Abstract
Background
Early rehabilitation improves outcomes, and increased use of physical therapist services in the intensive care unit (ICU) has been recommended. Little is known about the implementation of early rehabilitation programs or physical therapists' preparation and perceptions of care in the United States.
Objective
A national survey was conducted to determine the current status of physical therapist practice in the ICU.
Design
This study used a cross-sectional, observational design.
Methods
Self-report surveys were mailed to members of the Acute Care Section of the American Physical Therapy Association. Questions addressed staffing, training, barriers, and protocols, and case scenarios were used to determine perceptions about providing rehabilitation.
Results
The response rate was 29% (667/2,320). Staffing, defined as the number of physical therapists per 100 ICU beds, was highest in community hospitals (academic: median=5.4 [range=3.6–9.2]; community: median=6.7 [range=4.4–10.0]) and in the western United States (median=7.5 [range=4.2–12.9]). Twelve percent of physical therapists reported no training. Barriers to providing ICU rehabilitation included insufficient staffing and training, departmental prioritization policies, and inadequate consultation criteria. Responses to case scenarios demonstrated differences in the likelihood of consultation and physical therapists' prescribed frequency and intensity of care based on medical interventions rather than characteristics of patients. Physical therapists in academic hospitals were more likely to be involved in the care of patients in each scenario and were more likely to perform higher-intensity mobilization.
Limitations
Members of the Acute Care Section of the American Physical Therapy Association may not represent most practicing physical therapists, and the 29% return rate may have contributed to response bias.
Conclusions
Although staffing was higher in community hospitals, therapists in academic and community hospitals cited insufficient staffing as the most common barrier to providing rehabilitation in the ICU. Implementing strategies to overcome barriers identified in this study may improve the delivery of ICU rehabilitation services.
Complications of critical illness include intensive care unit (ICU)–acquired weakness, neuropsychiatric abnormalities, impaired functional mobility, decreased quality of life, and high costs of health care use.1–5 Physical therapist services provided in the ICU, including early mobilization, have been reported to improve functional mobility, promote weaning from mechanical ventilation, and reduce hospital readmissions.6–9 As a result, increased use of physical therapist services in the ICU have been recommended.5,10,11
Surveys of ICU physical therapists in Europe,10,12 Australia,13,14 and Canada15 have described variations in practice as well as differences in staffing and training between countries and regions. For example, European and Australian physical therapist practice includes both respiratory treatment and rehabilitation treatment of patients in the ICU. Physical therapists in Sweden, the Netherlands, Switzerland, and Australia are rarely involved with weaning patients from mechanical ventilation, whereas greater than 50% of physical therapists in Belgium and Portugal routinely participate in weaning patients from mechanical ventilation.10,13 Canadian physical therapists reported ambulation as an intervention 56% of the time, on average. Regionally, however, ambulation was implemented 100% of the time in Saskatchewan and 33% of the time in Nova Scotia.15 In Germany, larger proportions of patients were mobilized out of bed in community hospitals than in university and university-affiliated hospitals.12 Regarding training, 29% of European physical therapists reported postgraduate specialization in ICU therapy, and 43% reported postgraduate specialization in respiratory therapy, the largest percentage being from the United Kingdom.10
With regard to the United States, we published a survey in 2009 that identified functional mobility retraining and therapeutic exercise as the most common interventions performed in the ICU by physical therapists.16 Additionally, we reported that patients with neurological and trauma diagnoses were more likely to receive physical therapist services than patients with medical diagnoses.16 The evidence for ICU-based rehabilitation continues to evolve, and physical therapists are now recommended to play an integral role in the care of patients recovering from critical illness.5,7,17 In the United States, however, there is a paucity of information describing how ICU-based physical therapist services are implemented, and currently there are no descriptions of physical therapists' background (demographics, including age, years of licensure, and years of ICU experience), training (methods of gaining the knowledge, skills, and attributes needed to work in the ICU), or perceptions about providing care to patients who are critically ill.
The purpose of this study was to characterize current physical therapist practice, specifically, practitioner demographics, ICU staffing patterns, methods of training for ICU practice, barriers to providing rehabilitation services, and the influence of characteristics of patients on physical therapists' decision making regarding their plan of care. Additionally, the responses of physical therapists from academic and community hospitals and different regions of the United States were compared. The results of this survey identified barriers to the provision of rehabilitation that could be overcome, possibly improving ICU rehabilitation service delivery.
Method
Participants
We mailed self-administered surveys to all 2,320 physical therapist members of the Acute Care Section (ACS) of the American Physical Therapy Association (APTA). The APTA is a professional membership organization representing more than 88,000 member physical therapists, physical therapist assistants, and students. The ACS is 1 of 18 sections of APTA. To join the ACS, one must belong to APTA and pay national, chapter, and section membership fees. Members of the ACS have clinical, administrative, or research interests in acute care practice.
Survey Development
Questions and case scenarios were developed through an iterative process involving physical therapists with ICU experience, physical therapist academicians, and critical care physicians. A preliminary survey was distributed to several physical therapists with ICU experience nationally and internationally to assess for ease of completion. Modifications based on the clinicians' suggestions resulted in the final version of the survey.
