Abstract
Background
A wide variety of hip abduction and hip external rotation exercises are used for training, both in athletic performance and in rehabilitation programming. Though several different exercises exist, a comprehensive understanding of which exercises best target the gluteus maximus (Gmax) and gluteus medius (Gmed) and the magnitude of muscular activation associated with each exercise is yet to be established.
Purpose
The purpose of this systematic review was to quantify the electromyographic (EMG) activity of exercises that utilize the Gmax and Gmed muscles during hip abduction and hip external rotation.
Methods
Pubmed, Sports Discuss, Web of Science and Science Direct were searched using the Boolean phrases (gluteus medius OR gluteus maximus) AND (activity OR activation) AND (electromyography OR EMG) AND (hip abduction OR hip external rotation). A systematic approach was used to evaluate 575 articles. Articles that examined injury‐free participants of any age, gender or activity level were included. No restrictions were imposed on publication date or publication status. Articles were excluded when not available in English, where studies did not normalize EMG activity to maximum voluntary isometric contraction (MVIC), where no hip abduction or external rotation motion occurred or where the motion was performed with high acceleration.
Results
Twenty‐three studies met the inclusion criteria and were retained for analysis. The highest Gmax activity was elicited during the lateral step up, cross over step up and rotational single leg squat (ranging from 79 to 113 % MVIC). Gmed activity was highest during the side bridge with hip abduction, standing hip abduction with elastic resistance at the ankle and side lying hip abduction (ranging from 81 to 103 % MVIC).
Limitations
The methodological approaches varied between studies, notably in the different positions used for obtaining MVIC, which could have dramatically impacted normalized levels of gluteal activation, while variation also occurred in exercise technique and/or equipment.
Conclusions
The findings from this review provide an indication for the amount of muscle activity generated by basic strengthening and rehabilitation exercises, which may assist practitioners in making decisions for Gmax and Gmed strengthening and injury rehabilitation programs.
Keywords: EMG, gluteal musculature, hip strength, rehabilitation
INTRODUCTION
A wide variety of hip abduction and hip external rotation exercises are used for training, both in athletic performance and in rehabilitation programming. Though several different exercise protocols exist, scientific evaluation of their specific effects on the gluteus maximus (Gmax) and gluteus medius (Gmed) has yet to establish which exercises activate the musculature and what level of activation is elicited. The primary actions of the Gmax are hip extension and hip external rotation,1–3 with the superior area of the Gmax also functioning as a hip abductor.4,5 The Gmed functions as a hip abductor2 and hip rotator6 with the anterior area of the Gmed performing hip internal rotation while the posterior area performs hip external rotation.2,7 The gluteal musculature may significantly participate in dual roles of enhancing athletic performance3,8–10 while preventing and contributing to the rehabilitation of lower extremity injuries.10–14 The Gmax and Gmed musculature extensively contribute to weight bearing movements by assisting in load transference through the hip joint,15 supplying local structural stability to the hip joint and maintaining lower extremity alignment of the hip and knee joints.16 Performance deficiency in these selected hip muscles results in altered pelvofemoral biomechanics which is linked to lower extremity pathology.3,17–19 This is highlighted when the hip abductors and external rotators fail to produce sufficient torque during weight bearing movements resulting in excessive hip adduction and internal rotation, an increase in knee valgus angle and pelvic drop.17–20
Hip abductor weakness may lead individuals to adopt movement strategies to mask their weakness,21 resulting in compensatory motions at the lower back, hip, and knee.5,10,22 Consequently, individuals performing these movements are often observed doing both hip abduction and excessive lateral pelvic movement caused by increased activity of the quadratus lumborum.23 Gluteal weakness and ensuing hip dysfunction has a strong relationship (r = −.74) with knee pathology24 while a specific weakness in hip abduction and external rotation has been associated with patellofemoral pain syndrome.3,25 Janda and Jull26 and, Page, Frank and Lardner27 have suggested that an association between gluteal musculature inhibition and low back pain exists. Moreover, a weakness in hip abductor musculature and thus subsequent strengthening exercises are prescribed for iliotibial band syndrome,28,29 chronic ankle instability30,31 and patellofemoral pain syndrome.32,33
Examining hip abductor strength can be accomplished through various clinical tools and procedures and in both non‐weight‐bearing (NWB) body positions: side‐lying or supine and in a weight‐bearing (WB) body position: standing.34 The side‐lying position is frequently utilized to test hip abductor muscle strength in clinical settings35 and is generally the suggested position by manufacturers of isokinetic testing devices.34 The supine position neutralizes the effects of gravity and provides an option for individuals to avoid lying on an injured affected side36 while the standing position is proposed by Cahalan, Johnson and Chao37 to be the most functional position when assessing hip abductor strength as the majority of daily living activities involve hip abduction performed in this position. Wilder et al34 noted that most variations between hip abductor strength exist due to the chosen testing position.
Electromyography (EMG) may be used to assess the activation of a muscle as measured by electrical activity levels, with the general consensus assumed that exercises producing higher levels of activation are generally accepted to be more appropriate to use for strengthening.38 It has been proposed that the minimum effort to obtain a strengthening stimulus is approximately 40‐60% of a maximum voluntary isometric contraction (MVIC)38–42 with muscle activity of less than 25 % MVIC indicating that the muscle is functioning in an endurance capacity or to maintain stability.38 To assist with classification of low to high muscle activity in this article, the authors of the current study have used a classification scheme of activity.43–45 Activity from 0 % to 20 % MVIC is considered low level, 21 % to 40 % MVIC a moderate level, 41 % to 60 % MVIC a high level, while greater than 60 % MVIC a very high level. Analyzing exercises in such a manner may contribute to understanding neuromuscular control during activities and assist in assessing, selecting, and systematically progressing exercises.46
With this in mind the purpose and focus of this systematic review was to quantify the EMG activity associated with WB and NWB exercises that utilized hip abduction or external rotation. Exercises were grouped into levels of % MVIC as per the classification scheme43–45 to assist practitioners in making decisions for Gmax and Gmed strengthening and rehabilitation. The authors hypothesized that exercises that are more demanding in movement i.e. dynamic exercise that requires a changes in angle from more than one joint and therefore requires greater joint stabilization, would result in greater levels of % MVIC.
METHODS
Literature Search Strategies
The review was conducted in accordance with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta‐analyses) statement guidelines.47 A systematic search of the research literature was undertaken for studies that investigated EMG activity (given as mean % MVIC) for either the Gmax or Gmed in resistance training exercises (bodyweight, band, cable, free‐weight, machine) that utilized dynamic hip abduction or external rotation. Studies were found by searching Pubmed, Sports Discuss, Web of Science and Science Direct electronic databases from inception to March 2015. The following Boolean search phrases were used (gluteus medius OR gluteus maximus) AND (activity OR activation) AND (electromyography OR EMG) AND (hip abduction OR hip external rotation). Additional studies were also found by reviewing the reference lists from retrieved studies.
Inclusion and Exclusion Criteria
Articles that examined injury‐free participants of any age, sex or activity level were included. No restrictions were imposed on publication date or publication status. Studies were limited to English language. Studies were excluded that examined isometric hip abduction or external rotation movements (e.g. standing wall‐push exercise) as well as single leg hip extension movements (e.g. lunge and single leg bridge) as even though there is frontal/transverse plane stability and torque required, there is no hip abduction or external rotation motion required. Some exercises such as the lateral lunge, lateral step‐up and cross over step‐up were included since they involve hip abduction/external rotation motion and torque production, but movements like these do contain an unfair advantage since they also require hip extension torque and movement in the sagittal plane. Despite their combined action, authors made a judgment call to include them in the current analysis as these exercises are typically used in a physiotherapeutic setting for injury rehabilitation type activity. Plyometric or hopping movements were also excluded as they are performed with higher acceleration, thus they have an unfair advantage in terms of eliciting high levels of gluteal activation. Moreover, plyometric exercises are higher end performance type exercises and should be used once an individual exhibits prerequisite strength levels (eccentric) which includes activation, mobility and stability. Additionally studies were excluded that did not normalize EMG activity to MVIC.
