Abstract
Purpose/Background
Sprinting and jumping are two common and important components of high‐level sport performance. The weight‐bearing dorsiflexion test (WB‐DF) and Star Excursion Balance Test (SEBT) are tools developed to identify athletes at risk for lower extremity injury and may be related to running and jumping performance among athletes. The purposes of the present study were: 1) to identify any relationships between functional movement tests (WB‐DF and SEBT) and performance tests (jumping, sprinting and changing direction); 2) to examine any relationships between asymmetries in functional movements and performance tests.
Study Design
Descriptive cohort study.
Methods
Fifteen elite male basketball players (age: 15.4 ± 0.9 years) were assessed during a three‐week period to determine the reliability of functional screening tools and performance tests and to examine the relationships between these tests. Relative (intraclass correlation coefficient) and absolute (coefficient of variation) reliability were used to assess the reproducibility of the tests.
Results
Significant correlations were detected between certain functional movement tests and performance tests. Both left and right excursion composite scores related to slower performance times in sprint testing, demonstrating that greater dynamic reach relates to decreased quickness and acceleration among these elite basketball athletes. The various relationships between dynamic functional movement testing, speed, and jump performance provide guidance for the strength and conditioning professional when conducting and evaluating data in an effort to improve performance and reduce risk of injury.
Conclusions
The results of the present study suggest that these functional and performance tests do not measure the same components of human movement, and could be paired as outcome measures for the clinical and sport assessment of lower extremity function.
Level of Evidence
2b
Keywords: Vertical jump, sprinting speed, sports performance, functional testing
INTRODUCTION
Sprinting and various jumps are amongst the most widely used performance movements to assess lower limb performance.1 In this regard, bilateral and unilateral jumps (i.e., vertical and horizontal) have been included within team‐sports assessments due to the fact that they are quite similar to specific movements in such sports and have been shown to be reliable measurements.2,3 Interestingly, these unilateral jumps have a high ability to discriminate between the performance of the injured (i.e., anterior cruciate ligament [ACL]) and uninjured side among patients with injury to the ACL.2 Such testing may also be used in the decision‐making process for return to sport following injury.4 Furthermore, both jumps can predict both change of direction (COD) and sprinting performance.3,5,6 Thus, it seems that unilateral assessment is of interest for strength and conditioning coaches and sports medicine professionals alike.
The weight‐bearing dorsiflexion test (WB‐DF) is a functional screening tool developed to assess dorsiflexion range of motion (ROM).7 Backman et al8 have shown that a low WB‐DF value is a risk factor for developing patellar tendinopathy in junior elite basketball players because of load‐bearing compensation in the patellar tendon. Moreover, WB‐DF was a predictor of dynamic balance in healthy adults and individuals with chronic ankle instability.9 Impaired ankle dorsiflexion ROM during a squat can result in increased knee valgus and medial knee displacement, as well as decreased quadriceps activation and increased soleus activation.10
The Star Excursion Balance Test (SEBT) is another functional screening tool developed to assess lower extremity dynamic stability,11 for monitoring the rehabilitation process,12, 13 and to identify athletes at high risk for lower extremity injury.14 Plisky et al15 found the SEBT to be a good predictor of lower extremity injury in high school basketball players. The SEBT requires neuromuscular characteristics such as coordination, strength, and flexibility,16 thus, the SEBT has been used to assess dynamic postural control.16 According to Filipa et al,17 the SEBT may be a useful test to assess the efficacy of training programs designed to decrease injury risk. The SEBT reach distance has been correlated with hip ROM.18 Endo et al18 demonstrated that the direction from posterolateral to posteromedial motion of the SEBT was positively correlated with hip internal rotator and hamstring tightness, while negatively correlated with gastrocnemius tightness in junior high school baseball players. The direction from medial to lateral of the SEBT was negatively correlated with iliopsoas and gastrocnemius tightness. Anterior SEBT scores were fairly positively correlated with hip flexor and extensor strength. Posterolateral SEBT scores were fairly positively correlated with hip abductor, extensor, and flexor strength in collegiate female athletes.19 Recently, Lockie el al20 found a significant relationship between dynamic stability, as measured by functional reaching, and multidirectional speed in field sport athletes (e.g. soccer, rugby league, rugby, Australian football).
Despite the aforementioned data, little is known about the relationship between functional screening tools for lower body and jump and/or sprint performance in elite male basketball players. Therefore, the purposes of the present study were: 1) to identify any relationships between functional movement tests and performance tests; and 2) to examine any relationships between asymmetries in functional movements and performance tests, in elite male basketball players.
METHODS
Subjects
Fifteen elite male basketball players (age: 15.4 ± 0.9 years; height: 187.9 ± 8.0 cm; body mass: 73.1 ± 10.6 kg) volunteered to participate in the present study. Their maturational status was assessed through age at peak height velocity (APHV: 2.3 ± 0.9 cm/year).21 Data collection took place during the second month of the competitive season after a two‐month pre‐season period. Players belonged to a first Spanish basketball division (ACB‐Liga Endesa) club academy squad. All players participated an average of 12 hours of combined basketball (6‐7 sessions), strength/power (2 sessions) and speed, agility and quickness (SAQ) (1 session) training sessions plus two competitive matches per week. At the time of the study, all players were competing at the national level (i.e., Spanish National Basketball League). Furthermore, some players (n=6) were also competing at the international level (i.e., European and World Basketball Championships). Written informed consent was obtained from both the players and their parents before beginning the investigation. The present study was approved by the institutional research ethics committee, and conformed to the recommendations of the Declaration of Helsinki.