Survey Content
The final, 65-item questionnaire required 15 minutes to complete (eAppendix). The survey was divided into 2 sections. Section 1 addressed the following: demographics of the hospital or ICU and physical therapists (10 items), staffing patterns (2 items), training methods for working in the ICU (3 items), self-confidence working in the ICU (5 items), the presence of specific consultation and treatment guidelines (2 items), and perceived barriers to providing rehabilitation services in the ICU (6 items). The adequacy of training and barrier identification were assessed with a 5-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). Formal training was defined as ICU instruction that occurred as part of the entry-level physical therapist degree, postgraduate residency or fellowship program, or continuing education courses. Informal training was defined as on-site, facility-based training; senior staff mentorship; or completion of department-based competency requirements.
Section 2 of the survey addressed physical therapists' perceptions of rehabilitation practices by eliciting responses to 5 questions related to each of 6 hypothetical case scenarios. The complexity of patient care was influenced by the addition of a variable such as an artificial airway (endotracheal tube or tracheostomy tube), an altered mechanical ventilation setting (positive end-expiratory pressure or supplemental oxygen), or medical interventions to maintain hemodynamic stability (vasopressors or continuous renal replacement therapy) (Tab. 1). Cases differed by one variable only. All patients were described as being awake, alert, and able to follow instructions and were defined as weak. Questions in section 2 addressed the following: the likelihood of physical therapist consultation, frequency of care prescribed by physical therapists, physical therapists' confidence in and perception of the benefit of performing various interventions, identification of the single most beneficial intervention category, and physical therapists' confidence in mobilizing patients out of bed as part of a physical therapy intervention session. Confidence in mobilization was assessed with a 5-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree).
Table 1.
Six Case Scenariosa
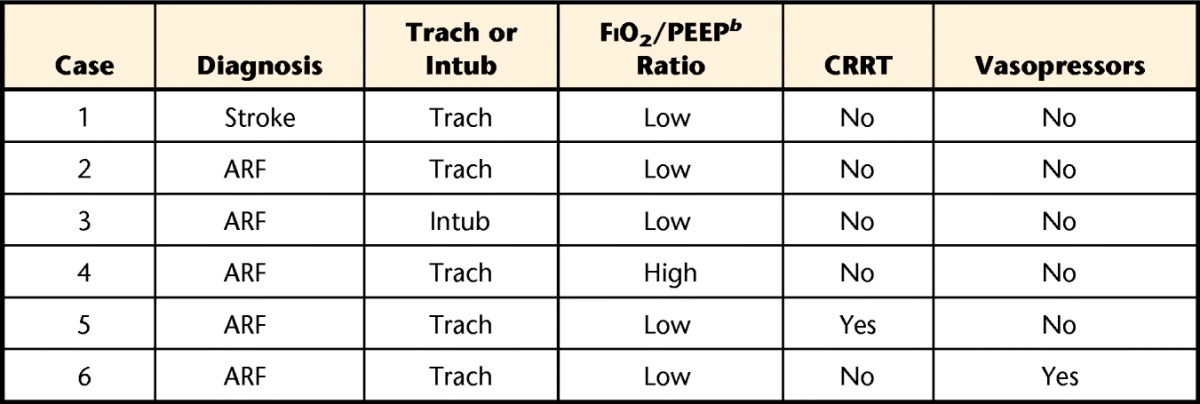
Trach=tracheostomy tube; Intub=oral endotracheal tube; FiO2=fraction of inspired oxygen; PEEP=positive end-expiratory pressure; CRRT=continuous renal replacement therapy via central venous access (nonfemoral); vasopressors=low, constant infusion of dobutamine, vasopressin, dopamine, or epinephrine; ARF=acute respiratory failure.
b Low FiO2/PEEP was defined as FiO2=0.40 (40% oxygen) and PEEP=5 cm H2O pressure. High FiO2/PEEP was defined as FiO2=0.70 (70% oxygen) and PEEP=10 cm H2O pressure.
Survey Administration
Surveys were mailed in March 2013 and included a self-addressed, stamped envelope for return. Two follow-up postcard reminders were sent at 6-week intervals, and reminders were posted to the ACS listserve to facilitate completion of the survey. No incentives were offered for return of the survey. Responses were recorded for total respondents and further categorized on the basis of the primary hospital at which the therapists were employed (ie, academic or community) and the region of the United States in which they were employed. Regions were defined as West, Midwest, Northeast, Southeast, and Southwest.
Survey Analysis
Normally distributed data were expressed as means (95% confidence intervals [CI]), and data that were not normally distributed were expressed as medians (interquartile ranges). Means of the Likert scale data were included in the analysis of physical therapists' confidence in their ability to provide rehabilitation. Chi-square tests of independence were used to examine categorical variables at baseline, including analyses of the effects of regional differences in the percentages of physical therapists with formal training and the type of hospital (academic or community) on the following outcomes: percentage of physical therapists with formal training, percentage of hospitals with established competency requirements or guidelines for physical therapist consultation, presence of barriers to physical therapy, and frequency of physical therapy in the 6 case scenarios. When the data were normally distributed, t tests were used to compare continuous characteristics of 2 groups, and analyses of variance were used when there were more than 2 groups. These analyses were used to determine the effect of physical therapists' confidence in their ability to provide rehabilitation. For all other univariate analyses, nonparametric testing was used because the data were not normally distributed. Multivariate logistic regression was used to evaluate the association between regions of the United States and formalized training (yes or no). Other potential independent predictors included in the analyses were type of hospital (academic or community) and length of employment (in number of years). JMP software (SAS Institute Inc, Cary, North Carolina) was used for all analyses, and a P value of less than .05 was considered statistically significant.
