Abstract
Objective
The aim of this study was to identify and describe the use of electronic health records for information sharing between patients and clinicians in primary care encounters. This topic is particularly important as computers and other technologies are increasingly implemented in multi-user health care settings where interactions and communication between patients and clinicians are integral to interpersonal and organizational outcomes.
Method
An ethnographic approach was used to classify the encounters into distinct technology-use patterns based on clinicians` interactions with the technology and patients. Each technology-use pattern was quantitatively analysed to assist with comparison. Quantitative analysis was based on duration of patient and clinician gaze at EHR.
Findings
Physicians employed three different styles to share information using EHRs:
Active information-sharing, in which a clinician turns the monitor towards the patient and uses the computer to actively share information with the patient;
Passive information-sharing, when a clinician does not move the monitor, but the patient might see the monitor by leaning in if they choose; and
Technology withdrawal, when a clinician does not share the monitor with the patient.
Conclusion
A variety of technology-mediated information-sharing styles may be effective in providing patient-centred care. New EHR designs may be needed to facilitate information sharing between patients and clinicians.
1. Introduction
Information Technology (IT) has been widely used in health care in the last decade. The benefits of information technology such as electronic health records (EHRs) include easy access to a patient’s medical history, medical data, and medical information (Shachak et al., 2009). However, computers in the exam rooms can impact communication cues, such as length of gaze, frequency of mutual gaze, and body language between patients and care providers, which can potentially affect patients’ perceptions of the visit (Montague et al., 2011, Beck et al., 2002). Communication cues also impact patient outcomes, such as adherence and satisfaction (Roter et al., 2006). Indeed, the use of computers in the consultation may alter the patient-clinician dynamic, including the sequence and frequency of communication cues (Margalit et al., 2006). A study addressing the social and personal factors which impact clinicians’ health information technology (HIT) use, found that HITs may alter the cognitive performance of clinicians who must use them to provide care (Holden, 2011). In another study, Karsh et al. (2004) found that even though EHR users have higher satisfaction with their medical records than paper record users, computer use can also serve as an interruption that negatively affects clinicians’ ability to actively attend to patients. Computer use can contribute to decreases in dialogue, which can negatively influence psychological and emotional communication and affect the development of rapport (Margalit et al., 2006), and patients can feel disengaged while the clinician is using the computer (Frankel et al., 2005). On the other hand, computer use has been associated with visit efficiency and a reduction in costs (Chaudhry et al., 2006). Lievre and Schultz (2010) found that clinician computer use can also positively impact patient satisfaction. Since technology is a viable solution for increasing efficiency in the care provision process, it is essential to mitigate any negative effects of computer use in primary care consultations by identifying better designs, better technology use patterns, and better clinician training interventions.
The integration of computers (EHRs) has created different behavioural styles that clinicians show when they interact with EHRs (Ventres et al., 2005, Pearce et al., 2009). Ventres et al. (2005) identified three distinct practice styles of clinicians—informational, interpersonal and managerial—through ethnographic analysis of videotaped visits. The informational style is characterized by gathering information from the monitor, while in the interpersonal style the clinician focuses primarily on the patient. The managerial style is a bridge between both the informational and interpersonal styles. Another study explored how clinicians orient computer monitors during different phases of a consultation (Chen et al., 2011). In order to increase patient participation and facilitate expression via eye contact during the visit, clinicians readjusted computers in different orientations during three different medical stages: a communication-intensive phase, a lecturing phase, and an ordering phase (Chen et al., 2011). However, thus far there have been no quantitative studies to identify and examine different technology-use patterns in primary care visits.
1.1 Shared computer use
A recent study proposed that because EHRs provide for information sharing between health care workers and patients, they are a collaborative technology (Pratt et al., 2004). Moreover, sharing information with the patient keeps them actively involved in the consultation and is a first step towards shared decision making (Elwyn et al., 1999). Studies have found that screens are sites for possible collaboration; thus sharing information from the EHR might be a feature of best practice of health information technology use in clinical encounters (Robles et al., 2009). Sharing information from the EHR will likely increase patients’ involvement in the visit and improve the patients’ knowledge about their health status.
HIT that assists with information sharing might have an essential role in engaging and informing patients about their health (Ahern et al., 2011). Collaborative document viewing with patient-centric information displays is recommended to overcome the difficulty of patient access to information in exam rooms (Wilcox et al., 2010). For instance, a shared view of a patient’s medical records, especially charts and images, could improve communication between clinician and patient (Piper and Hollan, 2011). Another recent study suggests that projecting large images and utilizing touch-based interactions with the computer itself could potentially turn exam room surfaces into collaborative, visual workspaces in oncology clinics (Unruh et al., 2010). In addition, tabletop computer displays were suggested as collaborative tools to facilitate eye contact while still allowing interaction with the display (Wang and Blevis, 2004). One study tested patient displays with older adults; patients reported that the touch-screen computer system facilitated communication with the doctor (Piper and Hollan, 2011). When the clinician and patient review diagrams and charts together, the conversation is enriched, patient comprehension is improved, and shared understanding is facilitated (Unruh et al., 2010). Designing information technologies that facilitate clinician-patient interaction and collaboration in primary care settings contributes to patient satisfaction, emotional health, compliance with medical recommendations, and symptom resolution (Stewart, 1995).
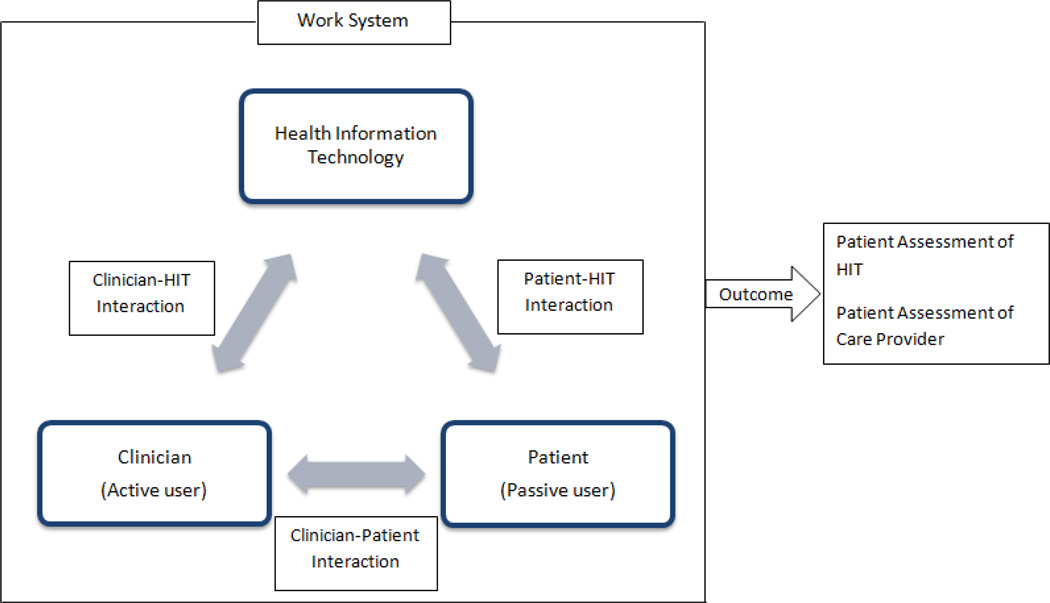
In primary care environments, technology-mediated interactions occur between the active user (clinician), passive user (patient), and the technology itself (Figure 1). The clinician completes certain tasks, such as information exchange with the patient, developing a treatment plan, and diagnosing a current disease, in the interaction process. These tasks influence patient outcomes such as trust and satisfaction. Various technology-use patterns might be employed by clinicians to complete the required tasks. For human-computer interaction (HCI) field researchers, identifying technology-use patterns and understanding how they facilitate communication in medical settings might improve the quality of patient care (Chen et al., 2011). Depending on the typologies of technology-use patterns, it is possible to design systems that optimize interactions between technology and humans. We can also propose training systems and new HIT design guidelines to optimize nonverbal interaction in computerized exam rooms.