Study Selection
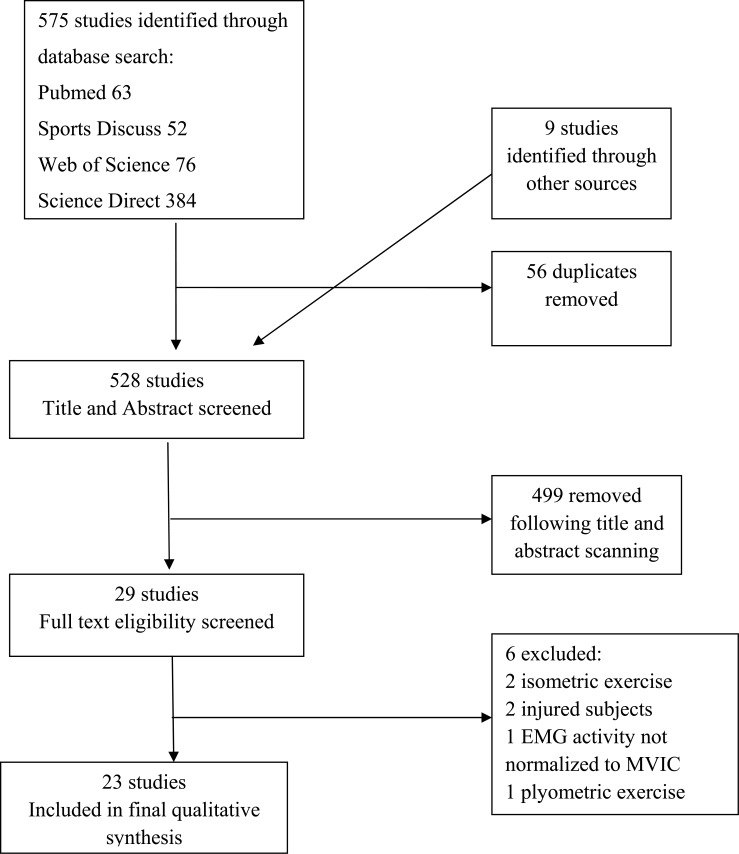
A search of electronic databases and a scan of article reference lists revealed 575 relevant studies (Figure 1). After applying the inclusion and exclusion criteria 23 studies were retained for further analysis.
Figure 1.
Flow chart of information through the different phases of the systematic review
RESULTS
There were a total number of 467 subjects (194 male, 197 female, 76 sex not provided) while the total number of exercise variations were 52. See Appendix 1 for details on all included studies.
Exercise Position
The studies considered in this systematic review were conducted in either a WB position (standing) or a NWB position (side‐lying and seated).
Standing position
Information regarding the gluteal activation for the standing position can be observed in Table 1. Eighteen studies used this position with twenty‐six exercise variations and 363 subjects. The most commonly studied exercise variation was the lateral step up (126 subjects). The highest Gmax (113.8 ± 89.5 % MVIC) activation occurred in the lateral step up,14 however, when averaged from six studies, the activation level was 49.6 ± 15 % MVIC. The highest Gmed (101 ± 7 % MVIC) activation occurred in the standing hip abduction Thera band at ankle (Borg (Borg Rating of Perceived Exertion CR10) ≥ 7 load)46 When all data was pooled, the average Gmax activation was 34.7 ± 14.3 % MVIC and the average Gmed activation was 47.2 ± 17.2 % MVIC for the standing exercise variations (see Table 4).
Table 1.
Comparison of muscle activation in the Gluteus Maximus and Gluteus Medius for all standing exercises. Values given as the mean and the standard deviation.
| Exercise | Number of Studies | Number of Subjects | Range % MVIC | Average % MVIC | ||
|---|---|---|---|---|---|---|
| Gmax | Gmed | Gmax | Gmed | |||
| Cross over step up | 1 | 15 | 103 ± 63.6 | 57.6 ± 19.5 | 103 ± 63.6 | 57.6 ± 19.5 |
| Lateral lunge | 2 | 61 | 41 ± 20 – 12 ± 3 | 39 ± 19 ‐ 13 ± 2 | 26.5 ± 11.5 | 26 ± 10.5 |
| Lateral stepping band at foot | 1 | 9 | 8 ± 5 | 35 ± 10 | 8 ± 5 | 35 ± 10 |
| Lateral stepping band at ankle | 3 | 50 | 27 ± 16 ‐ 6 ± 4 | 61 ± 34 ‐ 29 ± 9 | 15 ± 9.3 | 24 ± 20 |
| Lateral stepping band at knee | 2 | 29 | 27.4 ± 16.4‐ 5 ± 3 | 30.2 ± 15.2 ‐ 24 ± 9 | 16.2 ± 9.7 | 27.8 ± 12.1 |
| Lateral stepping , hip internally rotated band at ankle | 1 | 21 | 13 ± 9.1 | 43.8 ± 27 | 13 ± 9.1 | 43.8 ± 27 |
| Lateral stepping, hip externally rotated band at ankle | 1 | 21 | 27.3 ± 18.1 | 27.3 ± 18.1 | 14.8 ± 10.7 | 27.3 ± 18.1 |
| Lateral step up | 6 | 126 | 113.8 ± 9.5 ‐ 29 ± 13 | 59.8 – 18 ± 18 | 49.6 ± 15 | 41.4 ± 16.7 |
| Lateral step up with 10% BM | 1 | 13 | 23 ± 11 | ‐ | 23 ± 11 | ‐ |
| Lateral step up with 25 %BM | 1 | 19 | 20 ± 8 | ‐ | 20 ± 8 | ‐ |
| Monster walk band at foot | 1 | 9 | 6 ± 3 | 27 ± 10 | 6 ± 3 | 27 ± 10 |
| Monster walk band at ankle | 1 | 9 | 5 ± 2 | 25 ± 10 | 5 ± 2 | 25 ± 10 |
| Monster walk band at knee | 1 | 9 | 4 ± 2 | 19 ± 9 | 4 ± 2 | 19 ± 9 |
| Pelvic drop (standing hip abduction / adduction) | 3 | 49 | 17 ± 15 | 57 ± 32 ‐ 29.2 ± 10.6 | 17 ± 15 | 49.3 ± 25.6 |
| Shoulder dump (overhead throwing movement into hip rotation) | 1 | 30 | 28 ± 3 | ‐ | 28 ± 3 | ‐ |
| Standing hip abduction | 2 | 29 | ‐ | 33 ± 23 ‐ 30 ± 21 | ‐ | 31.5 ± 22 |
| Standing hip abduction with hip and knee in 20 ° of flexion | 1 | 16 | ‐ | 28 ± 21 | ‐ | 28 ± 21 |
| Standing hip abduction with 3% BM | 1 | 16 | ‐ | 42 ± 27 | ‐ | 42 ± 27 |
| Standing hip abduction with 3% BM and hip and knee in 20 ° of flexion | 1 | 16 | ‐ | 46 ± 34 | ‐ | 46 ± 34 |
| Standing hip abduction band at ankle (Borg ≤ 2) | 1 | 16 | 59 ± 10 | 73 ± 7 | 59 ± 10 | 73 ± 7 |
| Standing hip abduction band at ankle (Borg ≤ 2‐ < 5) | 1 | 16 | 65 ± 9 | 88 ± 7 | 65 ± 9 | 88 ± 7 |
| Standing hip abduction band at ankle (Borg ≤ 5‐ < 7) | 1 | 16 | 68 ± 11 | 93 ± 8 | 68 ± 11 | 93 ± 8 |
| Standing hip abduction band at ankle (Borg ≥ 7) | 1 | 16 | 73 ± 25 | 101 ± 7 | 73 ± 25 | 101 ± 7 |
| Standing hip abduction with band at ankle | 1 | 26 | 16.6 ± 10.8 | 52.9 ± 17.6 | 16.6 ± 10.8 | 52.9 ± 17.6 |
| Rotational single leg squat | 1 | 9 | 79 ± 45 | 68 ± 15 | 79 ± 45 | 68 ± 15 |
| Transverse lunge | 2 | 30 | 58 ± 23‐ 49 ± 20, | 68 ± 62 ‐ 48 ± 21 | 53.5 ± 26 | 58 ± 45.5 |
BM = Body Mass Gmax = Gluteus Maximus Gmed = Gluteus Medius MVIC = Maximum voluntary isometric contraction Borg = Borg Rating of Perceived Exertion
Table 4.
Summary of average % MVIC for Gluteus Maximus and Gluteus Medius in different exercise positions. Values given as the mean and the standard deviation.
| Exercise Position | Standing | Side‐lying | Seated |
|---|---|---|---|
| Number of Studies | 17 | 12 | 1 |
| Number of Subjects | 363 | 244 | 16 |
| Number of Exercises | 26 | 22 | 4 |
| Gmax Average % MVIC | 34.7 ± 14.3 | 30.4 ± 23.8 | 68.8 ± 10 |
| Gmed Average % MVIC | 47.2 ± 17.4 | 41.9 ± 16.5 | 65.3 ± 7.5 |
Gmax = Gluteus Maximus Gmed = Gluteus Medius MVIC = Maximum voluntary isometric contraction
Side‐lying position
Details of gluteal activation for the side‐lying position can be observed in Table 2. Twelve studies used this position with twenty‐two different exercise variations and 244 subjects. The most commonly studied exercise variation was the side‐lying hip abduction (197 subjects). The highest Gmax (72.8 % MVIC) and Gmed (103 % MVIC) activation was associated with the side bridge with abduction dominant leg (DL) down exercise.51 When all data was pooled the average Gmax activation was 30.4 ± 23.8 % MVIC and the average Gmed activation was 41.9 ± 16.5 % MVIC for the side lying exercise variations (see Table 4).