Protocol
Highly trained, young male basketball players were assessed during a three‐week period to determine the reliability of functional screening tools and performance tests and to examine the relationships between these tests. The experimental schedule consisted of three consecutive testing sessions: first (Monday), players carried out the injury prevention tests (i.e., WB‐DF and SEBT), and second (Wednesday), a battery of jump tests (bilateral vertical jump, and unilateral vertical and horizontal jump) were executed. Finally (Friday), linear sprint and COD tests were performed. This schedule was repeated three times (once per week over a three week period). Relative (intraclass correlation coefficient [ICC]) and absolute (coefficient of variation [CV]) reliability values were used to assess the reproducibility of the tests. The first week testing sessions were considered as familiarization sessions; therefore the ICC and CV of the tests were established through the results obtained during the second and third week. All tests were performed indoors on a basketball court. The leg motion ankle dorsiflexion test was preceded by two warm‐up attempts with the third attempt recorded. The SEBT test was preceded by four warm‐up attempts with the left leg (i.e., leg stance) and four with the right leg. Later, three consecutive trials were recorded with the same leg. With regard to performance tests, players performed a 15‐min standardized warm‐up, which included jogging (4 min), calisthenics (3 min), and accelerations (4 × 15 m). Additionally, prior to the commencement of jump tests, three maximal jumps were executed. Prior to performing the sprint and COD tests a specific warm‐up comprised of two sub‐maximal efforts and one maximal effort was performed. Three minutes of recovery were allotted between finishing the specific warm‐up (performance tests) and the beginning of every test. During unilateral tests (i.e., WB‐DF, SEBT, unilateral jumps and COD), the left leg was evaluated first. In every session, trials were performed at the same time of the day (18:00 to 20:00) under the same environmental conditions (20° to 22°). Prior to each testing session, players were informed not to take any stimulant (e.g., caffeine), not to eat within three hours prior to testing, to maintain their nutritional habits the two days prior to the test, and to avoid any vigorous exercise 24 hours before the testing session.
Functional movement tests
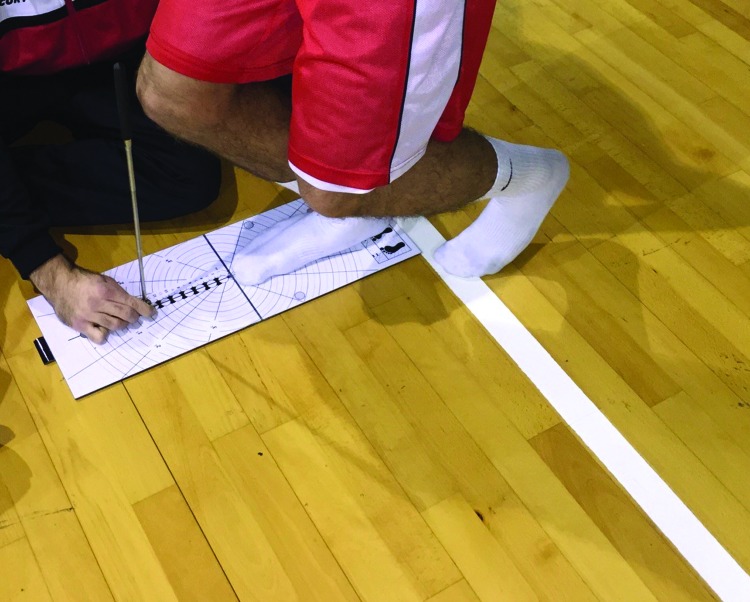
Weight‐bearing dorsiflexion test
Ankle dorsiflexion was evaluated through the LegMotion system (LegMotion, Check your MOtion, Albacete, Spain) (Figure 1).22 Each player started with their hands on their hips, and put the assigned foot on the middle of the longitudinal line just behind the transversal line on the platform. The alternate foot was positioned out of the platform with toes at the edge of the platform. While maintaining this position, subjects were instructed to perform a lunge in which the knee was flexed with the goal of making contact between the anterior knee and the metal stick. When subject were able to maintain heel and knee contact, the metal stick was progressed away from knee. The distance achieved was recorded in centimeters. Three trials were allowed with each ankle (i.e., left and right) with 10 seconds of passive recovery between trials. The third value in each ankle was selected for subsequent analysis of weight‐bearing dorsiflexion (WB‐DF).
Figure 1.
Weight bearing dorsiflexion test, conducted using the LegMotion system (LegMotion, Check your Motion, Albacete, Spain)
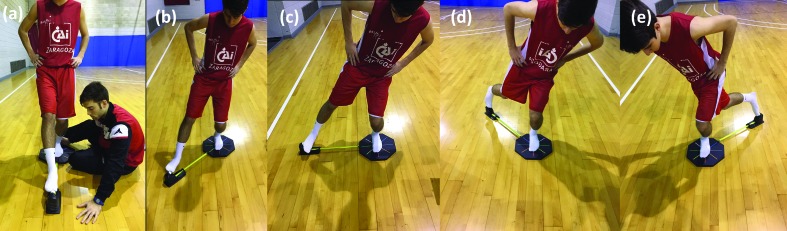
Modified Star Excursion Balance Test
Dynamic balance was assessed by using the OctoBalance device (OctoBalance, Check your MOtion, Albacete, Spain) (Figure 2), a modified version of the SEBT, which analyzed five lower limb excursion directions: anterior (SEBT‐A), anteromedial (SEBT ‐AM), medial (SEBT‐M), posteromedial (SEBT‐PM) and posterolateral (SEBT‐PL). The measurement system is based on an extending measuring tape, which is magnetized in each direction to an octagon‐shaped platform. Each trial consisted of pushing the marked point, situated at the top of the measuring tape, with the toes (i.e, big toe with the exception of the medial direction where the head of the 5th metatarsal was used) as far as possible in the designated direction. Prior to the commencement of each trial, the measuring tape was established at 30 cm, meaning it was placed at a minimum distance of 30 cm to start the excursion. Each trial was validated by a visual inspection to ensure that each trial was performed without putting the toes on the marked point, and to ensure that their heel remained on the anterior‐posterior line on the platform (the whole foot must be on the platform and with the heel on the border line of the octagon). Players were instructed to maintain their hands on their hips throughout the test. Warm‐up was followed by four trials with each leg (i.e., left stance and right stance). Three trials were allowed with each leg with 10 seconds of passive recovery between trials. The mean result of the three trials in each leg was utilized for subsequent analysis.