Role of the Funding Source
This study was funded by National Institutes of Health grant R01NR011051. The NIH had no role in study design; in data collection, analysis, or interpretation; in writing the manuscript; or in the decision to submit the manuscript for publication.
Results
General Demographics
A total of 2,320 surveys were mailed, and 667 were returned, for an overall response rate of 29%. Of the 667 respondents, 113 did not complete the survey because they did not currently practice in the acute care or ICU setting, or the survey was not deliverable because of an inaccurate address. Therefore, 554 surveys were included in the final analysis. Completed surveys represented 47 of the 50 states (missing were Delaware, Rhode Island, and Hawaii) and the District of Columbia. A total of 37% (n=205) of the respondents were from academic hospitals, and the remaining 63% (n=349) were from community hospitals. Regionally, 21% (n=117) of respondents were from the West, 22% (n=131) were from the Midwest, 18% (n=98) were from the Northeast, 22% (n=118) were from the Southeast, and 14% (n=75) were from the Southwest (Figure).
Figure.
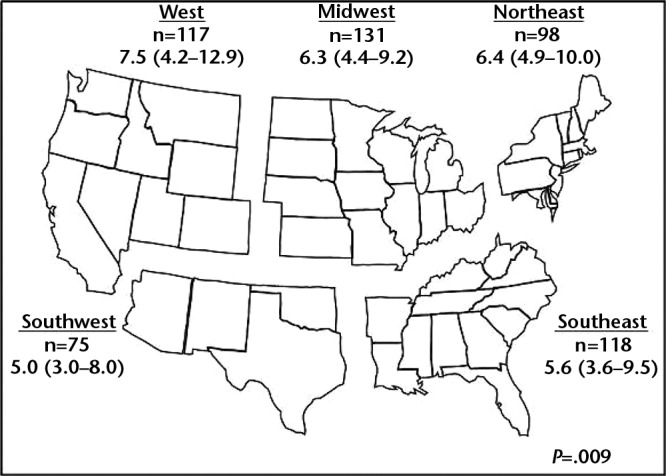
Regional breakdown of physical therapist staffing (number of therapists per 100 intensive care unit beds, shown as median [interquartile range]).
Staffing
Defined as the number of physical therapists per 100 hospital beds or ICU beds and reported as medians (interquartile ranges), staffing was 2.4 (1.7–3.3) for the hospital and 6.3 (4.0–10.0) for the ICU (P<.001). Academic hospitals had lower ICU staffing than community hospitals (academic: 5.4 [3.6–9.2]; community: 6.7 [4.4–10.0]; P=.005). Regionally, ICU staffing was highest in the West (7.5 [4.2–12.9]) and lowest in the Southeast (5.6 [3.6–9.5]) and Southwest (5.0 [3.0–8.0]) (P=.009) (Figure).
Physical Therapist Experience and Training
With regard to experience—which was reported as medians (interquartile ranges)—respondents had, on average, 13 (5.5–22) years of experience, 10 (5–17) years of experience working in the acute care hospital setting, and 7.8 (3–15) years of experience working in the ICU. Physical therapists at academic hospitals had greater acute care experience (academic: 13.2 years [11.9–14.4]; community: 11.0 years [10.1–12.0]; P=.009) and greater ICU experience (academic: 10.9 years [9.7–12.2]; community: 9.3 years [8.3–10.2]; P=.03).
Only 31.8% of the physical therapists had received formal ICU training. Most of the respondents had received hospital-based informal training (55.9%), and 12.3% had received no formal or informal training (Tab. 2). Physical therapists at community hospitals reported a higher percentage of formal training (34.3%) but also a higher percentage of no training (14.3%) than those at academic hospitals (P=.02). Physical therapists from academic settings reported that their departments were more likely to have established competency requirements than those from community settings (academic: 51.7%; community: 28.2%; P=.0001). Regionally, the percentage of physical therapists with formal training was highest in the Midwest, compared with other regions of the United States (eFigure). These regional training differences remained in a multivariable analysis adjusting for type of hospital and length of employment (P=.005).
Table 2.
Training of Physical Therapistsa
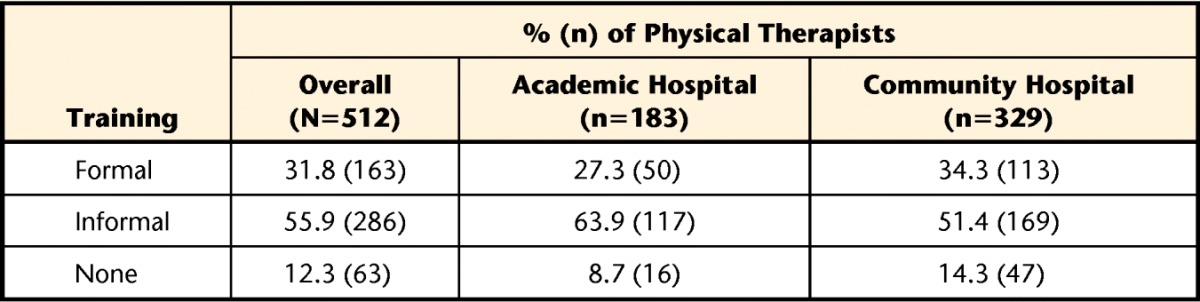
The P value for academic hospitals versus community hospitals was .02.
