Abstract
Posterior dislocation of the sterno‐clavicular (SC) joint is a rare injury in athletes. It normally occurs in high collision sports such as American football or rugby. Acute posterior dislocations of the SC joint can be life‐threatening as the posteriorly displaced clavicle can cause damage to vital vascular and respiratory structures such as the aortic arch, the carotid and subclavian arteries, and the trachea. The potential severity of a posterior SC joint dislocation provides multiple challenges for clinicians involved in the emergency care and treatment of this condition. Integration of clinical examination observations, rapid critical thinking, and appropriate diagnostic imaging are often required to provide the best management and outcome for the injured athlete. The criterion for return‐to‐play and participation in collision sports after suffering a posterior dislocation of the SC joint are unclear due to the rarity of this injury. The purpose of this case report is to describe the management, from the initial on‐field evaluation through the return‐to‐sport, of a collegiate Division I football player following a traumatic sports‐related posterior SC joint dislocation. The rehabilitation process and the progression to return to participation are also presented and briefly discussed.
Level of Evidence
4‐Single case report
Keywords: Athletes, shoulder rehabilitation, sterno‐clavicular joint dislocation
INTRODUCTION
Among all injuries of the shoulder complex, sternoclavicular (SC) joint dislocations are the least frequent1,2 and account for only about 3% of all shoulder girdle injuries in athletes.1,3,4 Most SC joint dislocations experienced during athletic participation have occurred in collision sports such as American football or rugby.2,4,5 The ratio to anterior to posterior SC joint dislocation is 9 to 1.6,7,8 Two main mechanisms for posterior SC joint dislocations have been described. One is a high velocity postero‐lateral compressive force to the involved shoulder.2,9 The other mechanism involves a direct force to the antero‐medial aspect of the clavicle, thus, causing the head of the clavicle to displace posteriorly.2,8,9
Due to the proximity of the SC joint to vital vascular (i.e. aortic arch, carotid and subclavian arteries,) and respiratory (i.e. tracheal) structures, life‐threatening conditions may occur with a posterior SC joint dislocation.8,9,10 These factors pose a particular challenge regarding clinical decision‐making for health care providers responsible for the on‐the‐field emergency management of acute SC joint injuries. There are only a few cases documented in the literature of athletes suffering SC joint dislocations.5,11,12,13 Therefore, there are limited data regarding the best evidence‐based approach for the return‐to‐play criteria and prognosis after this injury, specifically for athletes participating in contact or collision sports. The purpose of this case report is to describe the management, from the initial on‐field evaluation through the return‐to‐sport, of a collegiate Division I football player following a traumatic sports‐related posterior SC joint dislocation.
CLINCAL PRESENTATION
A 20‐year‐old Division I football cornerback jumped to intercept the ball and landed on the posterolateral aspect of the left shoulder during a game. The player was unable to stand up from the play and remained on the field, in a kneeling position. The medical team (head and assistant athletic trainers, and orthopedic surgeon) came on to the field to assess the player. During the on‐field assessment, the athlete reported significant left clavicular, chest, and anterior cervical pain. He exhibited dyspnea and dysphagia but denied upper extremity numbness or tingling. He also demonstrated decreased active range‐of‐motion of the left shoulder, particularly with attempts to elevate overhead. Once the shoulder pads were removed, there was a palpable defect over the left clavicle near its sternal attachment, although there was not a visible indentation at the joint. Based on this presentation, a sternoclavicular (SC) joint dislocation was suspected.
