Abstract
The prevalence of childhood overweight and obesity has risen substantially worldwide in less than one generation. In the USA, the average weight of a child has risen by more than 5 kg within three decades, to a point where a third of the country’s children are overweight or obese. Some low-income and middle-income countries have reported similar or more rapid rises in child obesity, despite continuing high levels of undernutrition. Nutrition policies to tackle child obesity need to promote healthy growth and household nutrition security and protect children from inducements to be inactive or to overconsume foods of poor nutritional quality. The promotion of energy-rich and nutrient-poor products will encourage rapid weight gain in early childhood and exacerbate risk factors for chronic disease in all children, especially those showing poor linear growth. Whereas much public health effort has been expended to restrict the adverse marketing of breastmilk substitutes, similar effort now needs to be expanded and strengthened to protect older children from increasingly sophisticated marketing of sedentary activities and energy-dense, nutrient-poor foods and beverages. To meet this challenge, the governance of food supply and food markets should be improved and commercial activities subordinated to protect and promote children’s health.
Introduction
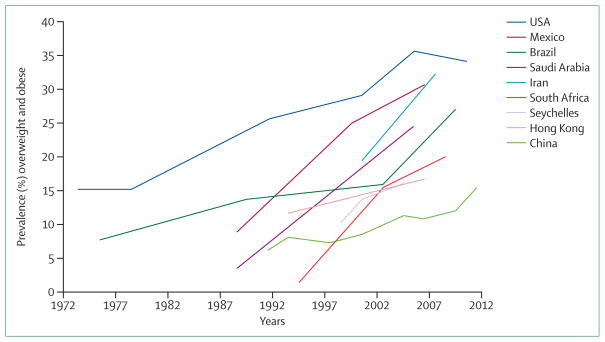
In the past three decades, child overweight and obesity prevalence has risen substantially in most high-income countries and, from the scarce data available, seems to be rising rapidly in low-income and middle-income countries. Although data for children aged younger than 5 years have been collected in large surveys in many countries, surveys of older children and adolescents are less common, and sample sizes tend to be smaller. Nonetheless, results of comparable surveys separated by half a decade or more show that the prevalence of overweight in these children is increasing rapidly. Figure 1 shows the prevalence of overweight (including obesity) in children in the USA and several low-income and middle-income countries. In general, the prevalence of overweight has increased in the past four decades, but with later onset, and in some cases much more rapid increase in prevalence, in several low-income and middle-income countries.
Figure 1. Prevalence trends for child overweight and obesity in the USA and eight low-income and middle-income countries.
Source: World Obesity Federation, collated from published sources. Further details in appendix. Measurements of body-mass index are based on professionally measured heights and weights.
Although the rise in obesity prevalence in several high-income countries might be reaching a plateau, prevalence remains historically high and is still a so-called time bomb1 for future demands on health services. To “halt the rise in diabetes and obesity”2 in adults and children was one of the global health targets set by the World Health Assembly in 2013.2
Key messages.
Monitoring of child growth in many low-income and middle-income countries shows rising levels of overweight, but the policy response remains slow
The continuing problem of growth retardation and stunting coincides with, and might in part contribute to, the rising prevalence of obesity in these countries
Strategies to tackle obesity need to avoid increasing the risk of undernourishment; a so-called healthy growth strategy is needed
Nutrition security in childhood includes the provision of a supply of healthy foods and assurance that children’s consumption of health foods is not jeopardised by the promotion of competing and less nutritious products
Agriculture, food supply, and food environment targets are needed in order to improve nutritional health; increased involvement of governments will be needed to achieve such targets
Child obesity prevention
Much research has been devoted to finding successful interventions that can prevent obesity in children. A PubMed search showed that the number of published papers on child obesity prevention rose from about 20 per year in the late 1980s, to 60 per year in the late 1990s, and to more than 1000 in 2013 alone. Few of these papers are reports of actual intervention studies: a 2013 systematic review3 found 124 childhood obesity prevention studies in school, home, community, child care, primary care, and multiple other settings in high-income countries. Most existing studies were school-based, and the review called for further research to test interventions in other settings and to test more comprehensive and systems-oriented approaches.
These and other reviews generally suggest that, rather than single-component interventions, the most sustainable and beneficial effect on obesity prevention involves multiple strategies that focus on meals, classroom activities, sports, and play activities, and involve home, school or kindergarten, and community participants.3–6 This conclusion should be no surprise: the more an environment consistently promotes healthy behaviour, the greater the likelihood that such behaviour will occur. However, reviewers also warn that interventions might not translate from one environment to another or across culturally diverse groups, and inequalities in outcomes might widen the existing differences in health status.7,8 Furthermore, as pointed out by Huang and colleagues9 in this Series, both a strengthened evidence base for community interventions at the local and intermediate levels (in towns and cities) and an analysis of the effectiveness of activities that empower communities to build health-promoting communities are needed.9
Notably, most intervention studies have been done in Asia, Australia, Europe, or North America, and the most common settings for controlled interventions are in schools where the experimental designs can ensure a degree of scientific validity to the results. However, this focus on schools creates a strong settings bias in the scientific literature.10 Additionally, the scarcity of well documented, effective interventions in low-income and middle-income countries creates a substantial limitation to the evidence.
From a policy-making perspective, the dearth of societal policies for childhood obesity prevention is noticeable, and corresponding assessment of such interventions in the literature is absent. Furthermore, of all reported intervention studies, only a few studies describe the probable costs of scaling up the intervention, despite such costs being a key issue for policy makers seeking policies and programmes to prevent child obesity.
Cost-effectiveness of child obesity prevention
The question of costs, or value for money, in obesity prevention is particularly relevant to policy makers and service providers concerned with the best use of resources,11 and cost estimates should be reported from intervention trials routinely. Only a few studies have estimated the likely cost-effectiveness (ie, the costs regarded acceptable for the benefits gained) of an intervention, perhaps in part because of the small number of obesity interventions for which there is strong evidence of effectiveness, and in part because of the complexity of the assumptions and associated uncertainty in translating behaviour change into improved body-mass index (BMI) and BMI into disability-adjusted life-years (DALYs) or other long-term health benefits for which costs can be assessed.12
Studies providing economic assessment were identified from several recent reviews of childhood obesity interventions13–16 and are listed in the table. Of the 21 economically assessed interventions, six are based in clinical settings with children who are already overweight or obese. Of the remaining interventions, most are focused on school, after-school, or school-community settings, targeting younger (pre-teenage) children. Only one population-wide policy intervention, which reduced television advertisement of unhealthy food for children, is included, and this intervention could potentially affect all children, irrespective of age, gender, or social class and could promote long-term sustainability.17 This intervention and five of the community-based, non-clinical interventions were judged dominant, in that they would result in both health gains and real cost savings to health services or society. 12 other interventions (including seven school-based interventions) were cost effective or deemed as probably cost effective. No cost estimates are available for built environment or town planning interventions, such as safety of neighbourhoods or provision of cycle lanes, although these probably have wider health benefits across a community.
Table.