Physical therapists had confidence in their ability to provide rehabilitation in the ICU (X=4.4 [95% CI=4.3, 4.4]), with a significant difference between academic and community settings (academic: X=4.5 [95% CI=4.4, 4.6]; community: X=4.3 [95% CI=4.2, 4.4]; P=.0007). Physical therapists also reported understanding mechanical ventilation (X=3.9 [95% CI=3.8, 4.0]), with physical therapists in academic settings reporting greater understanding than those in community settings (academic: X=4.1 [95% CI=4.0, 4.3]; community: X=3.7 [95% CI=3.6, 3.8]; P<.0001). Whether these differences are meaningful is questionable.
Physical Therapist Consultation
Overall, 38.6% of respondents reported facility-based guidelines for ICU consultation, and 43.5% of physical therapists reported specific guidelines for session termination. There were no differences between academic and community settings.
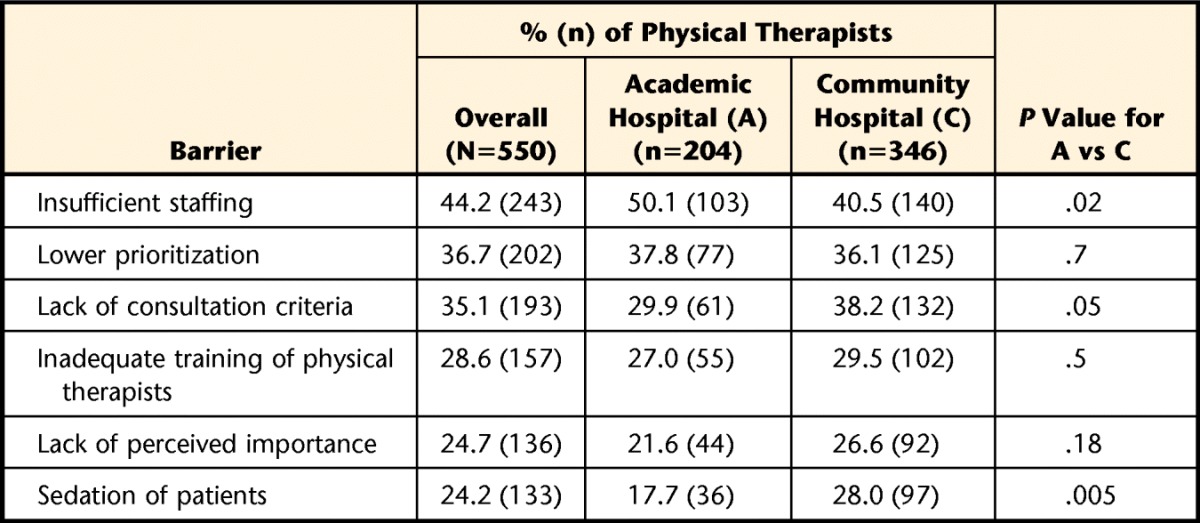
Barriers
The percentages of respondents who agreed or strongly agreed with the common barriers to providing physical therapist services in the ICU are shown in Table 3. Overall, the barriers chosen most frequently were insufficient staffing, lower prioritization of the ICU, and lack of specific consultation criteria for physical therapist services. Physical therapists in academic settings noted insufficient staffing as a more frequent barrier than physical therapists in community settings. Physical therapists in community hospitals identified sedation of patients as a more frequent barrier than physical therapists in academic hospitals. Additional barriers provided by respondents (n=280) included scheduling conflicts, such as a patient receiving bedside dialysis or being transported off the floor for diagnostic testing (19%, n=53), and inadequate equipment (19%, n=53).
Table 3.
Barriers to Providing Physical Therapy in the Intensive Care Unit
Perceptions of Physical Therapy Care
The 6 case scenarios (Tab. 1) showed that a physical therapy consultation was less likely for patients with more complex medical conditions. If physical therapists were consulted, then the prescribed frequency and intensity of care also decreased as the complexity increased (Tab. 4). For example, patient mobilization was limited, with ambulation being included in the care plan for only 12.4% of patients on vasopressors. Therapists were asked to predict what intervention would have the most positive impact on patient outcomes; functional mobility training was expected to be the most beneficial intervention, and the next most beneficial was expected to be therapeutic exercises (strengthening or aerobic). However, this prediction was influenced by characteristics of patients, as exercise was predicted to have a more positive impact for patients with more complex medical conditions. Finally, physical therapists who worked in academic hospitals believed that they were more likely to be involved in the care of patients in each scenario and were more likely to perform higher-intensity mobilization, such as transfers out of bed and ambulation, than those who worked in community hospitals (Tab. 5).
Table 4.