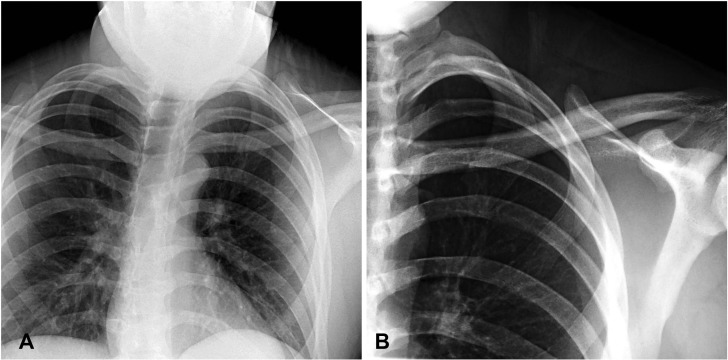
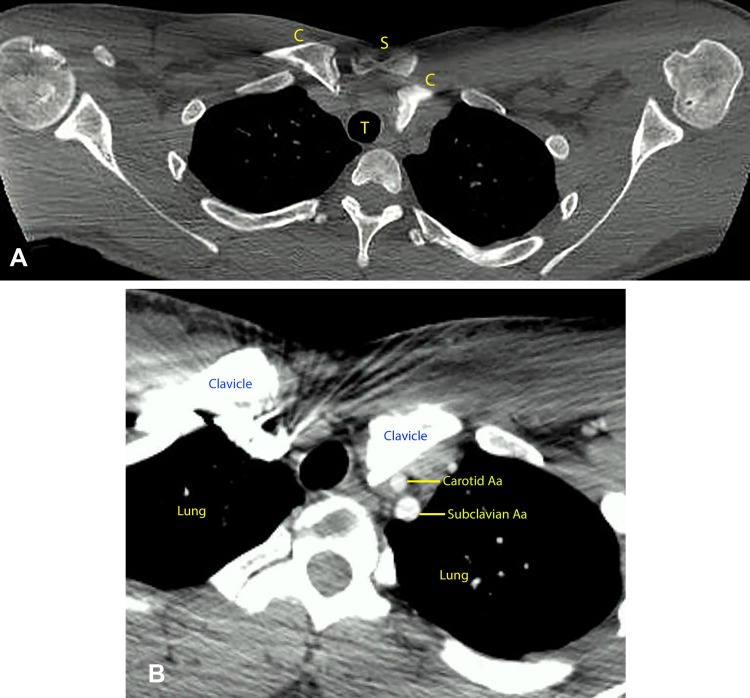
The athlete was immobilized with a shoulder sling and transported to the local emergency department. Standard chest and shoulder anterior‐posterior radiographs showed no definitive clavicular pathology (Figure 1A and 1B). As a result, a Computed Tomography (CT) scan was ordered. CT scan provides optimal visualization of the SC joint, including bony and soft tissue, and it can also allow assessment of other tissues within the mediastinum such as the heart, large vessels, trachea, esophagus, and bronchi. The CT scan confirmed the posterior SC dislocation (Figure 2A). The athlete was stable at this time with normal vital signs and, therefore, the CT scan helped to corroborate his current medical status. Because of the risks associated with the procedures necessary for SC joint reduction, the emergency room physician decided to further transport the athlete to a Level I trauma center with a cardiothoracic surgeon on‐call for definitive care.
Figure 1.
A‐1B. A standard AP view of chest (Figure 1A), and left clavicle and shoulder (Figure 1B) radiographs revealing no definitive clavicular pathology. Note the superimposition of overlapping structures such as the ribs, the clavicles, sternum, and vertebrae which make it difficult to visualize the SC joint.
Figure 2.
A‐2B. An axial view of a CT scan (Figure 2A), revealing a posterior dislocation of the left sternoclavicular joint. Note the posterior position of the medial head of the involved clavicle (C) compared to the uninvolved clavicle (C) in relationship to the sternum (S). Figure 2B, an axial view of a CT scan with injected contrast (angiography), shows the proximity of the dislocated clavicle (C) to the trachea (T). Note the dislocated clavicle sitting directly over the left carotid and subclavian arteries.
Upon arrival at the trauma center, a further CT scan with contrast (angiography) and a 3‐D reconstruction of the axial view of the CT scan were performed and revealed no evidence of vascular or pulmonary compromise (Figure 2B and Figure 3). The attending trauma physician proceeded to describe the nature and the risks of the reduction procedure to the athlete. He explained that closed joint reduction initially would be attempted. If the closed reduction was unsuccessful, an open reduction and internal fixation of the joint would be undertaken. The athlete was placed under general anesthesia on the operating table in the supine position with a towel roll between the scapulae. The orthopedic surgeon applied a posteriorly‐directed force through the anterior aspect of both shoulders (surgeon's hands were placed over the distal aspect of the clavicles and gleno‐humeral joints). Successful closed joint reduction occurred simultaneous with an audible “clunk”. The orthopedic surgeon performed a physical examination of the left SC joint under fluoroscopy using a serendipity view where the proper anatomical alignment of the reduced joint was visualized, confirming the impression based on the clinical exam (Figure 4). There were no secondary vascular, pulmonary, or bony injuries associated with the reduction maneuver. The patient was kept in the hospital for observation for 23 hours following the procedure and was then discharged home with his shoulder immobilized in a sling, under the supervision of the university medical team.
Figure 3.
A 3‐dimensional reconstruction of the axial view CT scan, showing the left sternoclavicular joint posterior dislocation without evidence of vascular or pulmonary compromise
Figure 4.
Intraoperative fluoroscopic “serendipity” view, demonstrating proper reduction of the left sternoclavicular joint. A physical exam of the left sternoclavicular joint was performed intra‐operatively using this imaging technique in order to confirm the correct position of the sternoclavicular joint.