Figure 2.
Dynamic balance assessment using the modified version of the Star Excursion Balance Test using the OctoBalance device (OctoBalance, Check your Motion, Albacete, Spain)
Performance tests
Bilateral countermovement jump (CMJ) test
Lower limb bilateral explosive power was assessed using a vertical countermovement jump (CMJ) (reported in centimeters) with flight time measured by the Optojump (Optojump, Microgate, Bolzano, Italy) to calculate jump height. Each trial was validated by a visual inspection to ensure that each landing was without any leg flexion, and players were instructed to maintain their hands on their hips during CMJ. The depth of the CMJ was self‐selected. Each test was performed three times, separated by 45 seconds of passive recovery, and the best jump was recorded and used for analysis. During CMJ, subjects wore athletic shoes.
Unilateral countermovement jump (CMJ) test
Each subject started by standing solely on the designated leg, maintaining their hands on their hips during unilateral CMJ and the alternate leg flexed to 90° at the hip and knee. Players were asked to jump as high as possible and to land on the assessed leg (Optojump, Microgate, Bolzano, Italy). Leg swing of the alternate leg was not allowed. Failure to maintain proper technique resulted in an invalid jump (i.e., hands on hips, 90° flexion and leg swing). Each test was performed twice, separated by 45 seconds of passive recovery, and the best jump was recorded and used for analysis. The variables used for analyses were: 1‐legged left CMJ (CMJL) and 1‐legged right CMJ (CMJR). During CMJ, subjects wore athletic shoes.
Unilateral horizontal jump (HJ) test
Unilateral horizontal jump test was measured using a standard measuring tape. Each subject standing with the toes of the designated leg positioned just behind a starting line (marked with tape), hands placed behind the back and the alternate leg flexed to 90° at the hip and knee. When ready, each subject flexed then rapidly extended the assessed leg, jumping as far as possible (forward distance), and landing on both feet simultaneously. The point of the shoe closest to the starting line upon landing was used to determine the distance jumped. Leg swing of the alternate leg was not allowed. Failure to maintain proper technique resulted in an invalid jump (i.e., hands behind back, 90° flexion and leg swing). Each test (left and right) was performed twice, separated by at least 45 seconds of passive recovery, and the best jump was recorded and used for analysis. The variables used in analyses were: 1‐legged left HJ (HJL) and 1‐legged right HJ (HJR). During HJ, subjects wore athletic shoes.
Speed tests
Running speed was evaluated by 25‐m sprint times (standing start) with 5‐m, 10‐m and 20‐m split times. The front foot was placed 0.5 m before the first timing gate. Time was recorded with photoelectric cells (Witty, Microgate, Bolzano, Italy). The 25‐m sprint was performed twice, separated by at least three minutes of passive recovery. The best time was recorded for analysis.
180° Change of direction test
A 10‐m sprint test was performed. The front foot was placed 0.5 m before the first timing gate (Witty, Microgate, Bolzano, Italy). Each player sprinted from the start/finish line, completely crossed the 5‐m line with either right or left foot, and turned 180° to sprint back to the start/finish line. Players executed two valid trials with each foot, separated by at least two minutes, with the fastest retained for analysis. The variables used in analyses were COD 180° with left (COD180L) and right leg (COD180R).
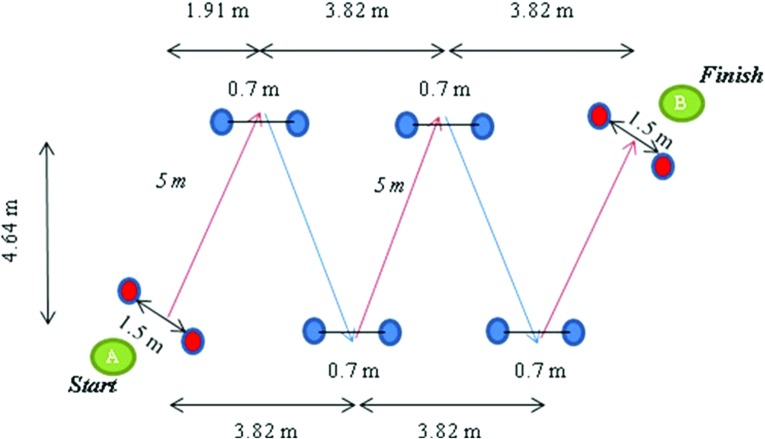
V‐cut test
In the V‐cut test, players performed a 25‐m sprint with four CODs of 45° 5 m each.. The front foot was placed 0.5 m before the first timing gate (Witty, Microgate, Bolzano, Italy). There were marks on the floor and cones, so subjects knew when to change of direction. For the trial to be valid, players had to pass the line, placed on the floor, with one foot completely at every turn. If the trail was considered a failed attempt, a new trial was allowed. The distance between each pair of cones was 0.7 m. Players performed two trials separated by at least three min. Time in the fastest trial was recorded (Figure 3).
Figure 3.