Table 2.
Comparison of muscle activation in the Gluteus Maximus and Gluteus Medius for all side lying exercises. Values given as the mean and the standard deviation.
| Exercise | Number of Studies | Number of Subjects | Range% MVIC | Average % MVIC | ||
|---|---|---|---|---|---|---|
| Gmax | Gmed | Gmax | Gmed | |||
| Clam shell with pelvic belt | 1 | 20 | 33 ± 23 | 21 ± 12 | 33 ± 23 | 21 ± 12 |
| Clam shell with band at knee | 1 | 20 | 43.6 ± 26.1 | 26.9 ± 18 | 43.6 ± 26.1 | 26.9 ± 18 |
| Clam shell with 5% BM | 1 | 20 | 34 ± 25 | 33 ± 17 | 34 ± 25 | 33 ± 17 |
| Clam shell 1 | 2 | 36 | 53.1– 20.5 ± 18.4 | 47.2‐16.4 ± 11.3 | 36.8 | 31.5 |
| Clam shell 2 | 1 | 26 | 12.3 | 62.4 | 12.3 | 62.4 |
| Clam shell 3 | 1 | 26 | 26.6 | 67.6 | 26.6 | 67.6 |
| Clam shell 4 | 1 | 26 | 26.2 | 76.8 | 26.2 | 76.8 |
| Clam shell PNHIP0 | 2 | 27 | 15 | 18 ‐9.4 | 15 | 13.7 |
| Clam shell PNHIP30 | 2 | 38 | 34 ± 27 ‐ 17 | 40 ± 38 ‐ 22 | 25.5 | 31 |
| Clam shell PNHIP60 | 3 | 58 | 39 ± 34 ‐ 20 | 38 ± 29 ‐ 23 | 23.6 ± 26 | 24 ± 20 |
| Clam shell PRHIP0 | 1 | 17 | 10 | 12 | 10 | 12 |
| Clam shell PRHIP30 | 1 | 17 | 9 | 13 | 9 | 13 |
| Clam shell PRHIP60 | 1 | 17 | 12 | 18 | 12 | 18 |
| Side bridge with abduction DL down | 1 | 26 | 72.8 | 103 | 72.8 | 103 |
| Side bridge with abduction DL up | 1 | 26 | 70.9 | 88.8 | 70.9 | 88.8 |
| Side lying hip abduction | 9 | 197 | 51.1 – 21 ± 16 | 81.2 ‐ 26.8 ± 12.8 | 32.4 ± 17 | 45.2 ± 16.2 |
| Side lying hip abduction with 5% BM | 1 | 20 | 25.3 ± 24.6 | 79.1 ± 29.9 | 25.3 ± 24.6 | 79.1 ± 29.9 |
| Side‐lying hip abduction with 5% BM and external rotation | 1 | 20 | 31.7 ± 24.1 | 54.3 ± 24.8 | 31.7 ± 24.1 | 54.3 ± 24.8 |
| Side‐lying hip abduction with pelvic belt | 1 | 20 | 37.3 ± 24.9 | 34.2 ± 15.9 | 37.3 ± 24.9 | 34.2 ± 15.9 |
| Side‐lying hip abduction against a wall | 1 | 10 | ‐ | 25.9 ± 5.65 | ‐ | 25.9 ± 5.65 |
| Side‐lying hip abduction Internal rotation | 2 | 30 | ‐ | 35.3 ± 12.5 ‐ 26.7 ± 6.7 | ‐ | 31.7 ± 9.6 |
| Side‐lying hip abduction External rotation | 2 | 30 | ‐ | 45.3 ± 20.5 ‐ 13 ± 4.25 | ‐ | 29.1 ± 12.5 |
BM = Body Mass DL = Dominant Leg Gmax = Gluteus Maximus Gmed = Gluteus Medius MVIC = Maximum voluntary isometric contraction Clam Shell 1 = Side‐lying with hips flexed to 45 °. Externally rotate top leg Clam Shell 2 = same as Clam 1 but internally rotate the top leg (knees together) Clam Shell 3 = Top thigh raised to parallel to table with hip in neutral rotation and 45 ° of flexion. Top leg then internally rotated. Knee height remains the same throughout the entire movement. Clam Shell 4 = Same as 3 except the top leg is in extension Clam shell PNHIP0 = pelvis neutral, hip in 0 ° of flexion Clam shell PNHIP30 = pelvis neutral, hip in 30 ° of flexion Clam shell PNHIP60 = pelvis neutral, hip in 60 ° of flexion Clam shell PRHIP0 = pelvis reclined, hip in 0 ° of flexion Clam shell PRHIP30 = pelvis reclined, hip in 30 ° of flexion Clam shell PRHIP60 = pelvis reclined, hip in 60 ° of flexion Borg = Borg Rating of Perceived Exertion CR10
Seated Position
Specifics regarding gluteal activation for the seated position are detailed in Table 3. One study used this position with four different exercise variations and sixteen subjects. The highest Gmax (70.8 ± 11 % MVIC) and Gmed (80 ± 8 % MVIC) activation was associated with the seated hip abduction machine (Borg ≥ 7 load).40 When all data was pooled, the average Gmax activation was 66.7 ± 10 % MVIC and the average Gmed activation was 65.2 ± 7.2 % MVIC for the seated variations (see Table 4).
Table 3.
Comparison of muscle activition in the Gluteus Maximus and Gluteus Medius for all seated exercises. Values given as the mean and the standard deviation.
| Exercise | Number of Studies | Number of Subjects | Range % MVIC | Average % MVIC | ||
|---|---|---|---|---|---|---|
| Gmax | Gmed | Gmax | Gmed | |||
| Seated hip abduction machine (Borg ≤ 2) | 1 | 16 | 67 ± 9 | 53 ± 7 | 67 ± 9 | 53 ± 7 |
| Seated hip abduction machine (Borg ≤ 2‐ < 5) | 1 | 16 | 65 ± 10 | 61 ± 7 | 65 ± 10 | 61 ± 7 |
| Seated hip abduction machine (Borg ≤ 5‐ < 7) | 1 | 16 | 69 ± 10 | 67 ± 7 | 69 ± 10 | 67 ± 7 |
| Seated hip abduction machine (Borg ≥ 7) | 1 | 16 | 70 ± 11 | 80 ± 8 | 70 ± 11 | 80 ± 8 |
Gmax = Gluteus Maximus Gmed = Gluteus Medius MVIC = Maximum voluntary isometric contraction Borg = Borg Rating of Perceived Exertion CR10
Summary of positions
Details of gluteal activation for all positions are summarized in Table 4. For both Gmax and Gmed, the standing position produced a higher activation compared to the side‐lying position whilst the seated position produced the highest average activation for both Gmax (66.7 ± 10 % MVIC) and Gmed (65.2 ± 7.2 % MVIC). While the seated position produced the highest activation, only one study used exercises in that position.
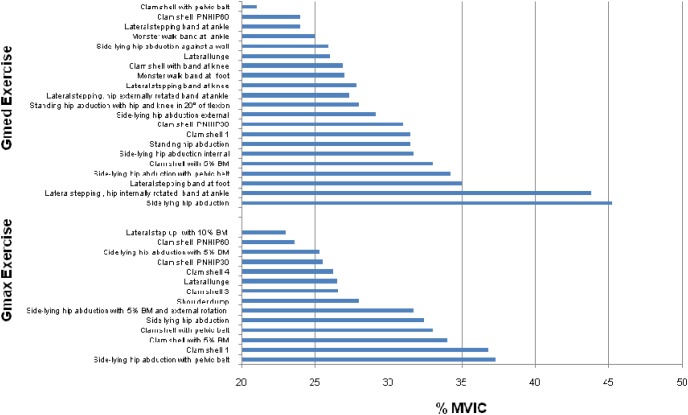
Exercise EMG Activity Level (% MVIC)
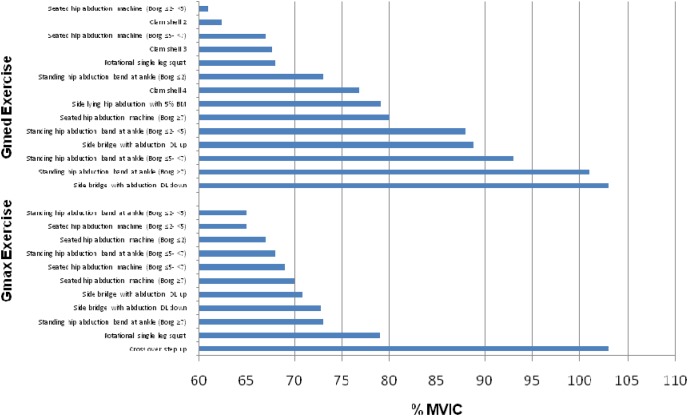
The magnitude of mean gluteal activation is stratified into the four levels of activity43–45 in Figures 2‐5. This classification scheme provides a means by which the practitioner can select exercises, that match the strength status of their client/athlete and also provides a means by which strengthening of the gluteals can be progressively overloaded in a systematic fashion.