CLINICAL EXAMINATION
Knowledge of the key anatomical structures and the joint architecture is essential in order to examine an acute injury of the SC joint. The SC joint occurs between the proximal end of the clavicle and the clavicular notch of the manubrium of the sternum together with a small part of the first costal cartilage. The SC joint is a saddle‐type articulation that allows movement of the clavicle, predominantly in antero‐posterior and vertical planes, although some rotation also occurs. The ability to flex and elevate the shoulder requires sound function of this joint. The SC junction is highly stable. Its stability is provided by the sternoclavicular, interclavicular and costoclavicular ligaments.8,9 Although SC joint sprains are more prevalent than dislocations in sports, SC joint dislocations are rare because they require a complete rupture of the costoclavicular ligament. Knowledge of the neighboring vital structures such as the trachea and the great vessels, which carry blood supply to and from the heart near this joint, is similarly essential. Dislocations to the SC joint can cause damage to these structures, which in turn, may lead to a medical emergency.
As is the case concerning the assessment of any traumatic sports‐related injury, the health care provider must initially rule‐out any potential life‐threatening conditions. Observation from the sidelines of the field can provide an initial impression of a potential injury and can aid the clinician to quickly identify structures that may be involved. In this case, the football player sustained a compressive force to the postero‐lateral shoulder when contacting the ground, and the mechanism of injury was in fact observed by the medical staff. Sports medicine clinicians must highly suspect a traumatic dislocation of any of the joints that comprise the shoulder girdle when assessing an injury presenting after such a mechanism.
Table 1 summarizes the clinical presentation and the signs and symptoms commonly reported in the literature following a SC joint dislocation. The subject of this case report reported immediate pain to the medial aspect of the left clavicle, chest, and anterior cervical area following the injury. He held his head in a forward and laterally flexed position toward the injured shoulder and reported increased pain with any attempts to return his head to a neutral position. He also had increased pain with left shoulder active and passive movement. Most concerning was that he complained of dysphagia and dyspnea. These findings are consistent with other cases of posterior SC joint dislocations previously described in the literature.5,8,9,10,13 Neurological involvement including paresthesia and loss of sensation on the side of the involved extremity have also been reported, specifically in those cases where neural tissue compression occurred.8,9,14 The subject described in this case had a normal neurological exam. Upon inspection of the area in an injured athlete, clavicular asymmetry may be present and has been described by previously reported cases. With SC joint dislocations, the medial aspect of the clavicle may be displaced relative to the lateral aspect with a palpable defect or step‐off deformity to the involved SC joint.8,9 Palpation of the injury can initially help to recognize the deformity associated with the potential pathology of the joint. Palpatory exam of the region, however, may be difficult to accomplish since tenderness and joint incongruence can mask a clavicular fracture, a subluxation or the direction of the dislocation of the joint.8,9
Table 1.
Common signs and symptoms and clinical presentation of SC joint injury
| Common signs and symptoms and clinical presentation of SC joint injury |
|---|
|
+++Symptoms exhibited by the athlete described in this case report
In approximately 30% of the cases, posterior SC joint dislocations may cause potentially fatal injuries because of its proximity of vital mediastinal structures.15,16,17 Life‐threatening Injuries associated with posterior SC joint dislocation include compression or laceration of the great vessels, tracheal compression or rupture, esophageal compression or rupture, injury to the brachial plexus and pleural disruption, which may lead to pneumothorax or subcutaneous emphysema.8,9,10,15,16,17 Fortunately, the subject in this case did not sustain any vascular or pulmonary injuries during the initial trauma or joint reduction.
