Abstract
Context
Many state and local areas are affected by the national epidemic of drug-related mortality, which recently has shown signs of a rising licit-to-illicit drug death ratio. Appropriate local public health surveillance can help to monitor and control this epidemic.
Objective
Using our state as an example, we sought to illustrate how to describe the changes in drug death rates, causes, and circumstances. In contrast to most other surveillance reports, our approach includes both drug-induced and drug-related deaths and both demographic and socioeconomic decedent characteristics.
Design
Cross-sectional study.
Setting
All residents of the State of Wisconsin.
Participants
Decedents from 1999–2008.
Main outcome measure
Annual numbers and population-based rates of deaths due to drugs, including both identified and unidentified drugs. Information was obtained from death certificates with any of approximately 270 underlying, immediate, or contributing cause of death codes from the International Classification of Diseases 10th Revision.
Results
Drug-related death rates increased during much of the 10-year study period, and the ratio of male to female deaths rose. The median age at death from drug-related causes was 43 years. Opioid analgesic poisoning surpassed cocaine and heroin poisoning as the most frequent type of fatal drug poisoning. Of all 4828 deaths from drug-related causes--virtually all of which were certified by a county medical examiner or coroner--3,410 (71%) were unintentional, and 1,053 (22%) were suicide. The unintentional-to-suicide death rate ratio grew from 1.6 to 3.5 during the study period. Methadone-related deaths increased from 10 in 1999 to 118 in 2008 (1080%), while benzodiazepine-related deaths rose from 23 to 106 (361%).
Conclusions
Although premature deaths from drug use and abuse continue to rise, in some states even surpassing motor vehicle crash deaths, multiple cause of death information from death certificates is available to monitor their occurrence and nature and to inform selection of prevention strategies.
Keywords: Death certificates, cause of death, narcotics poisoning, drug toxicity/epidemiology/mortality, population surveillance/methods
INTRODUCTION
The United States epidemic of drug-related deaths began in the 1960s (1). After decades when the majority of drug-related deaths were caused by illicit drug use, a rise in deaths from licit drug use has prompted new assessments of trends in drug-related mortality [2].
To achieve the Healthy People 2020 objective of reducing drug-related deaths by 10% [3], state and local groups will need information on mortality trends in small areas to develop strategies for disease prevention and treatment. Among the 50 states, methadone-related poisoning deaths range from about 1 to 4 per 100,000 population [4], and opioid analgesic-related poisoning deaths range from about 2 to 16 per 100,000 population [5].
In a few cases, medical examiner and death certificate records have been used to examine changes in drug mortality rates, causes, and circumstances. For example, medical examiner records have been used to describe multiyear trends for heroin death in an Oregon county (6), opiate death in a Washington county (7), methadone death in North Carolina (8), methadone and heroin death in Florida (9), and death from various drugs in Virginia (10), New Mexico (11), and West Virginia (12). Similarly, death certificate records have been used to describe multiyear trends in prescription opioid death in Washington (13) and the United States (5) and in death from various drugs in the United States (2, 4, 14–17). Finally, death certificate and medical examiner or other records have been combined to describe multiyear trends for cocaine death in 25 cities (18), heroin and other drug death in New Mexico (19), and death from various drugs in 13 states (20).
Although the U.S. drug death epidemic is now half a century old, the related public health surveillance is still under development. Using information from certificates of death that occurred during 10 recent years in a Midwestern state with a population of 5+ million inhabitants, our study sought to illustrate how to assess the changes in drug death rates, causes, and circumstances. In contrast to most previous reports, our approach includes both drug-induced and drug-related deaths and both demographic and socioeconomic decedent characteristics.
METHODS
Study population and setting
The study population was all residents of Wisconsin, a Midwestern state with a year 2000 census population of 5,363,675, who were certified to have died of a drug-related cause from 1999 to 2008. Drugs may be implicated as a cause of death or disease for conditions that are (a) directly related to substance abuse, e.g., drug dependence or (b) indirectly related to substance abuse as a contributory but not a necessary cause, e.g., suicide [21]. We purchased from the State of Wisconsin Vital Records Office a computer file of data on deaths meeting our study case definition. Case deaths were those whose death certificate had a cause of death – either underlying, immediate, or contributing-- that matched one or more of approximately 270 disease or drug codes from the World Health Organization’s 10th Revision of the International Classification of Diseases (ICD-10) (22). These 270 codes were chosen to identify deaths due to all types of drugs (except alcohol and tobacco) whether they are named or unnamed and licit or illicit, as in the study by Paulozzi [2].
Deaths were limited to those occurring from 1999—the first year that deaths were fully coded using ICD-10 rubrics, thus avoiding problems with cause of death codes in older versions of the ICD--through 2008, the latest year that death records were available when we obtained them in March 2010. To prepare the electronic data file for this study, the State Vital Records Office screened more than 450,000 deaths of Wisconsin residents in its electronic database and abstracted 18 elements on each case death.
The study was conducted to promote public health surveillance under a confidentiality and data use agreement between the Wisconsin Department of Health Services Vital Records Office and the University of Wisconsin-Whitewater Department of Occupational and Environmental Safely and Health. Before providing the death file, the state guardian removed personal identifiers such as decedents’ name and date of birth. The UW-Whitewater Office of Research and Sponsored Programs waived this study, which involved no living participants, from Institutional Review Board approval.
Outcome measures
We chose death certificates as our study data source because they are a valid source of information--comparable at national, state, and local levels—which is used to identify major health problems, set priorities, and monitor progress [23]. The study outcomes were deaths that were classified as “drug-induced” or “drug-related” (14) by the National Center for Health Statistics (5, 24) [see list of 270 codes in Appendix 1]. They included deaths from drug poisoning, mental disorders due to drug-taking, and drug-induced diseases (16). Drug-poisoning deaths result from overdoses of a drug, being given the wrong drug, taking the wrong drug in error, or taking a drug inadvertently [4]. Each death certificate allows up to 20 causes of death, including one “underlying” cause, one “immediate” cause, and up to 18 “contributing” causes (25). The certificate defines the underlying cause as “the disease or injury that initiated the chain of events that led directly and inevitably to death,” the immediate cause as “the final disease, injury, or complication directly causing death,” and the contributing cause as “all other significant diseases, conditions, or injuries that contributed to death but which did not result in the underlying cause of death.” State statute allows up to 21 days from the date of death for notification to the State Registrar.
Deaths with drugs as the underlying cause are called “drug-induced deaths,” while deaths with drugs as any cause are called “drug-related deaths” [14].