Physical Therapists' Responses to 6 Case Scenariosa
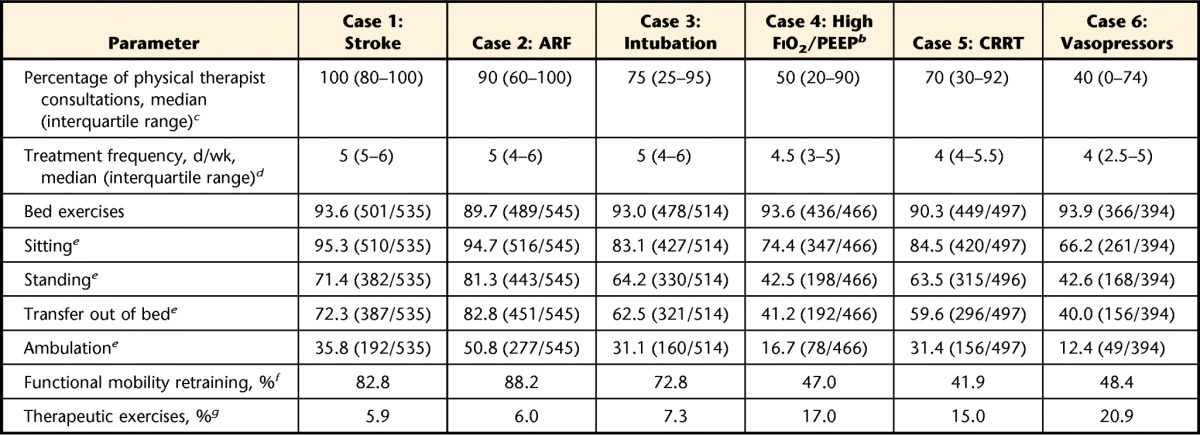
Data are reported as percentages (numbers) unless otherwise indicated. ARF=acute respiratory failure; FiO2=fraction of inspired oxygen; PEEP=positive end-expiratory pressure; CRRT=continuous renal replacement therapy via central venous access (nonfemoral); vasopressors=low, constant infusion of dobutamine, vasopressin, dopamine, or epinephrine.
b High FiO2 was defined as FiO2=0.70 (70% oxygen) and PEEP=10 cm H2O pressure.
c The frequency of consultation differed among the cases (P<.0001).
d The frequency of treatment differed among the cases (P<.0001).
e Progressive mobility (sitting to standing to transfer out of bed to ambulation) differed among the cases (P<.0001).
f The predicted benefit of functional mobility retraining decreased from cases 1 through 6 (P<.0001).
g The predicted benefit of therapeutic exercises increased from cases 1 through 6 (P<.0001).
Table 5.
Physical Therapists' Responses to 6 Case Scenarios Stratified by Academic Hospital (A) Versus Community Hospital (C)a
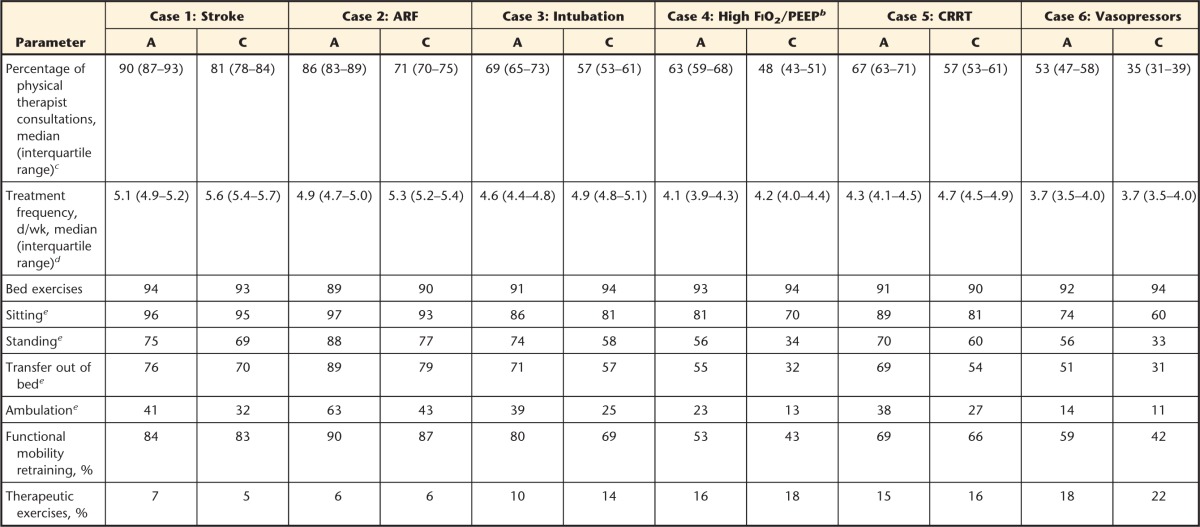
Data are reported as percentages unless otherwise indicated. ARF=acute respiratory failure; FiO2=fraction of inspired oxygen; PEEP=positive end-expiratory pressure; CRRT=continuous renal replacement therapy via central venous access (nonfemoral); vasopressors=low, constant infusion of dobutamine, vasopressin, dopamine, or epinephrine.
b High FiO2 was defined as FiO2=0.70 (70% oxygen) and PEEP=10 cm H2O pressure.
c The frequency of consultation differed for A versus C (P<.0001).
d The frequency of treatment differed for A versus C (P=.01).
e Progressive mobility (sitting to standing to transfer out of bed to ambulation) differed for A versus C (P<.0001).
Discussion
Physical therapy interventions aim to ameliorate physical and neurocognitive morbidity associated with critical illness and are safe and feasible in patients in the ICU.6–9 Our research revealed differences in current ICU-based physical therapist practice regionally and between academic and community hospital settings. Physical therapists frequently cited staffing, training, prioritization policies, sedation of patients, scheduling conflicts, and limited consultation criteria as barriers to rehabilitation in the ICU. Equipment in the ICU and the complexity of patients' medical conditions affected physical therapists' decision making and confidence in progressive mobilization.
