To the Editor
Parathyroidectomy can be difficult, with poor outcomes if abnormal parathyroid tissue is not fully resected or if critical neck structures, such as the recurrent laryngeal nerves, are injured during surgery. Complications may be more common in patients undergoing second surgeries, since scarring in the central neck can obscure anatomical landmarks, and in those with aberrant anatomy. We now report the use of intraoperative magnetic resonance imaging (MRI) integrated with real-time navigation to guide parathyroidectomy.
Five patients with primary hyperparathyroidism underwent intraoperative MRI to localize the parathyroid adenoma and recurrent laryngeal nerve for subsequent parathyroidectomy in an advanced multimodality image-guided operating (AMIGO) suite (Fig. 1).1 Fiducial markers were placed on the patient, around the surgical site. The MRI consisted of T1-weighted VIBE (volumetric interpolated breath-hold examination) sequences, T2-weighted BLADE (proprietary name for periodically rotated overlapping parallel lines with enhanced reconstruction [PROPELLER]) sequences, and T2-weighted TSE (turbo spin echo) sequences. Using semiautomatic segmentation techniques, we created three-dimensional patient-specific models of the skin, trachea, carotid artery, thyroid, and parathyroid adenoma in the open-source software 3D Slicer.2,3 We used a modified Bovie pencil that was fitted with an electromagnetic position sensor as a localization probe to assess the position of each structure in three-dimensional space. We developed a navigation software module in 3D Slicer, called EndoscopyNavigation, to track the instrument in real time and to display the instrument with virtual three-dimensional models.
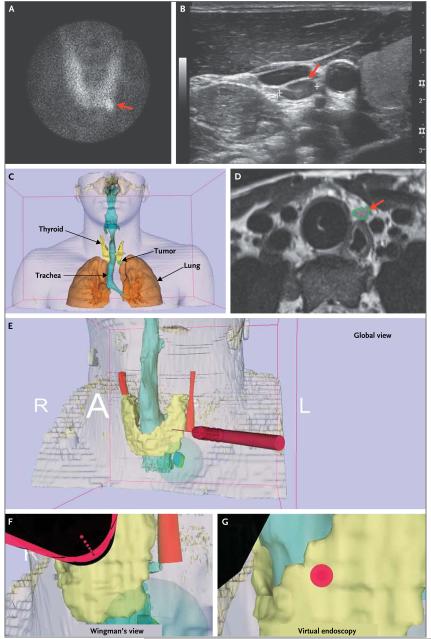
Figure 1. Intraoperative MRI Integrated with Real-Time Navigation to Guide Parathyroidectomy.
Technetium-99m–labeled sestamibi imaging shows an abnormal tracer uptake, indicating a suspected lesion (Panel A, arrow), as confirmed on ultrasonography (Panel B, arrow). A three-dimensional model generated from preoperative computed tomography shows the anterior view (Panel C), with the parathyroid adenoma clearly visible on intraoperative MRI (Panel D, arrow). The navigation system shows the global view of the surgical instrument (red cylinder) with respect to the neck anatomy, with skin indicated in orange, trachea in aqua, thyroid in yellow, and tumor in green (deformed by tissue manipulation during surgery) and blue (undeformed) (Panel E). The Wingman’s view shows the instrument tip and the surrounding anatomy (Panel F), and virtual endoscopy shows the view from the instrument tip (Panel G).
Using the imaging fiducial markers, we mapped the electromagnetic-tracker space to the image space (see the video, available with the full text of this letter at NEJM.org). The displays were arranged so that the surgeon could visualize the instrument and the surrounding anatomy simultaneously. Thereafter, the thyroid edge, trachea, and parathyroid adenoma were localized with the use of the probe, and their position was mapped to the image space. We calculated the target-registration error for the navigation system, which was defined as the difference in three-dimensional space between the position of seven distinct points on the patient mapped to the image space and their corresponding position on the intraoperative MRI. We computed the minimum distance between the localization probe and the various structures to evaluate the accuracy of the localization.
For the five patients, the mean (±SD) target-registration error was 3.1±0.3 mm. The minimum distance from the probe was 1.26 mm to the thyroid edge, 0.64 mm to the trachea, and 0.31 mm to the parathyroid adenoma. All parathyroid adenomas were successfully resected, and there were no recurrent laryngeal-nerve palsies or postoperative neck hematomas. In all five patients, postoperative normalization of calcium levels was confirmed.
Thus, the use of intraoperative MRI in conjunction with a navigation system might be a useful tool in the intraoperative identification of parathyroid adenomas. Such a procedure is particularly useful if the glands are ectopic or if a patient has undergone previous surgeries.
Acknowledgments
Supported by grants from the National Center for Research Resources and the National Institute of Biomedical Imaging and Bioengineering of the National Institutes of Health (P41EB015898 and P41RR019703).
Footnotes
Disclosure forms provided by the authors are available with the full text of this letter at NEJM.org.
References
- 1.Advanced multimodality image-guided operating suite (AMIGO) 2012 https://www.youtube.com/watch?v=LcZBc_po9yQ.
- 2.Fedorov A, Beichel R, Kalpathy-Cramer J, et al. 3D Slicer as an image computing platform for the Quantitative Imaging Network. Magn Reson Imaging. 2012;30:1323–41. doi: 10.1016/j.mri.2012.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.D’Agostino J, Diana M, Vix M, Soler L, Marescaux J. Three-dimensional virtual neck exploration before parathyroidectomy. N Engl J Med. 2012;367:1072–3. doi: 10.1056/NEJMc1201488. [DOI] [PubMed] [Google Scholar]