In the United States, while physicians certify most deaths, medical examiners and coroners are responsible for investigating and certifying the cause and manner of unnatural and unexplained deaths, including homicides, suicides, unintentional injuries, drug-related deaths, and other deaths that are sudden or unexpected (26, page 8). Wisconsin is one of 18 states with a “mixed system” in which some counties are served by coroners and others by medical examiners (26, page 8 and http://www.dhs.wisconsin.gov/vitalrecords/pdf/cormemap201006.pdf
Wisconsin Coroners and Medical Examiners, June 2010, Map of Counties, accessed 2 Feb 2011). According to Wysowski (15), certifiers may--and, if appropriate, should--designate one or more particular drugs as the underlying, immediate, or contributing cause of death. It is within the certifier’s purview to judge whether the absorbed drug dose was sufficient to be lethal.
Exposure measures
In addition to all ICD-10 cause of death codes for all study case deaths, we obtained information from the state death file on decedent risk factors, including age, sex, race, education, and county of residence. We assigned each county of residence as “metropolitan” or “non-metropolitan” according to a county-level urbanization classification developed after the 2000 census by the National Center for Health Statistics for use in studying the association between urbanization and health [27]. The year 2000 population census county median household income was used to determine each decedent’s residence county average income (28).
Data analysis
“Deaths due to chronic diseases,” as noted by Israel [29], “are often not well characterized by a single cause.” As explained above, use of the National Center for Health Statistics list of approximately 270 disease or drug codes from the 10th Revision of the International Classification of Diseases (ICD-10) (5, 24) [see list of codes in Appendix 1] enabled us to select case deaths reflecting the entire mortality burden from drug use, including both “drug-induced” and “drug-related” deaths. Using a “multiple cause of death” approach [29], we analyzed all drug deaths regardless of whether a drug was the underlying, immediate, or contributing cause of death [19].
After receiving the state drug-related death data file, we modified it to fit our study aim. To determine the number of mentions of unique types and names of drugs, we identified and deleted for each decedent all duplicates of ICD-10 codes either (a) within the “contributing” causes or (b) between the “contributing” causes and either the “underlying” or the “immediate” cause of death (25). After deleting these duplicates, we tabulated the proportion of all deaths that were caused, directly or indirectly, by type and of drug based on codes in the T series of Chapter XIX “Injury, poisoning and certain other consequences of external causes” of the ICD–10 [see Appendix 1 list of codes]. For all deaths with poisoning by and exposure to drugs, medicaments and biological substances as the “underlying” cause--which includes deaths with an ICD-10 code of X40–X44, X60–X64, X85, or Y10–Y14--we summarized the recorded manner of death, including unintentional (formerly called “accidents”), suicide, homicide, and undetermined intent.
Wisconsin’s population grew little, only 6%, from 2000 to 2008 [30], and we used denominator data from the year 2000 Wisconsin population census to calculate annual death rates per 100,000 population by levels of the study exposure measures. In the state computer file that we obtained, data were missing on race of four of 4828 decedents and on education level of 32 of 4387 decedents age 25 or over.
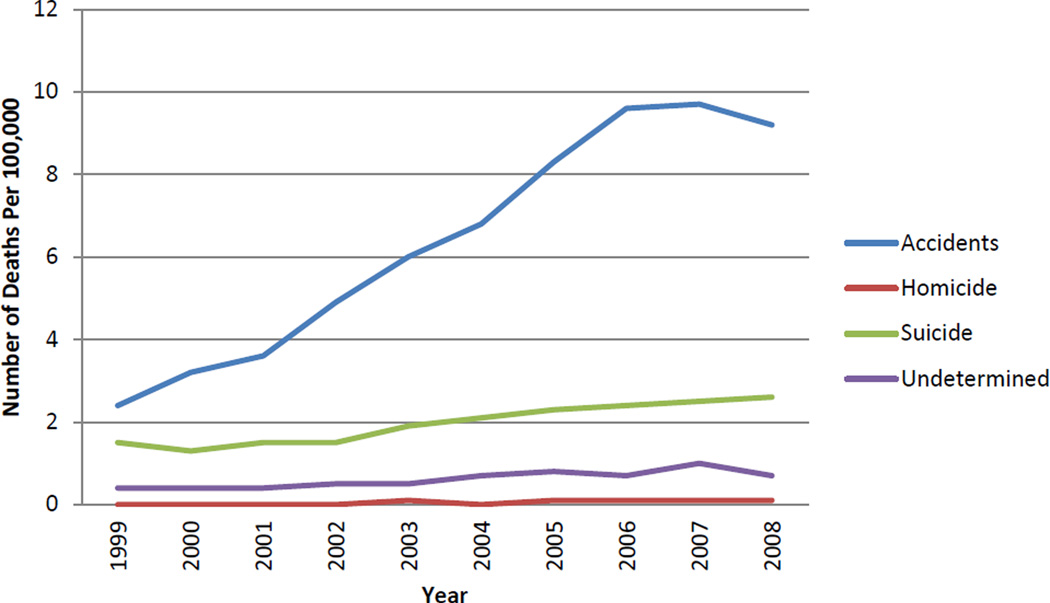
RESULTS
From 1999 to 2008, 4828 residents of Wisconsin died from drug-related causes, and opioid analgesic poisoning surpassed cocaine and heroin poisoning. The majority of all drug deaths, 71% (3410 of 4828), were unintentional (formerly called “accidents”), followed by suicide, 22% (1,053 of 4828), homicide, 1% (34 of 4828), and undetermined intent, 7% (331 of 4828). Unintentional deaths ranked highest in every year, and the death rate ratio of unintentional deaths to suicide deaths rose from 1.6 in 1999 to 3.5 in 2008 (Fig 1).
Fig 1.
Drug Death Rates by Manner and Year
The median age at death from drug-related causes was 43 years, with three-fourths of all 4828 deaths occurring in persons aged 25 to 54. One-half of all drug-related deaths occurred in four counties that have one-third of the state’s total population. Age-specific, drug-related death rates per 100000 population were lowest in persons aged 0–19 years old—0 (n=4 deaths) in 1999 and 2 (n=28 deaths) in 2008—and highest in persons aged 45–64 years old—6 (n=67 deaths) in 1999 and 25 (n=299 deaths) in 2008.
Of all 4828 study deaths, drug poisoning was the underlying cause of 3962 (82%) deaths, while injuries, poisonings, and certain other consequences of external causes were the immediate cause of 3800 (79%) deaths (see Appendix 2 for counts of deaths by ICD-10 underlying and immediate cause groups). About one-half (2290 of 4828) of all deaths had three (Range 0 to 11) unique contributing cause of death codes, in addition to one underlying cause of death code and one immediate cause of death code, after deletion of duplicate codes (see Methods section above). Of the 4828 deaths, a coroner or medical examiner certified all but 14 deaths, and 3826 deaths, or 79%, were autopsied, a rate 10-fold higher than the 8% autopsy rate of the total of some 450,000 deaths in Wisconsin during the study period.
