Abstract
Study Design
Case report: differential diagnosis and clinical decision making
Background and Purpose
Young adults with lateral hip pain are often referred to physical therapy (PT). A thorough examination is required to obtain a diagnosis and guide management. The purpose of this case report is to describe the physical therapist's differential diagnostic process and clinical decision making for a subject with the referring diagnosis of trochanteric bursitis.
Case Description
A 29‐year‐old female presented to PT with limited sitting and running tolerance secondary to right lateral hip pain. Her symptoms began three months prior when she abruptly changed her running intensity and frequency of weight bearing activities, including running and low impact plyometrics for the lower extremity. Physical examination revealed a positive Trendelenburg sign, manual muscle test that was weak and painless of the right hip abductors, and pain elicited when performing a vertical hop on a concrete surface (+single leg hop test), but pain‐free when performing the same single leg hop on a foam surface. Examination findings warranted discussion with the referring physician for further diagnostic imaging.
Outcomes
Magnetic resonance imaging revealed a focus of edema in the posterior acetabulum, suspicious for an acetabular stress fracture. The subject was subsequently diagnosed with an acetabular stress fracture and restricted from running and plyometrics for four weeks.
Discussion
Thorough examination and appropriate clinical decision making by the physical therapist at the initial examination led to the diagnosis of an acetabular stress fracture in this subject. Clinicians must be aware of symptoms and signs which place the subject at risk for stress fracture for timely referral and management.
Level of evidence
4
Keywords: Pelvic pain, stress fracture, trochanteric bursitis
INTRODUCTION/BACKGROUND AND PURPOSE
Lateral hip pain, more recently termed greater trochanteric pain syndrome (GTPS)1 is a common orthopaedic problem that affects 1.8 patients per 1000 annually.2,3 GTPS is estimated to affect between 10%‐25% of the population in industrialized societies and is 3‐4 times more likely to affect females.3 GTPS usually presents as intermittent pain over the buttock and/or lateral aspect of the thigh that is exacerbated by lying on the affected side, standing for prolonged periods of time, sitting with legs crossed, climbing stairs, running, or other high impact activities.3,4 Patients with GTPS usually have lateral hip pain, tenderness over and around the greater trochanter, pain at end‐range hip rotation, abduction or adduction, pain with resisted hip abduction, and a positive Patrick‐FABER test.3 Segal et al1 found that the prevalence of GTPS is associated with female gender, obesity, iliotibial band tenderness, knee osteoarthritis or knee pain, and low back pain.
Patients with lateral hip pain are often referred to physical therapy (PT) with a diagnosis of GTPS or trochanteric bursitis. Although often used interchangeably, trochanteric bursitis distinctly describes a localized inflammation of one or more bursae overlying the greater trochanter4 with erythema, edema, and rubor3,4 that is uncommon in patients with lateral hip pain.3 Most commonly, GTPS is related to gluteus medius tendinosis.5
Although GTPS is more prevalent between the fourth and sixth decades of life,3 it can be seen in active young adults.6 Young adults (18‐35 years old) with hip pain often present with non‐specific symptoms and vague findings from the history and physical examination7,8 which may lead to a misdiagnosis of GTPS or trochanteric bursitis.
Differential diagnosis of lateral hip pain can be challenging, even to experienced hip surgeons and diagnosticians, particularly in young adults.8,9,10 The list of competing diagnoses is outlined in Table 1.8,11,12 Several case reports have been published demonstrating misdiagnoses of GTPS. Wakeshima and Ellen13 reported on a subject with a giant cell carcinoma in a young athletic woman who was diagnosed with GTPS and treated in PT for nine months. Further, a non‐displaced, complete femoral neck fracture was found in a 46‐year‐old male recreational runner who was treated with two separate episodes of PT for GTPS.14
Table 1.
Differential diagnoses for lateral hip pain
| Acetabular labral tear |
| Stress fracture, dislocation, fracture, contusion |
| Osteonecrosis, avascular necrosis |
| Muscle strain/tear, ligament sprain |
| Low back pain, sacroiliac joint dysfunction |
| Snapping hip syndrome |
| Femoral acetabular impingement |
| Bursitis |
| Nerve entrapment syndrome |
| Inflammatory disorders such as seronegative arthropathy, rheumatoid arthritis |
| Infection |
| Childhood disorders (Leg‐Cave‐Perthes disease) |
| Metabolic disease |
| Tumor |
| Primary or secondary osteoarthritis |
| Psychosocial factors |
The possibility of a stress fracture at the hip and pelvis as a source of lateral hip pain should be ruled out hastily because appropriate treatment is required to prevent further complications, such as complete fracture(s) and avascular necrosis.8 Young adults who are involved in sports or recreational activities that require repetitive movement patterns may be predisposed to stress fractures due to cumulative stress placed on the hip joints. Bruist et al15 reported running related injuries occurring in 25.9% of novice and recreational runners (n=629) over an eight‐week training period. They also found females with higher body mass index and lack of running experience were most at risk for running related injuries.15 Runners who abruptly increase the intensity, frequency, and/or duration of activity are also at higher risk for stress fractures involving the hip.12 Other risk factors for stress fractures include muscle‐tendon imbalance involving the strength ratio between agonist and antagonist hip muscles,16 poor footwear, training on uneven surfaces, female gender, low bone mineral density, foot structure, leg length discrepancy, increased degree of hip external rotation, and the female athlete triad.17 Furthermore, hormonal factors, such as menstrual disturbance, age at menarche, use of oral contraceptive pills, and nutritional factors such as low calcium intake and eating disorders may also contribute to a higher risk of stress fracture.17,18
The purpose of this case report is to describe the differential diagnostic process and clinical decision‐making in a subject referred to PT with a diagnosis of right trochanteric bursitis.
