Abstract
The paper by Rachidi et al. suggests that antiplatelet drugs may play a role in ameliorating the clinical outcome in a large series of patients with head and neck cancer managed with either surgery or radiation. Our data, as well as confirming the results observed by the authors, enhance their clinical relevance pointing out the effect of antiplatelet drugs in terms of locoregional control in the setting of patients with advanced head and neck cancer managed with definitive chemo-radiotherapy.
Keywords: Head and neck cancer, Aspirin, Antiplatelets, Radiotherapy, Coagulation, Platelets, Larynx, Survival
Previous findings on patients with head and neck cancer exposed to antiplatelet drugs
We read with great interest the article by Rachidi et al. [1], which indicated that higher platelet count is associated with a worse survival in head and neck squamous cell carcinoma (HNSCC). In the same cohort the use of antiplatelet medications was associated with a reduced risk of death.
The authors included patients with stage I–IV HNSCC, irrespective of treatment type (surgery, chemotherapy, or radiation).
Case series report
We retrospectively reviewed a cohort of 58 consecutive patients with stage III-IV larynx-hypopharynx cancer managed with definitive chemoradiotehrapy at the Centro di Riferimento Oncologico of Aviano, Italy, between 2008 and 2012 (patients characteristics by use of antiplatelet drugs are shown in Table 1). Kaplan-Meier analysis confirmed a survival advantage in patients who were administered with antiplatelet medications, although not significant because of small sample size. At a median follow-up of 31 months, the 3-year survival of patients who were taking antiplatelet drugs (20 patients) was 69 % vs 54 % for those who were not taking (p = 0.12). Interestingly, our data also showed a significant difference in locoregional control (LRC) between patients who were and were not taking antiplatelet medications during radiotherapy (3-year LRC resulted 76 % and 45 %, respectively, p = 0.01 - Fig. 1).
Table 1.
Baseline socio-demographic and clinical characteristics of 58 larynx-hypopharynx cancer patients, according to regular antiplatelets use
| Non-Antiplatelets users | Antiplatelets users | Fisher exact test | |||
|---|---|---|---|---|---|
| N | (%) | n | (%) | ||
| Sex | |||||
| Men | 34 | (89.5) | 16 | (80.0) | p = 0.43 |
| Women | 4 | (10.5) | 4 | (20.0) | |
| Age (years) | |||||
| <65 | 28 | (73.7) | 5 | (25.0) | p <0.01 |
| ≥65 | 10 | (26.3) | 15 | (75.0) | |
| Tobacco smoking | |||||
| Never | 5 | (13.2) | 4 | (20.0) | p = 0.70 |
| Ever | 33 | (86.8) | 16 | (80.0) | |
| T status | |||||
| T2–T3 | 27 | (71.0) | 20 | (100.0) | p = 0.01 |
| T4 | 11 | (29.0) | 0 | (0.0) | |
| N status | |||||
| N0 | 11 | (29.0) | 8 | (40.0) | p = 0.56 |
| N1–N3 | 27 | (71.0) | 12 | (60.0) | |
| Stage | |||||
| III | 13 | (34.2) | 15 | (75.0) | p <0.01 |
| IV | 25 | (65.8) | 5 | (25.0) | |
| Platelet count at radiotherapy beginning (cells/μL) | |||||
| <250.000 | 19 | (51.3) | 11 | (57.9) | p = 0.78 |
| ≥250.000 | 18 | (48.7) | 8 | (42.1) | |
| Locoregional recurrence | |||||
| No | 17 | (44.7) | 16 | (80.0) | p = 0.01 |
| Yes | 21 | (55.3) | 4 | (20.0) | |
Fig. 1.
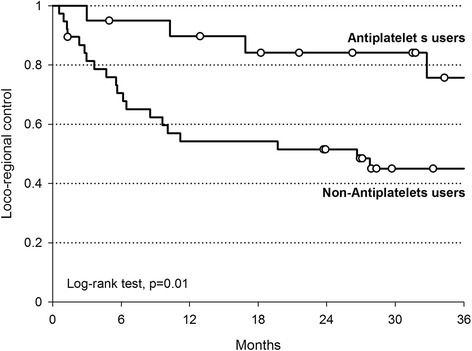
Locoregional control of 58 advanced larynx-hypopharynx cancer patients by use of antiplatelet drugs
Since antiplatelet treatment was significantly associated to age and tumor stage, subgroup analysis were also conducted. The same effect was observed both patients aged <65 year (3-year LRC was 80 % vs 40 % for those who were and were not taking antiplatelet drugs), and in the those aged ≥65 year (74 % vs 58 %, respectively), as well as in patients with stage III (75 % and 54 %, respectively) and stage IV cancer (74 % and 40 %, respectively).
Rachidi and colleagues [1] reported stronger effect of antiplatelet use on OS in patients with thrombocytosis. In our study, we also found a greater advantage from antiplatelet use among patients with platelet count >250.000/μL (Table 1) in both OS (3-year OS: 63 % vs 43 % in antiplatelet users and non users, p = 0.50) and LRC (3-year LRC : 71 % vs 18 %, p = 0.02).
Comment
Our results confirmed that the use of antiplatelet medications modify outcomes in patients with HNSCC. LRC is recognized as a surrogate endpoint of survival for patients with locally-advanced HNSCC [2], and our findings concerning LRC may be translated into survival at longer follow-up, confirming the results published in the paper. Moreover, these elements concerning the effects on LRC suggest that antiplatelet medications may have a role in enhancing the efficacy of radiation for HNSCC and indicate the strong need for a randomized clinical trial.
Acknowledgements
The authors thank Mrs. Silvia Cervo for the technical assistance.
The study is approved by the Internal Review Board of the Centro di Riferimento Oncologico (CRO) – Aviano, Italy.
Abbreviations
- HNCSS
Head and neck squamous cell carcinoma
- LRC
Locoregional control
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
CF conceived the study and drafted the manuscript. AS partecipated in its design and interpretation of the data. JP carried out statistical analysis. MT contributed in the study conception and design. EV and CG contributed to the data collection. DS critically revised the manuscript. LB and GF partecipated in its design and coordination. All authors read and approved the final manuscript.
Authors’ information
Not applicable.
Contributor Information
Carlo Furlan, Phone: +390434659081, Email: cfurlan@cro.it.
Agostino Steffan, Email: asteffan@cro.it.
Jerry Polesel, Email: polesel@cro.it.
Marco Trovo, Email: marcotrovo33@hotmail.com.
Carlo Gobitti, Email: cgobitti@cro.it.
Emanuela Vaccher, Email: evaccher@cro.it.
Diego Serraino, Email: serrainod@cro.it.
Luigi Barzan, Email: luigi.barzan@libero.it.
Giovanni Franchin, Email: gfranchin@cro.it.
References
- 1.Rachidi S, Wallace K, Day TA, Alberg AJ, Li Z. Lower circulating platelet counts and antiplatelet therapy independently predict better outcomes isn patients with head and neck squamous cell carcinoma. J Hematol Oncol. 2014;7:65. doi: 10.1186/s13045-014-0065-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Michiels S, Le Maître A, Buyse M, Burzykowski T, Maillard E, Bogaerts J, Vermorken JB, Budach W, Pajak TF, Ang KK, Bourhis J, Pignon JP, MARCH and MACH-NC Collaborative Groups Surrogate endpoints for overall survival in locally advanced head and neck cancer: meta-analyses of individual patient data. Lancet Oncol. 2009;10(4):341–50. doi: 10.1016/S1470-2045(09)70023-3. [DOI] [PubMed] [Google Scholar]