Drugs listed as the immediate or contributing cause of the 4828 study deaths included: heroin, methadone, and other opioids (2052 deaths or 42%); cocaine (1017 deaths or 21%); benzodiazepines and other sedatives, hypnotics, and antiepileptics (890 deaths or 18%); other specified non-narcotic drugs (682 deaths or 14%); and other and unspecified drugs (2023 deaths or 42%) (Table 1). Polydrug use documented by multiple cause of death codes leads the sum of drug type percentages to exceed 100%. From 1999 to 2008, annual deaths from methadone increased from 10 to 118, and annual deaths from benzodiazepines increased from 23 to 106.
Table 1.
Number of poisoning deaths by drug type mentioned: Wisconsin, 1999–2008
| ICD-10 | Substance | Total deaths | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | % change 1999–2008 | % change 2007–2008 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| code | ||||||||||||||
| T40.1 | Heroin | 303 | 17 | 31 | 20 | 26 | 24 | 19 | 32 | 28 | 36 | 70 | 312 | 94 |
| T40.2 | Codeine, morphine, other opioids | 1101 | 39 | 49 | 68 | 95 | 96 | 103 | 134 | 161 | 182 | 174 | 346 | −4 |
| T40.3 | Methadone | 648 | 10 | 19 | 20 | 39 | 39 | 71 | 74 | 118 | 140 | 118 | 1080 | −16 |
| T40.4 | Other synthetic narcotics | 377 | 16 | 22 | 24 | 26 | 38 | 40 | 50 | 54 | 55 | 52 | 225 | −5 |
| T40.5 | Cocaine | 1017 | 59 | 57 | 63 | 79 | 101 | 112 | 132 | 163 | 158 | 93 | 58 | −41 |
| T42.4 | Benzodiazepines | 653 | 23 | 32 | 37 | 51 | 52 | 77 | 72 | 92 | 111 | 106 | 361 | −5 |
| T43.0 | Tricyclic and tetracyclic antidepressants | 332 | 24 | 23 | 24 | 31 | 35 | 45 | 36 | 43 | 42 | 29 | 21 | −31 |
| T43.2 | Other and unspecified antidressants | 401 | 14 | 19 | 23 | 37 | 21 | 50 | 48 | 55 | 71 | 63 | 350 | −11 |
| T50.9 | Other and unspecified drugs | 2023 | 78 | 120 | 121 | 191 | 153 | 200 | 240 | 276 | 302 | 342 | 338 | 13 |
NOTES: Table excludes drug T codes with fewer than 300 mentions during the 10 year study period. Data in table include 6855 (84%) of the 8160 unduplicated mentions of T codes in the study. Because table includes multiple causes, the "total deaths" exceeds the 4828 deaths in the study.
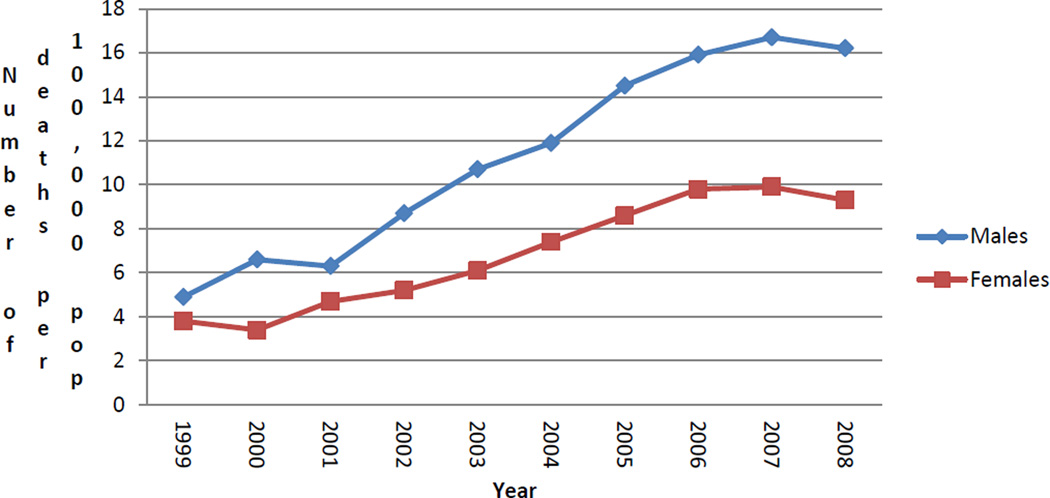
Per capita drug-related death rates increased during much of the study period, and the disparity by gender widened (Fig 2). While in 1999 drug use led to death in 130 men and 104 women—a 25% excess in men, in 2008 it had this effect in 429 men and 252 women—a 70% excess in men.
Fig 2.
Drug Death Rates by Sex and Year
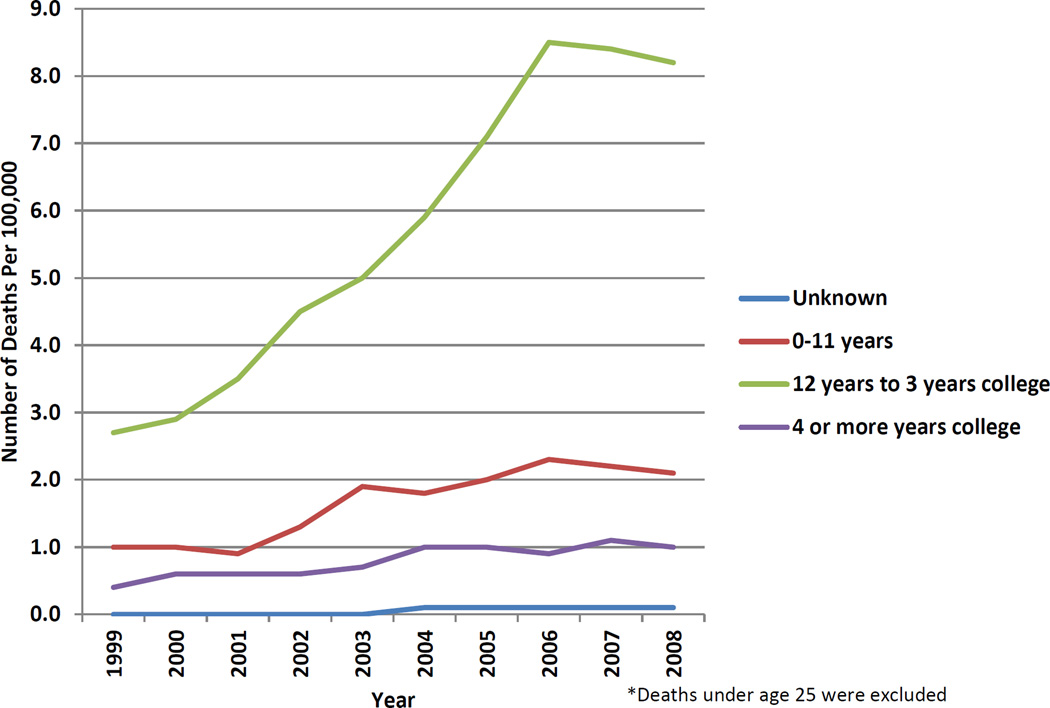
Of all drug deaths in persons aged 25 or older, the majority, 69% (3046 of 4387), occurred in persons who completed high school but not college, and 20% (884 of 4387) occurred in persons with 0–11 years of school but not high school completion. The rate ratio of deaths in high school completers to non-completers rose from 2.7 in 1999 to 3.9 in 2008 (Fig 3).