CASE DESCRIPTION: Subject History and Systems Review
A 29‐year‐old Caucasian female presented to PT with limited sitting and running tolerance secondary to right lateral hip pain. Onset of pain was approximately three months prior to her initial PT examination. After running on a treadmill at an 11‐minute/mile pace with 0% incline for 30 minutes, she changed her speed to an 8‐minute/mile pace and experienced a “twinge” in her right lateral hip. For the next two months the subject continued to experience that same “twinge” in her right lateral hip, but increased her running frequency from one time per week to two times per week. At that time, she also began working with a personal trainer four times per week, which consisted of performing low impact plyometric exercises for the lower extremity (LE).
During the initial evaluation, the subject reported worsening right lateral hip pain that caused her to stop running two weeks prior. The subject complained of deep aching, intermittent pain, and a “twinge” feeling rated 0/10 at best over the prior week, 2/10 during the evaluation, and 5/10 at worst on the Numeric Pain Rating Scale (0 = pain‐free; 10=worst pain imaginable).19 A body chart outlines the location of pain (Figure 1). Pain was localized to her right lateral hip approximately five centimeters proximal to the greater trochanter. She was unable to sit for more than 30 minutes or run for more than two minutes without right lateral hip pain. She also reported lateral hip pain during transitional movements (scooting on bed, repositioning in a chair) that quickly subsided. Sleeping and lying supine provided some pain relief. In spite of her limitations, the subject scored a 72/80 on the Lower Extremity Functional Scale20 indicating a high functional level.
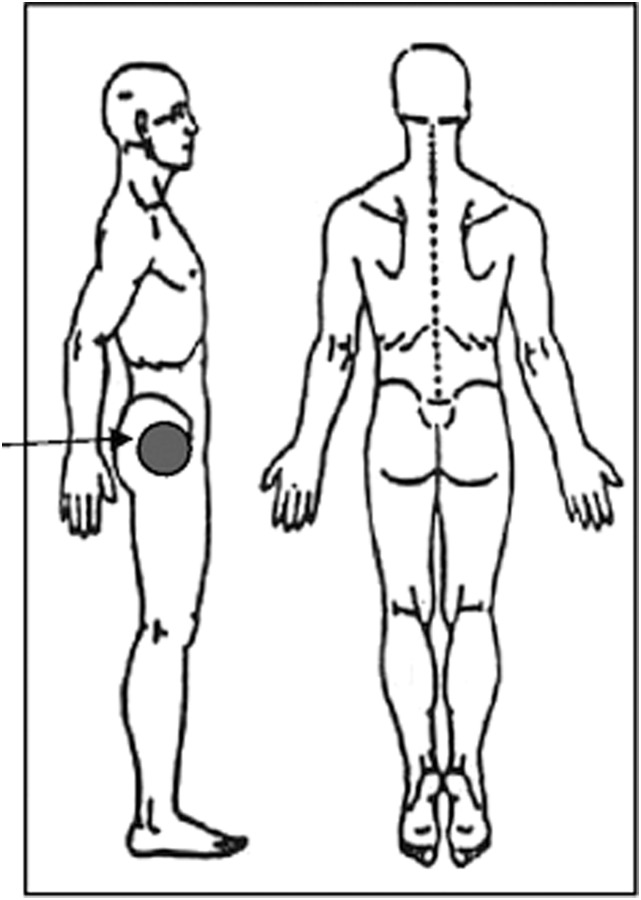
Figure 1.
Body Chart detailing the location of pain in the right lateral hip area (gray shaded region) at the time of initial evaluation.
Patient complaint: Right lateral hip pain; Location: approximately 5.08 cm proximal to the greater trochanter.
At the time of the evaluation, daily medication included Desogestrel‐Ethinyl Estradiol for birth control. A systems review for red flags was unremarkable for unexplained weight loss/gain, unexplained weakness, fatigue, malaise, fever, sweating, chills, nausea/vomiting, numbness/tingling, night pain, or difficulty sleeping. She reported no history of fractures, eating disorders, amenorrhea, or calcium deficiency. Family and medical history were also unremarkable. The subject had not received diagnostic imaging or previous treatment for her current complaints and reported no history of back, knee, and ankle injury/pain. Laboratory tests including complete blood count and basic metabolic count administered two weeks prior to her initial visit were within normal limits. She reported limited social use of alcohol but denied smoking or drug use. Her job as a fundraising administrator was unaffected per her report. The subject's goals included decreasing pain and returning to her workout activities as soon as possible to prepare for her upcoming wedding that would be in the next two months.