DIAGNOSTIC IMAGING
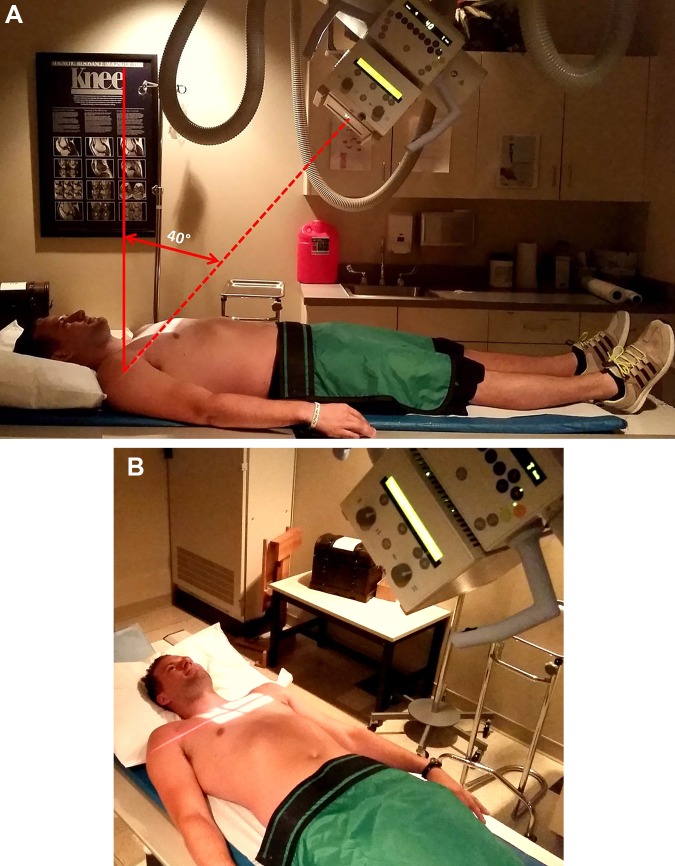
To assess for SC joint pathology, radiographs and CT scans are the primary imaging techniques. While standard view radiographs of the chest and the shoulder may show clavicular asymmetry, they may not provide a definitive diagnosis.18,19 In standard radiographic views, overlapping structures such as the clavicle, ribs, sternum, and vertebrae, complicate visualization of the SC joint. In the current case, initial standard chest and shoulder radiographs neither revealed a clavicular pathology nor conclusively showed a significant pathology of the SC joint. A “serendipity” view, an anterior to posterior view with a 40‐degree cephalic tilt of the x‐ray beam centered to the sternum, provides the most accurate assessment of the SC joint.7,20 (Figures 5A and 5B) This view provides the best image for assessing clavicular position relative to the manubrium and determining the direction of dislocation.7,20 Although in this case, a serendipity view was not used as part of the initial imaging work‐up, this view was used under a fluoroscope to determine appropriate anatomical positioning of the clavicle post reduction.
Figure 5.
A‐B. Photographs of “Serendipity” views, an anterior to posterior view with a 40 degree cephalic tilt of the x‐ray beam centered to the sternum.
CT scan is considered the gold standard for evaluating SC joint pathology.21,22,23 Sagittal and coronal reconstructions provide excellent visualization of the clavicle and its junction to the sternum, as well as determining potentially associated life‐threatening mediastinal injuries. CT scan with contrast (angiography) is the recommended imaging modality for definitive evaluation of acute SC joint dislocations and all secondary complications that can arise from such injury since it can best show these structures.7,21,22,23 In this case, CT scan was essential in confirming the posterior SC joint dislocation suffered by the subject. Likewise, this imaging was effective in ruling out any vascular or pulmonary injury from the initial trauma prior to the anatomical reduction of the joint.
ACUTE MANAGEMENT
The on‐field management of an athlete with a suspected acute SC joint injury, as suggested by symptomatology of vascular and respiratory compromise or with an obvious anatomical deformity, requires immobilization and transportation of the athlete to the most appropriate nearby facility for emergency management and definitive care.8,23 If a concurrent head or neck injury are also suspected, the cervical spine should be immobilized in the standard fashion for transportation. Care must be taken to not cause any further injury to the involved SC joint or increase the displacement of the dislocation while the athlete is placed on the supine position. Some athletes may experience increased pain when placed supine as the head goes to neutral position, which may cause further tension to the anterior chest area. If there are no concerns with cervical spine or head injury and the athlete is medically stable, a simple shoulder sling or a Figure of Eight brace may be sufficient to achieve immobilization while being transported to the emergency department. Reduction of the SC joint is not attempted on the field contrary to many other joints that may benefit from early reduction. This is due to the proximity of the SC joint to vital mediastinal structures that can possibly be disrupted with the reduction maneuver if they are not already compromised by the initial trauma.
Options for management of posterior SC joint dislocations include first attempting closed reduction in less than 24 to 48 hours post injury either under light sedation or general anesthesia.8,9,10,24 Two of the most described approaches for closed reduction involve placing the patient in supine with a rolled towel between the scapulae followed by either application of traction to the involved abducted shoulder moving the arm into extension, or by application of a posteriorly directed force to both shoulders (distal aspect of the clavicles and gleno‐humeral joints). The reported success rate for closed reduction using these techniques is approximately 68 to 80% if done early ( < 2 days post injury).8,9,10,24 As previously stated, with the subject described in this case, successful closed reduction of the joint was achieved by placing him under general anesthesia, and with a towel roll under his scapulae, after a posterior force was applied to both shoulders. Reduction took place with an audible pop at the involved SC joint and then the reduction was confirmed with imaging and physical examination.