Figure 1.
The multiple interactions in a primary care exam room
Purpose and research questions
This study aimed to understand clinicians’ technology-mediated information sharing with patients in primary care encounters. A mixed-method was used that included ethnographic analysis, quantified observation of behaviours, and qualitative analysis of coded events. The outcomes of this study are descriptions of information collaborative behaviour and recommendations for design.
Data for this study included 101 medical encounters that included patients, clinicians, and EHRs. An ethnographic approach was used to classify the encounters into distinct technology-use patterns. Then, each technology-use pattern was quantitatively analysed to assist with comparison.
2. Method
2.1 Study design
Data was derived from videotaped medical encounters of research patients who sought care in primary care clinics with their primary care doctors. 101 encounters were recorded with high resolution video using three cameras. The encounters took place in five different clinics in the Midwest between December 2010 and June 2011. Approval for this study was obtained from a Health Sciences Institutional Review Board. Because ensuring patient privacy is particularly important for videotaped studies, additional measures were taken to maintain confidentiality. All research protocols were designed and evaluated for compliance with human subjects ethics and Health Insurance Portability and Accountability Act (HIPAA) regulations.
2.2 Data collection and recruitment
Clinicians were invited to participate based on the established recruitment needs—two clinicians per clinic, 10 patients per clinician—across clinics that served a variety of patient populations. Efforts were made to recruit a diverse sample of patient participants across genders, racial/ethnic status, age, socioeconomic status and education. New patients were not recruited for this study, to mitigate the potential effects of first time encounters and the differing processes that are used for new patients as opposed to existing patients. Two clinicians at each clinic agreed to participate in the study by allowing video and audio taping of their normal care provision practices. Patients were invited to participate in the study if they were being seen on a day when data collection with the clinician was taking place and if they were on time for their visit. Since each clinician had a different schedule and frequency of seeing patients daily, data collection took 53 days throughout a six month period. The average recruitment rate was 1.9 patients per day.
Eligible patients were identified through the clinic’s electronic scheduling system by a staff member authorized to work with patient data. Several weeks before their appointment, a recruitment letter signed by the Principle Investigator and the primary care provider was sent by project staff to eligible patients. The letter included an opt-out card that could be mailed back to the researchers, indicating that the patient did not wish to be invited to participate when they arrived at the clinic. A research specialist affiliated with the clinic contacted candidate participants by phone two days before their clinical appointment. The research specialist described the study, invited the patient to participate in the study, and asked them to arrive at the clinic 15 minutes early to complete the informed consent procedures. Patients who did not wish to participate were not asked to arrive early for their visit. Patients who were not reachable before the visit or scheduled their visits within the last few days were invited to participate by the receptionist during check in with a standardized script explaining the study. These efforts were made so that invitations to participate were first made by a person directly involved in the patients’ care.
Informed consent was obtained from patients who agreed to participate in the study. Next, the patient was taken to the exam room that was instrumented for video recording. At this point, only the patient and the clinician were allowed in the exam room. After the consultation, the patient was taken to a private room to participate in an interview and complete a questionnaire. Interview questions and questionnaires included an assessment of the visit, open-ended questions about the physician and health system, and their perception of the electronic health records used in the visit. Patients who completed the study received a modest stipend for their participation.
2.3 Sample
Demographic characteristics were collected from clinicians and patients. Patient ages ranged from 18–65 (M 45.21, SD 13.3) and were relatively dispersed across age groups with 29 participants ages 18–29, 14 ages 30–29, 20 ages 40–49, 31 ages 50–59, 15 ages 60–65, and two who did not provide an age. Patients over the age of 65 and under the age of 18 were excluded from participation. 57 men and 44 women agreed to participate, and education levels varied: 10 had less than a high school degree, 28 were high-school graduates or GED equivalent, 24 had some college, 18 were college graduates, 20 had degrees above the bachelor’s degree, and one did not answer this question. 79 participants identified as white or Caucasian, 16 as Black or African American, 3 as Asian American, and 3 as Latino or Hispanic. The length of time of the patients’ relationship with their clinicians ranged from 1 to 37 years. Human subjects protocols prevented the recruitment of participants who did not speak English or who preferred to speak another language with their care provider during the visit. The clinician group was comprised of six males and four females (M 47.6 years old). The clinicians had been practicing family medicine for 5 to 37 years and had used computers in clinical consultations for the past 3 to 10 years.
2.4 Instrumentation
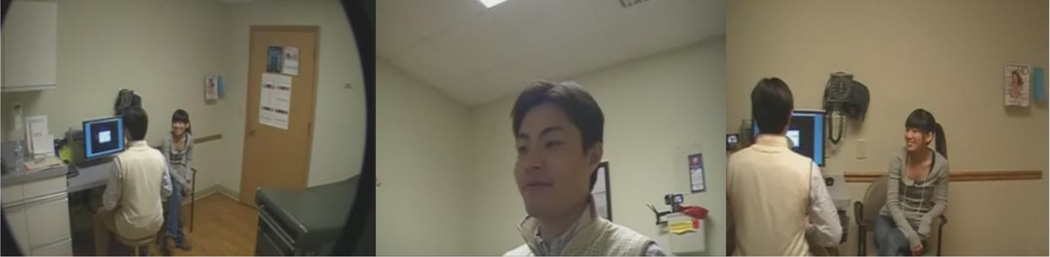
Three cameras were used to capture all interactions, such as body language and gazing direction, for both participant groups in this study. Each camera was placed at a different angle—one wide angle and two providing a close view of the patient and clinician—to clearly capture nonverbal behaviours (Figure 2). Cameras were fairly small to minimize distraction. In addition, clinicians were given a remote control in case they needed to stop the recording for any reason. Reasons included the discussion of socially stigmatizing or risky behaviour or if the patient chose to end their participation in the study before the end of the visit.