On average, physical therapists who worked in the ICU had a mean of 7.8 years of direct ICU experience; predictably, the type of training most frequently cited in the present survey was informal training relying on mentorship and department-based competency requirements. The high prevalence of informal training was expected because formal training options are limited, with only 3 cardiovascular and pulmonary residencies and only 2 critical care fellowships currently credentialed by the American Board of Physical Therapy Residency and Fellowship Education.18 Interestingly, physical therapists working in community settings reported a higher percentage of formal training but also a higher percentage of no training than those working in academic settings.
These data reflect the need for continual internal and external competent mentorship. “Competent mentorship” implies that the mentor is truly competent in the knowledge, skills, and abilities that will enable safe and successful physical therapist practice in the ICU. Anecdotally, mentoring tasks are often delegated to senior staff members, but this informal training has important ramifications for the successful preparation of future physical therapists for work in the ICU in the United States and elsewhere. The 2010 Physical Therapy Workforce Project revealed that hospitals can expect a turnover rate of approximately 12%, including junior staff and senior staff equally.19 The practice analysis concluded that staffing shortages and consistent turnover mean that more time must be devoted to direct patient care, limiting the ability of senior staff to mentor junior staff.19 To meet the needs of patients who are critically ill and guide and develop the specialized practice of ICU-based physical therapy, a multifaceted approach is required. For example, entry-level physical therapy curricula and clinical education should include ICU-based objectives and student exposures,20 clinical competency requirements and practice guidelines should be developed in hospital settings and subjected to peer review,21 continuing education courses should be based on current practice guidelines and assessed by content experts, and residencies and fellowship programs need to be expanded.
Staffing in the ICU was more limited in academic hospitals than in community hospitals, and regional differences were also observed. These findings confirm that insufficient staffing remains a frequently cited and consistent barrier to providing rehabilitation to patients in the ICU.10,17 Although patient outcomes were not addressed in the present survey, it will be important to examine whether limited staffing has a negative effect on patient outcomes, similar to data for ICU physicians and nurses.22,23 Early rehabilitation studies by Bailey et al,6 Schweickert et al,7 and Morris et al9 advocated for daily physical therapist services, and Burtin et al8 provided bedside interventions 5 days per week. Consistent with these recommendations, daily physical therapist services after joint arthroplasty,24 after trauma to the pelvis or spine,25 or for patients with neurological issues26 decreased the length of stay. Given limited resources, physical therapists cannot meet the recommendation of daily interventions. Limited staffing may be one reason why daily physical therapist interventions were not recommended by the respondents for any of the case scenarios. In a European survey addressing ICU-based physical therapist services, greater than 75% of ICUs were reported to have at least one designated physical therapist who was equally responsible for respiratory therapy management and early mobilization.10 Increasing staffing to meet the needs of the ICU population will require reallocation of hospital resources but is supported by evidence demonstrating improved patient morbidity and positive financial incentives.17
Consistent with other ICU literature, barriers identified in the present survey included sedation of patients,27–29 lack of specific consultation criteria,16 and scheduling conflicts related to the timing of medical procedures.30,31 Our 2009 survey showed that only 10% of ICUs had established guidelines for physical therapist consultation, whereas the current survey revealed that 40% of ICUs had such guidelines, indicating that changes in ICU practice are ongoing.16 Other barriers identified in the present survey, such as staffing, prioritization policies, consultation criteria, and training of physical therapists, likewise should be surmountable but will require changes in physical therapy department staffing and prioritization standards, direct discussions with ICU medical and nursing directors to establish consultation and intervention guidelines, and changes in educational models to improve physical therapist training and readiness to work in the ICU.
With regard to physical therapists' perceptions and treatments provided, the case scenarios demonstrated that physical therapists would most commonly perform bed-level exercises. Their confidence in progressive mobilization would be influenced by the presence of endotracheal tubes, central venous access, and supportive technology, such as mechanical ventilation and renal replacement therapy. For example, although each of the case scenarios indicated that the patient was stable, ambulation would be included in the care plan for only a minority of patients (Tab. 4). Studies have demonstrated that ambulation is feasible and safe for patients who have respiratory failure and are orally intubated or receiving life-sustaining therapies, such as extracorporeal membrane oxygenation.32,33 In the present survey, progressive mobilization, including ambulation, was more likely to occur in academic hospitals. This finding may have been due to greater experience of physical therapists in acute care and ICU environments, the presence of departmental competency requirements, or greater access to ICU-related education that occurs as part of grand rounds or physician training programs.