Open reduction of the SC joint is recommended if closed reduction fails or in cases of chronic SC joint instability.10,24 Some authors have reported persisting instability after early closed reduction of the SC joint, specifically in skeletally immature children whose open physeal plates were posteriorly displaced or fractured.25 The results of a systematic review by Glass et al, 2011 revealed that delaying definitive treatment for SC joint dislocations usually results in the need for open reduction and stabilization after normally failing closed reduction.25 The optimal method for stabilization of the SC joint with open reduction has not yet been established. Overall good outcomes have been reported with various methods using soft tissue repair and ligamentous reconstruction as well as the use of absorbable sutures to stabilize the clavicle to the manubrium of the sternum in both adults and children.24,25,26 Complication rates with the use of hardware fixation have been unacceptably high and sometimes catastrophic, leading some authors to not support their use.25,27
After either closed or open reduction and stabilization of the SC joint, a period of joint immobilization generally takes place. This is done through the use of a Figure of Eight splint or a shoulder sling.22,23 The length of the immobilization has been reported to be anywhere from three to eight weeks depending on the technique utilized and the amount of stability achieved post reduction.7,8,22,23The football player described in this case was immobilized with a shoulder sling for a period of four weeks.
COURSE OF REHABILIATION
Three days after the injury and joint reduction, the athlete began rehabilitation (Figure 6). During the initial physical therapy evaluation, the Rockwood scoring system28 for SC joint pathology was used for the assessment of impairments at that time. This scale has been used in patients with degenerative SC joint conditions.28 The Rockwood scoring system is specific to the SC joint and is an appropriate outcome measure for the early assessment of the impairments commonly seen with SC joint dislocations (i.e. range of motion, strength, and pain). At the first physical therapy evaluation, the athlete in this case scored 4/15 points on the scale, which represented a high degree of impairment and functional limitation (Table 2).
Figure 6.
Photograph showing left sternoclavicular joint status, three days post reduction.
Table 2.
The scoring system of Rockwood used for the clinical evaluation and progress made by the injured football player suffering a posterior SC joint dislocation
| Category | 3 Days Post Injury (Initial PT Eval) | 12 Weeks Post Injury (PT re‐evaluation) | 16 Weeks Post Injury (Initiation of Complex Agility Training) |
|---|---|---|---|
| Pain | 2 | 3 | 3 |
| None 3 | |||
| Slight 2 | |||
| Moderate 1 | |||
| Severe (at rest) 0 | |||
| Range of Motion | 0 | 3 | 3 |
| Normal 3 | |||
| Slight Restriction (<25%) 2 | |||
| Mod. Restriction (25‐50%) 1 | |||
| Severe Restriction (>50%) 0 | |||
| Strength | 0 | 3 | 3 |
| Normal 3 | |||
| Slight Weakness (<25%) 2 | |||
| Mod. Weakness (25‐50%) 1 | |||
| Severe Weakness (>50%) 0 | |||
| Limitation | 1 | 3 | 3 |
| None 3 | |||
| Slight 2 | |||
| Moderate 1 | |||
| Severe 0 | |||
| Subjective Result | 1 | 2 | 3 |
| Excellent 3 | |||
| Good 2 | |||
| Fair 1 | |||
| Poor 0 | |||
| Total Score (/15) | 4/15 | 14/15 | 15/15 |
The initial goals of his rehabilitation program were to protect the injured SC joint, to improve cervical range of motion, and to promote left shoulder stabilization using isometric training. As the athlete's symptoms improved, he began progressive left shoulder range of motion training, as well as continued scapular, rotator cuff, and cervical stabilization using progressive resisted exercises. Initially, flexion and abduction to 90 degrees and gleno‐humeral rotation at 0 degrees of abduction was encouraged. Then, mobility training was progressed to overhead planes above 90 degrees of flexion and abduction and external rotation greater than 45 degrees of abduction ensuring pain‐free activities. Twelve weeks post injury he was allowed to begin advanced shoulder complex activities including upper extremity plyometric training, weight lifting, and individual non‐contact football skills. His weight lifting program consisted of gradual loading of all major upper extremity muscle groups (e.g. pectoralis major, triceps brachii, biceps brachii, trapezius, and the posterior scapular muscles) initially with body resisted exercise. He was subsequently allowed to use dumbbells and free weights, and eventually progressed to complex activities such as Olympic lifting with overhead motions. All of these activities were monitored to ensure proper form and were done in a pain‐free environment. Sixteen weeks post injury; he scored 15/15 points on the Rockwood scoring system, demonstrating minimal impairment with pain, range of motion, and strength surrounding the left SC joint. He was cleared for football participation with gradual progression to limited contact activities five months after the injury.