Figure 2.
A sample representation of three-channel recording
2.5 Data analysis
This study used qualitative and quantitative methods to examine clinicians’ technology-mediated information-sharing styles in primary care visits. Evidence in published literature attests to the current use of combined quantitative and qualitative methods (mixed methods) in health research (Creswell et al., 2011, Ivankova et al., 2006, Plano Clark, 2010). A recent NHS report also indicates the strength of this mixed methods approach for suitable research problems in health care research (Creswell et al., 2011). An overview of the analysis process is as follows:
Videos were analysed qualitatively using an ethnographic approach.
Themes regarding information sharing styles were created.
Videos were coded temporally, in their entirety, for patient and clinician interactions with HIT to quantitatively evaluate information-sharing.
First, qualitative analyses were used to identify qualitative themes in technology-mediated information-sharing between clinicians and patients during the visit. These themes revealed different types of information-sharing styles. Second, a quantitative analyses were conducted to examine how often each style was used in the visits and to validate the occurrence and patterns of previously identified styles. Quantitative data consisted of clinicians’ and patients’ interactions with the HIT (measured by the frequency and duration of gaze) for each style.
2.5.1 Ethnographic analysis
Ethnography is a research process which provides an understanding of an organization and a comparison between what people say and what they do (Helman, 1991). Recently, scholars such as Savage have called for the increased use of ethnography in health research, arguing that ethnography—which combines many (usually qualitative) methods, including participant observation, interviews, and informal discussions—is particularly useful in exploring “complex clinical and organizational issues” (Savage, 2000:1400). Ethnographic approaches involve gathering detailed data from a complex environment, and organizing this data by methods such as memoing, coding and creating categories and themes (Creswell, 2009). The nature of ethnographic research makes it useful for identifying research questions which can then be further analysed using other qualitative or quantitative methods (Savage, 2000). This mixed-methods study used an ethnographic method in the early stages of data collection and to identify the technology-use patterns of clinicians. The categories identified using ethnographic methods were later used to guide temporal (or time based) coding of information sharing behaviour, during patient visits, which generated quantitative data (see 2.5.2). The ethnographic approach included video observation, followed by thematic analysis of observational data to develop classifications of technology-mediated information-sharing that occurred between doctors and patients.
2.5.2 Empirical analysis
2.5.2.1 Coding
Coding is the process of reducing large amounts of complex data into measureable and quantifiable units of analysis (Miles and Hubberman, 1994). A priori codes were developed for measureable behaviours of interest (e.g. gaze or typing). Each person’s behaviour was annotated using software for its presence, beginning, and end in the video. For example, the behaviour patient gazing at clinician would be coded by only annotating the patient’s behaviour and coding each time gaze began and ended over the time the visit occurred; the same approach would be used to code clinician behaviour. Coding activities were as followed: 1) the coding scheme was developed, 2) coders were trained, 3) each video was coded temporally, from the beginning to the end of the visit, in half speed (slow motion) 4) reliability analyses were conducted, and 5) statistical analyses of coded data were completed.
2.5.2.2 Coding scheme
Codes were comprised of three parts: a subject, behaviour, and object. Subjects included clinicians and patients, behaviours were gaze and typing, and the object was the health information technology (HIT) (Table 1). During coding videos were watched at half speed, and each behaviour was coded temporally, from its beginning to its end.
Table 1.
Coding Scheme
| Codes | Definition |
|---|---|
| Subjects | |
| Patient | The patient in the encounter. |
| Doctor | The primary care provider in the encounter. |
| Behaviours | |
| Gaze | Participant’s head and/or body were in the direction of the target object. |
| Typing | Participant used hand to type on the keyboard to enter information. |
| Object | |
| Health Information Technology (HIT) | The HIT used in the video encounter. |
2.5.2.3 Coding reliability
Reliability scores were calculated conservatively; scores were calculated at one-second levels, meaning if a coded event deviated between coders by one second or more, reliability was reduced. Each coder was trained with practice videos. When the coder achieved at least a 0.60 Kappa reliability score, they were allowed to code research data. Typically, a Cohen’s Kappa value of 0.60 is standard and above 0.75 is considered an excellent value (Bakeman, 2000). Each week all coders coded a single reliability video. At the end of the week, the video was discussed in detail and reliability scores were compared to maintain a reliability value score above 0.60. The reliability scores are illustrated in Table 2.
Table 2.
Reliability of coded videos
| Week | Kappa (Average) |
Kappa (Range) |
Proportion of agreements (Average) |
Proportion of agreements (Range) |
|---|---|---|---|---|
| Week 1 | 0.63 | 0.60~0.69 | 0.70 | 0.67~0.75 |
| Week 2 | 0.72 | 0.67~0.90 | 0.77 | 0.73~0.90 |
| Week 3 | 0.65 | 0.60~0.81 | 0.70 | 0.65~0.84 |
| Week 4 | 0.72 | 0.63~0.82 | 0.76 | 0.69~0.85 |
| Week 5 | 0.75 | 0.67~0.83 | 0.81 | 0.75~0.87 |
| Week 6 | 0.65 | 0.60~0.71 | 0.72 | 0.65~0.77 |
| Week 7 | 0.71 | 0.61~0.85 | 0.77 | 0.66~0.88 |
2.5.2.4 Statistical analysis of empirical data
Variables of interest were estimated for each visit. These included:
Time gazing at computer, the total time that an individual gazed at the computer screen.
Total visit length, the total length of the visit, including times when the clinician conducted a physical exam,(visit began was when the doctor entered room and ended when the doctor left the room).
Visit length, the length of time that the clinician and patient used verbal communication excluding the physical exam period.
Shared gaze at computer, the total time that both patient and clinician gazed at the computer.
Using coded data, it was possible to obtain the frequency and duration of shared gaze at the computer. Shared gaze was defined as an event where both clinician and patient gazed at an artefact (the HIT in this study). Quantified characteristics of events (start and stop time, duration, frequency, and overlap) were collected for patient and provider behaviours in all encounters for each interactive style identified in the qualitative analyses.
The effects of ‘shared gaze at a computer’ on ‘patient gaze at a computer,’ and the effect of ‘clinician gaze at a computer’ on visit length were estimated with a regression model. The random clinician effect was incorporated. Similar regression models were used to estimate the effect of ‘gaze duration at computer’ on visit length and total visit length. Descriptive statistics were used to describe the duration and percentage behaviours such as typing and gazing at computer occurred during the visit.