Clinical Impression #1
Based on the subjective history, the subject's right lateral hip pain was most likely due to overuse. She reported a change in running intensity prior to symptoms. In young adults, hip pain is often related to physical activity and overuse, and the inability to participate in the activity often leads these patients to seek medical attention.8 The authors were suspicious of the subject's chief complaints due to vague symptom description and aggravating factors. The subject consistently reported feeling a “twinge” and a deep ache in her right lateral hip that she randomly experienced throughout the day along with running and weight bearing activities, such as lunges and squats. This led the authors to suspect intra‐articular hip pathology, including but not limited to, femoral acetabular impingement (FAI), acetabular labral tears, and chondral and osseous lesions.
Intra‐articular hip pathology is often reported as lateral hip pain21 that can be worse with running and sitting.22 The results of research have demonstrated that the lack of groin pain helps rule out the potential for acetabular labral tear and FAI with a sensitivity ranging from 96‐100%.23 Further, the subject lacked clicking, catching, or snapping, which are often cues indicative of intra‐articular pathology and external snapping hip.24,25 Finally, individuals with hip joint stress fractures typically report a gradual onset of worsening hip, thigh, or groin pain that is described as a deep ache, aggravated by weight bearing, and partially relieved by rest.18,26
In those with hip joint pain, it is suggested that imaging be ordered to rule out serious pathology, such as cancer, osteonecrosis, or fracture.27 For other intra‐articular hip pathology, imaging is not recommended until a bout of conservative care is attempted.27 Due to the subject's young age and unremarkable past medical and family history, systemic pathology causing her hip pain was unlikely. Thus, in this subject, the authors hypothesized that imaging would be needed immediately only if a fracture was suspected after the physical examination. By restricting the physical activities that aggravated her right lateral hip pain, including running and certain weight bearing activities, the subject found symptom relief, which is consistent with hip pain of mechanical origin. The subject's report of pain and loss of function in the affected hip, which was severe enough to restrict her from physical activities, are also common complaints.8
However, as mentioned previously, several case reports have been published demonstrating misdiagnoses of GTPS.13,14 The subject's subjective history findings warranted a detailed objective examination of the subject's right hip joint in addition to screening the lumbar spine and sacroiliac joint to determine the source of symptoms and ensure proper diagnosis.
EXAMINATION
The subject had a mesomorphic body type with a height of 1.52 meters and weight of 55.45 kilograms (body mass index = 24 kg/m2) taken at her physician appointment two weeks prior to her initial PT evaluation. Posture assessment in standing revealed mild bilateral genu varum, but otherwise unremarkable. Gait assessment on level surface revealed increased bilateral trunk rotation and a positive Trendelenburg sign during right LE stance time without reproduction of the subject's symptoms. Functional task assessment on level surface included repetitive bilateral squats to 45 degrees of knee flexion and bilateral squat jumps to 45 and 90 degrees of knee flexion without reproduction of symptoms. Repetitive right single leg (SL) hops on a concrete surface reproduced her right lateral hip pain while repetitive right SL hops on a two‐inch foam surface were pain‐free. After, a right lateral lunge reproduced mild right lateral hip pain. Finally, deep palpatory pressure to the area approximately five centimeters proximal and posterior to the tip of the greater trochanter was severely tender and provoked the subject's symptoms. Additional physical examination findings are presented in Table 2. Namely, range of motion (ROM) of the lumbar spine and hip and special tests of the hip were negative for pain and were within normal limits.
Table 2.
Physical examination findings
| Objective Assessment | Findings |
|---|---|
| Single leg stance for 30 seconds28 | Able to perform and pain‐free bilaterally |
ROM:29
|
Within normal limits Within normal limits (External rotation 90 degrees bilaterally) Within normal limits Within normal limits |
|
One minute; stopped due to fatigue 4‐/5 bilaterally pain‐free 3+/5 R, 4‐/5 L, pain‐free 4‐/5 bilaterally, pain‐free 4‐/5 bilaterally, pain‐free Within normal limits Within normal limits |
| Joint mobility: | Within normal limits Within normal limits |
| Special tests
|
All negative All negative |
Palpation
|
All pain‐free |
ROM = range of motion
MMT = manual muscle test
R = right
L = left
FABER test = Flexion, abduction, external rotation
FADIR test = Flexion, adduction, internal rotation
Clinical Impression #2
The subject presented with multiple symptoms and signs that were suspicious for a stress fracture. The subject was a female who abruptly changed the frequency, duration, and intensity of her workout routine. Further, she reported a deep ache that gradually worsened in her hip, which was aggravated by high impact weight bearing activities and relieved by rest. These are all common in the presentation of those with stress fractures.18,26 Regarding the physical examination, the primary positive findings included a positive Trendelenburg sign, positive SL hop test on concrete surface (though negative hop test on foam surface), weakness of the right hip abductors, and significant palpable tenderness proximal and posterior to the greater trochanter that reproduced the subject's pain. A positive hop test, (report of pain when hopping on the injured leg), in conjunction with a Trendelenburg and gluteus medius weakness, increases the likelihood of an undisplaced stress fracture.16,38 The authors suspected that the concrete surface resulted in a higher load on the musculoskeletal system with higher ground reaction forces and peak load rates39 as well as poorer attenuation of pressure in comparison to the foam surface.40,41 Given the weakness of the gluteus medius in the involved leg, it would seem plausible to assume that the muscle would fatigue faster, decreasing the shock absorption capabilities of the musculoskeletal system18 increasing force transmitted to bone, and thus increasing risk of stress fracture.42,43,17 Further, fatigue of the gluteus medius has been shown to alter landing kinematics of the hip.44 The deep palpatory pain the subject experienced was similar to the findings in a subject with a femoral stress fracture.9 This may have been an area of increased hyperalgesia related to a fracture or palpation of a bursa that reproduced her pain.45 Interestingly, the subject had pain‐free ROM of the hip and all special tests about the hip were negative. According to Kovacevic et al,38 this is not uncommon in those with stress fractures around the hip.