Cost-effectiveness of childhood obesity prevention interventions
| Country | Setting | Target population | Time horizon | Measure of health gain | Reference | |
|---|---|---|---|---|---|---|
|
Dominant (positive financial benefit and health gain)
| ||||||
| Reduction of advertising of junk food | Australia | Media | Children 0–14 years | 1 year intervention, life-time modelling | Dominant (health gains and financial gains) | Magnus et al 200917 |
| Education programme to reduce sugar sweetened drink consumption | Australia | School | Primary school children 7–11 years | 1 year intervention, life-time modelling | Dominant | Victoria Dept of Human Services18 |
| Multifaceted targeted programme | Australia | School | Overweight or obese primary school children 7–10 years | 1 year intervention, life-time modelling | Dominant | Victoria Dept of Human Services18 |
| Multifaceted programme including nutrition and physical activity | Australia | School | Primary school children 6 years | 1 year intervention, life-time modelling | Dominant | Victoria Dept of Human Services18 |
| Education programme to reduce television viewing | Australia | School | Primary school children 8–10 years | 1 year intervention, life-time modelling | Dominant | Victoria Dept of Human Services18 |
| Family-targeted programme | Australia | Clinical | Obese children 10–11 years | 1 year intervention, life-time modelling | Dominant | Victoria Dept of Human Services18 |
|
| ||||||
|
Likely to be cost effective (financial costs are worthwhile for the health gains)
| ||||||
| Medical College of Georgia FitKid project | USA | School (after hours) | 3rd grade students | 1 year | US$317 per 0·76% reduction in body fat | Wang et al 200819 |
| Be Active Eat Well multifaceted community based programme | Australia | School | Primary school children 5–12 years | 3 year intervention, life time modelling | Net cost per DALY saved AU$29 798 | Moodie et al 2013b20 |
| APPLE multifaceted school-based programme | New Zealand | School | Primary school children 5–12 years | 4 years | NZ$664–1708 per kg of weight gain prevented | McAuley et al 201021 |
| Multifaceted programme excluding nutrition and physical activity | Australia | School | Primary school children 6 years | 1 year intervention, life-time modelling | AU$21 300 per DALY saved | Victoria Dept of Human Services18 |
| Cuenca Study-school-based physical activity programme | Spain | School | Primary school children 9–10 years old | 8 months | €500 saved per 1% decrease in triceps skinfold thickness | Martinez et al 201122 |
| Coordinated Approach to Child Health (CATCH) | USA | School | Children 8–11 years | 3 year intervention, modelling up to age 64 years | US$900 per QALY saved | Brown et al 200723 |
| Planet Health | USA | School | Children 11–14 years | 2 school-years intervention, modelled to age 65 years | US$4035 per QALY saved | Wang et al 200324 |
| Family-based group treatment | Finland | Clinical | Obese children 7–9 years | 6 months | €53 per 1% decrease in weight | Kalavainen et al 200925 |
| Laparoscopic adjustable gastric banding | Australia | Clinical | Severely obese adolescents 14–19 years | 1 year intervention, life-time modelling | AU$4400 per DALY saved | Ananthapavan et al 201026 |
| Family-based GP mediated programme | Australia | Clinical | Overweight or moderately obese children 10–11 years | 1 year intervention, life-time modelling | AU$4700 per DALY saved | Moodie et al 200827 |
| RCT-evaluated lifestyle interventions to treat overweight and obesity | UK | Clinical | Obese children 10–11 years | 1 year intervention, life-time modelling | £13 589 per life-year gained | Hollingworth et al 201228 |
| Family-based group treatment | Canada | Clinical | Children 8–12 years | 20 weeks intervention | Group treatment gave 14% reduction in overweight prevalence per $1000 spent. | Goldfield et al 200129 |
|
| ||||||
|
Unlikely to be cost effective
| ||||||
| Active after-school communities programmeme | Australia | School (after hours) | Primary school children 5–11 years | 1 year intervention, life-time modelling | AU$82 000 per DALY saved | Moodie et al 201030 |
| TravelSMART schools | Australia | Neighbourhood | Primary school children 10–11 years | 1 year intervention, life-time modelling | AU$117 000 per DALY saved | Moodie et al 201131 |
| Walking school bus | Australia | Neighbourhood | Primary school children 5–7 years | 1 year intervention, life-time modelling | AU$760 000 per DALY saved | Moodie et al 200932 |
These estimates regard effectiveness in terms of obesity reduction or change in body-mass index, but not other potential health benefits. DALY=disability-adjusted life-year. GP=general practitioner. RCT=randomised controlled trial. QALY=quality-adjusted life-year.
The investigators of the studies listed in the table estimated the effects of reduced child obesity rates on adult diseases. They did not consider the health benefits that might arise (eg, from increased physical activity or healthy eating) when there is no effect on obesity, and they generally did not include any effect on comorbidities that occur in childhood and adolescence (eg, gastrointestinal, endocrine, or orthopaedic disorders)33 because of the scarcity of reliable epidemiological evidence.34 Furthermore, relative to healthy peers, children who are overweight and obese have significantly lower mean scores of quality of life35,36 and experience a higher degree of social discrimination, which is often associated with poor self-esteem and depression, and, in turn, lower academic achievement and lower economic productivity.37 The methods for translating lost quality of life during childhood into economic evaluations warrant further attention because this will undoubtedly strengthen the economic arguments for intervention. Micromodelling of the effects of intervention could provide a metric for long-term comparisons.38
In summary, the need for action on childhood obesity is supported by strong evidence, and sufficient evidence and logic exists to conclude that all childhood settings can contribute to the creation of healthy environments, improved diet and physical activity patterns, and healthy body size; some of these approaches will be highly cost effective.
Energy balance in childhood
A Cochrane systematic review39 of 55 published interventions to prevent obesity found on average a small but significant (0·5–0·8%) relative reduction in BMI or a 0·2–0·3 kg relative weight reduction during the intervention period (all children are expected to gain weight as they grow, so comparisons must be relative). Whether further relative weight reduction could be achieved by longer interventions is unknown.
How shall such a relative change in weight be assessed, and how large is the achievable magnitude of change (eg, 0·3 kg) compared with the needed magnitude of change? The change needed depends on the target: a reduction of bodyweight from present levels to the levels seen in children a generation or more ago is a plausible target, although rather ambitious, and for this change, some relatively simple calculations can be made. Comparison of bodyweights of children in the USA in the 1976–80 Health and Nutrition Examination Survey40 with those of children in the 2003–06 Health and Nutrition Examination Survey41 shows an increase of about 5·3 kg (varying from about 2 kg in children up to 8 years of age to more than 8 kg in some adolescent age groups). Although an intervention achieving 0·3 kg relative weight reduction can be appreciated as of some value in younger children, a weight reduction of 0·3 kg represents only 3–4% of the average change needed for older children and an even lower percentage if the intervention is targeted at children who are overweight or obese.
Substantial progress has been achieved by Hall and colleagues42 in quantifying energy balance and bodyweight dynamics in adults, and this work has been used to predict bodyweight and body composition dynamics resulting from interventions in adult populations.43,44 The development of similar quantitative models of bodyweight dynamics in childhood is complicated by the processes of growth and development. A recent model that includes growth and development has been published by Hall and colleagues,45 and can be used to calculate the energy balance dynamics for children. Their formulae can be used to estimate the energy intake change that would lead to a relative change in weight at various ages:
Males (7–18 y): daily kcal per kg=68 − 2·5 × Age (y)
Females (7–18 y): daily kcal per kg=62 − 2·2 × Age (y)
From these formulae, a change in relative weight of 0·3 kg can be estimated to result by decreasing the energy intake by around 10–15 kcal per day. The more ambitious target in the USA of reducing bodyweight similar to those of children in the late 1970s would result from a lower average intake of some 190 kcal per day for girls and 210 kcal per day for boys. For interventions targeted at overweight and obese children, the average reduction of energy intake needs to be much larger than that calculated for the general population. For example, an obese girl 10 years of age and whose bodyweight is 20 kg in excess of the 50th centile is probably consuming some 800 kcal per day more than a healthy weight peer.