3. Results
3.1 Overview of the visits
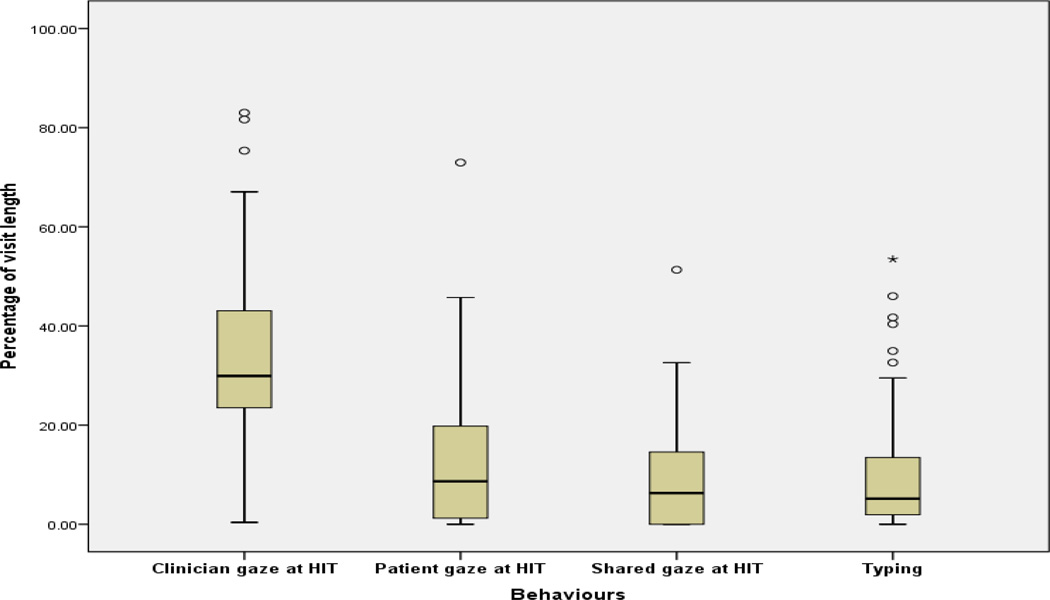
101 videos were analysed to obtain the duration (in seconds) of the variables of interest: ‘patient gaze at computer,’ ‘clinician gaze at computer,’ ‘clinician typing,’ ‘shared gaze at computer,’ ‘total visit length,’ and ‘visit length.’ ANOVA and regression analysis investigated the potential relationships between each measure. There was a significant relationship between the duration of ‘clinician gaze at computer’ with ‘total visit length’ and ‘visit length,’ respectively (F=117.33, p=0.00; F=77.871, p=0.00). The duration of ‘clinician gaze at the computer’ was also a significant predictor of ‘patient gaze at computer’ duration (F=46.247, p=0.00). Analyses showed a significant relationship between the duration of ‘shared gazing at computer’ and ‘clinician gaze at computer’ (F=57.24, p=0.00). The visit length varied between the visits, so gazing as a percentage of visit length was chosen as a more accurate illustration of the clinician’s interaction with HIT (Figure 3).
Figure 3.
The percentage representation of interaction with computer across all visit lengths
3.2 Qualitative analysis of the visits
Qualitative analyses were used to identify behavioural markers for technology-mediated information sharing between the clinicians and patients in the visits. Observation of videos suggested a list of themes that describe clinicians’ technology-mediated information-sharing behaviours. These behaviours include:
Clinician shifting the computer monitor towards the patient, so that both patient and clinician could see the monitor,
Patient moving his or her chair towards the monitor upon clinician’s verbal invitation so clinician could share the monitor with the patient,
Patient’s neutral viewing of the monitor where clinician does not shift the monitor and does not block the monitor,
Clinician does not shift the monitor and keeps it out of the patient’s line of sight, so patient does not have a chance to see the monitor.
All 101 visits were coded based on the coding scheme (table 1) and additional notes were taken on the clinicians’ information-sharing and communication style in each visit. Three distinct information-sharing styles emerged from the analysis. Each style was explained in detail with observational notes and ‘descriptive memos’ (Miles and Hubberman, 1994). Empirical analysis was conducted of each style for further explanation.
The first style is called ‘active information sharing,’ in which a clinician turns the monitor towards the patient and uses the computer to actively share information with the patient while explaining matters to the patient. The second style, ‘passive information sharing,’ is occurs when the clinician does not invite the patient to the monitor and does not move the monitor, but the patient might see the monitor by leaning in if they choose. The third style, ‘technology withdrawal,’ is when sharing does not occur. The clinician does not share the monitor and the patient does not shift his/her position to see the monitor.
3.3 Empirical overview of each technology-mediated information-sharing style
‘Active information sharing’ was identified in fifty-two visits. Qualitatively, the clinician moved the monitor towards the patient in each of the 52 visits and also verbally invited the patient to look at the monitor in 40 of these 52 visits. ‘Passive information sharing’ and ‘technology withdrawal’ were identified in 22 and 27 visits, respectively. The visit length varied between the styles: ‘active information sharing’ had the longest visit length (1229.83 s.) and ‘passive information sharing’ had the shortest visit length (833.75 s.). In addition, shared gazing took 13.8% of the visit length in ‘active information sharing’ and 9.16% of the visit length in ‘passive information sharing.’ Clinician gaze at the computer varied across the styles (26.50% to 37.58%). The ‘passive information sharing’ style had the highest percentage of ‘typing’ (12.18%). Patient gaze at the computer ranged between 1.37% and 18.15% of the visit length across styles. The estimation of all parameters for each style is illustrated in Table 3.
Table 3.
Estimate measures for each information sharing behaviour
| Number of Visits |
Total Visit Length |
Visit Length |
Clinician Gaze at HIT |
Patient Gaze at HIT |
Typing | Shared Gaze at HIT |
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Time (s) | Time (s) | Time (s) | % | Time (s) | % | Time (s) | % | Time (s) | % | ||
|
Active Information Sharing |
52 | 1433.22 | 1229.83 | 451.81 | 34.78 | 217.31 | 18.15 | 102.83 | 7.27 | 167.76 | 13.84 |
|
Passive Information Sharing |
22 | 1011.60 | 833.75 | 324.12 | 37.58 | 97.56 | 11.20 | 93.75 | 12.18 | 78.41 | 9.16 |
|
Technology Withdrawal |
27 | 1054.32 | 907.60 | 222.40 | 26.50 | 11.82 | 1.37 | 69.90 | 7.40 | 3.70 | 0.57 |
The results show that 42.23% of clinician gaze at computer and 77.35% of patient gaze at computer is shared gaze at computer in ‘active information sharing’ and 28.54% of clinician gaze at computer and 81.52% of patient gaze at computer is shared gaze at computer in the ‘passive sharing’ style. T-test results indicate that the visit length for active information sharing encounters is significantly different from passive information sharing and technology withdrawal (p= 0.002, p=0.035, respectively), and total visit length of active information sharing encounters also significantly differs from passive information sharing and technology withdrawal (p= 0.002, p= 0.006, respectively). This might indicate that active information sharing might extend the visit length. Furthermore, the duration difference between ‘total visit length’ and ‘visit length’ shows the time spent for the physical exam, if conducted, in the visit.