Functional mobility retraining was predicted to be most advantageous for patients with the least complicated scenarios and less beneficial as the complexity of patients' medical conditions increased. Therapeutic exercise was believed to be more valuable with increasing complexity of patients' medical conditions. These findings are consistent with those of recent studies with pediatric and adult populations. In a Canadian survey of children who were critically ill, passive range of motion was the intervention that was most frequently applied and gait training was infrequently performed.34 Similarly, in 1-day point-prevalence studies conducted across Germany, Australia, and New Zealand, patients who required mechanical ventilation were rarely mobilized out of bed. The likelihood of being mobilized out of bed was still lower for patients who had an endotracheal tube.12,35
Our study had several important limitations. Members of APTA and the ACS may not represent most hospital-based physical therapists, and the return rate was 29%. Therefore, our results were prone to nonresponder bias, and the data may not represent the entire population studied.36 The use of survey response rates has been noted to be a common but ineffective way to determine nonresponder bias, and comparative information about the population of interest may allow greater generalizability.36,37 Additionally, according to the 2013 Acute Care Section Demographic Profile Summary, 1,623 members of the ACS reported practicing in the acute care setting for an average of 15.8 years (Acute Care Section, American Physical Therapy Association; personal communication; April 29, 2014). In the present study, the data presented were only from respondents who worked in the acute care setting, and these respondents had 13 years of experience. Therefore, the respondents in the present study were similar to practicing members of the ACS, and our 667 respondents represented 41% of practicing members of the ACS—a more robust return rate.
Furthermore, despite the relatively low response rate, a post hoc analysis of the survey return rate (667 of 2,320 surveys sent) suggested that the results were accurate (95% confidence with 3% error). Additionally, self-report surveys may tend to underreport behaviors deemed inappropriate or overreport ideal behaviors due to bias. Self-report surveys have the advantage that respondents are providing their own personal perspective of themselves and their individual practice. Finally, the survey would have been improved by the inclusion of operational definitions for several items (eg, facility-based training, departmental competency requirements, and likelihood of physical therapist consultation) and the addition of questions addressing delirium as a barrier and the presence of rehabilitation technicians in the ICU.
The findings of the present survey provide insight into physical therapist practice in the United States and perceptions of care and reveal differences between academic and community settings as well as regionally. Consistent with prior reports, institutional and departmental barriers limiting early ICU rehabilitation remain pervasive. Identification of barriers is an initial step in developing quality improvement initiatives to facilitate the delivery of physical therapist services for patients who are critically ill. The findings of the present study suggest that continued efforts to develop strategies to ensure adequate physical therapist staffing in the ICU, increased awareness of the evidence supporting ICU rehabilitation for improved patient functional outcomes and institutional cost savings, the development of ICU rehabilitation service consultation criteria, and improvements in the training of physical therapists for ICU practice are warranted.
Supplementary Material
Footnotes
Dr Malone, Dr Ridgeway, Dr Nordon-Craft, Dr Schenkman, and Dr M. Moss provided concept/idea/research design, fund procurement, and institutional liaisons. Dr Malone, Dr Nordon-Craft, and Dr Schenkman provided writing. Dr Malone and Mr P. Moss provided data collection and project management. Dr Malone provided data analysis. Mr P. Moss provided administrative support. Dr Ridgeway and Dr Nordon-Craft provided consultation (including review of manuscript before submission).
This study was approved by the Colorado Multiple Institutional Review Board.
This study was funded by National Institutes of Health grant R01NR011051.
References
- 1. Dejonghe B, Sharshar T, Lefaucheur JP, et al. Paresis acquired in the intensive care unit: a prospective multicenter study. JAMA. 2002;288:2859–2867. [DOI] [PubMed] [Google Scholar]
- 2. Stevens RD, Dowdy DW, Michaels RK, et al. Neuromuscular dysfunction acquired in critical illness: a systematic review. Intensive Care Med. 2007;33:1876–1891. [DOI] [PubMed] [Google Scholar]
- 3. Herridge MS, Cheung AM, Tansey CM, et al. One year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med. 2003;348:683–693. [DOI] [PubMed] [Google Scholar]
- 4. Cheung AM, Tansey CM, Tomlinson G, et al. Two-year outcomes, health care use and costs in survivors of ARDS. Am J Respir Crit Care Med. 2006;174:538–544. [DOI] [PubMed] [Google Scholar]
- 5. Herridge MS, Tansey CM, Matte A, et al. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011;364:1293–1304. [DOI] [PubMed] [Google Scholar]
- 6. Bailey P, Thomsen GE, Spuhler VJ, et al. Early activity is feasible and safe in respiratory failure patients. Crit Care Med. 2007;35:139–145. [DOI] [PubMed] [Google Scholar]
- 7. Schweickert WD, Pohlman MC, Pohlman AS, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet. 2009;373:1874–1882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Burtin C, Clerckx B, Robbeets C, et al. Early exercise in critically patients enhances short-term functional recovery. Crit Care Med. 2009;37:2499–2505. [DOI] [PubMed] [Google Scholar]
- 9. Morris PE, Griffin L, Berry M, et al. Receiving early mobility during an intensive care unit admission is a predictor of improved outcomes in acute respiratory failure. Am J Med Sci. 2011;341:373–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Norrenberg M, Vincent JL. A profile of European intensive care unit physiotherapists. Intensive Care Med. 2000;26:988–994. [DOI] [PubMed] [Google Scholar]
- 11. Needham DM. Mobilizing patients in the intensive care unit: improving neuromuscular weakness and physical function. JAMA. 2008;300:1685–1690. [DOI] [PubMed] [Google Scholar]
- 12. Nydahl P, Ruhl AP, Bartoszek G, et al. Early mobilization of mechanically ventilated patients: a 1-day point-prevalence study in Germany. Crit Care Med. 2014;42:1178–1186. [DOI] [PubMed] [Google Scholar]
- 13. Chaboyer W, Gass E, Foster M. Patterns of chest physiotherapy in Australian intensive care units. J Crit Care. 2004;19:145–151. [DOI] [PubMed] [Google Scholar]
- 14. Wiles L, Stiller K. Passive limb movements for patients in an intensive care unit: a survey of physiotherapy practice in Australia. J Crit Care. 2010;25:501–508. [DOI] [PubMed] [Google Scholar]
- 15. King J, Crowe J. Mobilization practices in Canadian critical care units. Physiother Can. 1998;50:206–211. [Google Scholar]
- 16. Hodgin K, Nordon-Craft A, McFann K, et al. Physical therapy utilization in intensive care units: results from a national survey. Crit Care Med. 2009;37:561–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lord RK, Mayhew CR, Korupolu R, et al. ICU early physical rehabilitation programs: financial modeling of cost savings. Crit Care Med. 2013;41:717–724. [DOI] [PubMed] [Google Scholar]
- 18. American Board of Physical Therapy Residency and Fellowship Education. Residency and fellowship programs. ABPTRFE website. Available at: http://www.abptrfe.org/home.aspx Accessed June 9, 2015.