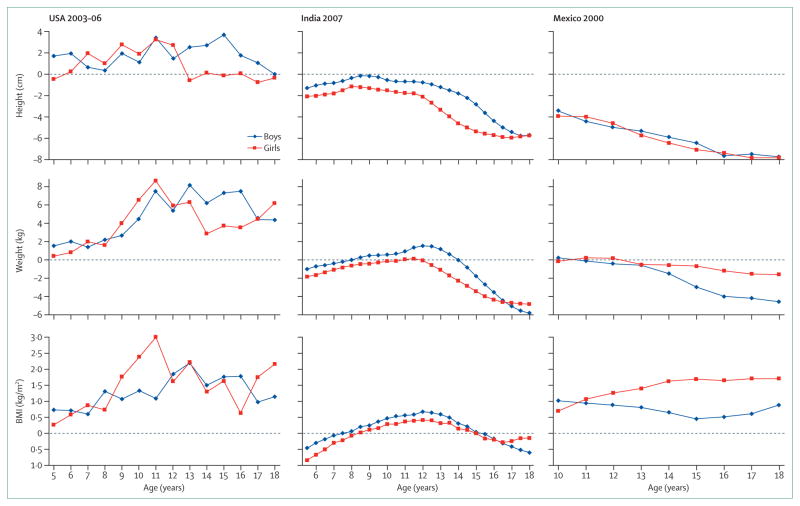
The American 2003–06 data41 were compared with the WHO reference values for child growth.46 WHO’s reference values provide a benchmark for countries that have no historical data of their own. On average, American children were around 4·3 kg heavier than the reference values (appendix). Application of the formulae by Hall and colleagues to these figures gives an estimated energy excess in the range of 160–200 kcal per day in American children compared with WHO’s reference values.
The same analysis was done for children surveyed in urban areas in India in 2007.47 Results of the survey found 18% of girls and 21% of boys to be overweight or obese according to their BMI. Surprisingly, we found an average energy deficit on the basis of the children’s median weights for their age, compared with WHO’s reference values (appendix). Unlike American children, the Indian children’s median weights for age were below the WHO references.
We undertook the same analysis for data from Mexico in 2000,48 a time when 25% of boys and 28% of girls were reported to be overweight or obese, according to their BMI.49 Again, we found an average energy deficit on the basis of the children’s median weights compared with WHO’s reference values. Similar to urban India, the average Mexican child was below a healthy weight for his or her age, despite the widespread prevalence of overweight measured by BMI.
Overweight or underheight?
We were concerned to find such low median bodyweight in samples in which significant proportions of children are reportedly overweight or obese, and therefore took a closer look at the growth patterns among children in the USA, urban India, and Mexico samples, compared with the WHO reference values. Figure 2 shows the age-specific 50th centile for weight, height, and BMI in the surveys sampled in the USA, India, and Mexico, expressed as a difference from the WHO reference values, across the age ranges surveyed. Urban Indian children have height values consistently below the WHO reference throughout childhood (averaging 2·5 cm below reference values), a negative deviation from reference bodyweights (averaging 1·4 kg below reference values) and BMI values slightly above reference values (average 0·04 kg/m2 above reference). Data for Mexico show a similar pattern: children’s heights are consistently well below the WHO reference values (averaging 6 cm below reference), and their weights are also lower than reference values (averaging 1·4 kg below), yet their BMI values are consistently higher than WHO reference values (averaging 1·1 kg/m2 above).
Figure 2. Deviation of height, weight, and body-mass index of children in the USA, urban India, and Mexico from the WHO growth reference values, by age46.
WHO values were sampled at mid-year for whole-year comparisons. WHO weight reference values were calculated from body-mass index values for children older than 10 years. Weight reference values and deviation scores are available in the appendix.
In these cross-sectional surveys, whether differences across age groups are age effects or cohort effects is unclear. Younger cohorts will have been exposed to only the most recent food environments in the rapid economic development and nutrition transition in India and Mexico, whereas their older peers have been exposed to the cumulative effects of changing food environments for a decade or more before the survey. Either way, when discussing overweight and obesity in children (and adults) in low-income and middle-income countries, an apparent increase in prevalence of apparent overweight needs to be recognised as perhaps not entirely due to excess bodyweight per se, but could be confounded by low height for age.
We recognise that an analysis of the 50th centile values might not reflect the true nature of the problem. A genuine problem of rising adiposity might exist, which is measured at the upper centiles of bodyweight and not adequately detected at the 50th centile. Simultaneously, a continuing problem of stunting is occurring, albeit not in the same children. More careful analysis of the original data might reveal separate clusters of children, with one cluster overweight and a separate cluster underheight. However, the evidence suggests that the two clusters are not entirely separate: results of a study50 in Vietnam found that 5% of the overweight children were also stunted, and a study51 in São Paulo, Brazil, found that 6% of children in low-income urban households showed excess bodyweight associated with stunting and that obesity associated with stunting was more common than obesity without stunting, both in younger children and adolescents. Similarly, results of a study52 of young children in urban areas of the Cape Peninsula, South Africa, found coexisting growth retardation and emergent obesity, and the investigators suggested that the community had moved from undernutrition to overnutrition without having achieved optimum nutritional status.
The coexistence of underheight and stunting with overweight and obesity is found not only in low-income and middle-income countries. The National School Measurement Programme in England showed a consistent increase in prevalence of obesity in children living in lower deciles of household deprivation. Repeated analysis53 of height of these same children showed a parallel decline in stature, with higher deprivation associated with lower stature and increased stunting in children age 5–6 years and age 10–11 years, both in the white British as well as some other ethnic groups.
In view of an estimated stunting prevalence of 28% of children younger than 5 years in low-income and middle-income countries in 2011 (down from 32% in 2004)54 and suboptimum linear growth (mild stunting) probably affecting far larger proportions of young people throughout their childhood and adolescence and into adulthood, it is important that policy makers ensure that interventions to reduce obesity are appropriate for the actual nutritional problems they face, rather than tackling excess bodyweight in isolation. Surveys of school children are needed to monitor their growth trends and should preferably use measures of adiposity in addition to BMI.
Nutrition policies to promote healthy growth
Whether or not suboptimum linear growth and overweight occur in the same individual, their coexistence in the same population means that care needs to be taken with nutrition policies and health promotion practices. Consideration of the messages about tackling child obesity given by policy makers, health practitioners, and kindergarten and school professionals is particularly necessary. An emphasis on weight measurement or BMI might mislead parents about the need for healthy growth, including height and muscle mass. Messages that promote the avoidance of excess weight gain might give the impression that children should be restricted in what they eat, rather than encouraged to eat healthily.
Tackling of overweight and underheight simultaneously will need a coherent nutrition policy to promote children’s health and prevent poor nutrition in all its forms. Therefore, the first consideration is to ensure that anti-obesity policies will not have unintended consequences and are appropriate in populations in which there is evidence of deficiency in linear growth as well as rising adiposity. Equally, programmes to remedy undernutrition should not focus too much on weight gain per se, but rather on healthy growth, particularly linear growth, and especially at an early age.55
Findings in systematic reviews and modelling studies56,57 of diets needed for optimum growth in younger children suggest that a key indicator of a healthy diet is diversity, and sources of food rich in animal protein and micronutrients. Dietary diversity reduced the incidence of stunting and improved height-for-age scores in a study58 of more than 18 000 infants in southern India, and similar results are reported for Cambodia,59 where consumption of animal products was also found to be protective.
Nutrient density is an important feature of dietary intake throughout childhood. Although energy demands for children reach adult levels by age 12 years, their needs for nutrients to generate lean body mass, as a proportion of the energy consumed, are higher than those for adults throughout much of childhood and adolescence. Children need nutrient-rich foods rather than high-energy foods.