According to Williams and Cohen,3 tenderness over the gluteus medius muscle and a positive Trendelenburg test, along with weakness of the hip abductors, may be indicative of gluteal tendinopathy or gluteus medius muscle dysfunction. Although these findings were present, the authors would have expected more pain when the subject landed on an unstable surface. Electromyographic analysis of the gluteus medius has shown increased activity during weight bearing activity on unstable surfaces.46 Thus, a diagnosis of gluteus medius muscle dysfunction was possible but seemed less likely.
There were multiple signs and symptoms that were not consistent with the initial physician diagnosis of trochanteric bursitis, or GTPS (Table 3). Although the subject was female and experienced lateral hip pain with running, her pain was not exacerbated by lying on the affected side, standing for prolonged periods of time, sitting with the affected leg crossed, or climbing stairs which usually occurs with GTPS.3,4 Upon physical examination, the subject also did not have distinct tenderness over the greater trochanter, pain at end‐range hip ROM, and pain with resisted hip abduction, all of which would have been indicative of GTPS.3 In addition, the subject did not have erythema, edema, or rubor that would suggest trochanteric bursitis.3,4 Therefore trochanteric bursitis and GTPS were less likely diagnoses. Based on the subjective and objective examination findings, concerns were discussed with the subject and referral back to her physician was considered.
Table 3.
Common risk factors, subjective and objective findings, and general intervention for greater trochanteric pain syndrome and hip stress fracture, and the findings for the subject of this case report
| GTPS | Hip Stress Fracture | Findings in this Case Report | |
|---|---|---|---|
| Risk factors | Female gender, obesity, knee osteoarthritis or knee pain, iliotibial band tenderness, and low back pain1, 40‐60 years of age3 | Training errors (high mileage, high intensity, abrupt change in training program, footwear, training surfaces), female gender, low bone mineral density, female athlete triad (disordered eating, amenorrhea, osteoporosis)17,18 | Abruptly changed frequency, duration, and intensity of workout routine, female gender |
| Pain description | Achiness, stiffness of lateral hip1 | Ache18 | Deep ache |
| Mechanism of injury | Often insidious, chronic, intermittent3,4 | Gradual onset, abrupt change of activity12 | Gradually worsening after abrupt change in workout |
| Aggravating factors | Lying on the affected side, prolonged standing, sitting cross‐legged, climbing stairs, running, high impact activities3,4 | Repetitive training, weight bearing,26 activity‐related pain18 | High impact weight bearing activities |
| Alleviating factors | Rest | Partially relieved by rest26 | Rest |
| Objective measures | Pain and/or weakness with resisted hip abduction3 | Weakness of right hip abductors | |
| Tenderness around greater trochanter3 | Focal tenderness, swelling, and erythema18 | Significant palpable tenderness proximal and posterior to greater trochanter | |
| Pain at end‐range hip ROM3 | Normal hip ROM38; pain at extreme end‐range internal or external rotation26 | Pain‐free hip ROM | |
| Trendelenburg sign3 | Antalgic gait18 | Positive Trendelenburg sign | |
| Positive heel tap or hop test18 | Positive SL hop test on concrete surface | ||
| Negative SL hop test on foam surface | |||
| Special tests | Positive FABER3 | Positive patellar‐pubic percussion test36,37 | Negative FADIR, FABER, hip scour |
| Negative patellar‐pubic percussion test | |||
| General intervention | Conservative treatment (nonsteroidal anti‐inflammatory drugs, ice, weight loss, physical therapy, behavior modification)3 | Varies from surgical intervention to relative rest17,18 | Conservative: patient to avoid running and high level LE plyometrics. Weight bearing as tolerated for four weeks |
GTPS = greater trochanteric pain syndrome; ROM = range of motion; SL = single legged; FABER test = flexion, abduction, external rotation; FADIR test = flexion, adduction, internal rotation; LE = lower extremity.
INTERVENTION
On the day of the initial evaluation, the subject was instructed to avoid provocative activities including running, jumping, hopping, lunging, and other plyometric activities to avoid further injury or joint complications. Further, the subject was educated to wear shoes with improved shock absorption, such as gym shoes, as often as possible during any weight bearing activity.
