Abstract
Hashimoto’s thyroiditis (HT) usually presents as painless thyroid swelling. Painful pediatric HT is a rare condition with limited literature on pain management. We report a 15-year-old female who presented with 4 weeks history of fatigue, malaise and progressive, painful midline thyroid swelling. There was no difficulty in swallowing, no fever or recent upper respiratory infection symptoms. Exam was remarkable for diffusely enlarged, very tender, and non-nodular thyroid. Thyroid function tests, C-reactive protein, and complete blood count were normal. Ultrasound revealed diffusely enlarged non-nodular, non-cystic gland with mild increased vascularity. Diagnosis of HT was confirmed by biopsy and thyroid antibodies. Over a 6 week period, pain management with ibuprofen, levothyroxine, corticosteroid, gabapentin and amitriptyline was unsuccessful. Ultimately, total thyroidectomy resulted in complete resolution of thyroid pain. We can conclude that thyroidectomy may be considered for the rare case of painful HT in children.
Key words: Painful goiter, pediatric Hashimoto’s thyroiditis, pain management
Case Report
A 15-year-old caucasian female presented to the pediatric emergency room with 4 weeks history of fatigue, malaise and progressive painful midline neck swelling without any difficulty in swallowing. There was no history of fever or recent upper respiratory infection (URI) symptoms. There was no previous history of thyroid disease or head and neck irradiation and trauma. The patient’s physical revealed pulse rate of 84/min, blood pressure of 112/65 mm of Hg, temperature of 98.5 F and weight of 72.2 kg, with a body mass index of 28 kg/m2. The oropharynx was normal. Thyroid gland was enlarged, tender, and non-nodular. There was no cervical lymphadenopathy. The trachea was in the midline. Examination of heart, lungs, abdomen and extremities was normal. There was no tremor and the skin was not warm and moist. Thyroid function tests (TFTs) revealed FT4 1.00 ng/dL (0.79-1.50) and TSH 1.54 UIU/mL (0.36-3.74). Complete blood count (CBC) and differential were normal. Erythrocyte sedimentation rate (ESR) was 6 mm/hr (0-20). Thyroid ultrasound (Figure 1) showed diffuse enlargement of thyroid gland with right lobe measuring 2.3×5.6×1.2 cm and left lobe measuring 1.8×5.6×1.4 cm with thickened isthmus of approximately 7 mm. There was nonspecific heterogeneity throughout the parenchyma of gland with no dominant nodule or cyst. Power Doppler imaging revealed mild increased vascularity throughout the gland. We made a preliminary diagnosis of subacute thyroiditis (SAT) and patient was started on ibuprofen 650 mg bid.
Figure 1.
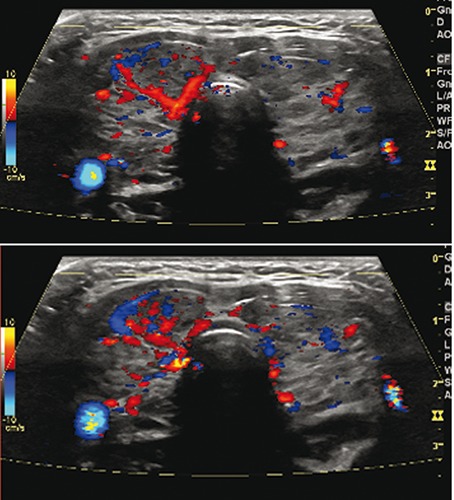
Thyroid ultrasound.
Hospital/outpatient course
She was not improving after 10 days. Anti-thyroperoxidase and anti-thyroglobulin antibodies were 281 IU/mL (<9.0), and 69 IU/mL (<2.0) respectively. Fine Needle Aspiration biopsy (FNAB) showed lymphocytic thyroiditis (Figure 2). Repeated TFTs were normal. By the third week, there was no improvement in pain. Ibuprofen was increased to 400 mg QID (four times daily), prednisone 2 mg/kg/day and levothyroxine 100 mcg/day were added. By the fourth week, we added gabapentin 300 mg TID (three times daily), increased dose of levothyroxine to 112 mcg/day and discontinued prednisone. By the fifth week, TFTs showed suppressed TSH of 0.04 UIU/mL and FT4 of 1.42 ng/dL, levothyroxine dose was reduced to 75 mcg/day and acetaminophen 500 mg BID (twice daily) was added. By the sixth week, there was no improvement in pain. Gabapentin was increased to 600 mg TID and amitriptyline 25 mg daily was started. She developed a skin rash. After 6 weeks of combined medical therapy, the patient’s pain was not improving and she was missing school due to pain. We then decided to perform total thyroidectomy on the seventh week, which resulted in complete disappearance of pain. Post-surgical thyroid biopsy specimen further confirmed Hashimoto’s thyroiditis (HT).
