Abstract
Context and objective:
Evidence that bacteria in the human gut may influence nutrient metabolism is accumulating. We investigated whether use of antibiotics influences the risk of developing type 2 diabetes and whether the effect can be attributed to specific types of antibiotics.
Methods:
We conducted a population-based case-control study of incident type 2 diabetes cases in Denmark (population 5.6 million) between January 1, 2000, and December 31, 2012. Data from the Danish National Registry of Patients, the Danish National Prescription Registry, and the Danish Person Registry were combined.
Results:
The odds ratio (OR) associating type 2 diabetes with exposure to antibiotics of any type was 1.53 (95% confidence interval 1.50–1.55) with redemption of more than or equal to 5 versus 0–1 prescriptions. Although no individual group of antibiotics was specifically associated with type 2 diabetes risk, slightly higher ORs for type 2 diabetes were seen with narrow-spectrum and bactericidal antibiotics (OR 1.55 and 1.48) compared to broad-spectrum and bacteriostatic types of antibiotics (OR 1.31 and 1.39), respectively. A clear dose-response effect was seen with increasing cumulative load of antibiotics. The increased use of antibiotics in patients with type 2 diabetes was found up to 15 years before diagnosis of type 2 diabetes as well as after the diagnosis.
Conclusions:
Our results could support the possibility that antibiotics exposure increases type 2 diabetes risk. However, the findings may also represent an increased demand for antibiotics from increased risk of infections in patients with yet-undiagnosed diabetes.
The human gut is populated by a dense community of microbes, the gut microbiota, that many-fold outnumbers our eukaryotic cell count and provides the host with an enormous complimentary microbial gene set, the gut microbiome (1). Several metabolic disease states such as obesity and type 2 diabetes have been linked with alterations in the microbiota composition and function (2, 3), and in animal models, it has been demonstrated that the microbiota actively contributes to a number of host metabolic pathways such as energy harvesting potential, regulation of gut hormone secretion, and nutrient storage (4–6).
Antibiotics cause marked alterations in the human gut microbiota with stereotypic declines and expansions in the abundance of certain taxa and incomplete recovery to the initial composition in some individuals (7–9). In observational studies, exposure to antibiotics has been linked with development of obesity (10–12), and specific antibiotics have been associated with glucose homeostasis disturbances in patients with type 2 diabetes (13). Recently, an observational study from the United Kingdom reported an increased risk of diabetes following exposure to any of five commonly prescribed antibiotics, also showing a clear dose-response effect. At the same time, patients with type 2 diabetes had increased incidence of infections, raising the possibility of confounding by indication.
We conducted a nationwide case-control study to investigate whether use of antibiotics influences the risk of developing type 2 diabetes and, if so, if the effect can be attributed to individual types of antibiotics, individual groups of antibiotics, or the number of antibiotics courses.
Materials and Methods
The analysis was conducted as a nationwide case-control study of incident cases of type 2 diabetes in Denmark (population 5.6 million) between January 1, 2000, and December 31, 2012. Virtually all medical care in Denmark is provided by public health authorities, whereby the Danish health registries allow true population-based studies, covering all inhabitants of Denmark.
Data sources.
We used data from three sources: the Danish National Registry of Patients, the Danish National Prescription Registry, and the Danish Person Registry.
The Danish National Registry of Patients (14) contains data on all secondary care contacts in Denmark since 1977. From 1995, outpatient diagnoses have been included systematically. Discharge diagnoses are coded according to International Classification of Diseases, eighth revision (ICD-8), from 1977 to 1993 and ICD-10 since 1994.
The Danish National Prescription Registry (15) contains data on all prescription drugs redeemed by Danish citizens since 1995. Prescription data include the Central Person Registry number, date of dispensing, the substance, brand name, and quantity. The dosing instruction and the indication for prescribing are not recorded. Drugs are categorized according to the Anatomical Therapeutic Chemical (ATC) code, a hierarchical classification system developed by the World Health Organization for purposes of drug use statistics (16). The quantity for each prescription is expressed by the defined daily dose (DDD) measure, also developed by the World Health Organization (16).