OUTCOME
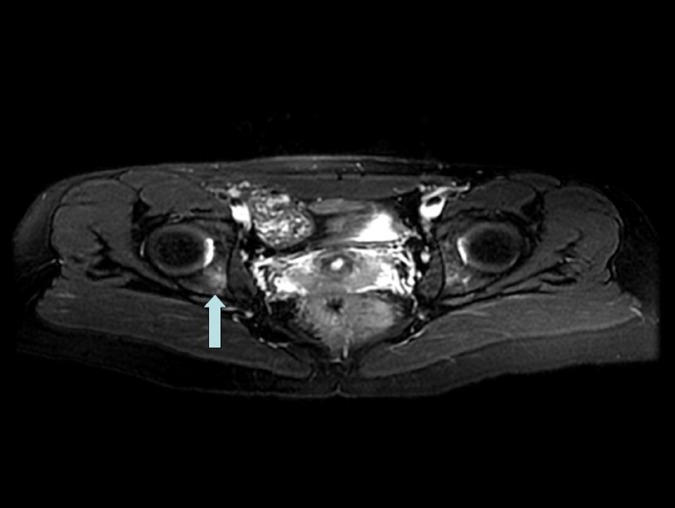
The referring physician was contacted by the primary author (J.I.L.), but the subject was unable to make an appointment with the physician. Four days after the initial examination, the subject was seen by PT and reported no change in symptoms; however, the subject had begun wearing gym shoes more frequently instead of heels. The primary and tertiary authors re‐assessed the subject's right lateral hip pain, and again, her symptoms were reproduced with right SL hopping on concrete surface and relieved when hopping on two‐inch foam surface. The subject was instructed to not participate in her normal workout routine and avoid running and high impact LE activities. The referring physician was again contacted. The subject was ultimately seen by her physician one week later. The authors recommended magnetic resonance imaging as it has demonstrated 95% sensitivity in detecting fractures47 and is considered by many to be the gold standard for diagnosing stress fractures.48,49 Radiographs of the hip and pelvis, however, were initially ordered and were unremarkable (Figure 2). The referring physician was contacted to discuss the need for further diagnostic imaging due to the sensitivity of plain radiographic film being as low as 15% in diagnosing stress fractures.9 A T2‐weighted MRI was ordered and revealed a focus of bony edema in the posterior acetabulum, just deep to the cortex of iliopectineal line which was suspicious for a stress fracture (Figure 3). A staff radiologist confirmed that there was marrow edema present in the acetabulum suggesting a stress injury.
Figure 2.
Radiograph of the right hip, unremarkable.
Figure 3.
MRI of bilateral hips (transverse cut) revealing a focus of bony edema in the posterior acetabulum, just deep to the cortex of the iliopectineal line, suspicious for a stress fracture.
The subject followed up with an orthopedic physician who gave her the diagnosis of acetabular stress fracture and advised her to avoid running and high level LE plyometrics. Since she was asymptomatic with walking and was to be married in a month, she was instructed to weight bear as tolerated (WBAT) for four weeks. One year later the subject reported that she had returned to her normal activity of running one to two times per week for 30 minutes without problems, but was no longer doing plyometrics. She was functioning throughout the day without pain.
DISCUSSION
This case described the clinical decisions and diagnostic process used by the physical therapist in a subject with lateral hip pain. The subject was originally referred to PT by her primary physician for trochanteric bursitis. However, several indicators suggested the diagnosis of a stress fracture in her hip region as a source of her symptoms and activity/participation restrictions. Namely, the subject was a female who abruptly increased her weight bearing activity intensity, frequency and duration. According to Nelson and Arciero18 one of the most common risk factors in the development of stress fractures is training errors, including high mileage, high intensity, or an abrupt change in the training program, which the subject in this case reported. The objective finding of a positive SL hop test on concrete surface and negative on foam also raised the authors’ suspicion of a stress fracture.
This subject had normal hip ROM, negative special tests of the hip including hip scour, FABER, FADIR, and a negative patellar‐pubic percussion test (PPPT). It has been noted that normal hip ROM in those with femoral stress fractures is not uncommon.38 The PPPT is an application of osteophony performed with the subject supine and the bell of the stethoscope placed on the pubic symphysis, held in place by the subject. The subject's legs are positioned symmetrically while the clinician stabilizes the patella. The clinician percusses the patella and compares the sounds from each leg for differences in pitch and loudness. In the case of bone pathology, the affected side will have a duller, diminished sound as compared to the unaffected side.50 The PPPT previously described by File36 has been shown to be 96% sensitive and 86% specific in detecting femoral neck fractures due to trauma.37 The negative results in the current subject are likely due to the fact that she had an acetabular stress fracture. Otherwise, the authors are unaware of any reliability or validity data on any of the above‐mentioned tests in regards to stress fractures about the hip.
There is a paucity of literature on the clinical presentation of acetabular stress fractures. In a study of 178 Navy and Marine Corps endurance athletes presenting with hip pain related to physical activity, only 12 subjects, or 6.7% had MRI findings consistent with acetabular stress fractures.43 The current subject presented similarly to a case report published by Thienpont and Simon51 in a 26 year old female professional ballet dancer diagnosed with an acetabular stress fracture. Both subjects of similar ages had right hip pain for a duration of three months, a positive right Trendelenburg test, and normal hip mobility. Though both subjects were successfully treated, the ballet dancer was instructed in six weeks partial weight bearing with crutches; the subject in the current case study remained WBAT for four weeks while reducing her high impact activities.