3.4 Qualitative descriptions of each technology-mediated information-sharing style
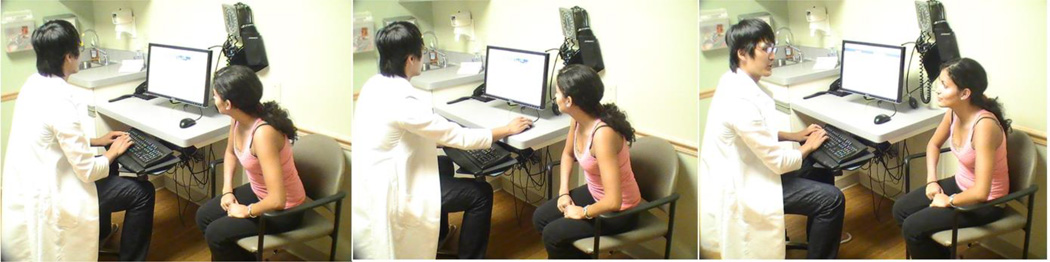
3.4.1. Active information sharing
Clinicians in the ‘active information sharing’ style shifted the monitor towards the patient at the beginning of the visit after logging in and tended to keep the computer in the same orientation during the entire visit (52 visits) (Figure 4). Clinicians also verbally invited patients to look at the monitor, and the computer played an active role in patient-clinician interaction. Clinicians used the computer in an informative way to explain results and display information. Clinicians in this style tended to type on the keyboard a smaller percentage of the visit length, when compared to the other two groups (passive sharing and technology withdrawal) (7.27%, 12.18%, and 7.40%). Qualitative analysis revealed that the lower amount of typing as a percentage of the visit may be the result of the clinician sharing information and discussing lab results, charts, or x-ray graphs while actively using the monitor. Clinicians also used the computer to retrieve information and shared this information in detail with patients while pointing to the screen. In this style, patients were also able to see what the clinician was typing, even though some researchers do not recommend this approach because of privacy issues (Chen et al., 2011). The focus in these encounters was on sharing information, rather than entering data into the computer. The ‘active information sharing’ style had the highest amount of ‘clinician gaze at computer’ (451.81 s), and the highest percentage of ‘patient gaze at computer’ (18.15%) and ‘shared gaze at computer’ (13.84%) as a percentage of visit length. This indicates that active information sharing with computer increases the amount of patient gaze at computer, and most of this gaze occurs simultaneously with clinician gaze at computer.
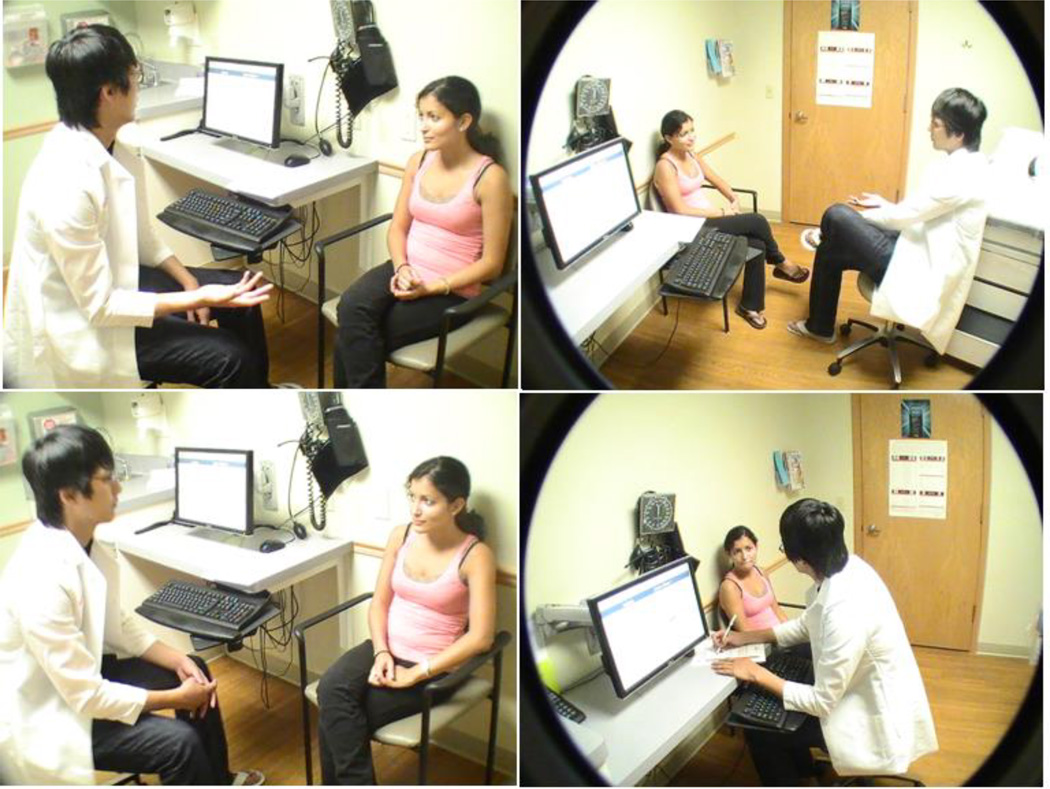
Figure 4.
Multiple snapshots from active information sharing visits
3.4.2 Passive information sharing
Passive information sharing occurred in 22 visits. In this style, the clinicians did not shift the monitor as they did in the active information sharing visits; however, patients could adjust their bodies to see the monitor if they wished (Figure 5). In the study, it appeared that patients had a desire to see the monitor, especially during the typing period. This also supports the notion that patients might be curious about what information the clinician is typing (Frankel et al., 2005). This style had the highest percentage of ‘clinician typing’ (12.18%) and ‘clinician gaze at computer’ (37.58%), as well as the lowest visit length (833.75 s), when compared to other styles. In addition, the total durations of ‘typing’ and ‘patient gaze at computer’ were similar (Table 3). Patients tended to gaze at the computer while the clinician entered data. It should also be noted that the clinicians in these visits were engaged in nonverbal communication and eye contact with the patient by shifting their gaze back and forth between the computer and the patient. These behaviours might help the clinician maintain positive nonverbal communication and mitigate possible negative effects of not collaboratively sharing the computer (Theadom et al., 2003). The content of the visits and clinicians’ behavioural styles might be an important factor that influences technology withdrawal behaviour within visits. Physicians reported in interviews that when highly emotional issues arise during clinical encounters, they avoid technology use and focus exclusively on the patient.