The Danish Person Registry (17) contains data on vital status (date of death) and migrations in and out of Denmark, which allowed us to extract controls and to keep track of all subjects.
All data sources were linked by use of the Central Person Registry number, a unique identifier assigned to all Danish citizens since 1968 that encodes gender and date of birth (14). All linkage occurred within Statistics Denmark, a governmental institution that collects and maintains electronic records for a broad spectrum of statistical and scientific purposes. Further information on the Danish registries can be found elsewhere (18).
Cases.
Because many type 2 diabetes patients are handled in the primary care system and only hospital diagnoses of type 2 diabetes are available for research purposes, we could not identify cases based solely on diagnoses. In particular, the timing of type 2 diabetes onset would be artificially delayed. Instead, cases were defined by a first-ever prescription of a noninsulin glucose-lowering agent (ATC A10B), using the date of the filling as the index date. To ensure consistency in the timing of the diabetes diagnosis and treatment of cases, we excluded cases that, before the index date, had a diabetes diagnosis (ICD-10 codes E10, E11, E12, E13, E14, and H360). We further excluded patients who were not inhabitants in Denmark at the index date or who immigrated to Denmark less than 5 years before their index date. Last, we excluded cases with chronic pancreatitis (ICD10 DK86*), pancreatic cancer (ICD10 DC25*), or polycystic ovary syndrome (ICD10 DE282).
With this inclusion strategy, we included most patients diagnosed with type 2 diabetes in Denmark in the study period, although we excluded patients on insulin monotherapy (assumed to account for less than 5% of Danish patients with type 2 diabetes (19)).
Controls.
Controls were extracted by use of a risk-set sampling strategy. For each case, we selected eight controls randomly among all Danish citizens, matching by gender and birth year, and assigning an index date identical to the corresponding case. Subsequently, we excluded those controls that fulfilled any of the exclusion criteria described under cases including type 2 diabetes diagnosis before their index date. We allowed subjects to be elected as controls before they became cases and that subjects could be elected as controls more than once. Thereby, the generated odds ratio (OR) is an unbiased estimate of the incidence rate ratio that would have emerged from a cohort study based on the same source population (20).
Exposure definition.
We obtained information on use of all systemic antibiotics (ATC, J01*, or P01AB01) for the cohort between January 1, 1995, and July 1, 2012. Antibiotics were classified into narrow-spectrum or broad-spectrum and bactericidal or bacteriostatic as described in the Supplemental Material.
Antibiotic prescriptions that were redeemed within 6 months before the index date where disregarded in the analysis to avoid reverse causation bias; a prediabetic condition could be exacerbated during infectious disease, early diabetes might cause infections before it was diagnosed, or first symptoms of undiagnosed type 2 diabetes could lead to antibiotic treatment for example by being misinterpreted as an infection.
Exposure was quantified according to number of antibiotic courses before the index date, three different categories were defined; 0–1 antibiotic courses (reference), 2–4 antibiotic courses or ≥5 antibiotic courses. Filling a prescription on the same antibiotic within 20 days of the first use was considered as belonging to the same course.
Data analysis.
The analysis conformed to a conventional matched case-control study. The crude and adjusted ORs for developing type 2 diabetes associated with antibiotic exposure were estimated using conditional logistic regression, controlling for potential confounders.
Our primary aim was to test if there was an increased OR of type 2 diabetes with increasing levels of antibiotic exposure, with and without adjustment for potential confounders. For all antibiotics, we calculated the exposure odds for a cumulative exposure of 2–4 versus 0–1 prescriptions and for ≥5 vs 0–1 prescriptions. As an explorative analysis, we also calculated the exposure odds for 2–4, 5–8, 9–15, 16–24 and ≥25 prescriptions in order not to overlook a potential dose-response effect outside of common exposure levels. These analyses were conducted for narrow-spectrum and broad-spectrum antibiotics, and bactericidal and for bacteriostatic antibiotics separately (classification listed in the Supplemental Material).