Fig 3.
Drug Death Rates by Education and Year
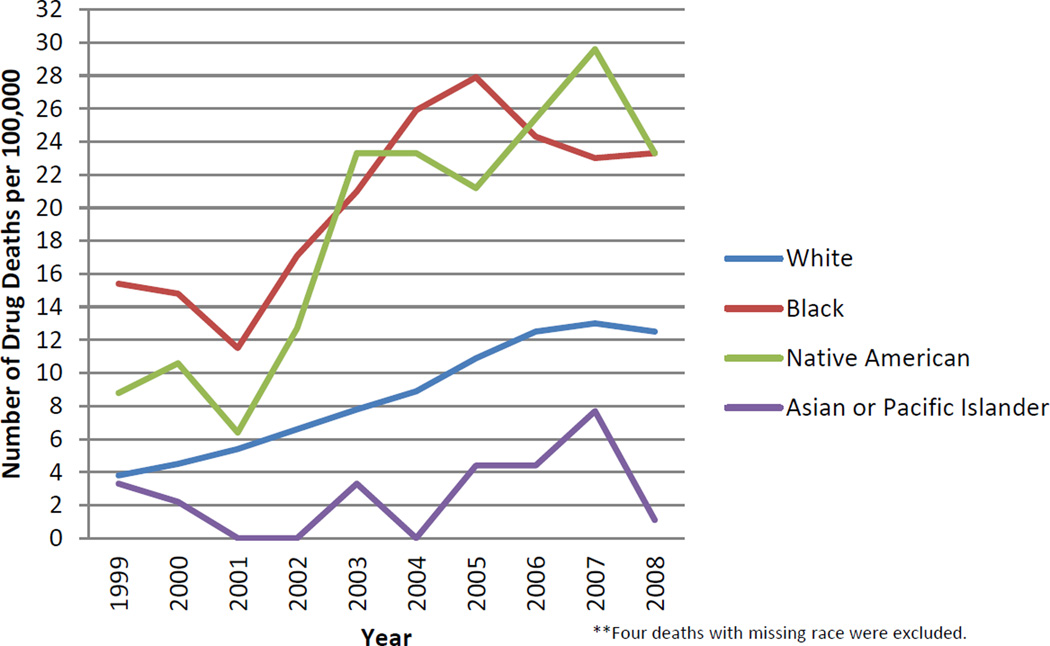
Two racial groups in Wisconsin--black and Native American residents--have drug death rates that are twice as high as those in white residents. In 2008 the number of drug deaths per 100,000 population was 23 in blacks (71 deaths of 304460 population) and 23 in Native Americans (11 deaths of 47228 population), while it was 12 in whites (597 deaths of 4769857 population) (Fig 4). For drug-related deaths, the average Native American dies four years younger than the average black or white. (Only one study death occurred in 2008 among the state’s 90393 Asian and Pacific Islander residents.)
Fig 4.
Drug Death Rates by Race and Year
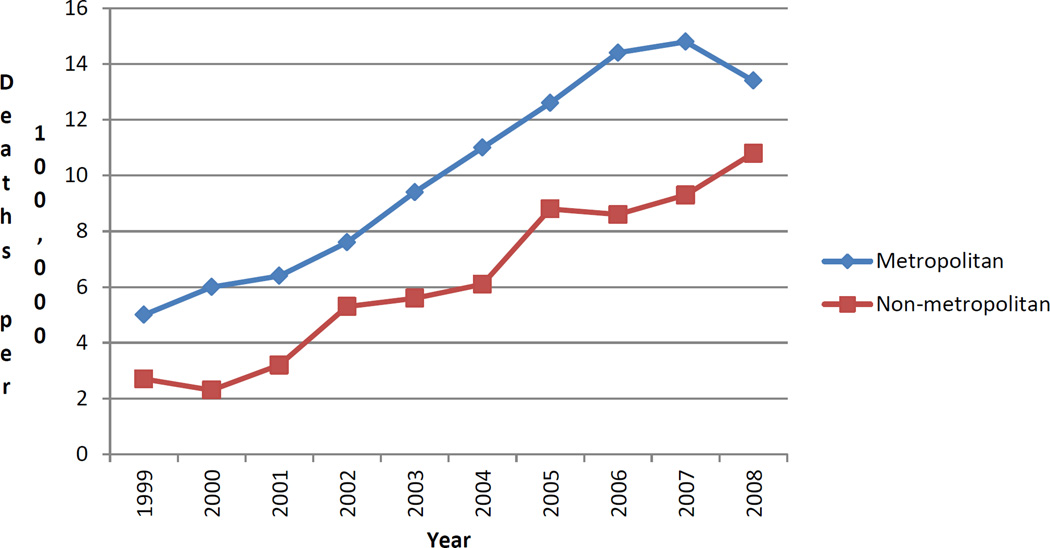
Throughout the 10 study years, drug death rates were higher in metropolitan areas than in non-metropolitan areas (Fig 5). In the final year, the rates moved closer together, with drug deaths per 100,000 population of 13 in metropolitan areas (520 deaths of 3868673 population) and 11 in non-metropolitan areas (161 deaths of 1495002 population).
Fig 5.