Common sites of stress fractures associated with physical activity are listed in Table 4 with the tibia and femoral shaft as the most common sites of stress injury in runners.52 Stress fractures of the acetabulum are extremely rare, but can occur in individuals who participate in repetitive training in which large forces pass through the hip joint.26 According to Datir et al,52 60% of stress injuries occur in the proximal femur and 40% occur in the pelvis. Among the stress injuries in the pelvis, 49% are located in the inferior pubic ramus, 41% in the sacrum, 4% in the superior pubic ramus, 4% in the iliac bone, and 1% in the acetabulum.52
Table 4.
Sites of stress fracture associated with physical activity
| Activity | Common sites of stress fracture |
|---|---|
| Long‐distance running | Femur: neck and shaft |
| Tibia: plateau and shaft | |
| Fibula | |
| Pubic ramus | |
| Military marching | Metatarsal |
| Calcaneus | |
| Sprinting | Navicular |
| Ballet | Pubic ramus |
| Femur: neck | |
| Tibia: shaft | |
| Fibula | |
| Metatarsal | |
| Sesamoid bones of the foot | |
| Pole vaulting | Talus |
| Gymnastics | Pars Interarticularis |
| Ulna | |
| Racquet sports/throwing | Pars Interarticularis |
| Humerus | |
| Olecranon | |
| Ulna | |
| Dancing | Metatarsal |
| Rowing/Golf | Ribs |
Adapted and used with permission from: Datir AP, Saini A, Connell A, Saifuddin A. Stress‐related bone injuries with emphasis on MRI. Clin Radiol. 2007;62:828‐83652, pg 829
Ultimately, to confirm suspicious findings indicative of a stress fracture, diagnostic imaging is recommended.52,53 Radiographs are usually the initial technique used to investigate stress fractures52,18 because they can detect periosteal bone reaction, cortical lucency, callus formation, or a fracture line that are typical findings of stress fractures.18 Upon suspicion of a stress fracture, the authors referred the subject back to her physician for further imaging to rule in/out a fracture. Radiographs were negative for fracture in this subject. However, radiographs have poor sensitivity with detection rates as low as 15%52 and may be normal even after several months since the onset of symptoms,18 which became apparent in this case. Williams et al43 report that the sensitivity of radiographs is 15‐28% in detecting pelvic stress fractures. Furthermore, only 50% of stress fractures may be evident on plain radiographs.18 Bone scintigraphy is more sensitive in detecting stress injuries than radiography, but has poor specificity and provides poor anatomic detail.8,52 Therefore, bone scintigraphy is commonly used to evaluate systemic symptoms indicative of bone and joint disease, rather than to evaluate a single joint.8 When radiographs revealed normal findings in our case, the referring physician was contacted by the primary author to determine the need for further diagnostic imaging, and ultimately, an MRI was ordered. MRI is considered the gold standard diagnostic tool for evaluating stress fractures.8,18,52 It is the most sensitive and specific imaging technique for detecting pathophysiological soft tissue, bone, and marrow changes associated with stress injuries about the hip.8,52 The high sensitivity of MRI also has the ability to detect early bone marrow edema, which is the diagnostic feature of the stress response.43,52
The importance of identifying stress fractures quickly is critical for appropriate management. While information is lacking in regards to acetabular stress fractures, authors have noted a delay in diagnosis of femoral neck stress fractures leading to a high complication rate.54,55,56 Thus, to ensure quick and safe recovery, appropriate diagnosis is necessary.
CONCLUSION
This case report describes the differential diagnosis and clinical decision making process used with an individual with undiagnosed acetabular stress fracture. Physical therapists should conduct a thorough examination to ensure appropriate management of the subject occurs. Although pelvic and acetabular stress fractures are rare, physical therapists should be aware of symptoms, signs, and risk factors that may suggest a stress fracture. In this case, the subject was a female who abruptly intensified a weight bearing workout routine and had pain with weight bearing activity, relieved by rest. Pain elicited by hopping on a firm surface, pain‐free hopping on a foam surface, a positive Trendelenburg sign, and weakness in hip abduction were key examination findings.