Variables included in our regression model as potential confounders were disposable income (categorized in four groups as described in Table 1), Charlson index of comorbidity (none = 0 points, low = 1 point, or high ≥2 points) (21), and exposure to certain drug classes known to influence the risk of type 2 diabetes. Exposure to a given drug class included as a confounder was defined as having filled prescriptions for more than 500 DDD (except 30 DDD of glucocorticoids) before the index date. The following drug classes were included: thiazide diuretics, glucocorticoids, oral contraceptives, statins, calcineurin inhibitors, and antipsychotics. As for exposure to antibiotics, only diagnoses or prescriptions occurring earlier than 6 months before the index date were included. Age and gender were not included in the regression because they were handled by the matching procedure.
Table 1.
Baseline Characteristics of Cases With Type 2 Diabetes and Control Subjects Free of Diabetes Matched by Gender and Age
| Cases | Controls | |
|---|---|---|
| All | (n = 170 504) | (n = 1 364 007) |
| Men | 89 237 (52.3%) | 713 887 (52.3%) |
| Women | 81 267 (47.7%) | 650 120 (47.7%) |
| Age (median, IQR) | 62 (51–71) | 62 (51–71) |
| Exposure to antibiotics (any) | ||
| 0–1 redemptions | 36 314 (21.3%) | 376 550 (27.6%) |
| 2–4 redemptions | 47 184 (27.7%) | 409 901 (30.1%) |
| ≥5 redemptions | 87 006 (51.0%) | 577 556 (42.3%) |
| Income | ||
| <24 444 USD | 90 015 (52.8%) | 602 291 (44.2%) |
| 24 444–44 069 USD | 69 089 (40.5%) | 615 345 (45.1%) |
| 44 070–66 105 USD | 8384 (4.9%) | 108 334 (7.9%) |
| ≥66 105 USD | 2826 (1.7%) | 37 762 (2.8%) |
| Unknown | 190 (0.1%) | 275 (0.0%) |
| Drug exposure | ||
| Glucocorticoids | 24 821 (14.6%) | 161 228 (11.8%) |
| Oral contraceptives | 13 923 (8.2%) | 121 745 (8.9%) |
| Statins | 31 777 (18.6%) | 125 479 (9.2%) |
| Antipsychotics | 4179 (2.5%) | 15 712 (1.2%) |
| Thiazides | 14 857 (8.7%) | 60 006 (4.4%) |
| Charlson index | ||
| None (0) | 112 500 (66.0%) | 995 998 (73.0%) |
| Low (1) | 29 899 (17.5%) | 183 867 (13.5%) |
| High (≥2) | 28 105 (16.5%) | 184 142 (13.5%) |
Abbreviation: IQR, interquartile range.
As sensitivity analyses we 1) considered only cases who redeemed two or more prescriptions of noninsulin antidiabetics (ATC codes A10B*), 2) considered only cases that received a type 2 diabetes diagnosis (ICD10 DE11) in the Danish National Registry of Patients following redemption of one or more prescriptions of noninsulin antidiabetics, 3) considered only antibiotic prescriptions occurring within the past 5 years of the index date (to detect an effect of variation in the available observation time), and 4) disregarded all antibiotic prescriptions occurring within the first 0–24 months (in 1-month intervals) from the index date.
Approval.
The study was approved by the scientific board of Statistics Denmark. Approval from an ethics committee is not required according to Danish law (22).
Results
Between January 1 and December 31, 2012, we identified 231 745 incident users of glucose-lowering agents. Following exclusions, we had 170 504 cases that were matched to 1 364 008 control persons without diabetes (52.3% males, median age 62 years, interquartile range 51–71) Supplemental Figure 1).
Patients with type 2 diabetes generally had slightly lower income, higher exposure to diabetogenic drugs, and higher Charlson index than the age- and gender-matched controls from the background population (Table 1).
Patients with type 2 diabetes redeemed on average 0.8 prescriptions on antibiotics per year compared to 0.5 prescriptions per year among controls. Only 15 809 (9%) of cases and 180 653 (13%) of controls did not redeem any antibiotics before their index date.