Drug Death Rates by Residence and Year
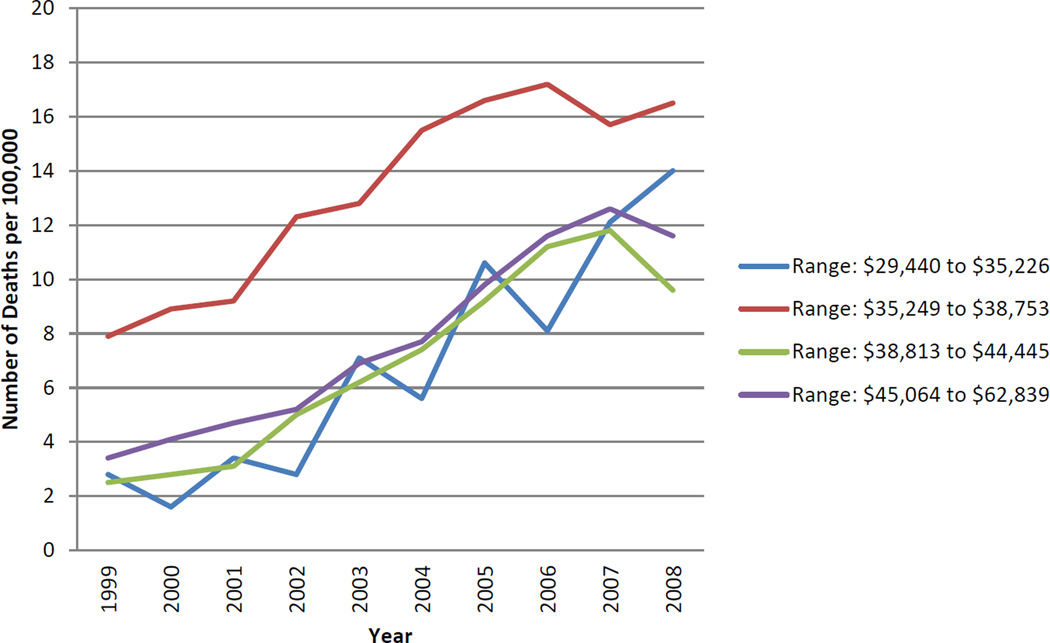
In all quartiles of county median household income (1999 dollars), drug death rates climbed throughout the study period (Fig 6). The rate of drug deaths per 100000 population was the highest in residents of the counties in the second lowest quartile of annual median household income. In some years, drug death rates in this quartile were double the death rates of the other quartiles.
Fig 6.
Drug Death Rates by Household Income and Year
When deaths related to benzodiazepines (n=653) were analyzed separately from all drug-related deaths (n=4828), the distributions by manner, sex, education, and household income were similar (data not shown). While black and Native American residents have overall drug death rates twice as high as those in white residents, the benzodiazepine death rates of these three racial groups were indistinguishable. Also, while during the study period total drug death rates in metropolitan areas and in non-metropolitan areas moved closer together, benzodiazepine death rates in these areas moved farther apart.
DISCUSSION
Using information from state death certificates, including all listed causes of death, we have documented a method for public health surveillance of drug-related mortality, an American epidemic now in its sixth decade. “Increasingly,” explained a university health service physician early in the epidemic, “people are unwilling to accept even minor discomforts and look to drugs for solutions” [31]. As has been observed for the nation as a whole [2], opioid analgesic poisoning has recently surpassed cocaine and heroin poisoning as the most frequent type of fatal drug poisoning in Wisconsin. During our 10 year study, annual deaths increased 10-fold from methadone and 3-fold from benzodiazepines. Wisconsin drug-related decedents are disproportionately middle-aged, male, non-white, non- college graduates, and residents of metropolitan areas of modest household income.
Study findings
Although states differ in the data sources and methods they use for drug-related mortality surveillance, their findings can be compared and contrasted with our results. Similar to our findings, four-fifths of drug overdose deaths in Virginia from 1997–2003 [10] and of poisoning deaths in New Mexico from 1989–1998 [19] were unintentional, while one-fifth of such deaths were suicidal. Methadone death rates increased five-fold during 4 years in North Carolina [8], three-fold during 5 years in Florida [9], and ten-fold during 10 years in Wisconsin. While heroin deaths rose in New Mexico [19] and Wisconsin, they fell in Florida [9]. High school graduates comprise similar proportions of drug decedents in Wisconsin, 69%, and Virginia, 64% [10]. (The proportions are probably inflated because death certificates tend to report people who did not graduate from high school as high school graduates (32).) Nearly one-half of decedents from drug overdose in Virginia from 1997–2003 were unemployed –with men more often unemployed than women--(10), and deaths from prescription opioids in Washington State during 2004–2007 occurred in 31 per 100,000 Medicaid enrollees versus 4 per 100,000 non-Medicaid enrollees [13], findings which are not inconsistent with the higher rates of male and of modest income drug deaths in our Wisconsin series. “Fatal drug overdoses are no longer a predominantly urban phenomenon,” concluded Paulozzi after observing U.S. metropolitan and non-metropolitan drug poisoning rates almost equalize in 2004 [17]. In Wisconsin, drug death rates remain higher in metropolitan areas than in non-metropolitan areas, as they did in New Mexico from 1994 to 2003, including when decedents’ residence was reanalyzed by class of drugs [11]. In contrast, of drug overdose deaths in western Virginia from 1997 to 2003, the rural rate of 11 deaths exceeded the metropolitan rate of 7 deaths, per 100,000 population [10].
Study implications
Variation in drug availability and use by state supports the suggestion by Mueller et al [11] that each jurisdiction needs to produce its own surveillance report to characterize this vexing social problem. Although the situation in each state will be unique, some general statements apply to all. One, both prevention and treatment approaches, which in the substance use field are somewhat intertwined, must be part of the solution. Two, effective control of substance use requires intersectoral action conducted at local, state, national, and international levels. Three, needed follow-up actions based on results from drug-related mortality surveillance are likely to include interventions in both clinical and community settings to reduce drug use and harm and to improve the cause-of-death certification. Four, substance use research, both basic and applied, will continue to be necessary.
Extensive professional experience and study have produced a list of risk factors for and partial solutions to the drug-related mortality epidemic [33–38]. Strategies in clinical settings include risk assessment and management, individual risk reduction, access to emergency and other health services, prescription drug monitoring programs, improved tools to screen patient pain, significant increases in drug treatment funding, access to opioid antagonists such as naloxone and naltrexone, drug treatment including opioid substitution programs, clean needle distribution to drug users, and first aid training for drug users. Strategies in public health settings include outreach and peer education, drug demand reduction programs, disease surveillance systems, calculation of the true population at risk for drug deaths, standardized periodic state reports on the nature and level of death certificate querying, optimal use of the ICD-10 classification, standardization of death certification for poisoning [26, page 4], building formal relationships between public health agencies and coroner and medical examiner offices [39], and applied research to improve knowledge of the risk factors for drug death.