Figure 2.
Mean Gluteus Maximus (Gmax) and Gluteus Medius (Gmed) exercises with very high activation (>60% of averaged EMG/MVIC).
BM = Body mass MVIC = Maximum voluntary isometric contraction Borg = Borg Rating of Perceived Exertion CR10 DL = Dominant leg Clam Shell 2 = Side‐lying with hips flexed at 45 °. Internally rotate the top leg (knees together) Clam Shell 3 = Top thigh raised to parallel to table with hip in neutral rotation and 45 ° of flexion. Top leg then internally rotated. Knee height remains the same throughout the entire movement Clam Shell 4 = Same as 3 except the top leg is in extensio
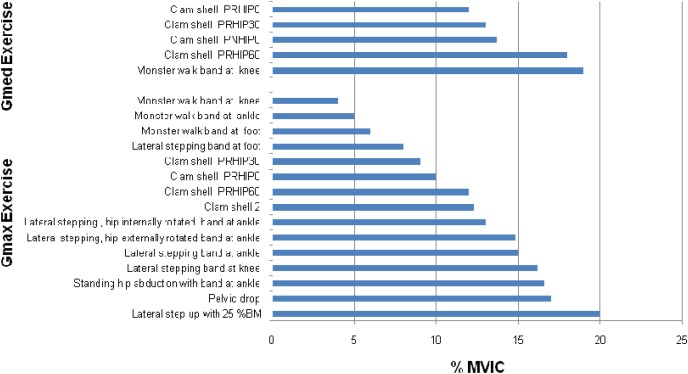
Figure 5.
Mean Gluteus Maximus (Gmax) and Gluteus Medius (Gmed) exercises with low activation (0‐20% of averaged EMG/MVIC).
BM = Body Mass MVIC = Maximum voluntary isometric contraction Clam Shell 2 = Side‐lying with hips flexed at 45 °. Internally rotate the top leg (knees together) Clam shell PNHIP0 = pelvis neutral, hip in 0 ° of flexion Clam shell PRHIP0 = pelvis reclined, hip in 0 ° of flexion Clam shell PRHIP30 = pelvis reclined, hip in 30 ° of flexion Clam shell PRHIP60 = pelvis reclined, hip in 60 ° of flexion
Very High EMG Activity Exercise
The very high activity exercises (Gmax: 11 exercises, Gmed: 14 exercises) can be observed in Figure 2. The cross over step up exercise produced the highest Gmax activation (103 ± 63.6 % MVIC), while the side bridge with hip abduction DL down produced the highest Gmed activation (103% MVIC).
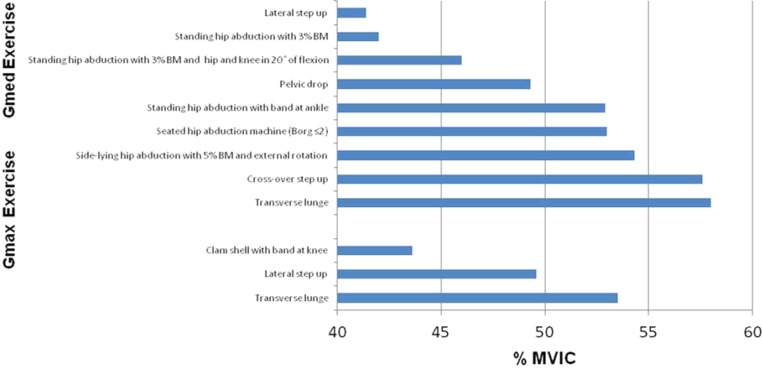
High EMG Activity Exercise
The high activity exercises (Gmax: 4 exercises, Gmed: 8 exercises) are detailed in Figure 3. This tier had the fewest number of exercises (12) compared to the other activation tiers with 9 of the exercises performed in the standing position.
Figure 3.
Mean Gluteus Maximus (Gmax) and Gluteus Medius (Gmed) exercises with high activation (>41 – 60% of averaged EMG/MVIC).
BM = Body mass MVIC = Maximum voluntary isometric contraction Borg = Borg Rating of Perceived Exertion CR10
Moderate EMG Activity Exercise
Moderate activity exercises (Gmax: 21 exercises, Gmed: 14 exercises) of the gluteal musculature can be viewed in Figure 4. This tier had the highest number of exercises (total 35).
Figure 4.
Mean Gluteus Maximus (Gmax) and Gluteus Medius (Gmed) exercises with moderate (>21 – 40% of averaged EMG/MVIC).
BM = Body mass MVIC = Maximum voluntary isometric contraction Borg = Borg Rating of Perceived Exertion CR10 DL = Dominant leg Clam Shell 1 = Side‐lying with hips flexed at 45 °. Externally rotate top Clam Shell 3 = Top thigh raised to parallel to table with hip in neutral rotation and 45 ° of flexion. Top leg then internally rotated. Knee height remains the same throughout the entire movement Clam Shell 4 = Same as 3 except the top leg is in extension PNHIP0 = pelvis neutral, hip in 0 ° of flexion Clam shell PNHIP30 = pelvis neutral, hip in 30 ° of flexion Clam shell PNHIP60 = pelvis neutral, hip in 60 ° of flexion
Low EMG Activity Exercise
The low activation exercises (Gmax: 15 exercises, Gmed: 5 exercises) are shown in Figure 5. Exercises in this tier corresponded considerably more to Gmax activation than Gmed. Three variations of the monster walk exercise required the least amount of activation for the Gmax (range 4‐6 % MVIC) while four variations of the clam shell exercise elicited the lowest amount of activation for the Gmed (ranging from 12‐18 % MVIC).
DISCUSSION
The results of this systematic review indicate that EMG activation (% MVIC) of the Gmax and Gmed musculature from hip abduction and external rotation exercises varied greatly depending on the position and complexity of the movement. Andersen et al38 proposed that exercises with higher % MVIC values are necessary for strength gains. A factor in strength progression is exercise intensity, indicated through EMG data with a greater % MVIC requiring greater motor control and joint stabilisation.38 Therefore, for enhancing muscular strength in a rehabilitation setting, it is valuable to be aware of the level of muscle activation an exercise elicits. Moreover, Boren et al52 noted that by knowing a muscles % MVIC during various exercises, the strengthening potential can be inferred. Exercises performed in a WB position produced a greater % MVIC compared to a NWB position for both muscle groups, with Gmed activity levels higher than Gmax in both positions. The top three Gmax and two of the top three Gmed EMG activity exercises were performed in a WB position suggesting that standing exercises imposed greater demands of the musculature and changes to the base of support can affect the activity level of the Gmax and Gmed.
Although several exercises in the very high tier are demanding, thus potentially inappropriate for beginners or weaker individuals due to the high stability requirements, the clam shell exercises versions 2 – 4 (ranging 62.4‐76.8 % MVIC) can be used to elicit strengthening of the Gmed as the side‐lying position provides stabilization. Clam shell version 2 requires internal hip rotation from a side‐lying position at 45 ° hip flexion, version 3 has internal hip rotation performed from the top leg which is raised and held in an abducted position, whilst version 4 is the same as version 3 but the top leg is in extension. Moreover, individuals who are unable to perform WB exercises can benefit from performing clam shell exercises and other NWB side‐lying exercises. The side lying abduction exercise is commonly prescribed by practitioners, evidenced by being used in nine studies with EMG activity ranging from 21.3 ‐ 51.1 % MVIC for the Gmax and 26.8 ‐ 81.2 % MVIC for the Gmed. The variance in EMG activity can be most likely attributed to differing testing positions such as the angle at which abduction was maintained, pelvis position and whether the leg abducted was in hip flexion or hip extension. Three other side‐lying abduction exercises produced moderate activation of the Gmax (range 25.3 – 37.3 % MVIC) noting its role as a secondary hip abductor, while six variations of the clam exercise highlight the Gmax's role as a lateral rotator (range 26.2 ‐39 % MVIC).