Based on the available literature, due to the rarity of this injury, there are no established consensus guidelines regarding rehabilitation procedures or return to play criteria following posterior SC joint dislocations in athletes participating of contact or collision sports. As a consequence, a theoretical framework based on principles of rehabilitation progression provided a guide for this case. The initial focus of rehabilitation for this injury was to promote SC joint protection as well as regaining shoulder girdle and cervical spine motion. After achieving proper mechanical function of the SC joint (normal and pain‐free mobility of the involved SC joint and all other joints making up the shoulder girdle as compared contra‐laterally), strengthening of muscles used to protect and stabilize the SC joint was initiated. Muscles that insert near the joint and that are directly involved with SC joint function such as the pectoralis major, pectoralis minor, upper trapezius, and sternocleidomastoid were incorporated in physical therapy. Likewise, rotator cuff and scapular muscles were relevant during this process. These muscles promote proper function of the other joints of the shoulder complex and are equally important for the overall “health” of the entire shoulder. Gradual introduction to sport‐specific skills and eventually contact activities (if SC joint stability is maintained) was the last step towards allowing the athlete to return to play. In this particular instance, the football player completed approximately four months of rehabilitation following the previously stated recovery outline.
The Rockwood scoring system was utilized as an outcome measure where he initially scored 4/15 points (day three post injury) and eventually improved to 15/15 points (four months post injury). In this case, physical examination, clinical judgment, and the use of sound rehabilitation progression, proved valuable to guide the athlete's rehabilitation process. Appendix 1 summarizes the framework utilized for the rehabilitation process and the activities and milestones that were used in order to progress our athlete after he suffered the SC joint dislocation.
OUTCOME
The football player described in this case was cleared after five months post injury for gradual return to football activities. He successfully completed spring football practices with limited contact. He wore a red jersey (indicating a protected status) and was allowed to do all non‐contact individual skills and drills. He was not allowed to hit or take direct hits during practice. Due to another unrelated injury (lower extremity); he did not compete during the following fall football season. He continued, however, with unrestricted upper extremity training and conditioning. Eighteen months after sustaining the posterior SC joint dislocation, he reported no SC joint pain and no signs of instability. He continued to perform all upper extremity weight lifting and functional agility training and was cleared for unrestricted football participation, having now also recovered from the unrelated lower extremity injury.
Although positive outcomes following posterior SC joint dislocations have been reported in the literature,24 there is very little available evidence regarding the long‐term functional ability for this patient population. Laffosse et al.24 retrospectively analyzed the outcomes of 30 (23 in rugby players and seven in other non‐collision sports) cases of posterior SC joint dislocations or epiphyseal disruption in sports participation. From the 23 cases that occurred in rugby, seven of these subjects decided to change sports for other activities with less contact, and only one subject reported that his occupational and sporting activities were restricted because of his injury. The rest of the rugby players resumed their usual sporting activity at the same level. The authors did not report any recurrent posterior SC joint dislocations with any of these cases. If satisfactory and stable reduction is obtained, these authors suggested that occupational and sports participation can be safely resumed after suffering a posterior SC joint dislocation.24 The available literature to date does not include any retrospective study assessing return to sporting activities in American football players after posterior dislocation of the SC joint.
RECOMMENDATIONS
As posterior SC joint dislocations are rare in athletics, clinicians involved in the management of acute injuries in athletes, especially in collision sports, need to be familiar with the clinical presentation of this injury and should exercise proper judgment in the presence of a life‐threatening condition associated with a posterior SC joint dislocation. Due to the proximity of the SC joint to vital vascular and pulmonary structures, reduction should only be attempted at a trauma facility with available cardiothoracic and/or cardiovascular services. Radiographs with standard views are not adequate to assess this injury because of overlapping osseous structures, specifically the clavicle, ribs, sternum, and vertebrae. A serendipity view radiograph may provide a good preliminary assessment of this condition and should be included as part of the initial radiographic study. A CT scan with injected contrast (angiography) is the recommended imaging technique for additional diagnostic information, giving greater visualization of the joint in multiple planes without superimposition of osseous structures in addition to being able to provide an evaluation of any associated mediastinal insult. Closed reduction of the SC joint is often sufficient as the primary management of this condition. In the event of closed reduction failure, open reduction and stabilization of the joint via soft tissue and ligamentous reconstruction and suturing of the bony structures is typically selected by surgeons. Both closed and open reduction procedures of the SC joint require a period of immobilization followed by a course of rehabilitation. The emphasis of post‐reduction physical therapy is to protect the involved SC joint and to restore proper function of the cervical spine and the involved shoulder girdle. Mobility and strengthening of structures that can help promote function and improve stability to the injured SC joint are imperative. Subsequently, functional training and sports specific activities can be introduced in order to allow the athlete to return to sports safely. Individuals suffering posterior dislocations of the SC joint normally have a good outcome in terms of successful return to their activities of daily living. There are not enough data to provide an accurate assessment of the prognostic outcome for return to play for those athletes competing in collision sports who suffer this injury. Although this is a rare injury, future research efforts should be geared towards defining appropriate methods and criteria to determine the readiness of those athletes involved in collision sports prior to their return to play.