One example of useful action is the research from North Carolina showing the source of methadone at the death scene was a tablet form used in pain treatment instead of the type of methadone used in drug treatment [26, page 17]. The dramatic rise in methadone-related deaths has attracted the attention of federal safety and health agencies. In a public health advisory issued in 2006, the U.S. Food and Drug Administration acknowledged that methadone can cause death due to respiratory depression and cardiac dysrhythmias, especially in patients newly starting methadone for pain control, and instituted lower dosing regimens for the treatment of pain [40]. A team of injury scientists from the U.S. Centers for Disease Control and Prevention has recommended additional changes, including nonuse of methadone for mild or acute pain, headache or low back pain, or as a first choice pain reliever for chronic noncancer pain [41].
However, because health behaviors and socioeconomic factors are independent determinants of mortality [42], even if public health policies and interventions that focus on individual risk behaviors succeed in reducing the disparity in risk behaviors by income, the residents of Wisconsin’s poorer counties are likely to continue to be at higher risk of dying from drug use than are residents of other counties.
Study strengths and limitations
Our study has several strengths. We used “that hardest of end points, death” [43] as the study outcome, a data source, the state death certificate, which is population-based and available for many years in all 50 states [23], a case definition of drug-related deaths based on the underlying, immediate, and contributing causes [44], deaths with a low rate of manner-undetermined and a high rate of autopsy, and identification of key socioeconomic correlates of drug-related death. Our study also has some limitations. Even after experts query the certifying physician about ambiguous or incomplete medical information on death certificates, drugs still seem to be under-reported as causes of death [45]. Death certificates do not record the source of the drugs involved, the purpose for which the drug was used, the decedent’s drug use history, the specific type or name of all of the drugs involved [46], whether the drug use was legal or illegal, or whether the drug was injected, smoked, or swallowed [6]. Finally, death certificate information that was not entered into the electronic database, such as decedents’ occupation and industry, was not available for analysis of social class. Because some ICD-10 cause of death codes mix legal and illegal drugs together [15], we do not know with certainty whether prior claims that licit drugs have replaced illicit drugs as the leading cause of U.S. fatal drug poisoning [2, 16] applies in Wisconsin.
Conclusion
Drug use and abuse lead to substantial premature mortality, especially in black and Native American middle-aged men. With drug-related deaths surpassing motor vehicle crash deaths in some states [16], including Wisconsin where the 681 drug-related deaths exceeded the 627 motor vehicle crash deaths in 2008 [47], this epidemic remains out of control. We show how to use multiple cause of death information from death certificates to monitor state rates, causes, and circumstances of drug-related deaths over time.
Supplementary Material
ACKNOWLEDGEMENTS
We thank Joyce Knapton, Wisconsin Department of Health Services Research Analyst, for assistance with obtaining and understanding death certificate information and Michael M. Miller, MD, Randy Brown, MD, PhD, James F. Cleary, MD, Aaron M. Gilson, PhD, and David E. Joranson, MSSW for their comments on an earlier draft of the manuscript.
This research was supported by University of Wisconsin-Whitewater through a 2010 Graduate Research Grant to Mieko L. Yokoi-Shelton and a 2010 College of Education and Professional Studies Summer Research Award to David L. Nordstrom.
APPENDIX 1
International Classification of Diseases, 10th Revision (ICD 10) cause of death codes for this study
Causes of death attributable to drug-induced mortality are these ICD–10 codes [24, page 120]:
D52.1, Drug-induced folate deficiency anemia; D59.0, Drug-induced hemolytic anemia; D59.2, Drug-induced nonautoimmune hemolytic anemia; D61.1, Drug-induced aplastic anemia; D64.2, Secondary sideroblastic anemia due to drugs and toxins; E06.4, Drug-induced thyroiditis; E16.0, Drug-induced hypoglycemia without coma; E23.1, Drug-induced hypopituitarism; E24.2, Drug-induced Cushing’s syndrome; E27.3, Drug-induced adrenocortical insufficiency; E66.1, Drug-induced obesity; selected codes from the ICD–10 title of mental and behavioral disorders due to psychoactive substance use, specifically, F11.0–F11.5, F11.7–F11.9, F12.0–F12.5, F12.7–F12.9, F13.0–F13.5, F13.7–F13.9, F14.0–F14.5, F14.7–F14.9, F15.0–F15.5, F15.7–F15.9, F16.0–F16.5, F16.7–F16.9, F17.0, F17.3–F17.5, F17.7–F17.9, F18.0–F18.5, F18.7–F18.9, F19.0–F19.5, F19.7–F19.9; G21.1, Other drug-induced secondary parkinsonism; G24.0, Drug-induced dystonia; G25.1, Drug-induced tremor; G25.4, Drug-induced chorea; G25.6, Drug-induced tics and other tics of organic origin; G44.4, Drug-induced headache, not elsewhere classified; G62.0, Drug-induced polyneuropathy; G72.0, Drug-induced myopathy; I95.2, Hypotension due to drugs; J70.2, Acute drug-induced interstitial lung disorders; J70.3, Chronic drug-induced interstitial lung disorders; J70.4, Drug-induced interstitial lung disorder, unspecified; K85.3, Drug-induced acute pancreatitis; L10.5, Drug-induced pemphigus; L27.0, Generalized skin eruption due to drugs and medicaments; L27.1, Localized skin eruption due to drugs and medicaments; M10.2, Drug-induced gout; M32.0, Drug-induced systemic lupus erythematosus; M80.4, Drug-induced osteoporosis with pathological fracture; M81.4, Drug-induced osteoporosis; M83.5, Other drug-induced osteomalacia in adults; M87.1, Osteonecrosis due to drugs; R50.2, Drug-induced fever; R78.1, Finding of opiate drug in blood; R78.2, Finding of cocaine in blood; R78.3, Finding of hallucinogen in blood; R78.4, Finding of other drugs of addictive potential in blood; R78.5, Finding of psychotropic drug in blood; X40–X44, Accidental poisoning by and exposure to drugs, medicaments and biological substances; X60–X64, Intentional self-poisoning (suicide) by and exposure to drugs, medicaments and biological substances; X85, Assault (homicide) by drugs, medicaments and biological substances; and Y10–Y14, Poisoning by and exposure to drugs, medicaments and biological substances, undetermined intent.
The following ICD–10 codes indicate whether and the type of drug(s) involved [5]:
T40.1, heroin; T40.2, other opioid; T40.3, methadone; any of the codes T40.2–T40.4, any opioid analgesic; T40.4, other synthetic narcotic; T40.5, cocaine; and T42.4, benzodiazepine; none of the codes T36–T50.9, no drug; any of the codes T36–T50.9 drug; only T50.9, only nonspecified drug(s); any of the codes T36–T50.8 other than T40.2–T40.4, specified drug(s) other than opioid analgesic.