References
- 1.Segal NA Felson DT Torner JC, et al. Greater trochanteric pain syndrome: Epidemiology and associated factors. Arch Phys Med Rehabil. 2007;88:988‐992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lievense A Bierma‐Zeinstra S Schouten B, et al. Prognosis of trochanteric pain in primary care. British Journal of General Practice. 2005;55:199‐204. [PMC free article] [PubMed] [Google Scholar]
- 3.Williams BS Cohen SP. Greater trochanteric pain syndrome: A review of anatomy, diagnosis and treatment. Anesth Analg. 2009;108:1662‐1670. [DOI] [PubMed] [Google Scholar]
- 4.Tortolani PJ Carbone JJ Quartararo LG. Greater trochanteric pain syndrome in patients referred to orthopedic spine specialists. The Spine Journal. 2002;2:251‐254. [DOI] [PubMed] [Google Scholar]
- 5.Long SS Surrey DE Nazarian LN. Sonography of greater trochanteric pain syndrome and the rarity of primary bursitis. AJR Am J Roentgenol. 2013;201:1083‐1086. [DOI] [PubMed] [Google Scholar]
- 6.Adkins SB Figler RA. Hip pain in athletes. Am Fam Physician. 2000;61:2109‐2118. [PubMed] [Google Scholar]
- 7.Northmore‐Ball MD. Young adults with arthritic hips. BMJ. 1997;315:265–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Troum OM Crues JV. The young adult with hip pain: Diagnosis and medical treatment, circa 2004. Clin Orthop. 2004;418:9‐17. [DOI] [PubMed] [Google Scholar]
- 9.Gurney B Boissonnault WG Andrews R. Differential diagnosis of a femoral neck/head stress fracture. J Orthop Sports Phys Ther. 2006;36:80‐88. [DOI] [PubMed] [Google Scholar]
- 10.Martin HD. Clinical examination of the hip. Oper Tech Orthop. 2005;15:177‐181. [Google Scholar]
- 11.Goodman CC Snyder TEK. Differential Diagnosis for Physical Therapists: Screening for Referral. 4th ed. St. Louis, MO: Saunders; 2007:731‐767. [Google Scholar]
- 12.Klein GR Sharkey PF. Evaluation of hip pain in the young adult. Semin Arthro. 2005;16:2‐9. [Google Scholar]
- 13.Wakeshima Y Ellen MI. Atypical hip pain origin in a young athletic woman: A case report of giant cell carcinoma. Arch Phys Med Rehabil. 2001;81:1472‐1475. [DOI] [PubMed] [Google Scholar]
- 14.Jones DL Erhard RE. Diagnosis of trochanteric bursitis versus femoral neck stress fracture. Phys Ther. 1997;77:58‐67. [DOI] [PubMed] [Google Scholar]
- 15.Buist I Bredeweg SW Bessem B, et al. Incidence and risk factors of running‐related injuries during preparation for a 4‐mile recreational running event. Br J Sports Med. 2010. Jun;44(8):598‐604. [DOI] [PubMed] [Google Scholar]
- 16.Noesberger B Eichenberger AR. Overuse injuries of the hip and snapping hip syndrome. Oper Tech Sports Med. 1997;5:138‐142. [Google Scholar]
- 17.Zeni AI Street CC Dempsey RL, et al. Stress injury to the bone among women athletes. Phys Med Rehabil Clin N Am. 2000;11:929‐947. [PubMed] [Google Scholar]
- 18.Nelson BJ Arciero RA. Stress fractures in the female athlete. Sports Med Arthroscopy Rev. 2002;10:83‐90. [Google Scholar]
- 19.Ferreira‐Valente MA Pais‐Ribeiro JL Jensen MP. Validity of four pain intensity rating scales. Pain. 2011;152:2399‐2404. [DOI] [PubMed] [Google Scholar]
- 20.Binkley JM Stratford PW Lott SA, et al. The lower extremity functional scale (LEFS): scale development, measurement properties, and clinical application. Phys Ther. 1999;79:371‐383. [PubMed] [Google Scholar]
- 21.Lesher JM Dreyfuss P Hager N, et al. Hip joint pain referral patterns: a descriptive study. Pain Med. 2008;9:22‐5. [DOI] [PubMed] [Google Scholar]
- 22.Sankar WN Matheney TH Zaltz I. Femoroacetabular impingement: current concepts and controversies. Orthop Clin North Am. 2013;44:575–589. [DOI] [PubMed] [Google Scholar]
- 23.Keeney JA Peelle MW Jackson J, et al. Magnetic resonance arthrography versus arthroscopy in the evaluation of articular hip pathology. Clin Orthop Relat Res. 2004;429:163‐169. [DOI] [PubMed] [Google Scholar]
- 24.Byrd JW Snapping hip. Oper Tech Sports Med. 2005;13:46‐54. [Google Scholar]
- 25.Narvani AA Tsiridis E Kendall S, et al. A preliminary report on prevalence of acetabular labrum tears in sports patients with groin pain. Knee Surg Sports Traumatol Arthrosc. 2003;11:403‐408. [DOI] [PubMed] [Google Scholar]
- 26.O’hEireamhoin S McCarthy T. Fractures around the hip in athletes. The Open Sports Medicine Journal. 2010;4:58‐63. [Google Scholar]
- 27.Enseki K. Harris‐Hayes M White DM, et al. Nonarthritic hip joint pain: Clinical Practice Guidelines Linked to the International Classification of Functioning, Disability and Health From the Orthopaedic Section of the American Physical Therapy Association. J Orthop Sports Phys Ther. 2014;44(6):A1‐A32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lequesne M Mathieu P Vuillemin‐Bodaghi V, et al. Gluteal tendinopathy in refractory greater trochanter pain syndrome: diagnostic value of two clinical tests. Arthritis Rheum. 2008;59:241‐246. [DOI] [PubMed] [Google Scholar]