Comparing having filled 2–4 prescriptions for antibiotics of any type to having filled 0–1 prescriptions for antibiotics, we found an adjusted OR of 1.21 (95% confidence interval [CI] 1.19–1.23) for type 2 diabetes, whereas redemption of prescriptions was associated with an OR of 1.53 (95% CI 1.50–1.55) for type 2 diabetes. Slightly higher ORs were found for narrow-spectrum and bactericidal antibiotics compared with broad-spectrum and bacteriostatic antibiotics, respectively (Table 2).
Table 2.
Crude and Adjusted ORs (95% CI) for Type 2 Diabetes According to Antibiotic Exposure (Categorized in Types of Antibiotics) Before initiation of Type 2 Diabetes Treatment
| Crude |
Adjusted |
|||
|---|---|---|---|---|
| Type of Antibiotics | 2–4 | ≥5 | 2–4 | ≥5 |
| Any antibiotic | 1.23 (1.21–1.25) | 1.65 (1.63–1.67) | 1.21 (1.19–1.23) | 1.53 (1.50–1.55) |
| Narrow-spectrum | 1.24 (1.23–1.26) | 1.68 (1.65–1.70) | 1.22 (1.20–1.23) | 1.55 (1.53–1.57) |
| Broad-spectrum | 1.24 (1.23–1.26) | 1.45 (1.43–1.48) | 1.18 (1.16–1.20) | 1.31 (1.29–1.34) |
| Bactericidal | 1.21 (1.20–1.23) | 1.61 (1.59–1.63) | 1.18 (1.17–1.20) | 1.48 (1.46–1.50) |
| Bacteriostatic | 1.25 (1.24–1.27) | 1.49 (1.47–1.52) | 1.20 (1.19–1.22) | 1.39 (1.36–1.41) |
Abbreviations: c, crude; OR1, the OR for type 2 diabetes with redemption of two to four antibiotic prescriptions compared with zero to one redemptions; OR2, the odds for type 2 diabetes with redemption of five or more compared with zero to one antibiotic prescriptions.
The most commonly redeemed antibiotics were β-lactamase sensitive penicillins followed by macrolides (ATC J01FA) and penicillins with extended spectrum (data not shown).
We found increased ORs for all groups of antibiotics except for clindamycin. Glycopeptides were very infrequently prescribed in primary care and therefore an OR could not be calculated for this drug (Table 3).
Table 3.
Adjusted OR (with 95% CI) for Type 2 Diabetes According to Antibiotic Exposure (Categorized in ATC Code Groups) Before Initiation of Type 2 Diabetes Treatment
| Group of Antibiotics | OR1 | OR2 |
|---|---|---|
| β-lactamase sensitive penicillins (J01CE) | 1.19 (1.18–1.21) | 1.51 (1.49–1.54) |
| β-lactamase-resistant penicillins (J01CF) | 1.35 (1.32–1.38) | 1.61 (1.52–1.70) |
| Trimethoprim and derivatives (J01EA) | 1.19 (1.13–1.25) | 1.26 (1.17–1.36) |
| Short-acting sulfonamides (J01EB) | 1.15 (1.13–1.17) | 1.16 (1.12–1.20) |
| Macrolides (J01FA) | 1.25 (1.23–1.27) | 1.49 (1.46–1.52) |
| Steroid antibacterials (fusidic acid) (J01XC) | 1.64 (1.36–1.98) | 1.62 (1.00–2.62) |
| Nitrofurantoin derivatives (J01XE) | 1.16 (1.11–1.21) | 1.30 (1.22–1.39) |
| Penicillins with extended spectrum (J01CA) | 1.19 (1.17–1.21) | 1.31 (1.28–1.34) |
| Tetracyclines (J01AA) | 1.17 (1.14–1.21) | 1.19 (1.13–1.25) |
| Combinations of penicillins including β-lactamase inhibitors (J01CR) | 1.22 (1.13–1.33) | 1.41 (1.19–1.67) |
| Fluoroquinolones (J01MA) | 1.16 (1.13–1.20) | 1.23 (1.15–1.32) |
| Metronidazole (J01XD01 & P01AB01) | 1.13 (1.09–1.16) | 1.12 (1.02–1.23) |
| Clindamycin (J01FF) | 1.18 (0.97–1.44) | 0.88 (0.45–1.72) |
| Cephalosporins (J01DB, J01DC, and J01DD) | 1.24 (1.01–1.53) | 1.28 (0.74–2.20) |
| Comb. of sulfonamides and trimethoprim (J01EE) | 1.18 (1.03–1.34) | 0.95 (0.74–1.22) |
| Linezolid (J01XX) | 1.29 (1.06–1.57) | 1.46 (1.24–1.72) |
Abbreviations: ATC, Anatomical Therapeutic Chemical; OR1, the OR for type 2 diabetes with redemption of 2–4 compared with 0–1 prescriptions of the specific antibiotic group; OR2, the odds for type 2 diabetes with redemption of ≥5 compared with 0–1 prescriptions of the specific antibiotic group.