APPENDIX 2
Number of drug-related deaths by ICD-10 category of underlying and immediate cause, Wisconsin, 1999–2008 (n=4828)
| ICD-10 category | Underlying cause | Immediate cause |
|---|---|---|
| A. Infectious diseases | 1 | 9 |
| C. Malignant Neoplasms | 6 | 5 |
| D. Other Neoplasms and blood diseases | 0 | 1 |
| E. Endocrine, Nutritional, and Metabolic diseases | 9 | 12 |
| F. Mental and behavioral disorders | 147 | 97 |
| G. Nervous sys diseases | 6 | 90 |
| I. Circulatory sys diseases | 90 | 351 |
| J. Respiratory sys diseases | 31 | 141 |
| K. Digestive sys diseases | 9 | 22 |
| N. Genitourinary sys diseases | 3 | 11 |
| R. Symtoms, signs, findings not else classified | 0 | 276 |
| S. Injuries | 0 | 193 |
| T. Injuries, burns, poisoning, etc | 0 | 3610 |
| V. Transport accidents | 57 | 0 |
| W. Falls etc | 191 | 2 |
| X. Poisoning etc | 3962 | 8 |
| Y. Other external causes | 316 | 0 |
| Total deaths | 4828 | 4828 |
NOTE: Deaths are allowed to have only one underlying cause and one immediate cause. Contributing causes are not shown above.
Footnotes
Some results from this research report were presented at the annual meeting of the American College of Epidemiology, 10–11 Sept 2012, in Chicago, Illinois.
Contributor Information
David L. Nordstrom, University of Wisconsin-Whitewater, Department of Occupational and Environmental Safety and Health, College of Education and Professional Studies, Whitewater WI 53190.
Mieko L. Yokoi-Shelton, University of Wisconsin-Whitewater, Department of Occupational and Environmental Safety and Health, College of Education and Professional Studies, Whitewater WI 53190.
Amy Zosel, Department of Emergency Medicine, Medical College of Wisconsin, Milwaukee, Wisconsin 53226.
REFERENCES
- 1.Hewitt D, Milner J. Drug-Related Deaths in the United States: First Decade of an Epidemic. Health Services Reports. 1974;89(3):211–218. [PMC free article] [PubMed] [Google Scholar]
- 2.Paulozzi LJ, Budnitz DS, Xi Y. Increasing deaths from opioid analgesics in the United States. Pharmacoepidemiol Drug Saf. 2006;15(9):618–627. doi: 10.1002/pds.1276. [DOI] [PubMed] [Google Scholar]
- 3.Substance abuse objective 12. Washington, DC: U.S. Department of Health and Human Services. Office of Disease Prevention and Health Promotion. Healthy People 2020; [Accessed 12 June 2012]. Healthy People 2020 Summary of Objectives. Available at http://www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=40. [Google Scholar]
- 4.Fingerhut LA. Increases in poisoning and methadone-related deaths: United States, 1999–2005. Hyattsville, MD: National Center for Health Statistics; 2008. [Google Scholar]
- 5.Warner M, Chen LH, Makuc DM. NCHS Data Brief. 22. Hyattsville MD: National Center for Health Statistics; 2009. Increase in fatal poisonings involving opioid analgesics in the United States, 1999–2006. [PubMed] [Google Scholar]
- 6.U.S. Centers for Disease Control and Prevention. Heroin overdose deaths--Multnomah County, Oregon, 1993–1999. MMWR Morb Mortal Wkly Rep. 2000;49(28):633–636. [PubMed] [Google Scholar]
- 7.U.S. Centers for Disease Control and Prevention. Unintentional opiate overdose deaths—King County, Washington, 1990–1999. MMWR Morb Mortal Wkly Rep. 2000;49(28):636–640. [PubMed] [Google Scholar]
- 8.Ballesteros MF, Budnitz DS, Sanford CP, Gilchrist J, Agyekum GA, Butts J. Increase in deaths due to methadone in North Carolina. JAMA. 2003;290(1):40. doi: 10.1001/jama.290.1.40. [DOI] [PubMed] [Google Scholar]
- 9.Graham NA, Merlo LJ, Goldberger BA, Gold MS. Methadone- and heroin-related deaths in Florida. Am J Drug Alcohol Abuse. 2008;34(3):347–353. doi: 10.1080/00952990802010892. [DOI] [PubMed] [Google Scholar]
- 10.Wunsch MJ, Nakamoto K, Behonick G, Massello W. Opioid deaths in rural Virginia: a description of the high prevalence of accidental fatalities involving prescribed medications. Am J Addict. 2009;18(1):5–14. doi: 10.1080/10550490802544938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mueller MR, Shah NG, Landen MG. Unintentional prescription drug overdose deaths in New Mexico, 1994–2003. Am J Prev Med. 2006;30(5):423–429. doi: 10.1016/j.amepre.2005.12.011. [DOI] [PubMed] [Google Scholar]
- 12.U.S. Centers for Disease Control and Prevention. Alcohol and other drug use among victims of motor-vehicle crashes--West Virginia, 2004–2005. MMWR Morb Mortal Wkly Rep. 2006;55(48):1293–1296. [PubMed] [Google Scholar]
- 13.U.S. Centers for Disease Control and Prevention. Overdose deaths involving prescription opioids among Medicaid enrollees - Washington, 2004–2007. MMWR Morb Mortal Wkly Rep. 2009;58(42):1171–1175. [PubMed] [Google Scholar]
- 14.Wysowski DK, Schober SE, Wise RP, Kopstein A. Mortality attributed to misuse of psychoactive drugs, 1979–88. Public Health Rep. 1993;108(5):565–570. [PMC free article] [PubMed] [Google Scholar]
- 15.Wysowski DK. Surveillance of prescription drug-related mortality using death certificate data. Drug Saf. 2007;30(6):533–540. doi: 10.2165/00002018-200730060-00007. [DOI] [PubMed] [Google Scholar]
- 16.Paulozzi LJ, Annest JL. US data show sharply rising drug-induced death rates. Inj Prev. 2007;13(2):130–132. doi: 10.1136/ip.2006.014357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Paulozzi LJ, Xi Y. Recent changes in drug poisoning mortality in the United States by urban-rural status and by drug type. Pharmacoepidemiol Drug Saf. 2008;17(10):997–1005. doi: 10.1002/pds.1626. [DOI] [PubMed] [Google Scholar]
- 18.Pollock DA, Holmgreen P, Lui KJ, Kirk ML. Discrepancies in the reported frequency of cocaine-related deaths, United States, 1983 through 1988. JAMA. 1991;266(16):2233–2237. [PubMed] [Google Scholar]
- 19.Landen MG, Castle S, Nolte KB, Gonzales M, Escobedo LG, Chatterjee BF, Johnson K, Sewell CM. Methodological issues in the surveillance of poisoning, illicit drug overdose, and heroin overdose deaths in New Mexico. Am J Epidemiol. 2003;157(3):273–278. doi: 10.1093/aje/kwf196. [DOI] [PubMed] [Google Scholar]
- 20.Breiding MJ, Wiersema B. Variability of undetermined manner of death classification in the US. Inj Prev. 2006;12(Suppl 2):ii49–ii54. doi: 10.1136/ip.2006.012591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Single E, Rehm J, Robson L, Truong MV. The relative risks and etiologic fractions of different causes of death and disease attributable to alcohol, tobacco and illicit drug use in Canada. CMAJ. 2000;162(12):1669–1675. [PMC free article] [PubMed] [Google Scholar]
- 22.World Health Organization. ICD-10 Online. Available from: http://apps.who.int/classifications/apps/icd/icd10online/.