- 29.Norkin CC White DJ. Measurement of Joint Motion: A Guide to Goniometry. 3rd Ed. Philadelphia, PA: F.A. Davis Company:2003. [Google Scholar]
- 30.Reese NB. Muscle and Sensory Testing. 2nd Ed. Saint Louis, MO:Elsevier:2005. [Google Scholar]
- 31.Maitland G Hengleveld E Banks K, et al. Maitland’s Vertebral Manipulation. 7th Ed. New York, NY: Elsevier;2005. [Google Scholar]
- 32.Hengleveld E Banks K. Maitland’s Peripheral Manipulation. 4th Ed. New York, NY: Elsevier; 2005. [Google Scholar]
- 33.Laslett M Aprill CN McDonald B, et al. Diagnosis of Sacroiliac Joint Pain: Validity of individual provocation tests and composites of tests. Man Ther. 2005;10; 207–218. [DOI] [PubMed] [Google Scholar]
- 34.van der Wurff P Buijs EJ Groen GJ. A multitest regimen of pain provocation tests as an aid to reduce unnecessary minimally invasive sacroiliac joint procedures. Arch Phys Med Rehabil. 2006;87:10‐4. [DOI] [PubMed] [Google Scholar]
- 35.Magee DJ. Orthopedic Physical Therapy Assessment. 5th Ed. Saint Louis, MO:Saunders:2008. [Google Scholar]
- 36.File P Wood JP Kreplick LW. Diagnosis of hip fracture by the auscultatory percussion technique. Am J Emerg Med. 1998;16:173‐176. [DOI] [PubMed] [Google Scholar]
- 37.Tiru M Goh SH Low BY. Use of percussion as a screening tool in the diagnosis of occult hip fractures. Singapore Med J. 2002;43:467‐469. [PubMed] [Google Scholar]
- 38.Kovacevic D Mariscalco M Goodwin RC. Injuries about the hip in the adolescent athlete. Sports Med Arthrosc. 2011;19:64‐74. [DOI] [PubMed] [Google Scholar]
- 39.Ferris DP Liang K Farley CT. Runners adjust leg stiffness for their first step on a new running surface. J Biomech. 1999;32:787–794. [DOI] [PubMed] [Google Scholar]
- 40.Tessutti V Ribeiro AP Trombini‐Souza F, et al. Attenuation of foot pressure during running on four different surfaces: asphalt, concrete, rubber, and natural grass. J Sports Sci. 2012;30:1545‐50. [DOI] [PubMed] [Google Scholar]
- 41.Wang L Hong Y Li JX, et al. Comparison of plantar loads during running on different overground surfaces. Res Sports Med. 2012;20:75‐85. [DOI] [PubMed] [Google Scholar]
- 42.Anderson M Greenspan A. Stress fractures. Radiology. 1996;199:1–12. [DOI] [PubMed] [Google Scholar]
- 43.Williams TR Puckett ML Denison G, et al. Acetabular stress fractures in military endurance athletes and recruits: Incidence and MRI and scintigraphic findings. Skeletal Radiol. 2002;31:277‐281. [DOI] [PubMed] [Google Scholar]
- 44.Jacobs CA Uhl TL Mattacola CG, et al. Hip abductor function and lower extremity landing kinematics: Sex differences. J Athl Train. 2007;42:76‐83. [PMC free article] [PubMed] [Google Scholar]
- 45.Woodley SJ Mercer SR Nicholson HD. Morphology of the bursae associated with the greater trochanter of the femur. J Bone Joint Surg Am. 2008;90:284‐294. [DOI] [PubMed] [Google Scholar]
- 46.Krause DA Jacobs RS Pilger KE, et al. Electromyographic analysis of the gluteus medius in five weight‐bearing exercises. Strength Cond Res. 2009;23:2689‐94. [DOI] [PubMed] [Google Scholar]
- 47.Nachtrab O Cassar‐Pullicino VN Lalam R, et al. Role of MRI in hip fractures, including stress fractures, occult fractures, avulsion fractures. Eur J Radiol. 2012;81:3813‐23. [DOI] [PubMed] [Google Scholar]
- 48.Daffner RH Pavlov H. Stress fractures: Current concepts. AJR Am J Roentgenol. 1992;159:245‐252. [DOI] [PubMed] [Google Scholar]
- 49.De Paulis F Cacchio A Michelini O, et al. Sports injuries in the pelvis and hip: Diagnostic imaging. Eur J Radiol. 1998;27:S49‐59. [DOI] [PubMed] [Google Scholar]
- 50.Borgerding LJ Kikillus PJ Boissonnault WG. Use of the patellar‐pubic percussion test in the diagnosis and management of a patient with a non‐displaced hip fracture. J Man Manip Ther. 2007;15:E78‐E84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Thienpont E Simon JP. Stress fracture of the acetabulum in a ballet dancer: A case report. Acta Orthop. Belg. 2005;71:740‐742. [PubMed] [Google Scholar]
- 52.Datir AP Saini A Connell A, et al. Stress‐related bone injuries with emphasis on MRI. Clin Radiol. 2007;62:828‐836. [DOI] [PubMed] [Google Scholar]
- 53.Margo K Drezner J Motzkin D. Evaluation and management of hip pain: An algorithmic approach. J Fam Pract. 2003;52:607‐617. [PubMed] [Google Scholar]
- 54.Boden BP Osbahr DC. High‐risk stress fractures: Evaluation and treatment. J Am Acad Orthop Surg. 2000;8:344‐353. [DOI] [PubMed] [Google Scholar]
- 55.Clough TM. Femoral neck stress fracture: The importance of clinical suspicion and early review. Br J Sports Med. 2002;36:308‐309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Johansson C Ekenman I Tornkvist H, et al. Stress fractures of the femoral neck in athletes: The consequence of a delay in diagnosis. Am J Sports Med. 1990;18:524‐528. [DOI] [PubMed] [Google Scholar]