The greater demands of the step up exercises as demonstrated by greater Gmed activity, highlight the synergist role of the Gmed in maintaining pelvis and knee stability (cross over step up 57.6 ± 19.5 and mean lateral step up 41.4 ± 16.7 % MVIC). Variations in EMG activation during the lateral step up exercise may be attributed to an individual's familiarity with the complexity of the movement and the height of the box with Gmed activity ranging from 18 – 59.8 % MVIC and Gmax ranging from 29 to 113 % MVIC. This is exemplified by the highest box height 45.7cm used by Simenz et al.14 resulting in the highest Gmax activity of 113 % MVIC. Compared to the step‐up exercises, the pelvic drop (standing hip abduction/adduction) exercise may be considered a simpler exercise to be taught and implemented, yet it produced high Gmed activation (mean 49.3 ± 25.6 and highest 57.6 ± 19.5 % MVIC) due to the pelvis‐on‐femur adduction and abduction control, as noted by Reiman et al.3
Though often prescribed to target the Gmed, the standing hip abduction exercise with Thera band attached to the ankle produced a high level of Gmax activation (59 % MVIC) highlighting its role as a secondary hip abductor. Three variations of the monster walk exercise required the least amount of activation for the Gmax (range 4‐6 % MVIC) while four variations of the clam shell exercise elicited the lowest amount of activation for the Gmed (ranging from 12‐18 % MVIC). Of consideration to practitioners is that during the monster walk exercise, distal band placement resulted in greater activation of Gmax and Gmed, as compared to proximal band placement.
Interpretation Limitations
The reader needs to be cognisant of a number of limitations that affect interpretation, namely that the methodological approaches varied greatly between the twenty‐three studies (see Appendix 1). For example, some studies used different exercise positions for determination of the MVIC, which could dramatically impact normalized levels of gluteal activation. This is especially important in the case of the Gmax, since Worrell et al48 showed that the level of maximal activation is highly dependent on the hip angle. Moreover, the placement of the electrodes on the Gmax and Gmed differed between some studies. All studies used surface electrodes, with the exception of Selkowitz et al58 who used indwelling electrodes. To normalize the EMG signals recorded for each muscle, different studies used different approaches e.g. root mean square of 3 trials or average EMG of 3 trials. Moreover, the EMG's signal moving window varied from 11.7 to 5000 milliseconds. Furthermore, data was extrapolated from the Figures of Cambridge et al., 53 Webster and Gribble, 59 Oliver 58 and Willcox and Buden,60 which potentially introduces measurement error. Where concentric and eccentric data was provided by Philippon et al10 and Simenz et al,14 the data was averaged and presented as such in this review. In order to accurately compare EMG activity between two studies, at the very least, their MVIC positions, electrode site placements, data processing, and amplitude presentations should be identical, and other variables such as range of motion, relative load, effort, tempo, gender, age, and training status should be similar when possible.
Several studies investigated the same exercise, however, differences in the way the exercises were performed need to be considered when analysing the findings. For example, the step up height used for lateral step up exercise ranged between 15 to 45.7cm, therefore, differing levels of EMG activation would be an expected outcome. Moreover, the thickness and therefore level of resistance for the rubber tubing / band resistance exercises is another consideration when comparing findings. Additional limitations related to this review pertain to many exercises that would meet the inclusion criteria but have yet to undergo EMG examination.
Future research should be conducted to compare a wide variety of Gmax and Gmed exercises, perhaps the exercise that top the charts in this review, under the same testing conditions (ie: MVIC position, electrode site placement, data processing, amplitude presentation), to verify that the data in this review are accurate. Finally, this review summarises information obtained from healthy subjects; therefore, vigilance is necessary when extrapolating these findings to patients with pathology.
CONCLUSION AND PRACTICAL APPLICATION
The purpose of this systematic review was to quantify the EMG activity of the Gmax and Gmed musculature during hip abduction and hip external rotation exercises. It would seem that EMG activity levels can be affected by changes in body position (WB vs. NWB) and the complexity of the exercise. EMG activity for Gmax ranged from 4 to 113 % MVIC and Gmed ranged from 12 to 103 % MVIC. Exercises with greater movement complexity, e.g. exercises such as the lateral step‐up where the body must change the angles of more than one joint while performing the action, were found to elicit greater % MVIC for both Gmax and Gmed. Exercises performed WB produced a greater % MVIC for both Gmax and Gmed compared to NWB. Although the NWB seated position was found to have the greatest activity levels, only one study assessed this position making analysis and comparison limited.
The higher EMG activation found in WB movements is explained by Reiman et al3 who suggested that when an exercise pattern imposes greater movement demands, the Gmax and Gmed are required to maintain a level pelvis position, through hip abduction, and minimize knee valgus, through hip external rotation. Hence, practitioners ought to consider trunk position in relation to the base of support, in addition to the direction of movement when applying a progressive strengthening program.3 Individuals who have difficulty performing WB exercises can benefit from using NWB side‐lying or seated exercises to strengthen the gluteal musculature. When strengthening a weaker muscle or muscle group, practitioners may wish to prescribe a gradual and progressive exercise program to ensure the targeted area is developed. This may be of importance if individuals seek and implement a compensatory movement pattern when faced with weakness or dysfunction. Individuals may benefit from being prescribed exercises that they can perform with good technique without substitution. Subsequently, once this can be achieved exercise difficulty can be progressed with more difficult exercises.
Appendix 1.
Summary of the 23 studies reviewed with EMG activation (%MVIC) values given as the mean and the standard deviation.
| Author and Date | Subjects (Sex, age, height, mass) | Methodology (MVIC position, data processing, and amplitude presentation) | Exercises | EMG Activation (%MVIC) |
|---|---|---|---|---|
| Worrell et al48 | Group 1: 13 (6 males, 7 females) 22 ± 8.6 years, 1.71 ± 0.15 m, 69.1 ± 14.1 kg Group 2: 19 (13 males, 6 females) 27.5 ± 5 years, 1.75 ± 0.09 m, 73.3 ± 15.3 kg |
Gmax : Prone hip extension against manual resistance at 0 ° of hip flexion RMS: 11.7‐millisecond moving window |
Group 1 Lateral step up (+10 % BM) Lateral step up (unloaded) Group 2 Lateral step up (+25 % BM) Lateral step up (unloaded) |
Gmax 23 ± 11 Gmax 20 ± 11 Gmax 20 ± 8 Gmax 16 ± 7 |
| Bolga and Uhl21 | 16 (8 males, 8 females) 27 ± 5 years, 1.7 ± 0.2 m, 76 ± 15 kg | Gmed: Side lying hip abduction at 25 ° against a strap RMS: 500‐millisecond moving window |
Side‐lying hip abduction Standing hip abduction Standing hip abduction (3% BM) Standing abduction (BM) with hips and knees in 20 ° of flexion Standing hip abduction (3% BM) with hip and knee in 20 ° of flexion Pelvic drop |