Figure 2.
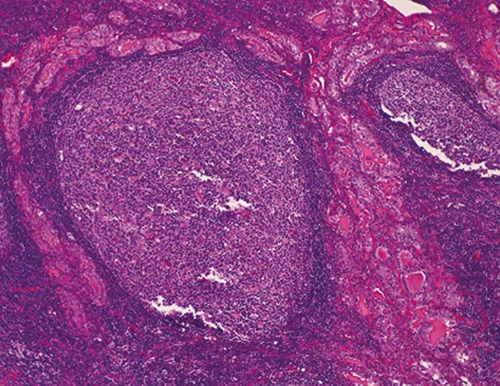
Histological finding: lymphocytic infiltration of thyroid gland.
Final diagnosis: Hashimoto’s thyroiditis.
Discussion
Hashimoto’s thyroiditis is an autoimmune disease that usually presents as non-tender diffuse goiter. It is more common in women than men. Few cases of painful HT have been reported in adult literature.1,2 To the best of our knowledge, we report the first case of pediatric painful HT including its diagnostic and management challenges.
Differential diagnosis of painful enlarged thyroid includes most commonly subacute thyroiditis hemorrhage into thyroid cyst, invasive fibrous thyroiditis, radiation thyroiditis, primary or metastatic thyroid malignancy and other inflammatory or infectious causes of thyroiditis.3-6 It is very important to distinguish between SAT and HT because clinical course, treatment options and responses may be different. SAT usually presents painful goiter while HT as painless goiter. There may be history of preceding URI in subacute thyroiditis. CRP and ESR are usually elevated in SAT and normal or elevated in HT. Biopsy shows fibrosis and lymphocytes in HT while Giant cells and polymorphs are diagnostic findings in SAT. Our patient complained of a severe-painful thyroid gland for the duration of one month with prior history normal thyroid gland function. We therefore considered SAT as possible initial diagnosis but finally proven to be HT by biopsy. Etiology of thyroid pain is unknown with some studies suggesting the role of capsular distension with rapid thyroid growth while others suggesting inflammation and various cellular and humoral immune factors as a possible mechanism. Various medical therapies with aspirin, levothyroxine, propranolol, thiamazole, and corticosteroid have been tried with variable pain relief.3 Gabapentin possess antihyperalgesia and antiallodynia properties and has been shown to reduce acute postoperative pain in patients undergoing thyroidectomy.3,5 In our patient there was no improvement with medical therapy for 6 weeks. She became pain free only after total thyroidectomy. Similar results have been reported in adult literatures.1,2,7
Conclusions
Hashimoto’s thyroditis should be considered as one possible differential diagnosis of painful thyroid gland if there is no resolution of pain with analgesic therapy. Thyroid antibodies and family history of autoimmune thyroid history are important clues in differentiating from subacute thyroiditis. Biopsy is a diagnostic procedure in differentiating two conditions. If medical therapy fails in resolution of pain, total thyroidectomy could be considered by experienced pediatric surgeon.
References
- 1.Kon YC, DeGroot LJ. Painful Hashimoto’s thyroiditis as an indication for thyroidectomy: clinical characteristics and outcome in seven patients. J Clin Endocrinol Metab 2003;88:2667-72. [DOI] [PubMed] [Google Scholar]
- 2.Zimmerman RS, Brennan MD, McConahey WM, et al. Hashimoto’s thyroiditis. An uncommon cause of painful thyroid unresponsive to corticosteroid therapy. Ann Intern Med 1986;104:355-7. [DOI] [PubMed] [Google Scholar]
- 3.Kubota S, Nishihara E, Kudo T, et al. Initial treatment with 15 mg of prednisolone daily is sufficient for most patients with subacute thyroiditis in Japan. Thyroid 2013;23:269-72. [DOI] [PubMed] [Google Scholar]
- 4.Levine SN. Current concepts of thyroiditis. Arch Intern Med 1983;143:1952-6. [PubMed] [Google Scholar]
- 5.Ohye H, Fukata S, Kubota S, et al. Successful treatment for recurrent painful Hashimoto’s thyroiditis by total thyroidectomy. Thyroid 2005;15:340-5. [DOI] [PubMed] [Google Scholar]
- 6.Kasagi K. Painful Hashimoto’s thyroiditis. Intern Med 2006;45:351-2. [DOI] [PubMed] [Google Scholar]
- 7.Konno S, Konno N, Yokobori M, et al. Autoimmune thyroid disease accompanied by recurring episodes of painful thyroid ameliorated by thyroidectomy. J Endocrinol Invest 2002;25:996-1000. [DOI] [PubMed] [Google Scholar]