Policy proposals to reduce child undernutrition are described in many papers, including that by Bhutta and colleagues60 in the recent Lancet Series on maternal and child nutrition. While Bhutta and colleagues correctly identify issues such as “women’s empowerment, agriculture, food systems, education, employment, social protection, and safety nets”,60 we believe that a closer look at the forces shaping food supplies is needed to tackle both undernutrition and overnutrition, both for children less than 5 years old and for children in school. We are particularly concerned that proposals to improve nutrition need to recognise the market forces behind the rapid transition from undernutrition to overnutrition and the products and their producers that shape these markets.61
Governments and development agencies might inadvertently encourage families to become dependent on mass-produced, nutrient-poor foods by encouraging their participation in the marketplace. UNICEF’s retrospective review of nutrition programmes and the Millennium Development Goals62 discusses problems seen in Peru (and likely to be found in many other countries), where ”instead of giving attention to home gardens generally managed by women, small producers are encouraged to sell their produce and purchase foods from the market with the proceeds…the potential diversity that might have been possible through home-produced foods instead becomes sugar and fat-rich processed foods with low nutrient density”. Market-making corporations also need to be held to account: the UNICEF report also notes that, regarding the progressive policies of Brazil, there is a need to recognise that some agribusiness practices ”are clearly at odds with the government’s pro-health, pro-equity and anti-poverty platforms”.62
Food supplies and market controls
Although governments and development agencies tend to focus on promotion and diversification of traditional food production, they usually say little about the threats posed by commercial markets. Experience suggests that the competitive nature of food multinationals and their rapid penetration of low-income and middle-income markets need greater recognition in international aid, development strategies, and national nutrition policies. For example, despite 20 years of public health advocacy, campaigning, and exhortation by non-governmental organisations and the World Health Assembly, breastfeeding and complementary feeding remain under continued threat from major food companies seeking to expand their markets for their formula milks and weaning products.63,64
We fear that the situation relating to breastmilk substitutes is being repeated in the feeding of older children. Campaigns by food companies impair the transfer from breastmilk to family meals by encouraging a transfer from breastmilk to highly processed foods and sweetened beverages, which contain ingredients that condition the taste buds of children to a lifetime of consuming energy-rich and nutrient-poor products.65 Markets for processed infant foods are expected to grow rapidly: sales of dried and ready-to-eat commercial complementary foods are projected to rise worldwide between 2007 and 2015, from US$3·2 billion to $4·9 billion for dried products and from $10·5 billion to $14·1 billion for ready-to-eat products, and with sales in Asian countries expected to triple in value during the same period.66
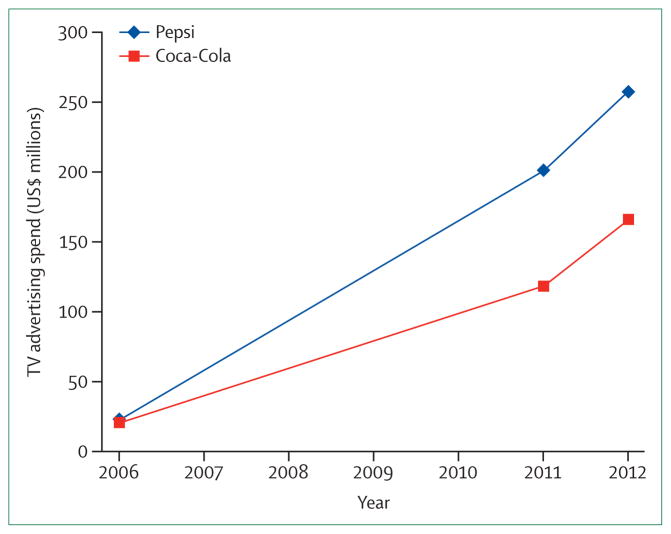
Expansion of the supply of commercially produced complementary foods is matched by the promotion of commercially-branded highly processed foods to older children. Analysis of surveys of advertisements on children’s television in Australia, Europe, and the USA showed high levels of promotion of products such as soft drinks, sweetened cereals, snacks, biscuits, confectionery, and fast-food outlets for several decades,67,68 and advertising is increasingly dominating the media in emerging economies. Evidence from the Middle East suggests that television advertising for food and beverages is led by soft drinks (37%), savoury snacks (24%), confectionery (21%), and fast foods (18%), particularly between 1400–2100 h, when children tend to watch television the most.69 Advertisement expenditure for the two leading soft drinks companies in the region has risen more than ten-fold in 6 years (figure 3).69,70
Figure 3. Television advertising expenditure for the two leading soft drinks companies in the pan-Arab region, 2006–12.
Sources: Pan Arab Research Center 2007 and 2013.
The rise in the promotion of soft drinks shows the forces underlying the nutrition transition; the move from traditional food supplies to food supplies strongly influenced by mass produced, branded, and highly promoted products. The soft drinks sector is especially relevant because these products are closely associated with weight gain in children and adults71 and because the supply is dominated by a few companies. Analysis of data72 collected in 2009 shows that ten soft-drink companies accounted for 52·3% of sales worldwide, with two, The Coca-Cola Company and PepsiCo, accounting for 25·9% and 11·5% of sales, respectively. In comparison, the top ten food companies accounted for 15·2% of packaged food sales worldwide, with each individual company contributing less than 3·3%. Furthermore, whereas sales of soft drinks have been relatively static or declining in many high-income countries in recent years, worldwide sales have been increasing at 3% during 2007–11,73 with much of the increase occurring in low-income and middle-income countries; Brazil has shown 6% annual increases in sales74 and India 7%.75
Food environments and commercial interests
Although we recognise that children need to be encouraged to take plentiful physical activity and reduce their sedentary behaviour, the focus of this Series paper is on nutrition policies and food supplies. We recognise that physical activity in early life can help reduce stunting and encourage healthy linear growth and should be included in national health promotion policies. A Lancet Series on physical activity is available for the interested reader.
The series of papers by Swinburn and colleagues76 for the INFORMAS project and the paper by Roberto and colleagues77 in this Series focus on food environments as a leading factor that drives obesogenic behaviour, and argue for redesigning food choice environments to encourage people to make healthy food choices. As discussed by Hawkes and colleagues78 in this Series, interventions to prevent child obesity need to be broadened to include interventions that change the nature of the food and consumer environment, including the availability, price, and formulation of different types of food products and the marketing practices that influence food choices and preference.
Although parents might be held responsible for their children’s diets, multimillion dollar marketing budgets can readily undermine parental efforts to give their children healthy foods. New digital marketing techniques using social networking software, mobile phone messages, and embedded messages in web-based games and mobile phone apps, give companies access to children without parental oversight.79 Further examples of children’s potential exposure to marketing without parental or school supervision are developing rapidly and include interactive advert creation, behaviour profile capture, e-voucher messaging, and other novel methods to contact and engage children.80
The food industry has a special interest in targeting children. Not only can the companies influence children’s immediate dietary preferences, but they also benefit from building taste preferences and brand loyalty early in life, which last into adulthood. Furthermore, the food and beverage industries as a whole have a financial investment in creating overweight. As discussed earlier, children in the USA are, on average, more than 5 kg heavier than their counterparts 30 years ago, which implies that children today consume more than 200 kcal per day (73 000 kcal per year) more than was consumed by a child in the 1970s. The additional intake of calories is needed to warm, move, and physiologically maintain the additional mass. Average expenditure spent on food per person in the USA in 2011 was $11·59 per day,81 and average food energy intake in 2009–10 was 2081 kcal per day,82 which gives about 56 cents per 100 kcal. Thus an average excess consumption of 200 kcal per day implies purchases of excess food worth on average $1·12 per day, or more than $400 per year per child. With about 50 million school-age children in the USA, the combined value of their excess food consumption each year approaches $20 billion. A high proportion of these children will continue over-consuming through adulthood, creating a market for the US food and beverage industry, which we estimate to be worth considerably more than $60 billion each year.
Economic investments embedded in the creation and perpetuation of sales of food to children suggests that the debate over policies to prevent child obesity is primarily a political argument about competing economic and health interests. Proposals for controlling food environments, and especially food marketplaces, are likely to be strongly resisted, as they have been with alcohol and tobacco policy making.83,84
Nutrition policy, governance and accountability
Several policy tools are available to intervene in markets for better nutrition. These include the setting of specific nutrient standards for products, the use of financial incentives and penalties to encourage reformulation, regulatory oversight of marketing activities, and the use of public-sector purchasing power to affect market prices and distribution. Further examples can be found in policy databases such as the World Cancer Research Fund International NOURISHING framework and WHO’s GINA resources.