Figure 5.
Multiple snapshots from a passive information sharing visit
3.4.3 Technology withdrawal
There were also 27 ‘technology withdrawal’ visits in which clinicians did not share the monitor and patients did not attempt to look at the monitor during the visits (Figure 6). During these visits, clinicians gazed at the computer the least amount when compared to the other styles. The clinicians often sat face to face with patients and focused on the patient with minimal computer use. Clinicians logged into the computer at the beginning of the visit or after listening to patients’ concerns. They typed towards the end of the visit, and made several brief gazes at the computer throughout the encounter. This might also support the notion that screen gaze is negatively correlated with a clinicians’ engagement in psychosocial question asking and emotional responsiveness (Booth et al., 2004). Two clinicians who used paper charts (in addition to EHRs) also actively faced the patient with minimal computer use. Interestingly, patients did not adjust their body to see the monitor; this might be because clinicians maintained a focus on the patient.
Figure 6.
Multiple snapshots from a technology withdrawal visit
4. Discussion and Implications
The purpose of this study was to identify and describe health information technology use for information sharing between patients and their care providers during clinical encounters. The qualitative results showed three technology-mediated information-sharing styles: active information sharing, passive information sharing, and technology withdrawal. Descriptions of the interactions in these visits were described. The quantitative results show that level of patient involvement with EHRs varies based on physicians’ information sharing styles.
Patient-centeredness has been an important goal for primary care environments and health practice in general (Bates & Bitton, 2010). Physicians’ patient-centred communication is assumed to stimulate patients’ active participation, thus leading to more effective and humane exchanges in the medical consultation (Zandbelt et al., 2006). Physicians’ facilitating behaviour was found to be positively associated with patients’ relative contribution to the conversation as well as patients’ active participation behaviour. EHRs introduce a “third party” into exam room interactions that reshapes the patient–physician encounter, alters the patient’s narrative, and diverts the physician’s attention away from the patient (Lown & Rodriguez, 2012). However, EHRs and other forms of health information technology hold the promise of enabling health care workers to provide more effective, more efficient, more coordinated, and safer care (Lown and Rodrigues, 2012). In particular, the application of HIT innovations should target patient-centred goals such as helping patients become more involved in their care, or “activated,” through sharing the EHRs more during the visit (Bates & Bitton, 2010). EHRs can also have a positive influence on clinical encounters because they allow doctors to share data displays, images, and salient information to enable shared decision making during the visit (Elwyn et al., 1999).
Differences were found in the amount of patient gaze at computer between the ‘active information sharing’ style and ‘passive information sharing’ style (18.15% and 11.20% of visit length). This may indicate that the clinician’s verbal invitation to share the monitor is integral to a patient’s desire to gaze at the computer. Involving patients by directly inviting them to view the computer screen also creates an environment for active listening (Wilcox et al., 2010). Showing the monitor to the patient is a recommended practice in patient-centred clinician training (Frankel et al., 2005). In addition, the relationship between ‘clinician gaze at computer’ and ‘visit length’ was explored. Significant correlation between ‘clinician gaze at computer’ with ‘visit length’ (F=77.871, p=0.000) was found; clinicians who spend a longer time gazing at the computer were more likely to have extended visit length. Active information sharing visits were significantly longer than the other two visit types (p= 0.002, p=0.035, respectively). This might be because active information sharing extends the discussion and may take more time. In particular, our findings show that patients asked physicians more questions during active sharing encounters. This lengthened the visit, but it also increased patient understanding and created a more collaborative relationship between patient and physician, leading to patient-centred care. Therefore, our study supports some previous research that indicates that the strong correlation between computer use and visit length indicates a patient-centred approach (Als, 1997), and it contradicts those previous studies which have found that integrating an EHR makes the visit more clinician-centred (Shachak and Reis, 2009).
According to recent literature, computer monitor sharing (shared EHR view with the patient) is described as an essential element of patient-centered care (Wilcox et al., 2010). Active information sharing might integrate the patient into the overall communication effectively and improve the shared decision making process (Almquist et al., 2009). Using visual aids is one of the strongest ways of explaining an issue to a patient effectively. Active information sharing is also proposed as a way of effective educating patients. Results show that when monitors are collaboratively shared with patients, patients gaze at the computer the most (18.15%). This may indicate that there is more information sharing because gaze at computer is a way of retrieving information. Some patients may wish to be involved in the decision process and see details about their current health, so for such motivated patients, the “active information sharing” strategy may be the best way for physicians to interact. Under these circumstances, active sharing can be a very effective way of creating patient centred visits, especially when certain content is involved (such as educating patients about a health condition). For this reason active information sharing is best for follow up visits, after a patient has already been diagnosed and when the patient is in need of information about how to best manage their condition or specifically for visits in which the main purpose is providing information to the patient. This style seems to actively involve the patient in asking for, receiving, and comprehending information.
Furthermore, technology withdrawal has both positive and negative implications based on clinicians’ work styles and the visit content. When the clinician focuses on the patient and minimizes the negative effect of computers on the communication, ‘technology withdrawal’ could be a positive use of the technology. In this case doctors might use a paper chart to take notes and keep a high level of eye contact, with body facing the patients. They tend to interact with EHRs at the breakdown periods, such as when the patient is moving to the exam table or changing his/her dress, etc. Technology withdrawal might be positive if the content of the visit requires a high level of empathy, leading doctors just to focus on the patient and not involve the computer in that sensitive interaction. In addition, some doctors would like to type notes about their diagnosis or ideas, but they do not want to show patients what is written into the EHR because of privacy reasons. These doctors might also follow a technology withdrawal style while inputting information. On the other hand, if the technology withdrawal strategy makes doctors disengage with the patient, this might affect patient outcomes negatively. Therefore, our findings show that technology withdrawal can also be very effective in certain circumstances, especially when the patient is sharing with the doctor a new medical condition or set of symptoms. (In other words, technology withdrawal can be most effective in preliminary visits, when the doctor’s job is primarily to listen carefully to the patient, rather than to provide information to the patient.) This is especially true if the patient’s concerns are very emotional or sensitive in nature.
In this study, the passive information sharing visits also showed that all patients have a certain degree of willingness to see the monitor even if it was not intentionally shared by the doctor (patient gaze at monitor =11.20%). However, this method is not as effective as active information sharing at providing information to the patient or actively involving the patient in shared decision making. In particular, our study did not find that passive information sharing extended the visit or increased the patient’s willingness to ask questions, so it did not contribute as well to patient-centred visits. This suggests that active information sharing is a better approach, especially when retrieving patient health related data from the EHRs and sharing information with patients.