The V‐cut test, performed over 25 meters, with four changes of direction, measured using a timing gate (Witty, Microgate, Bolzano, Italy)
Data analysis
Data are presented as mean ± SD. The distribution of each variable was examined with the Shapiro‐Wilk normality test. Relative reliability analysis was examined by the intraclass correlation coefficients (ICC). An ICC equal at or above 0.70 was considered acceptable for clinical use.23,24 To examine absolute reliability pairwise comparisons were first applied with paired t‐test to assess any significant differences between the sessions. The magnitude of between‐session differences was also expressed as standardized mean difference (Cohen effect sizes, ES). The criteria to interpret the magnitude of the ES were as follows: < 0.2 trivial, > 0.2 to 0.6 small, > 0.6 to 1.2 moderate, > 1.2 large.25 The spreadsheet of Hopkins26 was also used to determine the change in the mean between trials and the typical error of measurement (TEM), expressed as a CV (%). A CV of less than 5% was set as the criterion for reliability. Relationships between variables were determined using Pearson´s correlations. A symmetry between legs was calculated using the following formula27:
The significance level was set at p ≤ 0.05. Data were analyzed using PASW/SPSS Statistics 20.0 (SPSS Inc, Chicago, IL, USA).
RESULTS
Descriptive data
Descriptive values for functional movement tests and performance tests are reported in Table 1.
Table 1.
Descriptive values for functional movement tests and performance tests (n = 15)
| Mean | SD | ||
|---|---|---|---|
| Functional movement tests | |||
| WB‐DFR (cm) | 11.5 | 2.9 | |
| WB‐DFL (cm) | 10.4 | 4.1 | |
| SEBT‐AR (cm) | 58.9 | 3.9 | |
| SEBT‐AL (cm) | 58.9 | 4.8 | |
| SEBT‐AMR (cm) | 65.3 | 4.1 | |
| SEBT‐AML (cm) | 63.8 | 4.5 | |
| SEBT‐MR (cm) | 64.0 | 6.8 | |
| SEBT‐ML (cm) | 64.7 | 6.1 | |
| SEBT‐PMR (cm) | 83.0 | 7.5 | |
| SEBT‐PML (cm) | 81.2 | 6.3 | |
| SEBT‐PLR (cm) | 78.8 | 7.4 | |
| SEBT‐PLL (cm) | 76.7 | 7.9 | |
| SEBT‐CompositeR (cm) | 71.5 | 4.7 | |
| SEBT‐CompositeL (cm) | 70.2 | 4.9 | |
| Performance tests | |||
| CMJ (cm) | 34.5 | 4.1 | |
| CMJR (cm) | 13.7 | 2.5 | |
| CMJL (cm) | 13.5 | 2.3 | |
| HJR (cm) | 149.2 | 9.2 | |
| HJL (cm) | 149.5 | 10.2 | |
| 5‐m (s) | 1.1 | 0.1 | |
| 10‐m (s) | 1.8 | 0.1 | |
| 20‐m (s) | 3.2 | 0.1 | |
| 25‐m (s) | 3.8 | 0.1 | |
| COD180R (s) | 2.6 | 0.1 | |
| COD180L (s) | 2.7 | 0.1 | |
| V‐cut (s) | 7.0 | 0.3 |
R: Right; L: Left; WB‐DF: weight‐bearing dorsiflexion; SEBT‐A: anterior direction, SEBT‐AM: anteromedial direction, SEBT‐M: medial direction, SEBT‐PM: posteromedial direction, and SEBT‐PL: posterolateral direction; SEBT‐Composite: composite; CMJ: countermovement jump; CMJR: one‐legged vertical jump; HJ: one‐legged horizontal jump; COD180R: 5 + 5 m sprint test with a 180° change of direction; V‐cut: 25‐m sprint test with 4 × 45° changes of direction.
Functional movement tests and performance tests reliability
There were no significant differences (p ≥ 0.05) between Trials 2 and 3 in any variable and between‐trial differences (ESs) were all trivial with the exception of the anterior left line (p = 0.028; ES=0.2), anterior right line (p = 0.001; ES=0.36) and medial left line (p < 0.001; ES=0.33). All the other measures of reliability of functional movement tests are presented in Table 2. There were no significant differences (p ≥ 0.05) between Trials 2 and 3 in any variable. Between‐trial ESs were all trivial (ES<0.2), all the other measures of reliability of performance tests are presented in Table 3.
Table 2.
Measures of reliability in functional movement tests (n = 15).
| ICC (90%CL) | CV (90%CL) | |
|---|---|---|
| WB‐DFR (cm) | 0.97 (0.93; 0.99) | 6.6 (5.0; 11.8) |
| WB‐DFL (cm) | 0.99 (0.97; 1.00) | 7.9 (6.0; 11.7) |
| SEBT‐AR (cm) | 0.94 (0.87; 0.98) | 2.1 (1.6; 3.1) |
| SEBT‐AL (cm) | 0.94 (0.86; 0.98) | 3.0 (2.3; 4.4) |
| SEBT‐AMR (cm) | 0.85 (0.66; 0.94) | 3.1 (2.4; 4.6) |
| SEBT‐AML (cm) | 0.91 (0.79; 0.96) | 3.0 (2.3; 4.4) |
| SEBT‐MR (cm) | 0.94 (0.85; 0.97) | 3.3 (2.5; 4.8) |
| SEBT‐ML (cm) | 0.97 (0.94; 0.99) | 2.1 (1.6; 3.0) |
| SEBT‐PMR (cm) | 0.93 (0.84; 0.97) | 2.2 (1.7; 3.3) |
| SEBT‐PML (cm) | 0.94 (0.86; 0.98) | 2.4 (1.9; 3.6) |
| SEBT‐PLR (cm) | 0.97 (0.92; 0.99) | 2.3 (1.8; 3.4) |
| SEBT‐PLL (cm) | 0.97 (0.93; 0.99) | 2.5 (1.9; 3.7) |
ICC: intraclass correlation coefficient; CL: confidence limits; CV: coefficient of variation. R: Right; L: Left; WB‐DF: weight‐bearing dorsiflexion; SEBT‐A: anterior direction, SEBT‐AM: anteromedial direction, SEBT‐M: medial direction, SEBT‐PM: posteromedial direction, and SEBT‐PL: posterolateral direction; SEBT‐Composite: composite of all directions.