However, interventions that affect food markets need political determination to challenge industrial interests, and this will need to be accompanied by approaches to reframe the narrative of responsibility for obesity and the determinants of the food environment.61,84 These tasks are not easy. For example, whereas the need to tackle children’s exposure to advertising from the food industry was recognised in World Health Assembly resolutions and supported by a set of recommendations85 and an implementation framework from WHO,86 few countries have taken regulatory steps to protect children, and most have relied on voluntary moves by food companies, which is not sufficient to accomplish the task.87
We have been in this situation before. Considerable public health effort has been devoted to the defence of breastfeeding and the imposition of restrictions on the promotion of breastmilk substitutes. Implemented partly or fully into law in more than 60 countries, the International Code of Marketing of Breastmilk Substitutes88 is an example of an international and comprehensive attempt to regulate food company marketing behaviour to protect existing highly nutritious food supplies and promote child health. We believe the need to extend this approach and greatly strengthen mechanisms for its implementation to protect the health of children of all ages is urgent. This requires a substantial change in the governance of food supplies, controls on commercial competition, and measures to protect and promote healthy food supplies.
Control of nutrition policy and the food supply is as important for prevention of stunting and short stature as it is for prevention of obesity and chronic disease: an integrated nutrition policy focuses on providing children with the means to achieve optimum growth. To meet nutritional goals, integrated nutrition and health policies need to be translated into food supply targets. Food supply targets cannot be left to the whim of multinational food companies, commodity markets, and speculative financiers, but will need to be kept under tight supervision and regulation. Agricultural production and food supply targets need to be set by international governmental agencies without conflicted economic interests, with independent monitoring, and with the actions of all participants held to account. Left to the market, children’s nutrition security is all too easily undermined (panel).
Panel: Threats to children’s nutrition security.
We define nutrition security as the assured supply, availability, and affordability of adequate food for a healthy diet as well as the consumption of such food, in accordance with recommended food-based dietary guidelines. Such consumption might be jeopardised by an absence of facilities, skills, or knowledge or by persuasive messages and inducements to consume unhealthy products. Policies to ensure children’s optimum growth and development need to focus both on ensuring a supply of healthful foods and that consumption is consistently promoted and fully protected from competing interests.
An example of a threat to children’s food security took place in Egypt, where the prevalence of stunting among children younger than 5 years increased from 23% to 28% in the period 2005–08.89 The growing prevalence of stunting was attributed, in part, to the culling of millions of chickens in response to the avian influenza outbreak in 2006. This eradication especially affected low-income households, where domestic poultry-keeping fell from nearly 100% to less than 60% of households, which, in turn, had a substantial and sustained effect on household consumption of poultry meat and eggs, especially for young children. This situation also reduced household financial resources since poultry sales accounted for a third of income for poorer families.90
Meanwhile, results of a 2011 survey of the health behaviour of teenage children in Egypt indicated that 60% of boys and 51% of girls consume one or more carbonated, sugar-sweetened drinks every day, 87% do not take regular physical activity, and 28% are sedentary for at least three hours per day.91 A third of the teenagers were overweight, according to self-reported heights and weights. Indicators of the national food supply show that the number of McDonald’s outlets has risen from four in 1994 to 56 in 2013, sales of Coca-Cola have increased from 18 portions per person per year in 1992 to 64 portions per person per year in 2012, and regional car ownership and television ownership have doubled in two decades.92
Immediate tasks include the monitoring of children’s nutritional status and growth indicators along with the food environments and commercial food promotion experienced by children in all regions of the world. While data are being collated and assessed, a set of policy measures are needed and are to be led by the development of a strong International Code of Food Marketing to Children, an extension of the Breastmilk Substitutes code. These policy measures are to identify inappropriate marketing of foods for infants and need to be supported by the strengthened health priorities in agriculture and food supply strategies in the post-2015 development agenda. We urge member states to call upon WHO to coordinate the development of these policies and to work with UN agencies to protect and promote nutrition security for all children.
Acknowledgments
The work for this paper was supported by the World Obesity Federation, formerly the International Association for the Study of Obesity (IASO). Additional work was done in part for the Envision Project, supported by the US National Collaborative on Childhood Obesity Research, which coordinates childhood obesity research across the National Institutes of Health (NIH), Centers for Disease Control and Prevention (CDC), US Department of Agriculture, and the Robert Wood Johnson Foundation (RWJF). The work was also supported in part by grants from RWJF (grant 260639), CDC (U48/DP00064) and NIH (1R01HD064685–01A1, U54HD070725), including the Nutrition and Obesity Policy, Research and Evaluation Network, and the Office of Behavioural and Social Sciences Research of NIH. We thank Faten Ben Abdelaziz of WHO Regional Office for the Eastern Mediterranean for comments and advice on the manuscript and for regional media advertising data. We thank Caroline Hancock for sharing her MSc in Public Health dissertation. We thank Jaap Seidell and Carolyn Summerbell for their comments on an earlier version of the manuscript, and to the anonymous reviewers of the submitted drafts.
Footnotes
Contributors
All authors jointly formulated the major concepts of this paper and approved the final version. TL wrote and edited successive versions of the paper. RJ-L provided child obesity prevalence estimates. MLM wrote the section on cost-effectiveness. KDH provided new estimates of energy balance. KM provided overall supervision. All authors provided information and references for this paper.
Declaration of interests
We declare no competing interests. The authors alone are responsible for the views expressed in this paper, and they do not necessarily represent the views or policies of the institutions with which they are affiliated.
For the National School Measurement Programme in England see http://www.hscic.gov.uk/ncmp
For the Lancet Series on Maternal and Child Nutrition see http://www.thelancet.com/series/maternal-and-child-nutrition
For the Lancet Series on Physical Activity see http://www.thelancet.com/series/physicalactivity
For the NOURISHING Framework see http://www.wcrf.org/int/policy/nourishing-framework
For the GINA resource see http://www.who.int/nutrition/gina/en/
See Online for appendix
Contributor Information
Tim Lobstein, World Obesity Federation (formerly the International Association for the Study of Obesity), London, UK.
Rachel Jackson-Leach, World Obesity Federation (formerly the International Association for the Study of Obesity), London, UK.
Prof. Marjory L Moodie, Deakin Health Economics, Deakin University, Melbourne, VIC, Australia.
Kevin D Hall, National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health, Bethesda, MD, USA.
Prof. Steven L Gortmaker, Department of Social and Behavioral Sciences, Harvard School of Public Health, Boston, MA, USA.
Prof. Boyd A Swinburn, WHO Collaborating Centre for Obesity Prevention Deakin University, Melbourne, VIC, Australia, and School of Population Health, University of Auckland, New Zealand.
Prof. W Philip T James, World Obesity Federation (formerly the International Association for the Study of Obesity), London, UK.
Prof. Youfa Wang, Department of Epidemiology and Environmental Health, School of Public Health and Health Professions, University at Buffalo, State University of New York, NY, USA.
Prof. Klim McPherson, New College, University of Oxford, Oxford, UK.