There was a dose-response relation between exposure to antibiotics and type 2 diabetes for all types of antibiotics, although the dose-response relationship was slightly stronger for narrow-spectrum and bactericidal antibiotics compared to broad-spectrum and bacteriostatic types, respectively. The OR for type 2 diabetes increased almost linearly with the exposure to antibiotics, also outside the common exposure window as shown in Figure 1.
Figure 1.
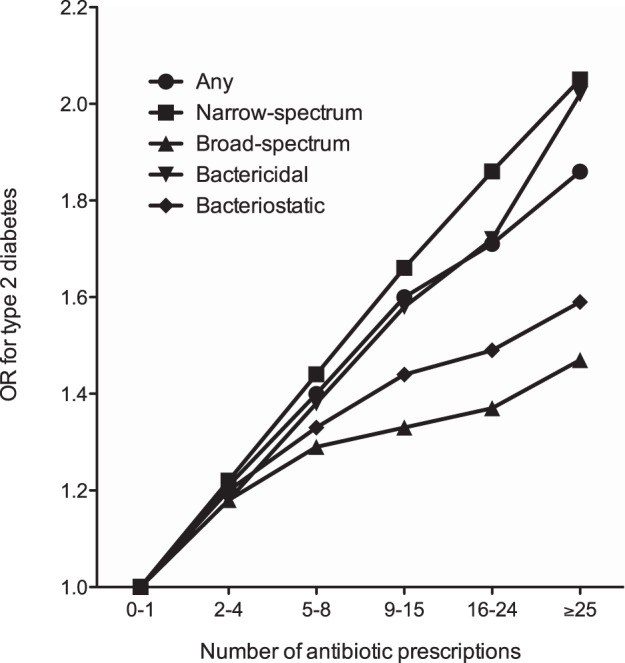
OR for type 2 diabetes according to the number of antibiotics prescriptions prior to the initiation of treatment for type 2 diabetes.
The observed associations between antibiotic exposure and type 2 diabetes risk were identical when stratifying by age, gender, and observation periods (data not shown). Also, when considering only antibiotic exposure occurring within the past 5 years prior to the index date, the associations were unchanged (Supplemental Tables 1–3). The observed associations were confirmed in sensitivity analyses using more strict criteria to define cases (ie, those receiving a hospital diagnosis of type 2 diabetes or those filling two or more prescriptions for antidiabetics) (supplemental tables).
In post hoc analyses, we found a steep increase in OR for type 2 diabetes with increasing exposure to narrow-spectrum antibiotics when the exposure to broad-spectrum antibiotics was held fixed. In contrast, there was a relatively unchanged OR for type 2 diabetes with increasing exposure to broad-spectrum antibiotics when exposure to narrow-spectrum antibiotics was fixed (Table 4).
Table 4.
OR (with 95% CI) for Type 2 Diabetes According to the Number of Exposures to Broad-Spectrum and/or Narrow-Spectrum Antibiotics Before Initiation of Type 2 Diabetes Treatment
| Broad Spectrum (0–1) | Broad Spectrum (2–4) | Broad Spectrum (≥5) | |
|---|---|---|---|
| Narrow spectrum (0–1) | (Reference) | 1.14 (1.09–1.19) | 1.12 (1.01–1.25) |
| Narrow spectrum (2–4) | 1.22 (1.20–1.24) | 1.27 (1.23–1.31) | 1.24 (1.17–1.32) |
| Narrow spectrum (≥5) | 1.52 (1.49–1.55) | 1.59 (1.55–1.63) | 1.64 (1.59–1.69) |
When exposure to narrow-spectrum antibiotics was held fixed, a relatively unchanged OR for type 2 diabetes was seen with increasing exposure to broad-spectrum antibiotics.