Gmed 42 ± 23 Gmed 33 ± 23 Gmed 42 ± 27 Gmed 28 ± 21 Gmed 46 ± 34 Gmed 57 ± 32 |
| Ayotte et al41 | 23 (16 males, 7 females) 31.2 ± 5.8 years, 1.73 ± 0.11 m, 77 ± 13.9 kg | Gmax: Supine hip extension against a fixed pad at 30 ° hip flexion Gmed: Side lying hip abduction at 25 ° against a fixed pad Average EMG of 3 trails |
Lateral step up | Gmax 56 ± 29, Gmed 18 ± 18 |
| Bolga and Uhl49 | 13 (7 males, 6 females) 24 ± 7 years, 1.6 ± 0.2 m, 78 ± 14 kg | Gmed: Side lying hip abduction at 25 ° against a strap RMS: 500‐millisecond moving window |
Side‐lying hip abduction Standing hip abduction Standing abduction with hip and knee in 20 ° of flexion Pelvic drop |
Gmed 40 ± 22 Gmed 30 ± 21 Gmed 27 ± 20 Gmed 54 ± 30 |
| Ekstorm et al50 | 30 (19 males, 11 females) 27 ± 8 years, 1.76 ± 0.8 m, 74 ± 11 kg | Gmax: Prone hip extension against manual resistance with the knee flexed at 90 ° Gmed: Side lying hip abduction to end range against manual resistance RMS: 20‐millisecond moving window |
Side‐lying hip abduction Lateral step up |
Gmax 21 ± 16, Gmed 39 ± 7 Gmax 2 9 ± 13, Gmed 43 ± 18 |
| DiStefano et al42 | 21 (9 males, 12 females) 22 ± 3 years, 1.71 ± 0.11 m, 70.4 ± 15.3 kg | Gmax: Prone hip extension against manual resistance with knee flexed at 90 ° Gmed: Side lying hip abduction at 25 ° against a strap Average EMG of 3 trials |
Side‐lying hip abduction Lateral stepping band at ankle Lateral lunge Transverse lunge Clam shell PNHIP30 Clam shell PNHIP60 |
Gmax 39 ± 18, Gmed 81 ± 2 Gmax 27 ± 16, Gmed 6 1 ± 34 Gmax 41 ± 20, Gmed 39 ± 19 Gmax 49 ± 20, Gmed 48 ± 21 Gmax 34 ± 27, Gmed 40 ± 38 Gmax 39 ± 34, Gmed 38 ± 29 |
| O’Sullivan et al25 | 16 (7 males, 8 females) 22 ± 4 years, 1.70 ± 0.1 m, 68 ± 12 kg | Gmed: the highest EMG reading from all three hip abduction movements against a fixed pad: 1) standing with the hip at 30 ° abduction 2) internal and 3) external rotation was tested prone with the hip in neutral rotation and the knee flexed at 90 °. RMS: 150‐millisecond moving window |
Pelvic drop | Gmed 29.2 ± 10.6 |
| Park et al23 | 31 (15 males, 16 females) 19.2 ± 1.44 years, 1.67 ± 0.08 m, 60.6 ± 10 kg | Gmed: Side lying hip abduction against manual resistance RMS: 5000‐millisecond moving window |
Side‐lying hip abduction Side‐lying hip abduction with pelvic belt | Gmed 26.8 ± 12.8 Gmed 35 ± 18.2 |
| Boren et al51 | 26 ( Anthropometrical details not provided) | Gmax: Prone hip extension against a strap with the knee flexed at 90 ° Gmed: Side lying hip abduction at 10 ° against a strap RMS: 50‐millisecond moving window |
Side‐lying hip abduction Side bridge with abduction DL down Side bridge with abduction DL up Lateral step up Clam shell 1 Clam shell 2 Clam shell 3 Clam shell 4 |
Gmax 51.1, Gmed 62.9 Gmax 72.8, Gmed 103 Gmax 70.9, Gmed 88.8 Gmax 63.8, Gmed 59.8 Gmax 53.1, Gmed 47.2 Gmax 12.3, Gmed 62.4 Gmax 26.6, Gmed 67.6 Gmax 26.2, Gmed 76.8 |
| Philippon et al.10 | 10 (5 males, 5 females) 28.7 ± 2.2 years, 1.72 ± 0.04 m, 67.4 ± 4.3 kg | Gmed: Standing hip abduction with external rotation against manual resistance RMS: 50‐millisecond moving window |
Clam shell Clam shell PNHIP0 Side‐lying hip abduction – internal rotation Side‐lying hip abduction – external rotation Side‐lying hip abduction against a wall |
Gmed 13.9 ± 3.6 Gmed 9.4 ± 2.75 Gmed 26.7 ± 6.7 Gmed 13 ± 4.25 Gmed 25.9 ± 5.65 |
| Bouillon et al52 | 40 (20 males, 20 females) 22 ± 1 years, 1.7 ± 0.01 m, 65 ± 13 kg | Gmax: Prone hip extension against manual resistance with the knee flexed at 90 ° Gm: Side lying hip abduction against manual resistance RMS: 300‐millisecond moving window |
Lateral lunge | Gmax 12 ± 3, Gmed 13 ± 2 |
| Cambridge et al53 | 9 males, 22 ± 2 years, 1.81 ± 0.92 m, 85.8 ± 15.4 kg | Gmax : Prone hip extension in Biering–Sorensen position against manual resistance Gmed: Side lying hip abduction against manual resistance Average EMG |
Lateral stepping band at foot Lateral stepping band at ankle Lateral stepping band at knee Monster walk band at foot Monster walk band at ankle Monster walk band at knee |
Gmax 8 ± 5, Gmed 35 ± 10 Gmax 6 ± 4, Gmed 29 ± 9 Gmax 5 ± 3, Gmed 24 ± 9 Gmax 6 ± 3, Gmed 27 ± 10 Gmax 5 ± 2, Gmed 25 ± 10 Gmax 4 ± 2, Gmed 19 ± 9 |
| McBeth et al54 | 20 (9 males, 11 females) 26.3 ± 6 years, 1.71 ± 0.06 m, 64 ± 6.8 kg | Gmax : Prone hip extension against manual resistance with the knee flexed at 90 ° Gmed: Side lying hip abduction at 35 ° against manual resistance RMS: 20‐milliseconds moving window |
Side‐lying hip abduction (5% BM) Side‐lying hip abduction – external rotation (5% BM) Clam shell (5% BM) |
Gmax 25.3 ± 24.6, Gmed 79.1 ± 29.9 Gmax 31.7 ± 24.1, Gmed 54.3 ± 24.8 Gmax 34.2 ± 24.8, Gmed 32.6 ± 16.9 |
| Simenz et al14 | 15 females, 20.8 ± 1.56 years, 1.66 ± 0.07 m, 64 ± 6.92 kg | Gmax : Prone hip extension at 70 ° hip flexion on a decline bench Gmed: Side lying hip abduction at 25 ° against fixed resistance RMS: 125‐milliseconds moving window |
Lateral step up Cross over step up | GM 113 ± 89.5,Gm 45 ± 14 GM 103 ± 63.6,Gm 57.6 ± 19.5 |
| Brandt et al.46 | 16 females, 45.7 ± 8.6 years, 1.65 ± 0.52 m, 61.8 ± 7.2 kg | Gmax: Prone hip extension against manual resistance with the knee flexed at 90 ° Gmed: Supine with hip abduction at 10 ° and pressing the knees outwards against a rigid band RMS: 500 milliseconds moving window |
Standing hip abduction band at ankle load: light (Borg ≤ 2) Standing hip abduction band at ankle load: moderate Borg ≤ 2‐ < 5) Standing hip abduction band at ankle load: heavy (Borg ≤ 5‐ < 7) Standing hip abduction band @ ankle load: near maximum (Borg ≥ 7) Seated hip abduction machine load: light (Borg ≤ 2) Seated hip abduction machine load: moderate (Borg ≤ 2‐ < 5) Seated hip abduction machine load: heavy (Borg ≤ 5‐ < 7) Seated hip abduction machine load: near maximum (Borg ≥ 7) |
Gmax 59 ± 10, Gmed 73 ± 7 Gmax 65 ± 9, Gmed 88 ± 7 Gmax 68 ± 11, Gmed 93 ± 8 Gmax 73 ± 25, Gmed101 ± 7 Gmax 67 ± 11, Gmed 53 ± 7 Gmax 65 ± 10, Gmed 61 ± 7 Gmax 69 ± 10, Gmed 67 ± 7 Gmax 70 ± 11, Gmed 80 ± 8 |
| Lee, J et al55 | 20, 22.3 ± 1.9 years, 1.69 ± 0.72 m, 66 ± 12.4 kg | Gmed: Side‐lying hip abduction against manual resistance RMS: 50 milliseconds moving window |
Side‐lying hip abduction Side‐lying hip abduction – external rotation Side‐lying hip abduction – internal rotation |
Gmed 34.2 ± 11.8 Gmed 35.3 ± 12.5 Gmed 45.3 ± 20.5 |
| Lee, K et al58 | 20 males, 22.9 ± 2.1 years, 1.74 ± 0.39 m, 70 ± 6.2 kg | Gmed: Side lying hip abduction at 25 ° against a strap RMS |
Side‐lying hip abduction Side‐lying hip abduction with pelvic belt Clam shell 1 Clam shell with pelvic belt |
Gmax 27.6 ± 19, Gmed 38 ± 21.6 Gmax 37.3 ± 24.9, Gmed 34.2 ± 15.9 Gmax 20.5 ± 18.4, Gmed 16.4 ± 11.3 Gmax 33.1 ± 23.2, Gmed 21.7 ± 12.6 |
| Oliver et al57 | 30, 23.5 ± 1.34 years, 1.74 ± 0.11 m, 76.6 ± 16.9 kg | Gmax : Prone hip extension against manual resistance with the knee flexed at 90 ° RMS: 100‐milliseconds moving window |
Shoulder dump | Gmax 28 ± 3 |
| Selkowtiz et al58 | 20 (10 males, 10 females) 27.9 ± 6.2 years | Fine Wire Electrodes EMG Gmax : Prone hip extension against a strap with the knee flexed at 90 ° Gmed: Side lying hip abduction at 30 ° against a strap RMS: 75‐milliseconds moving window |
Side‐lying hip abduction Clam shell with band at knee Lateral stepping band at knee Pelvic Drop |
Gmax 23.7 ± 15.3, Gmed 43.5 ± 14.9 Gmax 43.6 ± 26.1, Gmed 26.9 ± 18 Gmax 27.4 ± 16.4, Gmed 30.2 ± 15.7 Gmax 17.7 ± 15.2, Gmed 37.7 ± 15.1 |