References
- 1.Department of Health, Chief Medical Officer. On the state of the public’s health. London: Stationery Office; 2002. Annual report of the Chief Medical Officer. [Google Scholar]
- 2.WHO. Resolutions and decisions, sixty-sixth World Health Assembly, 20–27 May 2013. Geneva: World Health Organization; 2013. WHA66/2013/REC/1. [Google Scholar]
- 3.Wang Y, Wu Y, Wilson RF, et al. Comparative effectiveness review no. 115. Rockville, MD: Agency for Healthcare Research and Quality; 2013. [accessed Jan 7, 2015]. Childhood obesity prevention programs: comparative effectiveness review and meta-analysis. http://www.ncbi.nlm.nih.gov/books/NBK148737/ [PubMed] [Google Scholar]
- 4.Nixon CA, Moore HJ, Douthwaite W, et al. Identifying effective behavioural models and behaviour change strategies underpinning preschool- and school-based obesity prevention interventions aimed at 4–6-year-olds: a systematic review. Obes Rev. 2012;13:106–17. doi: 10.1111/j.1467-789X.2011.00962.x. [DOI] [PubMed] [Google Scholar]
- 5.Khambalia AZ, Dickinson S, Hardy LL, Gill T, Baur LA. A synthesis of existing systematic reviews and meta-analyses of school-based behavioural interventions for controlling and preventing obesity. Obes Rev. 2012;13:214–33. doi: 10.1111/j.1467-789X.2011.00947.x. [DOI] [PubMed] [Google Scholar]
- 6.Larson N, Ward DS, Neelon SB, Story M. What role can child-care settings play in obesity prevention? A review of the evidence and call for research efforts. J Am Diet Assoc. 2011;111:1343–62. doi: 10.1016/j.jada.2011.06.007. [DOI] [PubMed] [Google Scholar]
- 7.Flynn MA, McNeil DA, Maloff B, et al. Reducing obesity and related chronic disease risk in children and youth: a synthesis of evidence with ‘best practice’ recommendations. Obes Rev. 2006;7:7–66. doi: 10.1111/j.1467-789X.2006.00242.x. [DOI] [PubMed] [Google Scholar]
- 8.Dixon B, Peña MM, Taveras EM. Lifecourse approach to racial/ethnic disparities in childhood obesity. Adv Nutr. 2012;3:73–82. doi: 10.3945/an.111.000919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huang TT-K, Cawley JH, Ashe M, et al. Mobilisation of public support for policy actions to prevent obesity. Lancet. 2015 doi: 10.1016/S0140-6736(14)61743-8. published online Feb 19. http://dx.doi.org/10.1016/S0140-6736(14)61743-8. [DOI] [PubMed]
- 10.Lobstein T, Swinburn B. Health promotion to prevent obesity: evidence and policy needs. In: McQueen D, Jones C, editors. Global perspectives on health promotion effectiveness. New York: Springer Science & Business Media; 2007. pp. 125–50. [Google Scholar]
- 11.Cawley J. The cost-effectiveness of programs to prevent or reduce obesity: the state of the literature and a future research agenda. Arch Pediatr Adolesc Med. 2007;161:611–14. doi: 10.1001/archpedi.161.6.611. [DOI] [PubMed] [Google Scholar]
- 12.Moodie M, Carter R. Economic evaluation of obesity interventions. In: Waters E, Seidell J, Swinburn B, Uauy R, editors. Community-based obesity prevention: evidence, practice and policy. Oxford, UK: Blackwell Publishing; 2010. [Google Scholar]
- 13.Oude Luttikhuis H, Baur L, Jansen H, et al. Interventions for treating obesity in children. Cochrane Database Syst Rev. 2009;1:CD001872. doi: 10.1002/14651858.CD001872.pub2. [DOI] [PubMed] [Google Scholar]
- 14.John J, Wolfenstetter SB, Wenig CM. An economic perspective on childhood obesity: recent findings on cost of illness and cost effectiveness of interventions. Nutrition. 2012;28:829–39. doi: 10.1016/j.nut.2011.11.016. [DOI] [PubMed] [Google Scholar]
- 15.National Institute for Health and Care Excellence (NICE) Review of cost-effectiveness evidence. London: NICE; 2011. Whole system approaches to obesity prevention. [Google Scholar]
- 16.National Institute for Health and Care Excellence (NICE) Evidence statements and reviews: CG43. London: NICE; 2007. Obesity: full guideline, section 6- health economics. [Google Scholar]
- 17.Magnus A, Haby MM, Carter R, Swinburn B. The cost-effectiveness of removing television advertising of high-fat and/or high-sugar food and beverages to Australian children. Int J Obes (Lond) 2009;33:1094–102. doi: 10.1038/ijo.2009.156. [DOI] [PubMed] [Google Scholar]
- 18.Department of Health, Victoria, Australia. Summary of results. Melbourne: State Government of Victoria; 2006. ACE-Obesity. Assessing cost-effectiveness of obesity interventions in children and adolescents. [Google Scholar]
- 19.Wang LY, Gutin B, Barbeau P, et al. Cost-effectiveness of a school-based obesity prevention program. J Sch Health. 2008;78:619–24. doi: 10.1111/j.1746-1561.2008.00357.x. [DOI] [PubMed] [Google Scholar]
- 20.Moodie ML, Herbert JK, de Silva-Sanigorski AM, et al. The cost-effectiveness of a successful community-based obesity prevention program: the Be Active Eat Well program. Obesity (Silver Spring) 2013;21:2072–80. doi: 10.1002/oby.20472. [DOI] [PubMed] [Google Scholar]
- 21.McAuley KA, Taylor RW, Farmer VL, et al. Economic evaluation of a community-based obesity prevention program in children: the APPLE project. Obesity (Silver Spring) 2010;18:131–36. doi: 10.1038/oby.2009.148. [DOI] [PubMed] [Google Scholar]
- 22.Moya Martínez P, Sánchez López M, López Bastida J, et al. Cost-effectiveness of an intervention to reduce overweight and obesity in 9–10-year-olds. The Cuenca study. Gac Sanit. 2011;25:198–204. doi: 10.1016/j.gaceta.2010.11.003. (in Spanish) [DOI] [PubMed] [Google Scholar]
- 23.Brown HS, 3rd, Pérez A, Li YP, Hoelscher DM, Kelder SH, Rivera R. The cost-effectiveness of a school-based overweight program. Int J Behav Nutr Phys Act. 2007;4:47. doi: 10.1186/1479-5868-4-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang LY, Yang Q, Lowry R, Wechsler H. Economic analysis of a school-based obesity prevention program. Obes Res. 2003;11:1313–24. doi: 10.1038/oby.2003.178. [DOI] [PubMed] [Google Scholar]
- 25.Kalavainen M, Karjalainen S, Martikainen J, Korppi M, Linnosmaa I, Nuutinen O. Cost-effectiveness of routine and group programs for treatment of obese children. Pediatr Int. 2009;51:606–11. doi: 10.1111/j.1442-200X.2009.02810.x. [DOI] [PubMed] [Google Scholar]
- 26.Ananthapavan J, Moodie M, Haby M, Carter R. Assessing cost-effectiveness in obesity: laparoscopic adjustable gastric banding for severely obese adolescents. Surg Obes Relat Dis. 2010;6:377–85. doi: 10.1016/j.soard.2010.02.040. [DOI] [PubMed] [Google Scholar]
- 27.Moodie M, Haby M, Wake M, Gold L, Carter R. Cost-effectiveness of a family-based GP-mediated intervention targeting overweight and moderately obese children. Econ Hum Biol. 2008;6:363–76. doi: 10.1016/j.ehb.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 28.Hollingworth W, Hawkins J, Lawlor DA, Brown M, Marsh T, Kipping RR. Economic evaluation of lifestyle interventions to treat overweight or obesity in children. Int J Obes (Lond) 2012;36:559–66. doi: 10.1038/ijo.2011.272. [DOI] [PubMed] [Google Scholar]
- 29.Goldfield GS, Epstein LH, Kilanowski CK, Paluch RA, Kogut-Bossler B. Cost-effectiveness of group and mixed family-based treatment for childhood obesity. Int J Obes Relat Metab Disord. 2001;25:1843–49. doi: 10.1038/sj.ijo.0801838. [DOI] [PubMed] [Google Scholar]
- 30.Moodie ML, Carter RC, Swinburn BA, Haby MM. The cost-effectiveness of Australia’s Active After-School Communities program. Obesity (Silver Spring) 2010;18:1585–92. doi: 10.1038/oby.2009.401. [DOI] [PubMed] [Google Scholar]
- 31.Moodie M, Haby MM, Swinburn B, Carter R. Assessing cost-effectiveness in obesity: active transport program for primary school children—TravelSMART schools curriculum program. J Phys Act Health. 2011;8:503–15. doi: 10.1123/jpah.8.4.503. [DOI] [PubMed] [Google Scholar]
- 32.Moodie M, Haby M, Galvin L, Swinburn B, Carter R. Cost-effectiveness of active transport for primary school children—Walking School Bus program. Int J Behav Nutr Phys Act. 2009;6:63. doi: 10.1186/1479-5868-6-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Obesity: Preventing and managing the global epidemic. Geneva: World Health Organization; 2000. WHO Technical Report Series 894. [PubMed] [Google Scholar]
- 34.Haby MM, Carter R, Swinburn B, et al. New approaches to Assessing Cost-Effectiveness of obesity interventions in children and adolescents. (ACE-Obesity project) Int J Obes. 2006;30:1463–75. doi: 10.1038/sj.ijo.0803469. [DOI] [PubMed] [Google Scholar]