Table 3.
Measure of reliability in performance tests (n = 15).
| ICC (CL90%) | CV (CL90%) | |
|---|---|---|
| CMJ (cm) | 0.94 (0.80; 0.99) | 3.3 (0.80; 0.99) |
| CMJR (cm) | 0.96 (0.93; 0.98) | 4.2 (3.5; 9.3) |
| CMJL (cm) | 0.91 (0.85; 0.95) | 4.8 (4.2; 5.6) |
| HJR (cm) | 0.86 (0.77; 0.92) | 3.8 (3.2; 4.8) |
| HJL (cm) | 0.86 (0.77; 0.92) | 3.7 (3.1; 4.6) |
| 5‐m (s) | 0.73 (0.55; 0.84) | 2.9 (2.4; 3.7) |
| 10‐m (s) | 0.73 (0.54; 0.85) | 2.8 (2.3; 3.6) |
| 20‐m (s) | 0.84 (0.71; 0.91) | 1.8 (1.5; 2.3) |
| 25‐m (s) | 0.88 (0.77; 0.93) | 1.6 (1.3; 2.0) |
| COD180R (s) | 0.85 (0.75; 0.92) | 1.7 (1.4; 2.1) |
| COD180L (s) | 0.78 (0.62; 0.87) | 2.1 (1.8; 2.7) |
| V‐cut (s) | 0.92 (0.87; 0.95) | 1.4 (1.2; 1.7) |
ICC: intraclass correlation coefficient; CL: confidence limits; CV: coefficient of variation; CMJ: countermovement jump; CMJR: one‐legged vertical right jump; CMJL: one‐legged vertical left jump; HJR: one‐legged horizontal right jump; HJL: one‐legged horizontal left jump; COD180R: 5 + 5 m sprint test with a 180° change of direction with right leg; COD180L: 5 + 5 m sprint test with a 180° change of direction with right leg; V‐cut: 25‐m sprint test with 4 x 45° changes of direction.
Correlations
The correlations between the functional movement tests and performance tests are reported in Table 4, a moderate, negative relationship was found between SEBT‐composite and speed tests (0‐5m) (r=‐0.59; p<0.05). The correlations between functional movement and performance asymmetries are reported in Table 5, a moderate, negative relationship was found between WB‐DF asymmetry and COD tests (r=‐0.52; p<0.05).
Table 4.
Correlations between functional movement and performance tests (n = 15).
| CMJR | HJR | 0‐5m | 0‐10m | 0‐20m | 0‐25m | COD180R | V_cut | ||
|---|---|---|---|---|---|---|---|---|---|
| WB‐DFR | Pearson | 0.265 | 0.333 | 0.335 | 0.095 | 0.050 | −0.049 | 0.125 | 0.067 |
| P | 0.340 | 0.225 | 0.222 | 0.736 | 0.858 | 0.862 | 0.657 | 0.820 | |
| SEBT‐AR | Pearson | −0.381 | −0.266 | 0.560* | 0.392 | 0.388 | 0.242 | 0.205 | 0.250 |
| P | .0162 | 0.339 | 0.030 | 0.149 | 0.153 | 0.385 | 0.463 | 0.388 | |
| SEBT‐AMR | Pearson | −0.395 | −0.188 | 0.680** | 0.551* | 0.532* | 0.406 | 0.117 | 0.239 |
| P | 0.145 | 0.503 | 0.005 | 0.033 | 0.041 | 0.133 | 0.678 | 0.410 | |
| SEBT‐MR | Pearson | 0.022 | 0.173 | 0.535* | 0.362 | 0.352 | 0.293 | 0.257 | 0.337 |
| P | 0.939 | 0.538 | 0.040 | .185 | 0.198 | 0.290 | 0.355 | 0.239 | |
| SEBT‐PMR | Pearson | 0.126 | −0.021 | 0.484 | 0.560* | 0.443 | 0.398 | 0.265 | 0.311 |
| P | 0.654 | 0.940 | 0.068 | 0.030 | 0.098 | 0.142 | 0.339 | 0.279 | |
| SEBT‐PLR | Pearson | 0.265 | 0.344 | 0.318 | 0.227 | 0.150 | 0.080 | 0.038 | 0.126 |
| P | 0.340 | 0.210 | 0.247 | 0.416 | 0.593 | 0.777 | 0.893 | 0.669 | |
| SEBT‐CompositeR | Pearson | −0.010 | 0.032 | 0.584* | 0.516* | 0.434 | 0.330 | 0.189 | 0.278 |
| P | 0.972 | 0.910 | 0.022 | 0.049 | 0.106 | 0.230 | 0.499 | 0.336 | |
| CMJL | HJL | 0‐5m | 0‐10m | 0‐20m | 0‐25m | COD180L | V_cut | ||
|---|---|---|---|---|---|---|---|---|---|
| WB‐DFL | Pearson | −0.018 | 0.192 | 0.488 | 0.293 | 0.243 | 0.18 | 0.335 | 0.373 |
| P | 0.949 | 0.493 | 0.065 | 0.29 | 0.384 | 0.52 | 0.222 | 0.189 | |
| SEBT‐AL | Pearson | −0.486 | −0.03 | 0.560* | 0.302 | 0.325 | 0.225 | 0.633* | 0.485 |
| P | 0.067 | 0.914 | 0.03 | 0.275 | 0.238 | 0.42 | 0.011 | 0.079 | |
| SEBT‐AML | Pearson | −0.299 | 0.101 | 0.650** | 0.457 | 0.405 | 0.287 | 0.472 | 0.483 |
| P | 0.279 | 0.72 | 0.009 | 0.087 | 0.134 | 0.299 | 0.076 | 0.08 | |
| SEBT‐ML | Pearson | −0.294 | 0.136 | 0.563* | 0.316 | 0.312 | 0.268 | 0.493 | 0.552* |
| P | 0.287 | 0.628 | 0.029 | 0.252 | 0.257 | 0.334 | 0.062 | 0.041 | |
| SEBT‐PML | Pearson | −0.012 | 0.229 | 0.506 | 0.396 | 0.287 | 0.234 | 0.224 | 0.415 |
| P | 0.966 | 0.411 | 0.054 | 0.144 | 0.299 | 0.401 | 0.421 | 0.14 | |
| SEBT‐PLL | Pearson | 0.16 | 0.356 | 0.363 | 0.203 | 0.109 | 0.057 | 0.099 | 0.256 |
| P | 0.569 | 0.193 | 0.183 | 0.469 | 0.698 | 0.84 | 0.726 | 0.377 | |
| SEBT‐CompositeL | Pearson | −0.127 | 0.234 | 0.597* | 0.388 | 0.31 | 0.22 | 0.376 | 0.461 |
| P | 0.652 | 0.402 | 0.019 | 0.152 | 0.261 | 0.431 | 0.167 | 0.097 |