The benefits and drawbacks of each information sharing style proposed in this study suggest new design approaches to EHRs. In particular, this study suggests that practitioners and patients would benefit from a more interactive system in which patients will be more involved, as well as a more simplified and standardized interface for data entry so physicians can spend minimal time typing during the visit. Both of these design changes would allow the medical practitioner to focus more on the patient during medical visits, promoting patient-centered care. Furthermore, one of the design suggestions might be to have separate patient displays, so physicians can share specific information with patients through that display. This will increase patient involvement and the active information sharing behaviour of doctors. This design might also address two essential concerns. The first one is related to privacy—some doctors do not want the patient to see what they type into the computer. The second one is related to the complexity of current EHR systems, which are designed for doctors and might be too complicated and difficult for some patients to understand. A separate patient display might provide clearer and more understandable information for patients, facilitating those doctors who would like to move from a passive information sharing style to a more active information sharing style, which can better promote patient-centred care. Another suggestion might be having patient portals for early data input available for patients in the waiting area. By allowing patients to enter their medical history and concerns directly into EHRs, this might save time for doctors and give them opportunity to review information right before patient comes in so it will minimize data entry and increases doctors’ current information about that particular patient.
This study also suggests some ideas for improved training of physicians in EHR use. If physicians are trained to recognize their own information sharing style, then they can actively choose either active information sharing or technology withdrawal, based on the purpose of the visit or patient needs. This way doctors can best set up the visit to facilitate either teaching the patient through active sharing or listening carefully and empathetically to the patient through technology withdrawal. Because our study suggests that passive information sharing is not as effective as either of these other two methods, training doctors in the active information sharing and technology withdrawal may help to avoid passive information sharing. This can lead to more patient-centred care.
Study limitations include the small sample of clinicians, limited participant diversity, and the limited type of visits. Of the eligible patients, the recruitment rate of the study was 47%. The recruitment rate varied across and between clinics depending on participants’ social statuses, educational backgrounds, willingness to contribute to science, and overall demographic characteristics of the clinic. Patients who chose not to participate may have different attitudes towards their clinician or HIT, and may have more complex health needs. The study clinics’ setting might not be representative of all primary care offices such as other clinics that may not have movable monitors. Finally, in the future there could be some sort of longitudinal study that would track things such as patient satisfaction, patients’ decisions to return to this same doctor or switch doctors, patients’ long-term health outcomes related to physicians’ information sharing style.
5. Conclusion
Future electronic record systems may incorporate a great deal of useful information that can be shared with patients. However, the features that contribute to HIT information sharing and the potential effects of information sharing are not well known. Understanding facilitators to HIT information sharing can inform health care work system design in various ways. For instance, new training guidelines for effective HIT use during the visit can be created to educate residents in medical schools, new technology design could provide easier visual data sharing functions during the visit, and finally optimized interactions could be advocated, so clinicians could employ best information sharing behaviours based on the context. This study describes different technology-use patterns clinicians employ to share information with patients. These patterns might have implications for new HIT design in medical settings. It is essential to identify effective strategies for integrating HIT use into clinician-patient interactions (Shachak and Reis, 2009). It is necessary to identify HIT designs which will support positive exam-room dynamics by providing information transparency during clinician–patient interactions (Chen et al., 2011). HIT design should also address optimal interactions between the clinician, patient, and computer. For instance, future design of HIT might have functions to help clinicians educate patients and share information easily with visual tools. Voice recognition, handwriting recognition, and touch screens might be alternative aids for data entry (Shachak and Reis, 2009). Therefore, these functions could enhance interactions and patient-centred communication by allowing the clinician to continue facing toward the patient. These functions also might increase mutually perceived personal connections during HIT use. Future studies should explore each technology-mediated information-sharing style with a larger sample of patients and doctors. Each style should also be explored specifically to observe the effect of styles on patient perception and outcomes.
Acknowledgements
This research was supported by grant 1UL1RR025011 from the Clinical and Translational Science Award (CTSA) program of the National Center for Research Resources (NCRR), National Institutes of Health (NIH). We thank undergraduate research assistants who assisted with data analysis and graduate research assistants who assisted with data collection.
REFERENCES
- Ahern DK, Woods SS, Lightowler MC, Finley SW, Houston TK. Promise of and potential for patient-facing technologies to enable meaningful use. American Journal of Preventive Medicine. 2011;40:S162–S172. doi: 10.1016/j.amepre.2011.01.005. [DOI] [PubMed] [Google Scholar]
- Als AB. The desk-top computer as a magic box: patterns of behaviour connected with the desk-top computer; GPs’ and patients’ perceptions. Family Practice. 1997;14:17–23. doi: 10.1093/fampra/14.1.17. [DOI] [PubMed] [Google Scholar]
- Almquist JR, Kelly J, Bromberg J, Bryant SC, Christianson T, Montori V. Consultation room design and the clinical encounter: the space and interaction randomized trial. Health Environments Reseach & Design Journal. 2009;3:41–78. doi: 10.1177/193758670900300106. [DOI] [PubMed] [Google Scholar]
- Bakeman R. Handbook of research methods in social and personality psychology. Cambridge,UK: Cambridge University Press; 2000. Behavioural observation and coding; pp. 138–159. [Google Scholar]
- Bates DW, Bitton A. The future of health information technology in the patient-centered medical home. Health Affairs. 2010;29:614–621. doi: 10.1377/hlthaff.2010.0007. [DOI] [PubMed] [Google Scholar]
- Beck R, Daughtridge R, Sloane P. Physician-patient communication in the primary care office: a systematic review. The Journal of the American Board of Family Medicine. 2002;15:25–38. [PubMed] [Google Scholar]