| Webster and Gribble59 | 9 (1 males, 8 females) 22.9 ± 4.5 years, 1.64 ± 0.65 m, 65.4 ± 10kg | Gmax : Prone hip extension against manual resistance with the knee flexed at 90 ° Gmed: Side lying hip abduction against manual resistance Average EMG of 3 trails |
Rotation single leg squat Transverse lunge |
Gmax 78 ± 45, Gmed 68 ± 15 Gmax 58 ± 32, Gmed 68 ± 62 |
| Willcox and Buden60 | 17(10 males, 7 females) 24 ± 4 years, 1.74 ± 0.6 m, 69 ± 12kg | Gmax: Prone hip extension against manual resistance with the knee flexed at 90 ° Gmed: Side lying hip abduction against manual resistance RMS: 150‐milliseconds moving window |
Clam shell PNHIP0 Clam shell PNHIP30 Clam shell PNHIP60 Clam shell PRHIP0 Clam shell PRHIP30 Clam shell PRHIP60 |
Gmax 15, Gmed 18 Gmax 17, Gmed 22 Gmax 20, Gmed 23 Gmax 10, Gmed 12 Gmax 9, Gmed 13 Gmax 12, Gmed 18 |
| Youdas et al61 | 21 (10 males, 11 females) 25.2 ± 3.1 years, 1.8 ± 0.1 m, 82.2 ± 7.9kg | Gmax: Prone position, a pillow placed under the pelvis to provide 10 °‐15 ° of hip flexion, knee flexed at 90 °, hip extension against manual resistance Gmed: Side lying hip abduction at 30 ° against manual resistance RMS: 125‐milliseconds moving window |
Lateral stepping band at ankle Lateral stepping, hip internally rotated stance band at ankle Lateral stepping, hip externally rotated stance band at ankle |
Gmax 12.1 ± 8.4, Gmed 32.8 ± 21.9 Gmax 13 ± 9.1, Gmed 43.8 ± 27 Gmax 14.8 ± 10.7, Gmed 27.3 ± 18.1 |
| Youdas et al 45 | 26 (13 males, 13 females) 25 ± 2 years, 1.75 ± 0.6 m, 72.5 ± 10.1kg | Gmax: Prone position, a pillow placed under the pelvis to provide 10 °‐15 ° of hip flexion, knee flexed at 90 °, hip extension against manual resistance Gmed: Side lying hip abduction at 30 ° against manual resistance RMS: 125‐milliseconds moving window |
Standing hip abduction with band at ankle | Gmax 16.6 ± 10.8, Gmed 52.9 ± 17.6 |
BM = Body Mass DL = Dominant Leg Gmax = Gleteus Maximus Gmed = Gleteus Medius Clam Shell 1 = Side‐lying with hips flexed at 45 °. Externally rotate top leg Clam Shell 2 = Same as Clam 1 but internally rotate the top leg (knees together) Clam Shell 3 = Top thigh raised to parallel to table with hip in neutral rotation and 45 ° of flexion. Top leg then internally rotated. Knee height remains the same throughout the entire movement. Clam Shell 4 = Same as 3 except the top leg is in extension Clam shell PNHIP0 = pelvis neutral, hip in 0 ° of flexion Clam shell PNHIP30 = pelvis neutral, hip in 30 ° of flexion Clam shell PNHIP60 = pelvis neutral, hip in 60 ° of flexion Clam shell PRHIP0 = pelvis reclined, hip in 0 ° of flexion Clam shell PRHIP30 = pelvis reclined, hip in 30 ° of flexion Clam shell PRHIP60 = pelvis reclined, hip in 60 ° of flexion
REFERENCES
- 1.Kendall F McCrear E Provance P, et al. Muscles testing and function. 5th ed. Baltimore: Williams & Wilkin; 2005. [Google Scholar]
- 2.Nakagawa TH. Muniz TB de Marche Baldon R, et al. The effect of additional strengthening of hip abductor and lateral rotator muscles in patellofemoral pain syndrome: A randomized controlled pilot study. Clin Rehab. 2008;22:1051‐1060. [DOI] [PubMed] [Google Scholar]
- 3.Reiman MP Bolgla LA Loudon JK. A literature review of studies evaluating gluteus maximus and gluteus medius activation during rehabilitation exercises. Physio Theory & Pract. 2012;28:257‐268. [DOI] [PubMed] [Google Scholar]
- 4.Lyons K Perry J Gronley JK Barnes L Antonelli D Timing and relative intensity of hip extensor and abductor muscle action during level and stair ambulation: An EMG study. Phys Ther. 1983;63:1597‐1605. [DOI] [PubMed] [Google Scholar]
- 5.Wilson JD Ireland ML Davis I. Core strength and lower extremity alignment during single leg squats. Med & Sci in Sports & Exer. 2006;38:945. [DOI] [PubMed] [Google Scholar]
- 6.Flack NAMS Nicholson HD Woodley SJ. A review of the anatomy of the hip abductor muscles, gluteus medius, gluteus minimus, and tensor fascia lata. Clin anatomy. 2012; 25:697‐708. [DOI] [PubMed] [Google Scholar]
- 7.Conneely MO Sullivan K Edmondston S. Dissection of gluteus maximus and medius with respect to their suggested roles in pelvic and hip stability: implications for rehabilitation? Phys Ther in Sport. 2006;7:176‐178. [Google Scholar]
- 8.Blazevich AJ. Optimizing hip musculature for greater sprint running speed. J Strength Cond Res. 2000;22:22. [Google Scholar]
- 9.Schache AG Blanch PD Dorn TW, et al. Effect of running speed on lower limb joint kinetics. Med & Sci in Sports & Exerc. 2011;43:1260‐1271. [DOI] [PubMed] [Google Scholar]
- 10.Philippon MJ Decker MJ Giphart JE, et al. Rehabilitation exercise progression for the gluteus medius muscle with consideration for iliopsoas tendinitis in vivo electromyography study. Am J Sports Med. 2011;39:1777‐1785. [DOI] [PubMed] [Google Scholar]
- 11.Robertson DGE Wilson JM St. Pierre TA. Lower extremity muscle functions during full squats. J Appli Biom. 2008;24:333–339. [DOI] [PubMed] [Google Scholar]
- 12.Hollman JH Ginos BE Kozuchowsk J, et al. Relationships between knee valgus, hip‐muscle strength, and hip‐muscle recruitment during a single‐limb step‐down. J Sport Rehab. 2009:18:104–117. [DOI] [PubMed] [Google Scholar]
- 13.Hamstra‐Wright KL Blive KH. Effective exercises for targeting the gluteus medius. J Sport Rehab. 2012;21(3):296‐300. [DOI] [PubMed] [Google Scholar]
- 14.Simenz CJ Garceau LR Lutsch BN, et al. Electromyographical analysis of lower extremity muscle activation during variations of the loaded step‐up exercise. J Strength Cond Res. 2012;26:3398‐3405. [DOI] [PubMed] [Google Scholar]
- 15.Lee D. Instability of the sacroiliac joint and the consequences to gait. J Manual & Manip Ther. 1996;4:22‐29. [Google Scholar]
- 16.Presswood L Cronin J Keogh JW Whatman C. Gluteus medius: Applied anatomy, dysfunction, assessment, and progressive strengthening. Strength & Cond J. 2008;30:41‐53. [Google Scholar]
- 17.Ireland M L Willson JD Ballantyne BT Davis IM. Hip strength in females with and without patellofemoral pain. J of Orthop & Sports Phys Ther. 2003;33:671‐676. [DOI] [PubMed] [Google Scholar]
- 18.Powers CM. The influence of altered lower‐extremity kinematics on patellofemoral joint dysfunction: a theoretical perspective. J Orthop Sports Phys Ther. 2003;33:639‐646. [DOI] [PubMed] [Google Scholar]
- 19.Souza RB Powers CM. Differences in hip kinematics, muscle strength, and muscle activation between subjects with and without patellofemoral pain. J Orthop Sports Phys Ther. 2009;39:12‐19. [DOI] [PubMed] [Google Scholar]
- 20.Delp SL Hess WE Hungerford DS Jones LC. Variation of rotation moment arms with hip flexion. J Biom.1999;32:493‐501. [DOI] [PubMed] [Google Scholar]
- 21.Bolgla LA. Uhl TL. Electromyographic analysis of hip rehabilitation exercises in a group of healthy subjects. J Orthop Sports Phys Ther. 2005;35: 487‐494. [DOI] [PubMed] [Google Scholar]
- 22.Cynn HS O JS Kwon OY Yi CH. Effects of lumbar stabilization using a pressure biofeedback unit on muscle activity and lateral pelvic tilt during hip abduction in sidelying. Archives Phys Med and Rehab. 2006;87:1454‐1458. [DOI] [PubMed] [Google Scholar]
- 23.Park KM Kim SY Oh DW. Effects of the pelvic compression belt on gluteus medius, quadratus lumborum, and lumbar multifidus activities during side‐lying hip abduction. J Electromyogr Kinesiol. 2010;20:1141‐1145. [DOI] [PubMed] [Google Scholar]
- 24.Reima MP Bolgla LA Lorenz D. Hip function's influence on knee dysfunction: a proximal link to a distal problem. J Sport Rehab. 2009;18:33. [DOI] [PubMed] [Google Scholar]