Aknowledgments
Seth Means, MD, Board Certified Radiologist at Premier Diagnostic Imaging in Cookeville TN, who provided his diagnostic imaging expertise with the interpretation and the selection of the images and photographs for this case report.
Appendix 1.
Guidelines followed for rehabilitation of SC joint dislocation in the subject of the case report
| GOALS | SUGGESTED ACTIVITIES | MILESTONES/CRITERIA FOR PROGRESSION |
|---|---|---|
| SC joint protection | Joint immobilization using a sling | Proper SC joint stability |
| Edema/swelling control | Ice | Pain‐free full ROM of cervical spine and shoulder all planes |
| Normal mobility of cervical spine and involved upper extremity | Cervical spine pain‐free AROM exercises all planes, shoulder pain‐free A‐AROM (PROM as needed) exercises all planes, submaximal cervical spine and shoulder isometrics | Minimal swelling |
| Cervical spine and shoulder strengthening (Below shoulder height) | Cervical 4‐way resistance exercises with bands and tubing, shrugs, Swiss ball stability exercises for the neck | Proper SC joint stability Minimal swelling |
| Rows, shoulder extension, internal and external rotation, PNF patterns with tubing and dumbbells, Swiss ball scapular stabilizing exercises | MMT grading scale of 5/5 with all planes of the cervical spine and bilateral shoulders and scapular muscles | |
| Proper shoulder proprioception | Body Blade®, manual and medicine ball rhythmic stabilization activities | No pain reported at the SC joint with these activities |
| Fitness improvement and maintenance | Aerobic training with bike, elliptical, running, etc. (avoid sprinting and potential activities that can lead to falls or collision) | |
| Increase of shoulder girdle/UE power | Rotator cuff and scapular strengthening above shoulder height with resistance cables and free weights | Proper SC joint stability No pain reported at the SC joint with these activities |
| Bench press, incline bench, flies, high pulls, Olympic lifting, etc. (as previously performed) | Rockwood scale score of > 13/15 Physician's clearance to contact and collision activities |
|
| Introduction to non‐contact agility training | Upper extremity plyometric training with trampoline, boxes, BOSU ball, etc. | |
| Increased in fitness and conditioning | Sprinting, cutting, jumping, pivoting, ball/object handling, etc. per sports demands (no contact allowed) | |
| Return to contact and collision activities | Gradual progression of contact activities from using dummies, to supervised collision, to full contact and collision activities as required by the sport | Pain‐free SC joint with sporting activities Proper SC joint stability with no recurrence of SC joint subluxation or dislocation |
| Full participation of conditioning and strength training activities | Continued strength and conditioning activities per sports requirements | Return to full unrestricted sports participation upon final clearance by physician |
| Independent program/HEP | Independent home/gym maintenance program including cervical stabilization, rotator cuff and scapular strengthening 2‐3/week |
REFERENCES
- 1.McGown AT. Blunt abdominal and chest trauma. Athletic Therapy Today. 2004;9(1):40‐41. [Google Scholar]
- 2.Prentice WE. Rehabilitation Techniques for Sports Medicine and Athletic Training. 4th ed. New York, NY: McGraw‐Hill; 2004. [Google Scholar]
- 3.Lampasi M Bochicchio V Bettuzzi C Donzelli O. Sternoclavicularphyseal fracture associated with adjacent clavicle fracture in a 14‐year‐old boy: A case report and literature review. Knee Surg Sports Traumatol Arthrosc. 2008;16:699‐702. [DOI] [PubMed] [Google Scholar]
- 4.Little NJ Bismil Q Chipperfield A Ricketts DM. Superior dislocation of the sternoclavicular joint. J Shoulder Elbow Surg. 2008;17: e22‐e23. [DOI] [PubMed] [Google Scholar]
- 5.Mirza A H Alam K Ali A. Posterior sternoclavicular dislocation in a rugby player as a cause of silent vascular compromise: a case report. Br J Sports Med 2005. 39: e28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nettles JL Linscheid RL. Sternoclavicular dislocations. J Trauma 1968;8(2):158‐64. [DOI] [PubMed] [Google Scholar]