- 35.Keating CL, Moodie ML, Richardson J, Swinburn BA. Utility-based quality of life of overweight and obese adolescents. Value Health. 2011;14:752–58. doi: 10.1016/j.jval.2011.02.1181. [DOI] [PubMed] [Google Scholar]
- 36.Keating CL, Moodie ML, Swinburn BA. The health-related quality of life of overweight and obese adolescents—a study measuring body mass index and adolescent-reported perceptions. Int J Pediatr Obes. 2011;6:434–41. doi: 10.3109/17477166.2011.590197. [DOI] [PubMed] [Google Scholar]
- 37.Puhl RM, Latner JD. Stigma, obesity, and the health of the nation’s children. Psychol Bull. 2007;133:557–80. doi: 10.1037/0033-2909.133.4.557. [DOI] [PubMed] [Google Scholar]
- 38.Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet. 2011;378:815–25. doi: 10.1016/S0140-6736(11)60814-3. [DOI] [PubMed] [Google Scholar]
- 39.Waters E, de Silva-Sanigorski A, Hall BJ, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2011;12:CD001871. doi: 10.1002/14651858.CD001871.pub3. [DOI] [PubMed] [Google Scholar]
- 40.Ogden CL, Fryar CD, Carroll MD, Flegal KM. Advance data from vital and health statistics, no 347. Hyattsville, MD: National Center for Health Statistics; 2004. Mean body weight, height, and body mass index, United States 1960–2002. [PubMed] [Google Scholar]
- 41.McDowell MA, Fryar CD, Ogden CL, Flegal KM. National health statistics reports; no 10. Hyattsville, MD: National Center for Health Statistics; 2008. Anthropometric reference data for children and adults: United States, 2003–2006. [PubMed] [Google Scholar]
- 42.Hall KD. Modeling metabolic adaptations and energy regulation in humans. Annu Rev Nutr. 2012;32:35–54. doi: 10.1146/annurev-nutr-071811-150705. [DOI] [PubMed] [Google Scholar]
- 43.Lin BH, Smith TA, Lee JY, Hall KD. Measuring weight outcomes for obesity intervention strategies: the case of a sugar-sweetened beverage tax. Econ Hum Biol. 2011;9:329–41. doi: 10.1016/j.ehb.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 44.Hall KD, Sacks G, Chandramohan D, et al. Quantification of the effect of energy imbalance on bodyweight. Lancet. 2011;378:826–37. doi: 10.1016/S0140-6736(11)60812-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hall KD, Butte NF, Swinburn BA, Chow CC. Dynamics of childhood growth and obesity: development and validation of a quantitative mathematical model. Lancet Diabetes Endocrinol. 2013;1:97–105. doi: 10.1016/s2213-8587(13)70051-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.WHO. Growth reference data for 5–19 years. Geneva: World Health Organization; 2013. [accessed Jan 7, 2015]. http://www.who.int/childgrowth/en/ [Google Scholar]
- 47.Khadilkar VV, Khadilkar AV, Cole TJ, Sayyad MG. Crosssectional growth curves for height, weight and body mass index for affluent Indian children, 2007. Indian Pediatr. 2009;46:477–89. [PubMed] [Google Scholar]
- 48.Del-Rio-Navarro BE, Velazquez-Monroy O, Santos-Preciado JI, et al. Mexican anthropometric percentiles for ages 10–18. Eur J Clin Nutr. 2007;61:963–75. doi: 10.1038/sj.ejcn.1602612. [DOI] [PubMed] [Google Scholar]
- 49.del Río-Navarro BE, Velázquez-Monroy O, Sánchez-Castillo CP, et al. the Encuesta Nacional de Salud 2000 Working Group, National Health Survey 2000. The high prevalence of overweight and obesity in Mexican children. Obes Res. 2004;12:215–23. doi: 10.1038/oby.2004.28. [DOI] [PubMed] [Google Scholar]
- 50.Le Nguyen BK, Le Thi H, Nguyen Do VA, et al. Double burden of undernutrition and overnutrition in Vietnam in 2011: results of the SEANUTS study in 0·5–11-year-old children. Br J Nutr. 2013;110:S45–56. doi: 10.1017/S0007114513002080. [DOI] [PubMed] [Google Scholar]
- 51.Sawaya AL, Dallal G, Solymos G, et al. Obesity and malnutrition in a Shantytown population in the city of São Paulo, Brazil. Obes Res. 1995;3:107s–15s. doi: 10.1002/j.1550-8528.1995.tb00453.x. [DOI] [PubMed] [Google Scholar]
- 52.Steyn K, Bourne L, Jooste P, Fourie JM, Rossouw K, Lombard C. Anthropometric profile of a black population of the Cape Peninsula in South Africa. East Afr Med J. 1998;75:35–40. [PubMed] [Google Scholar]
- 53.Hancock C. MSc thesis. Oxford Brookes University; 2013. What effect does socioeconomic status have on the height of the current child population in England? [Google Scholar]
- 54.Black RE, Victora CG, Walker SP, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382:427–51. doi: 10.1016/S0140-6736(13)60937-X. [DOI] [PubMed] [Google Scholar]
- 55.Uauy R, Kain J, Mericq V, Rojas J, Corvalán C. Nutrition, child growth, and chronic disease prevention. Ann Med. 2008;40:11–20. doi: 10.1080/07853890701704683. [DOI] [PubMed] [Google Scholar]
- 56.Working Group on Infant and Young Child Feeding Indicators. Food and Nutrition Technical Assistance Project. Washington, DC: Academy for Educational Development; 2006. Developing and validating simple indicators of dietary quality and energy intake of infants and young children in developing countries: summary of findings from analysis of 10 data sets. [Google Scholar]
- 57.Santika O, Fahmida U, Ferguson EL. Development of food-based complementary feeding recommendations for 9- to 11-month-old peri-urban Indonesian infants using linear programming. J Nutr. 2009;139:135–41. doi: 10.3945/jn.108.092270. [DOI] [PubMed] [Google Scholar]
- 58.Menon P, Bamezai A, Subandoro A, Ayoya MA, Aguayo V. Age-appropriate infant and young child feeding practices are associated with child nutrition in India: insights from nationally representative data. Matern Child Nutr. 2013 doi: 10.1111/mcn.12036. published online April 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Darapheak C, Takano T, Kizuki M, Nakamura K, Seino K. Consumption of animal source foods and dietary diversity reduce stunting in children in Cambodia. Int Arch Med. 2013;6:29. doi: 10.1186/1755-7682-6-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bhutta ZA, Das JK, Rizvi A, et al. the Lancet Nutrition Interventions Review Group, and the Maternal and Child Nutrition Study Group. Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost? Lancet. 2013;382:452–77. doi: 10.1016/S0140-6736(13)60996-4. [DOI] [PubMed] [Google Scholar]
- 61.Stuckler D, McKee M, Ebrahim S, Basu S. Manufacturing epidemics: the role of global producers in increased consumption of unhealthy commodities including processed foods, alcohol, and tobacco. PLoS Med. 2012;9:e1001235. doi: 10.1371/journal.pmed.1001235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Levinson FJ, Balarajan Y. Addressing malnutrition multisectorally: what have we learned from recent international experience? UNICEF Nutrition Working Paper. New York: UNICEF and MDG Achievement Fund; 2013. [Google Scholar]
- 63.Keen YJ, Allain A, Razak RA. Breaking the rules, stretching the rules 2010: evidence of violation of the International Code of Marketing of Breastmilk Substitutes and subsequent resolutions. Penang: International Code Documentation Centre, International Baby Food Action Network; 2010. [Google Scholar]
- 64.Smith J, Blake M. Infant food marketing strategies undermine effective regulation of breast-milk substitutes: trends in print advertising in Australia, 1950–2010. Aust N Z J Public Health. 2013;37:337–44. doi: 10.1111/1753-6405.12081. [DOI] [PubMed] [Google Scholar]
- 65.WHO. Meeting report of first meeting of the WHO scientific and technical advisory group on inappropriate promotion of foods for infants and young children. Geneva: World Health Organization; 2013. [accessed Jan 7, 2015]. http://www.who.int/nutrition/publications/STAGmeeting_report/en/ [Google Scholar]
- 66.Internal Markets Bureau. Global pathfinder report: baby food market indicator report. Ottawa: Agriculture and Agri-Food Canada; 2011. [Google Scholar]
- 67.Lobstein T, Dibb S. Evidence of a possible link between obesogenic food advertising and child overweight. Obes Rev. 2005;6:203–08. doi: 10.1111/j.1467-789X.2005.00191.x. [DOI] [PubMed] [Google Scholar]
- 68.Kelly B, Halford JC, Boyland EJ, et al. Television food advertising to children: a global perspective. Am J Public Health. 2010;100:1730–36. doi: 10.2105/AJPH.2009.179267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Anonymous. Pan Arab Research Center, Safat, Kuwait. [accessed Jan 7, 2015];Online market information database. http://arabresearch.iniquus.com/KnowledgeBase.aspx.