- 25.O’Sullivan K Smith SM Sainsbury D. Electromyographic analysis of the three subdivisions of gluteus medius during weight‐bearing exercises. BMC Sports Sci Med and Rehab. 2010;2:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Janda V Jull GA. Muscles and motor control in low back pain: assessment and management. Physical Therapy of the Low Back. Edinburgh, Scotland: Churchill Livingston; 1987. [Google Scholar]
- 27.Page P Frank C Lardner R. Assessment and treatment of muscle mbalance: The Janda approach. Champaign: Human Kinetics; 2010. [Google Scholar]
- 28.Fairclough J Hayashi K Toumi H, et al. Is iliotibial band syndrome really a friction syndrome? J Sci & Med in Sport. 2007;10:74‐76. [DOI] [PubMed] [Google Scholar]
- 29.Noehren B Davis I Hamill J. ASB Clinical Biomechanics Award Winner 2006: Prospective study of the biomechanical factors associated with iliotibial band syndrome. Clin Biomech. 2007;22:951‐956. [DOI] [PubMed] [Google Scholar]
- 30.Friel K McLean N Myers C Caceres M. Ipsilateral hip abductor weakness after inversion ankle sprain. J Athl Train. 2006;41:74. [PMC free article] [PubMed] [Google Scholar]
- 31.Nadler SF Malanga GA DePrince M, et al. The relationship between lower extremity injury, low back pain, and hip muscle strength in male and female collegiate athletes. Clin J Sport Med. 2000;10:89‐97. [DOI] [PubMed] [Google Scholar]
- 32.Robinson RL Nee RJ. Analysis of hip strength in females seeking physical therapy treatment for unilateral patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2007;37:232‐238. [DOI] [PubMed] [Google Scholar]
- 33.Bolgla LA Malone TR Umberger BR Uhl TL. Hip strength and hip and knee kinematics during stair descent in females with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2008;38:12‐18. [DOI] [PubMed] [Google Scholar]
- 34.Widler KS Glatthorn JF Bizzini M, et al. Assessment of hip abductor muscle strength. A validity and reliability study. J Bone & Joint Surgery. 2009;91(11):2666‐2672. [DOI] [PubMed] [Google Scholar]
- 35.Hislop HJ Montgomery J. Daniels and Worthingham's muscle testing: techniques of manual examination. 7th ed, Philadelphia, PA: WB Saunders; 2002. [Google Scholar]
- 36.Fenter PC Bellew WJ Pitts TA Kay RE. Reliability of stabilised commercial dynamometers for measuring hip abduction strength: a pilot study. Br J Sports Med. 2003;37:331‐334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cahalan TD Johnson ME Liu S Chao EYS. Quantitative measurements of hip strength in different age groups. Clin Orthop & Relative Res. 1989;246: 136‐145. [PubMed] [Google Scholar]
- 38.Andersen LL Magnusson SP Nielsen M, et al. Neuromuscular activation in conventional therapeutic exercises and heavy resistance exercises: implications for rehabilitation. Phys Ther. 2006;86:683‐697. [PubMed] [Google Scholar]
- 39.Atha J. Strengthening muscle. Exerc and Sport Sci Reviews. 1981; 9:1‐4. [PubMed] [Google Scholar]
- 40.Myers JB Pasquale MR Laudner KG, et al. On‐the‐field resistance‐tubing exercises for throwers: An electromyographic analysis. J Athl Train 2005;40:15. [PMC free article] [PubMed] [Google Scholar]
- 41.Ayotte NW Stetts DM Keenan G Greenway EH. Electromyographical analysis of selected lower extremity muscles during 5 unilateral weight‐bearing exercises. J Orthop Sports Phys Ther. 2007;37:48‐55. [DOI] [PubMed] [Google Scholar]
- 42.Distefano LJ Blackburn JT Marshall SW Padua DA. Gluteal muscle activation during common therapeutic exercises. J Orthop Sports Phys Ther. 2009;39:532‐540. [DOI] [PubMed] [Google Scholar]
- 43.DiGiovine N Jobe F Pink M Perry J. An electromyographic analysis of ther pper extremity in pitching. J Shoulder Elbow Surg. 1992;1:15‐25. [DOI] [PubMed] [Google Scholar]
- 44.Escamilla RF Lewis C Bell D, et al. Core muscle activation during Swiss ball and traditional abdominal exercises. J Orthop Sports Phys Ther. 2010;40:265‐276. [DOI] [PubMed] [Google Scholar]
- 45.Youdas JW Adams KE Bertucci JE, et al. Muscle activation levels of the gluteus maximus and medius during standing hip‐joint‐strengthening exercises using elastic‐tubing resistance. J Sport Rehab. 2014;23:1‐11. [DOI] [PubMed] [Google Scholar]
- 46.Brandt M Jakobsen MD Thorborg K, et al. Perceived loading and muscle activity during hip strengthening exercises: Comparison of elastic resistance and machine exercises. Int J Sports Phys Ther. 2013;8:811. [PMC free article] [PubMed] [Google Scholar]
- 47.Moher D Liberati A Tetzlaff J Altman DG. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. Annals of internal med. 2009;151(4):264‐269. [DOI] [PubMed] [Google Scholar]
- 48.Worrell TW Karst G Adamczyk D, et al. Influence of joint position on electromyographic and torque generation during maximal voluntary isometric contractions of the hamstrings and gluteus maximus muscles. J Orthop Sports Phys Ther. 2001;31:730‐740. [DOI] [PubMed] [Google Scholar]
- 49.Bolgla LA Uhl TL. Reliability of electromyographic normalization methods for evaluating the hip musculature. J Electromyogra Kinesiol. 2007;17:102‐111. [DOI] [PubMed] [Google Scholar]
- 50.Ekstrom RA Donatelli RA Carp KC. Electromyographic analysis of core trunk, hip, and thigh muscles during 9 rehabilitation exercises. J Orthop Sports Phys Ther. 2007;37:754‐762. [DOI] [PubMed] [Google Scholar]
- 51.Boren K Conrey C Le Coguic J, et al. Electromyographic analysis of gluteus medius and gluteus maximus during rehabilitation exercises. Int J Sports Phys Ther. 2011;6:206. [PMC free article] [PubMed] [Google Scholar]
- 52.Bouillon LE Wilhelm J Eisel P, et al. Electromyographic assessment of muscle activity between genders during unilateral weight‐bearing tasks using adjusted distances. Int J Sports Phys Ther. 2012;7:595. [PMC free article] [PubMed] [Google Scholar]
- 53.Cambridge ED Sidorkewicz N Ikeda DM McGill SM. Progressive hip rehabilitation: the effects of resistance band placement on gluteal activation during two common exercises. Clin Biomech. 2012;27:719‐724. [DOI] [PubMed] [Google Scholar]
- 54.McBeth JM Earl‐Boehm JE Cobb SC Huddleston WE. Hip muscle activity during 3 side‐lying hip‐strengthening exercises in distance runners. J Athl Train. 2012;47:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lee JH Cynn HS Choi SA, et al. Effects of different hip rotations on gluteus medius and tensor fasciae latae muscle activity during isometric side‐lying hip abduction. J Sport Rehab. 2013;22. [DOI] [PubMed] [Google Scholar]
- 56.Lee KS Ko E Lim CG. Effect of pelvic belt on gluteal muscles activity during therapeutic exercise. J of Phys Ther Sci. 2013;25:337‐340. [Google Scholar]
- 57.Oliver GD Sola M Dougherty C Huddleston S. Quantitative examination of upper and lower extremity muscle activation during common shoulder rehabilitation exercises using the Bodyblade. J Strength Cond Res. 2013;27(9):2509‐2517. [DOI] [PubMed] [Google Scholar]
- 58.Selkowitz DM Beneck GJ Powers CM. Which exercises target the gluteal muscles while minimizing activation of the tensor fascia lataϿ. Electromyographic assessment using fine‐wire electrodes. J Orthop Sports Phys Ther. 2013;43(2):54‐64. [DOI] [PubMed] [Google Scholar]
- 59.Webster KA Gribble PA. A comparison of electromyography of gluteus medius and maximus in subjects with and without chronic ankle instability during two functional exercises. Phys Ther in Sport. 2013;14(1):17‐22. [DOI] [PubMed] [Google Scholar]
- 60.Willcox EL Burden AM. The influence of varying hip angle and pelvis position on muscle recruitment patterns of the hip abductor muscles during the clam exercise. J Orthop Sports Phys Ther. 2013;43(5):325‐331. [DOI] [PubMed] [Google Scholar]
- 61.Youdas JW Foley BW Kruger BL, et al. Electromyographic analysis of trunk and hip muscles during resisted lateral band walking. Phys Theory & Practice. 2013;29: 113‐123. [DOI] [PubMed] [Google Scholar]