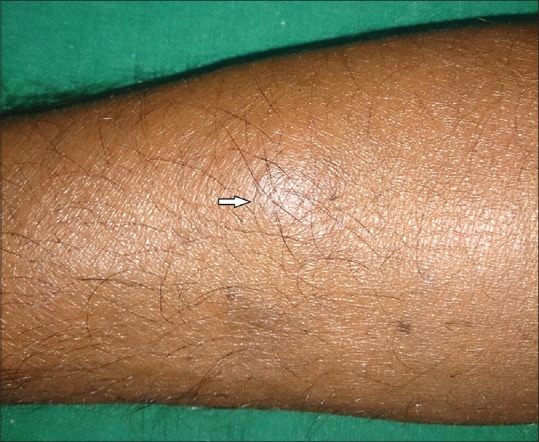
Nodulocystic lesion on right forearm (arrow) better felt than seen
The patient's blood hemogram, biochemistry, blood sugar, and liver and renal function tests, were within normal limits and serological tests for HIV 1 and 2 were negative. Chest X-ray was normal. A fine-needle aspiration cytology (FNAC) of the lesion demonstrated histiocytes, neutrophils, and thick-walled septate spores and pigmented branching hyphae suggestive of a subcutaneous fungal infection [Figure 2]. An excision biopsy of the nodulo-cystic lesion was performed. Hematoxylin and eosin (H and E)-stained sections of the tissue showed a gross inflammatory cell infiltrate extending throughout the dermis to the subcutaneous tissue, composed of histiocytes, neutrophilic abscesses, foreign body giant cells, and thick-walled septate fungal bodies and pigmented hyphae [Figure 3]. Some of the fungal elements were seen within the giant cells and had a beaded appearance [Figure 4]. Gomori's silver methenamine stain (GMS) highlighted the fungal bodies [Figure 5]. A fungal culture revealed mixed growth. A final diagnosis of subcutaneous phaeohyphomycosis was made. The patient was started on itraconazole 100 mg twice daily.
Figure 2.
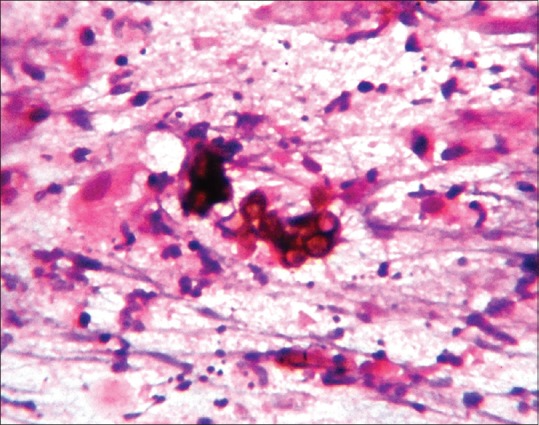
Fine-needle aspiration cytology showing thick-walled fungal spores and pigmented hyphae, Papanicolau ×400
Figure 3.
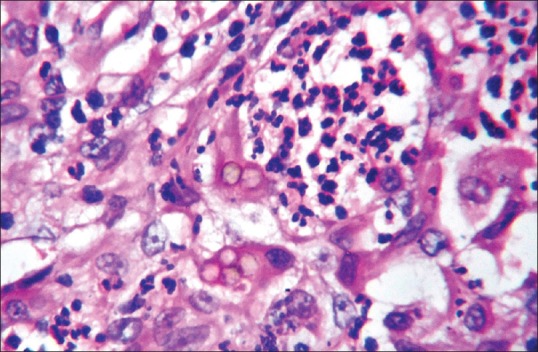
Histiocytes, neutrophilic abscess, and thick-walled brown fungal bodies, H and E ×400
Figure 4.