- 7.Rockwood CA Wirth MA. Fractures in adults. 5th ed. Philadelphia: Lippincott‐Raven; 2001. p. 1245‐92. [Google Scholar]
- 8.Yeh GL Williams GR. Conservative management of sternoclavicular injuries. Orthop Clin North Am 2000;31:189‐203. [DOI] [PubMed] [Google Scholar]
- 9.Bulstrode CKJ, et al. , editors. Oxford textbook of orthopedics and trauma. 10th ed. Oxford: Oxford University Press; 2001. p.693‐6; 2053‐5. [Google Scholar]
- 10.Wirth MA, Rockwood CA Jr. Acute and chronic traumatic injuries of the sternoclavicular joint. J Am Acad Orthop Surg 1996;4:268‐78. [DOI] [PubMed] [Google Scholar]
- 11.Garg S Alshameeri Z Wallace WA. Posterior sternoclavicular joint dislocation in a child: a case report with review of literature. J Shoulder Elbow Surg (2012) 21, e11‐e16 [DOI] [PubMed] [Google Scholar]
- 12.Kuzak N Ishkanian A Abu‐Laban RB. Posterior sternoclavicular joint dislocation: case report and discussion. Can J Emerg Med 2006;8(5):355‐7 [DOI] [PubMed] [Google Scholar]
- 13.Marker L B Klareskov B. Posterior sternoclavicular dislocation: an American football injury. Br J Sports Med 1996. 30: 71‐72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rayan GM. Compression brachial plexopathy caused by chronic posterior dislocation of the sternoclavicular joint. J Okla State Med Assoc 1994;87:7‐9. [PubMed] [Google Scholar]
- 15.Nakayama E Tanaka T Noguchi T Yasuda J Terada Y. Tracheal stenosis caused by retrosternal dislocation of the right clavicle. Ann Thorac Surg 2007;83:685‐7 [DOI] [PubMed] [Google Scholar]
- 16.O’Connor PA Nolke L O’Donnell A Lingham KM. Retrosternal dislocation of the clavicle associated with a traumatic pneumothorax. Interact Cardio Vasc Thorac Surg 2003;2:9‐11. [DOI] [PubMed] [Google Scholar]
- 17.Wasylenko MJ Busse EF. Posterior dislocation of the clavicle causing fatal tracheoesophageal fistula. Can J Surg 1981;24:626‐7. [PubMed] [Google Scholar]
- 18.Abdulla SR Gandham SG. Posterior dislocation of sternoclavicular joint in a child. J Accid Emerg Med 1999;16:385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Carmichael KD Longo A Lick S Swischuk L. Posterior sternoclavicular epiphyseal fracture‐dislocation with delayed diagnosis. Skeletal Radiol 2006;35‐8:608‐12 [DOI] [PubMed] [Google Scholar]
- 20.MacDonald P Lapointe P. Acromioclavicular and sternoclavicular joint injuries. Orthop Clin North Am. 2008;39:535‐545 [DOI] [PubMed] [Google Scholar]
- 21.Cope R Riddervold HO. Posterior dislocation of the sternoclavicular joint: report of two cases, with emphasis on radiologic management and early diagnosis. Skeletal Radiol 1988;17:247‐50. [DOI] [PubMed] [Google Scholar]
- 22.Gove N Ebraheim NA Glass E. Posterior sternoclavicular dislocations: Review of management and complications. Am J Orthop 2006; 35:132‐6. [PubMed] [Google Scholar]
- 23.Groh GI Wirth MA. Management of traumatic sternoclavicular joint injuries. J Am Acad Orthop Surg 2011;19:1‐7. [DOI] [PubMed] [Google Scholar]
- 24.Laffosse JM Espie A Bonnevialle N Mansat P Tricoire JL Bonnevialle P, et al. Posterior dislocation of the sternoclavicular joint and epiphyseal disruption of the medial clavicle with posterior displacement in sports participants. J Bone Joint Surg [Br] 2010;92‐B:103‐9 [DOI] [PubMed] [Google Scholar]
- 25.Glass ER Thompson JD Cole PA Gause TM Altman GT. Treatment of sternoclavicular joint dislocations: A systematic review of 251 dislocations in 24 case series. J Trauma Acute Care Surg 2011;70:1294‐8. [DOI] [PubMed] [Google Scholar]
- 26.Waters PM Bae DS Kadiyala RK. Short‐term outcomes after surgical treatment of traumatic posterior sternoclavicular fracture‐dislocations in children and adolescents. J Pediatr Orthop 2003;23:464‐9. [PubMed] [Google Scholar]
- 27.Clark RL Milgram JW Yawn DH. Fatal aortic perforation and cardiac tamponade due to a Kirschner wire migrating from the right sternoclavicular joint. South Med J 1974;67:316‐8. [DOI] [PubMed] [Google Scholar]
- 28.Pingsmann A Patsalis T Michiels I. Resection arthroplasty of the sternoclavicular joint for the treatment of primary degenerative sternoclavicular arthritis. J Bone Joint Surg [Br] 2002;84‐B:513‐7 [DOI] [PubMed] [Google Scholar]