- 23.Rosenberg HM. Improving cause-of-death statistics. Am J Public Health. 1989;79(5):563–564. doi: 10.2105/ajph.79.5.563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Heron M, Hoyert DL, Murphy SL, Xu J, Kochanek KD, Tejada-Vera B. Deaths: final data for 2006. Natl Vital Stat Rep. 2009;57(14):1–134. [PubMed] [Google Scholar]
- 25.U.S. National Center for Health Statistics. U.S. Standard Certificate of Death. 2003 [Google Scholar]
- 26.Institute of Medicine. Medicolegal death investigation system: workshop summary. Washington, D.C.: National Academies Press; 2003. Committee for the Workshop on the Medicolegal Death Investigation System. [PubMed] [Google Scholar]
- 27.Ingram DD, Franco S. 2006 NCHS Urban-Rural Classification Scheme for Counties. 2006 Available from: www.cdc.gov/nchs/data_access/urban_rural.htm#resources.
- 28.U.S. Census Bureau. Census 2000 Summary File 3 - Sample Data - Table P53. [Accessed 25 April 2010]; Available from: http://factfinder.census.gov.
- 29.Israel RA, Rosenberg HM, Curtin LR. Analytical potential for multiple cause-of-death data. Am J Epidemiol. 1986;124(2):161–179. doi: 10.1093/oxfordjournals.aje.a114375. [DOI] [PubMed] [Google Scholar]
- 30.Egan-Robertson D. Demographic Services Center's 2009 Final Estimates Summary. Madison, WI: Wisconsin Department of Administration; 2009. [Google Scholar]
- 31.Lipinski E. Motivation in drug misuse. Some comments on agent, environment, host. JAMA. 1972;219(2):171–175. [PubMed] [Google Scholar]
- 32.U.S. National Center for Health Statistics. Health, United States, 2009. 2010:511. [PubMed] [Google Scholar]
- 33.Compton WM, Volkow ND. Major increases in opioid analgesic abuse in the United States: concerns and strategies. Drug Alcohol Depend. 2006;81(2):103–107. doi: 10.1016/j.drugalcdep.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 34.Morin SF, Collins C. Substance abuse prevention: moving from science to policy. Addict Behav. 2000;25(6):975–983. doi: 10.1016/s0306-4603(00)00125-8. [DOI] [PubMed] [Google Scholar]
- 35.World Health Organization. Geneva: WHO; 1998. Opioid overdose: Trends, risk factors, interventions and priorities for action. WHO/HSC/SAB/98.4. [Google Scholar]
- 36.Injury Surveillance Workgroup 7. The Safe States Alliance. Atlanta, GA: 2012. Consensus recommendations for national and state poisoning surveillance. [Google Scholar]
- 37.Webster LR, Cochella S, et al. An analysis of the root causes for opioid-related overdose deaths in the United States. Pain Med. 2011;12(Suppl 2):S26–S35. doi: 10.1111/j.1526-4637.2011.01134.x. [DOI] [PubMed] [Google Scholar]
- 38.State of Wisconsin State Council on Alcohol and Other Drug Abuse. Reducing Wisconsin’s Prescription Drug Abuse: A Call to Action. Madison, WI: The Council; 2012. [Google Scholar]
- 39.Hanzlick R. Medical examiners, coroners, and public health: a review and update. Arch Pathol Lab Med. 2006;130(9):1274–1282. doi: 10.5858/2006-130-1274-MECAPH. [DOI] [PubMed] [Google Scholar]
- 40.U.S. Food and Drug Administration. Washington, D.C.: 2006. Nov 27, [Accessed 15 August 2012]. Public Health Advisory: Methadone Use for Pain Control May Result in Death and Life-Threatening Changes in Breathing and Heart Beat. Available at http://www.fda.gov/drugs/drugsafety/postmarketdrugsafetyinformationforpatientsandproviders/drugsafetyinformationforheathcareprofessionals/publichealthadvisories/ucm124346.htm. [Google Scholar]
- 41.U.S. Centers for Disease Control and Prevention. Vital Signs: Risk for Overdose from Methadone Used for Pain Relief – United States, 1999–2010. MMWR Morb Mortal Wkly Rep. 2012;61(26):493–497. [PubMed] [Google Scholar]
- 42.Lantz PM, House JS, et al. Socioeconomic factors, health behaviors, and mortality: results from a nationally representative prospective study of US adults. JAMA. 1998;279(21):1703–1708. doi: 10.1001/jama.279.21.1703. [DOI] [PubMed] [Google Scholar]
- 43.Comstock GW, Markush RE. Further comments on problems in death certification. Am J Epidemiol. 1986;124(2):180–181. doi: 10.1093/oxfordjournals.aje.a114376. [DOI] [PubMed] [Google Scholar]
- 44.Poikolainen K. Mortality related to psychotropic substances: current knowledge and research problems. Br J Addict. 1981;76(4):363–374. doi: 10.1111/j.1360-0443.1981.tb03233.x. [DOI] [PubMed] [Google Scholar]
- 45.Lahti RA, Penttilä A. Cause-of-death query in validation by expert panel; effects on mortality statistics in Finland, 1995. Forensic Science International. 2003;131(2–3):113–124. doi: 10.1016/s0379-0738(02)00418-8. [DOI] [PubMed] [Google Scholar]
- 46.Wysowski DK, Nourjah P. Analyzing prescription drugs as causes of death on death certificates. Public Health Rep. 2004;119(6):520. doi: 10.1016/j.phr.2004.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wisconsin Department of Health Services. Wisconsin Deaths 2008. Madison, WI: Wisconsin Department of Health Services; 2009. Division of Public Health, Office of Health Informatics. (P-45368-08). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.