- Booth N, Robinson P, Kohannejad J. Identification of high-quality consultation practice in primary care: the effects of computer use on doctor-patient rapport. Informatics in Primary Care. 2004;12:75–83. doi: 10.14236/jhi.v12i2.111. [DOI] [PubMed] [Google Scholar]
- Chaudhry B, Wang J, Wu S, Maglione M, Mojica W, Roth E, Morton SC, Shekelle PG. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Annals of Internal Medicine. 2006;144:E-12–E-22. doi: 10.7326/0003-4819-144-10-200605160-00125. [DOI] [PubMed] [Google Scholar]
- Chen Y, Ngo V, Harrison S, Duong V. Unpacking exam-room computing: negotiating computer-use in patient-physician interactions In Proceedings of CHI 2011, ACM Press (2011), 183–192. ACM. 2011:3343–3352. [Google Scholar]
- Creswell JW. Qualitative inquiry & research design: Choosing among five approaches. London: Sage Publications Inc.; 2007. [Google Scholar]
- Creswell JW. Research design: Qualitative, quantitative, and mixed methods approaches. London: Sage Publications Inc.; 2009. [Google Scholar]
- Creswell JW, Klassen LAC, Clark VLP, Smith LKC. Best practices for mixed methods research in the health sciences. Washington, DC: Office of Behavioral and Social Sciences Research; 2011. Retrieved from http://obssr.od.nih.gov/scientific_areas/methodology/mixed_methods_research/pdf. [Google Scholar]
- Elwyn G, Edwards A, Kinnersley P. Shared decision-making in primary care: the neglected second half of the consultation. The British Journal of General Practice. 1999;49:477–482. [PMC free article] [PubMed] [Google Scholar]
- Frankel R, Altschuler A, GEORGE S, Kinsman J, Jimison H, Robertson NR, Hsu J. Effects of Exam-Room Computing on Clinician-Patient Communication: A Longitudinal Qualitative Study. Journal of General Internal Medicine. 2005;20:677–682. doi: 10.1111/j.1525-1497.2005.0163.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helman C. Primary care research: Traditional and innovative approaches. London: Sage Publications Inc.; 1991. Research in primary care: the qualitative approach. [Google Scholar]
- Holden RJ. Theoretical Issues in Ergonomics Science, First published on: 28 March 2011 (iFirst) 2011. Social and personal normative influences on healthcare professionals to use information technology: towards a more robust social ergonomics. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivankova NV, Creswell JW, Stick SL. Using mixed-methods sequential explanatory design: From theory to practice. Field Methods. 2006;18:3–20. [Google Scholar]
- Karsh BT, Beasley J, Hagenauer ME. Are electronic medical records associated with improved perceptions of the quality of medical records, working conditions, or quality of working life? Behaviour and Information Technology. 2004;23:327–335. [Google Scholar]
- Lelievre S, Schultz K. Does computer use in patient-physician encounters influence patient satisfaction? Canadian Family Physician. 2010;56:e6–e12. [PMC free article] [PubMed] [Google Scholar]
- Lown BA, Rodriguez D. Lost in Translation? How electronic health records structure communication, relationships, and meaning. Academic Medicine. 2012;87:392–394. doi: 10.1097/ACM.0b013e318248e5ae. [DOI] [PubMed] [Google Scholar]
- Margalit RS, Roter D, Dunevant MA, Larson S, Reis S. Electronic medical record use and physician-patient communication: an observational study of Israeli primary care encounters. Patient Education and Counseling. 2006;61:134–141. doi: 10.1016/j.pec.2005.03.004. [DOI] [PubMed] [Google Scholar]
- Miles MB, Hubberman AM. Data management and analysis methods. In: Denzin NK, Lincoln YS, editors. Qualitative data analysis: An expanded sourcebook. 2nd. CA: Thousand Oaks: 1994. [Google Scholar]
- Montague E, Xu J, Chen P, Asan O, Barrett BP, Chewning B. Modeling Eye Gaze Patterns in Clinician-Patient Interaction With Lag Sequential Analysis. Human Factors. The Journal of the Human Factors and Ergonomics Society. 2011;53(5):502–516. doi: 10.1177/0018720811405986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearce C, Dwan K, Arnold M, Phillips C, Trumble S. Doctor, patient and computer--A framework for the new consultation. International Journal of Medical Informatics. 2009;78:32–38. doi: 10.1016/j.ijmedinf.2008.07.002. [DOI] [PubMed] [Google Scholar]
- Piper AM, Hollan JD. Supporting medical communication for older patients with a shared touch-screen computer. International Journal of Medical Informatics. 2011 doi: 10.1016/j.ijmedinf.2011.03.005. [DOI] [PubMed] [Google Scholar]
- Plano Clark VL. The adoption and practice of mixed methods: US trends in federally funded health-related research. Qualitative Inquiry. 2010;16:428–440. [Google Scholar]
- Pratt W, Reddy MC, Mcdonald DW, Tarczy-Hornoch P, Gennari JH. Incorporating ideas from computer-supported cooperative work. Journal of Biomedical Informatics. 2004;37:128–137. doi: 10.1016/j.jbi.2004.04.001. [DOI] [PubMed] [Google Scholar]
- Robles E, Nass C, Kahn A. The social life of information displays: How screens shape psychological responses in social contexts. Human-Computer Interaction. 2009;24:48–78. [Google Scholar]
- Roter D, Frankel R, Hall J, Sluyter D. The expression of emotion through nonverbal behaviour in medical visits. Journal of General Internal Medicine. 2006;21:S28–S34. doi: 10.1111/j.1525-1497.2006.00306.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savage J. Ethnography and health care. British Medical Journal. 2000;321:1400–1402. doi: 10.1136/bmj.321.7273.1400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shachak A, Hadas-Dayagi M, Ziv A, Reis S. Primary care physicians’ use of an electronic medical record system: a cognitive task analysis. Journal of general internal medicine. 2009;24:341–348. doi: 10.1007/s11606-008-0892-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shachak A, Reis S. The impact of electronic medical records on patient-doctor communication during consultation: a narrative literature review. Journal of Evaluation in Clinical Practice. 2009;15:641–649. doi: 10.1111/j.1365-2753.2008.01065.x. [DOI] [PubMed] [Google Scholar]
- Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ: Canadian Medical Association Journal. 1995;152:1423–1433. [PMC free article] [PubMed] [Google Scholar]
- Theadom A, De Lusignan S, Wilson E, Chan T. Using three-channel video to evaluate the impact of the use of the computer on the patient-centredness of the general practice consultation. Informatics in Primary Care. 2003;11:149–156. doi: 10.14236/jhi.v11i3.563. [DOI] [PubMed] [Google Scholar]
- Unruh KT, Skeels M, Civan-Hartzler A, Pratt W. Proceedings of CHI 2010. ACM Press; 2010. Transforming clinic environments into information workspaces for patients; pp. 183–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ventres W, Kooienga S, Marlin R, Vuckovic N, Stewart V. Clinician style and examination room computers: a video ethnography. Family Medicine. 2005;37:276–281. [PubMed] [Google Scholar]
- Wang H, Blevis E. Concepts that support collocated collaborative work inspired by the specific context of industrial designers. ACM. 2004:546–549. [Google Scholar]
- Wilcox L, Morris D, Tan D, Gatewood J. Proceedings of CHI 2010. ACM Press; 2010. Designing patient-centric information displays for hospitals; pp. 2123–2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zandbelt L, Smets E, Oort F, Godfried M, Haes H. Patient participation in the medical specialist encounter: Does physicians’ patient-centred communication matter? Patient Education and Counseling. 2006;65:396–406. doi: 10.1016/j.pec.2006.09.011. [DOI] [PubMed] [Google Scholar]