- 70.et al. PARC Year Book 2007. Safat, Kuwait: Pan Arab Research Center; 2007. [accessed Jan 7, 2015]. http://arabresearch.iniquus.com/Docs/PDFs/PARCBookY2007.pdf. [Google Scholar]
- 71.Malik VS, Pan A, Willett WC, Hu FB. Sugar-sweetened beverages and weight gain in children and adults: a systematic review and meta-analysis. Am J Clin Nutr. 2013;98:1084–102. doi: 10.3945/ajcn.113.058362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Alexander E, Yach D, Mensah GA. Major multinational food and beverage companies and informal sector contributions to global food consumption: implications for nutrition policy. Global Health. 2011;7:26. doi: 10.1186/1744-8603-7-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.et al. Global Soft Drinks. London: MarketLine; 2013. [accessed Jan 7, 2015]. http://marketpublishers.com/report/consumers_goods/food_beverage/global_soft_drinks.html. [Google Scholar]
- 74.et al. Industry profile. London: MarketLine; 2013. [accessed Jan 7, 2015]. Brazil—soft drinks. http://store.marketline.com/Product/brazil_soft_drinks?productid=MLIP1415-0005. [Google Scholar]
- 75.Anonymous. Soft drinks industry in India. New Delhi: NIIR Project Consultancy Services; 2012. [accessed Sept 3, 2014]. http://www.niir.org/information/content.phtml?content=184. [Google Scholar]
- 76.Swinburn B, Sacks G, Vandevijvere S, et al. INFORMAS (International Network for Food and Obesity/non-communicable diseases Research, Monitoring and Action Support: overview and key principles. Obes Rev. 2013;14:1–12. doi: 10.1111/obr.12087. [DOI] [PubMed] [Google Scholar]
- 77.Roberto CA, Swinburn B, Hawkes C, et al. Patchy progress on obesity prevention: emerging examples, entrenched barriers, and new thinking. Lancet. 2015 doi: 10.1016/S0140-6736(14)61744-X. published online Feb 19. http://dx.doi.org/10.1016/S0140-6736(14)61744-X. [DOI] [PubMed]
- 78.Hawkes C, Smith TG, Jewell J, et al. Smart food policies for obesity prevention. Lancet. 2015 doi: 10.1016/S0140-6736(14)61745-1. published online Feb 19. http://dx.doi.org/10.1016/S0140-6736(14)61745-1. [DOI] [PubMed]
- 79.WHO. Marketing of foods high in fat, salt and sugar to children: update 2012–2013. Copenhagen: World Health Organization Regional office for Europe; 2013. [Google Scholar]
- 80.Spencer J. [accessed Jan 7, 2015];Getting rid of junk food marketing in schools—it may be a lot harder than you think. 2012 Apr 20; http://www.momsrising.org/blog/es/getting-rid-of-junk-food-marketing-in-schools-%E2%80%93-it-may-be-a-lot-harder-than-you-think.
- 81.Coleman-Jensen A, Nord M, Andrews M, Carlson S. USDA Economic Research Service, Economic Research Report Number 141. Washington, DC: United States Department of Agriculture; 2012. Household food security in the United States in 2011. [Google Scholar]
- 82.US Department of Agriculture, Agricultural Research Service. Table 5 in What We Eat in America, NHANES 2009–2010. Washington, DC: ARS; 2012. [accessed Jan 7, 2015]. Energy intakes: percentages of energy from protein, carbohydrate, fat, and alcohol, by gender and age. www.ars.usda.gov/ba/bhnrc/fsrg. [Google Scholar]
- 83.Moodie R, Stuckler D, Monteiro C, et al. Profits and pandemics: prevention of harmful effects of tobacco, alcohol, and ultra-processed food and drink industries. Lancet. 2013;381:670–79. doi: 10.1016/S0140-6736(12)62089-3. [DOI] [PubMed] [Google Scholar]
- 84.Gortmaker SL, Swinburn BA, Levy D, et al. Changing the future of obesity: science, policy, and action. Lancet. 2011;378:838–47. doi: 10.1016/S0140-6736(11)60815-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.WHO. Set of recommendations on the marketing of foods and non-alcoholic beverages to children. Geneva: World Health Organization; 2010. [accessed Jan 7, 2015]. http://www.who.int/dietphysicalactivity/publications/recsmarketing/en/index.html. [Google Scholar]
- 86.WHO. A framework for implementing the set of recommendations on the marketing of foods and non-alcoholic beverages to children. Geneva: World Health Organization; 2012. [accessed Jan 7, 2015]. http://www.who.int/dietphysicalactivity/MarketingFramework2012.pdf. [Google Scholar]
- 87.Galbraith-Emami S, Lobstein T. The impact of initiatives to limit the advertising of food and beverage products to children: a systematic review. Obes Rev. 2013;14:960–74. doi: 10.1111/obr.12060. [DOI] [PubMed] [Google Scholar]
- 88.WHO. International code of marketing of breast-milk substitutes. Geneva: World Health Organization; 1981. [accessed Jan 9, 2015]. http://www.who.int/nutrition/publications/code_english.pdf. [Google Scholar]
- 89.El-Zanaty F, Way A. Egypt: demographic and health survey 2008. Cairo, Egypt: Ministry of Health, El-Zanaty and Associates, and Macro International; 2009. [accessed Jan 7, 2015]. http://dhsprogram.com/pubs/pdf/FR220/FR220.pdf. [Google Scholar]
- 90.Limon G, de Haan N, Schwabenbauer K, Ahmed ZS, Rushton J. Highly pathogenic avian influenza: a rapid assessment of its socio-economic impact on vulnerable households in Egypt. Rome: Food and Agriculture Organization of the United Nations; 2009. [accessed Jan 7, 2015]. http://www.fao.org/docrep/013/al686e/al686e00.pdf. [Google Scholar]
- 91.WHO. Global school-based student health survey: Egypt 2011 Health Survey. Geneva: World Health Organization; 2013. [accessed Jan 7, 2015]. http://www.who.int/chp/gshs/Egypt_GSHS_FS_2011.pdf. [Google Scholar]
- 92. [accessed Jan 7, 2015];Households with television: countries compared. http://www.nationmaster.com/graph/med_hou_wit_tel-media-householdswith-television.