R: Right; L: Left; WB‐DF: weight‐bearing dorsiflexion; SEBT‐A: anterior direction, SEBT‐AM: anteromedial direction, SEBT‐M: medial direction, SEBT‐PM: posteromedial direction, and SEBT‐PL: posterolateral direction; SEBT‐Composite: composite of all directions; CMJR: one‐legged vertical right jump; CMJL: one‐legged vertical left jump; HJR: one‐legged horizontal right jump; HJL: one‐legged horizontal left jump; COD180R: 5 + 5 m sprint test with a 180° change of direction with right leg; COD180L: 5 + 5 m sprint test with a 180° change of direction with right leg; V‐cut: 25‐m sprint test with 4 x 45° changes of direction.
p < 0.05;
p < 0.01.
Table 5.
Correlations between functional movement and performance asymmetries (n = 15).
| CMJ_% asymm | HJ_% asymm | COD180_% asymm | ||
|---|---|---|---|---|
| WB‐DF % asymm | Pearson | −0.490 | −0.051 | ‐.523* |
| P | 0.064 | 0.856 | 0.045 | |
| SEBT‐A_% asymm | Pearson | ‐0.520* | −0.22 | 0.08 |
| P | 0.047 | 0.426 | 0.787 | |
| SEBT‐AM_% asymm | Pearson | ‐0.773** | −0.18 | −0.19 |
| P | 0.001 | 0.532 | 0.505 | |
| SEBT‐M_% asymm | Pearson | −0.142 | −0.037 | 0.320 |
| P | 0.613 | 0.896 | 0.245 | |
| SEBT‐PM_% asymm | Pearson | −0.422 | 0.080 | 0.347 |
| P | 0.117 | 0.778 | 0.205 | |
| SEBT‐PL_% asymm | Pearson | −0.280 | 0.023 | 0.052 |
| P | 0.312 | 0.934 | 0.855 | |
| SEBT‐Composite_% asymm | Pearson | ‐0.583* | −0.056 | 0.141 |
| P | 0.023 | 0.842 | 0.616 |
Asymm: asymmetry; CMJ: countermovement jump; HJ: horizontal jump; COD180: 5 + 5 m sprint with a 180 change of direction; WB‐DF: weight‐bearing dorsiflexion; SEBT‐A: anterior direction, SEBT‐AM: anteromedial direction, SEBT‐M: medial direction, SEBT‐PM: posteromedial direction, and SEBT‐PL: posterolateral direction; SEBT‐Composite: composite of all directions.
= significant at p < 0.05;
= significant at p < 0.01.
DISCUSSION
The primary finding of the present study is that significant correlations were detected between modified star excursion balance test and speed test. Moreover, this study provides evidence that significant correlations were observed between functional movement and performance asymmetries. Overmoyer and Reiser11 suggested that asymmetries and functional movement impairments are most likely to be expressed in multiple tasks and that tests most relevant to the sport should be employed in evaluation. Understanding these relationships and asymmetries can aid in proper evaluation and intervention among basketball players with functional asymmetries and performance limitations.
The WB‐DF measures did not show any significant correlations to performance tests until asymmetries were evaluated. No relationship was found with CMJ or HJ; however, a moderate, negative relationship was found between WB‐DF asymmetry and COD tests (r=‐0.52). Thus, asymmetries in weight bearing dorsiflexion related to a reduction in COD performance, a factor of great importance to elite basketball performance. Dorsiflexion of the ankle is important in multi‐directional running tasks in order to facilitate ground clearance and preparation for foot impact.20,28 Therefore, limited performance on the WB‐DF test would suggest potential movement impairment that could alter movement mechanics in multi‐directional running tasks.
SEBT data demonstrated various moderate, significant relationships to performance measures, primarily in 0‐5m, 0‐10m, and 0‐20m sprint times. Both left and right excursion scores during SEBT related to slower performance times during sprint test, demonstrating that greater dynamic reach relates to decreased quickness and acceleration among these elite basketball athletes. One kinematic factor that influences sprinting speed is the large ROM at the hip.20 Greater reach in the SEBT tasks suggests a possibility of greater range of motion at the hip, which might foster faster sprint performance. In addition, activation of muscles surrounding the hip, including the biceps femoris and hamstrings, may be required for performance of the SEBT reaches and sprinting performance.29‐31 However, the current data suggest the opposite to be occurring. Greater reaches are related to slower run times (poor performance). Pruyn et al.32 demonstrated that higher levels lower‐body stiffness possibly advantageous when performing rapid, ballistic movements like running and jumping. It was suggested that increased stiffness may enhance the ability to store and release elastic energy during stretch‐shortening cycle movements. The current data seem to support that theory as sprint times were slower in those athletes with greater lower‐body ROM. There may, in fact, be an optimal amount of flexibility that fosters higher levels of sprinting performance with too much or too little ROM inhibiting performance.