- 19. Physical Therapy Workforce Data. Physical therapy vacancy and turnover rates in acute care hospitals. American Physical Therapy Association website. Available at: http://www.apta.org/WorkforceData/ Accessed June 9, 2015.
- 20. Rapport MJ, Sweeney JK, Dannemiller L, Heriza CB. Student experiences in the neonatal intensive care unit: addendum to neonatal physical therapy competencies and clinical training models. Pediatr Phys Ther. 2010;22:439–440. [DOI] [PubMed] [Google Scholar]
- 21. Sweeney JK, Heriza CB, Blanchard Y. Neonatal physical therapy, part I: clinical competencies and neonatal intensive care unit clinical training models. Pediatr Phys Ther. 2009;21:296–307. [DOI] [PubMed] [Google Scholar]
- 22. Pronovost PJ, Jenckes MW, Dorman T. Organizational characteristics of intensive care units related to outcomes of abdominal aortic surgery. JAMA. 1999;281:1310–1317. [DOI] [PubMed] [Google Scholar]
- 23. Pronovost PJ, Angus DC, Dorman T, et al. Physician staffing patterns and clinical outcomes in critically ill patients: a systematic review. JAMA. 2002;288:2151–2162. [DOI] [PubMed] [Google Scholar]
- 24. Hughes K, Kuffner L, Dean B. Effect of weekend physical therapy treatment on postoperative length of stay following total hip and total knee arthroplasty. Physiother Can. 1993;45:245–249. [PubMed] [Google Scholar]
- 25. Holden MK, Daniele CA. Comparison of seven- and five-day physical therapy coverage in patients with acute orthopedic disorders. Phys Ther. 1987;67:1240–1246. [DOI] [PubMed] [Google Scholar]
- 26. Rapoport J, Judd Van Eerd M. Impact of physical therapy weekend coverage on length of stay in an acute care community hospital. Phys Ther. 1989;69:32–37. [DOI] [PubMed] [Google Scholar]
- 27. Pohlman MC, Schweickert WD, Pohlman AS, et al. Feasibility of physical and occupational therapy beginning from initiation of mechanical ventilation. Crit Care Med. 2010;38:2089–2094. [DOI] [PubMed] [Google Scholar]
- 28. Zanni JM, Korupolu R, Fan E, et al. Rehabilitation therapy and outcomes in acute respiratory failure: an observational pilot project. J Crit Care. 2010;25:254–262. [DOI] [PubMed] [Google Scholar]
- 29. Appleton RTD, MacKinnon M, Booth MG, et al. Rehabilitation within Scottish intensive care units: a national survey. Journal of the Intensive Care Society. 2011;12:221–227. [Google Scholar]
- 30. Leditschke IA, Green M, Irvine H, et al. What are the barriers to mobilizing intensive care patients? Cardiopulm Phys Ther J. 2012;23:26–29. [PMC free article] [PubMed] [Google Scholar]
- 31. Bakhru RN, Fuchs BD, Butler K, et al. Barriers to early mobilization of critically ill patients [abstract]. Am J Respir Crit Care Med. 187;2013:A3900. [Google Scholar]
- 32. Needham DM, Korupolu R, Zanni JM, et al. Early physical medicine and rehabilitation for patients with acute respiratory failure: a quality improvement project. Arch Phys Med Rehabil. 2010;91:536–542. [DOI] [PubMed] [Google Scholar]
- 33. Rehder KJ, Turner DA, Hartwig MG, et al. Active rehabilitation during extracorporeal membrane oxygenation as a bridge to lung transplantation. Respir Care. 2013;58:1291–1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Choong K, Koo KK, Clark H, et al. Early mobilization in critically ill children: a survey of Canadian practice. Crit Care Med. 2013;41:1745–1753. [DOI] [PubMed] [Google Scholar]
- 35. Berney SC, Harrold M, Webb SA, et al. Intensive care unit mobility practices in Australia and New Zealand: a point prevalence study. Crit Care Resusc. 2013;15:260–265. [PubMed] [Google Scholar]
- 36. Halbesleben JR, Whitman MV. Evaluating survey quality in health services research: a decision framework for assessing nonresponse bias. Health Serv Res. 2013;48:913–930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Davern M. Health nonresponse rates are a problematic indicator of nonresponse bias in survey research. Health Serv Res. 2013;48:905–912. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