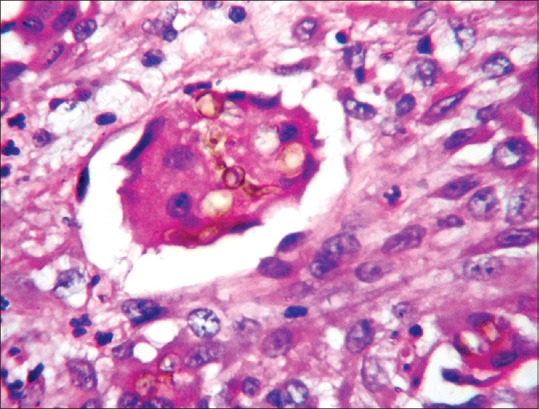
Fungal bodies, pigmented hyphae with beading in giant cells, H and E ×400
Figure 5.

Thick-walled fungal bodies with beading and hyphae, Gomori's methenamine silver ×400
Classical presentation with a nodulocystic lesion, presence of fungal elements in the FNAC, H and E-stained sections showing the presence of brown thick-walled fungal bodies, and typical beaded pigmented hyphae among the infiltrate and giant cells confirmed as fungal elements by GMS stain enabled us to make a diagnosis of subcutaneous PH, although the fungal culture showed mixed growth by contaminants. One interesting feature in our case was the presentation as a solitary lesion instead of dissemination, in spite of immunosuppresion. Beading of the fungal elements as seen in our case is a very important histological clue for the diagnosis of PH [Figure 4]. In addition to the aforementioned histomorphological features, PH may sometimes show a large cystic space surrounded by a fibrous capsule, the cavity showing necrotic material, neutrophils, fibrin, and the fungal bodies. This is termed as the “phaeomycotic cyst.”[4] The unique feature of PH is its ability to cause infection both in the immunocompetent and the immunosuppressed.
The best treatment modality for solitary lesions is complete excision followed by itraconazole 100 mg twice daily.[5] In immunosuppressed patients and in disseminated lesions, long-term itraconazole, fluconazole, terbinafine, amphotericin-B, and 5-fluocytosine are effective. In resistant cases, voriconazole and posaconazole can be tried.[6]
We report this case to highlight a rare mycotic infection occurring in an immunosuppressed patient presenting as a solitary lesion, rather than disseminated lesions and the role of a simple diagnostic tool such as the FNAC for its diagnosis.
REFERENCES
- 1.Singal A, Pandhi D, Bhattacharya SN, Das S, Aggarwal S, Mishra K. Pheohyphomycosis caused by Exophiala spinifera: A rare occurrence. Int J Dermatol. 2008;47:44–7. doi: 10.1111/j.1365-4632.2007.03430.x. [DOI] [PubMed] [Google Scholar]
- 2.Pereira RR, Nayak CS, Deshpande SD, Bhatt KD, Khatu SS, Dhurat RS. Subcutaneous phaeohyphomycosis caused by Cladophialophora boppii. Indian J Dermatol Venereol Leprol. 2010;76:695–8. doi: 10.4103/0378-6323.72474. [DOI] [PubMed] [Google Scholar]
- 3.Revankar SG. Dematiaceous fungi. Mycoses. 2007;50:91–101. doi: 10.1111/j.1439-0507.2006.01331.x. [DOI] [PubMed] [Google Scholar]
- 4.Sheikh SS, Amr SS. Mycotic cysts: Report of 21 cases including eight pheomycotic cysts from Saudi Arabia. Int J Dermatol. 2007;46:388–92. doi: 10.1111/j.1365-4632.2007.03179.x. [DOI] [PubMed] [Google Scholar]
- 5.Sharkey PK, Graybill JR, Rinaldi MG, Stevens DA, Tucker RM, Peterie JD, et al. Itraconazole treatment of phaeohyphomycosis. J Am Acad Dermatol. 1990;23:577–86. doi: 10.1016/0190-9622(90)70259-k. [DOI] [PubMed] [Google Scholar]
- 6.Hossain MA, Ghannoum MA. New investigational antifungal agents for treating invasive fungal infections. Exp Opin Invest Drugs. 2000;9:1797–813. doi: 10.1517/13543784.9.8.1797. [DOI] [PubMed] [Google Scholar]