Left anterior excursion measures showed a significant, moderate relationship to COD180 (r=0.63) scores while left medial excursion showed a correlation to the V‐cut test (r=0.55). Lockie et al.20 conducted a similar study with field sport athletes and found that longer reach distances in excursion tests were related to COD tasks such as the T‐test. However, they did not find significant correlations between excursion tests and short distance speed tests (10m and 20m) but did find moderate correlations to 40m sprint speed. The difference between these findings may be the athletes used in each study. Basketball players, confined to a smaller court area as compared to larger field sports such as soccer, rugby, and lacrosse, may differ in their performance in shorter, acceleration‐type testing thus creating possible differences in correlations to dynamic reach.
The negative relationship between CMJ and asymmetries in SEBT‐A, SEBT‐AM, and SEBT‐Composite suggests that dynamic balance and reach differences between legs may cause a reduction in jumping performance. Leg stiffness may influence stored elastic energy and optimization of performance during a jumping task in older individuals.33 Decreased dynamic reach in the excursion task in one leg may signal excessive stiffness and less elastic energy potential in that leg which would result in decreased jump performance.
The current data suggest that both functional and performance testing can provide the practitioner with useful information. It does not appear possible to simply replace performance tests with specific functional testing, nor do a small number of functional tests provide the strength and conditioning or rehabilitation professional with all needed information regarding functional limitations. The combination of various functional tests, asymmetries in those functional tests, and standard performance measures provides useful information regarding performance limitations and potential injury risks. Screening for asymmetries may offer predictive value with regards to sport injuries34,35, but the specific screens and the overall sensitivities and specificities as well as predictive values need to be further evaluated. This results of this study demonstrate the potential value for the use of modified excursion testing as well as dorsiflexion testing among basketball players. More research is needed to identify key connections to injury risk as well as strategies for integrating the data collected from a blended testing battery towards the goal of improving performance and limiting injury risk.
The present study has some limitations. First, the sample size was small. For this reason, the effect size was analyzed to determine the magnitude of the effect independent of the sample size. Secondly, the authors have tested only elite male basketball players (∼15 years). Further studies with athletes from different sports and of various ages are required to further understand the relationships between functional movement testing and performance testing.
Conclusions
The various relationships between dynamic functional movement testing, speed, and jump performance provides guidance for the professional when conducting and evaluating data in an effort to improve performance and reduce risk of injury. The results of the present study suggest that although some relationships exist between tests, the studied functional and performance tests do not measure the same components of human movement, and could be paired as outcome measures for the clinical and sport assessment of lower extremity function. Additionally, asymmetries in weight bearing dorsiflexion were related to decreased performance in change of direction tasks and greater range of motion was related to decreased sprint performance in some tests. To support elite levels of performance in basketball, strength and conditioning specialists should conduct a variety of dynamic functional movement tests, sport‐specific performance tests, and conduct evaluations to examine each athlete's limitations. Training programs that foster appropriate dynamic range of motion and muscular symmetry may be designed based on testing data to influence performance. Further research is needed to identify the optimal degree of ROM and symmetries that foster optimal performance.
REFERENCES
- 1.Maulder PC, J. Horizontal and vertical jump assessment: reliability, symmetry, discriminative and predictive ability. Phys Ther in Sport. 2005;6(2):74–82. [Google Scholar]
- 2.Gustavsson A Neeter C Thomee P, et al. A test battery for evaluating hop performance in patients with an ACL injury and patients who have undergone ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2006;14(8):778‐788. [DOI] [PubMed] [Google Scholar]
- 3.Meylan C McMaster T Cronin J Mohammad NI Rogers C Deklerk M. Single‐leg lateral, horizontal, and vertical jump assessment: reliability, interrelationships, and ability to predict sprint and change‐of‐direction performance. J Strength Cond Res. 2009;23(4):1140‐1147. [DOI] [PubMed] [Google Scholar]
- 4.Myer GD Martin L Jr. Ford KR, et al. No association of time from surgery with functional deficits in athletes after anterior cruciate ligament reconstruction: evidence for objective return‐to‐sport criteria. Am J Sports Med. 2012;40(10):2256‐2263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Robbins DW. Relationships between National Football League combine performance measures. J Strength Cond Res. 2012;26(1):226‐231. [DOI] [PubMed] [Google Scholar]
- 6.Castillo‐Rodriguez A Fernandez‐Garcia JC Chinchilla‐Minguet JL Carnero EA. Relationship between muscular strength and sprints with changes of direction. J Strength Cond Res. 2012;26(3):725‐732. [DOI] [PubMed] [Google Scholar]
- 7.Chisholm MD Birmingham TB Brown J Macdermid J Chesworth BM. Reliability and validity of a weight‐bearing measure of ankle dorsiflexion range of motion. Physiother Can. 2012;64(4):347‐355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Backman LJ Danielson P. Low range of ankle dorsiflexion predisposes for patellar tendinopathy in junior elite basketball players: a 1‐year prospective study. Am J Sports Med. 2011;39(12):2626‐2633. [DOI] [PubMed] [Google Scholar]
- 9.Basnett CR Hanish MJ Wheeler TJ, et al. Ankle dorsiflexion range of motion influences dynamic balance in individuals with chronic ankle instability. Int J Sports Phys Ther. 2013;8(2):121‐128. [PMC free article] [PubMed] [Google Scholar]
- 10.Dill KE Begalle RL Frank BS Zinder SM Padua DA. Altered knee and ankle kinematics during squatting in those with limited weight‐bearing‐lunge ankle‐dorsiflexion range of motion. J Athl Train. 2014;49(6):723‐732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Overmoyer GV Reiser RF, 2nd. Relationships between asymmetries in functional movements and the star excursion balance test. J Strength Cond Res. 2013;27(7):2013‐2024. [DOI] [PubMed] [Google Scholar]
- 12.O’Driscoll J Kerin F Delahunt E. Effect of a 6‐week dynamic neuromuscular training programme on ankle joint function: A Case report. Sports Med Arthrosc Rehabil Ther Technol. 2011;3:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Delahunt E Chawke M Kelleher J, et al. Lower limb kinematics and dynamic postural stability in anterior cruciate ligament‐reconstructed female athletes. J Athl Train. 2013;48(2):172‐185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sman AD Hiller CE Rae K, et al. Predictive factors for ankle syndesmosis injury in football players: a prospective study. J Sci Med Sport. 2014;17(6):586‐590. [DOI] [PubMed] [Google Scholar]
- 15.Plisky PJ Rauh MJ Kaminski TW Underwood FB. Star Excursion Balance Test as a predictor of lower extremity injury in high school basketball players. J Orthop Sports Phys Ther. 2006;36(12):911‐919. [DOI] [PubMed] [Google Scholar]
- 16.Gribble PA Hertel J Plisky P. Using the Star Excursion Balance Test to assess dynamic postural‐control deficits and outcomes in lower extremity injury: a literature and systematic review. J Athl Train. 2012;47(3):339‐357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Filipa A Byrnes R Paterno MV Myer GD Hewett TE. Neuromuscular training improves performance on the star excursion balance test in young female athletes. J Orthop Sports Phys Ther. 2010;40(9):551‐558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Endo Y Sakamoto M. Relationship between Lower Extremity Tightness and Star Excursion Balance Test Performance in Junior High School Baseball Players. J Phys Ther Sci. 2014;26(5):661‐663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ambegaonkar JP Mettinger LM Caswell SV Burtt A Cortes N. Relationships between core endurance, hip strength, and balance in collegiate female athletes. Int J Sports Phys Ther. 2014;9(5):604‐616. [PMC free article] [PubMed] [Google Scholar]
- 20.Lockie RG Schultz AB Callaghan SJ Jeffriess MD. The Relationship between Dynamic Stability and Multidirectional Speed. J Strength Cond Res. 2013. [DOI] [PubMed] [Google Scholar]
- 21.Mirwald RL Baxter‐Jones AD Bailey DA Beunen GP. An assessment of maturity from anthropometric measurements. Med Sci Sports Exerc. 2002;34(4):689‐694. [DOI] [PubMed] [Google Scholar]
- 22.Calatayud J Martin F Gargallo P Garcia‐Redondo J Colado JC Marin PJ. The validity and reliability of a new instrumented device for measuring ankle dorsiflexion range of motion. Int J Sports Phys Ther. 2015;10(2):197‐202. [PMC free article] [PubMed] [Google Scholar]
- 23.Baumgartner TA Chung H. Confidence limits for intraclass reliability coefficients. Meas Phys Educ Exerc Sci. 2001;5:179‐188. [Google Scholar]
- 24.Hori N Newton RU Kawamori N McGuigan MR Kraemer WJ Nosaka K. Reliability of performance measurements derived from ground reaction force data during countermovement jump and the influence of sampling frequency. J Strength Cond Res. 2009;23(3):874‐882. [DOI] [PubMed] [Google Scholar]
- 25.Hopkins WG Marshall SW Batterham AM Hanin J. Progressive statistics for studies in sports medicine and exercise science. Med Sci Sports Exerc. 2009;41(1):3‐13. [DOI] [PubMed] [Google Scholar]
- 26.Hopkins W. Reliability from consecutive pairs of trials (Excel spreadsheet). Internet Society for Sport Science, sportsci.org/resource/stats/xrely.xls. 2012. [Google Scholar]
- 27.Bell DR Sanfilippo JL Binkley N Heiderscheit BC. Lean mass asymmetry influences force and power asymmetry during jumping in collegiate athletes. J Strength Cond Res. 2014;28(4):884‐891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jonhagen S Ericson MO Nemeth G Eriksson E. Amplitude and timing of electromyographic activity during sprinting. Scand J Med Sci Sports. 1996;6(1):15‐21. [DOI] [PubMed] [Google Scholar]
- 29.Mann RA Moran GT Dougherty SE. Comparative electromyography of the lower extremity in jogging, running, and sprinting. Am J Sports Med. 1986;14(6):501‐510. [DOI] [PubMed] [Google Scholar]
- 30.Kyrolainen H Avela J Komi PV. Changes in muscle activity with increasing running speed. J Sports Sci. 2005;23(10):1101‐1109. [DOI] [PubMed] [Google Scholar]
- 31.Earl JE Hertel J. Lower‐extremity muscle activation during the Star Excursion Balance Tests. J Sports Rehab. 2001;10(2):93‐104. [Google Scholar]
- 32.Pruyn EC Watsford M Murphy A. The relationship between lower‐body stiffness and dynamic performance. Appl Physiol Nutr Metab. 2014;39(10):1144‐1150. [DOI] [PubMed] [Google Scholar]
- 33.Liu Y Peng CH Wei SH Chi JC Tsai FR Chen JY. Active leg stiffness and energy stored in the muscles during maximal counter movement jump in the aged. J Electromyogr Kinesiol. 2006;16(4):342‐351. [DOI] [PubMed] [Google Scholar]
- 34.Shambaugh JP Klein A Herbert JH. Structural measures as predictors of injury basketball players. Med Sci Sports Exerc. 1991;23(5):522‐527. [PubMed] [Google Scholar]
- 35.Paterno MV Schmitt LC Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38(10):1968‐1978. [DOI] [PMC free article] [PubMed] [Google Scholar]