The increased exposure to antibiotics was observed both 5 years before and 5 years after the type 2 diabetes index date for cases, with a small but consistent increase in relative exposure rate (between cases and controls) in the year immediately before and after the index date (Supplemental Figure 2).
In further analyses, we found that the increased exposure to antibiotics among cases was observed up to 15 years before the type 2 diabetes index date with a relative exposure rate (cases versus controls) that slowly but consistently increased from 1.20 15 years before the index date to 1.35 in the year prior to the index date (Figure 2). A similar pattern was seen when considering broad-spectrum, narrow-spectrum, bactericidal, and bacteriostatic antibiotics separately (data not shown).
Figure 2.
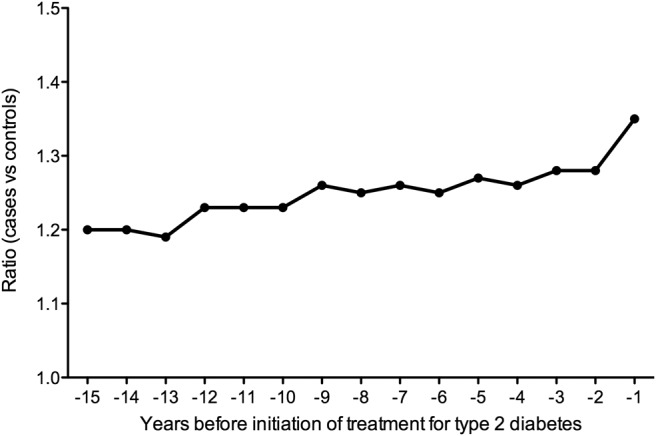
Proportional ratio of antibiotics (any) use in cases versus controls in the 15 years before the initiation of treatment for type 2 diabetes. Results are only for cases with an index date between 2010 and 2012.
Discussion
In this nationwide register-based study, we find an increased OR for risk of type 2 diabetes with increasing exposure to antibiotics. A slightly stronger association was seen with bactericidal and narrow-spectrum antibiotics compared to bacteriostatic and broad-spectrum groups, although the OR for type 2 diabetes risk with individual types of antibiotics was generally found to be homogenous. Importantly, the increased use of antibiotics among patients with type 2 diabetes was found after the time of type 2 diabetes onset as well as for the 15 years leading up to this.
As for any observational study, the impact of bias and confounding must be considered carefully. We used the Danish Person Registry Number as a unique linkage to combine data from the Danish National Prescription Registry, the Danish National Registry of Patients, and the Danish Person Registry. This allowed us to identify all Danish citizens who started treatment with a noninsulin glucose-lowering agent during 2000–2012 and compare the antibiotic exposure pattern in this population with an age- and gender-matched control population free of diabetes for a period of up to 17 years before type 2 diabetes index date. The combined data from the registers allowed adjustment for differences in income, Charlson index of comorbidity, and exposure to diabetogenic drugs in both the case and the control group. However, we did not have access to data on anthropometric measures such as body mass index, blood sample results, or assessments of the gut microbiota composition in these individuals that could provide hints toward the mechanisms underlying our observations. Moreover, we were unable to study the influence of antibiotic prescriptions occurring in the early life of our population (median age 62 years) because the Danish National Prescription Registry did not provide data on drugs prescriptions before 1995.
An inherent difficulty in observational studies of type 2 diabetes lies in the definition of type 2 diabetes onset. It has been estimated that at least 40% of patients with type 2 diabetes in Denmark are undiagnosed (23), and before diagnosis, patients may have had impaired glucose tolerance, prediabetes, or as-yet undiagnosed type 2 diabetes for several years (24). In a recent register study from Denmark, around 26% of Danish patients with type 2 diabetes did not receive glucose-lowering agents in the first year following diagnosis (19). These patients were only included in our study if they later and within the study period redeemed a prescription on a noninsulin glucose-lowering agent. As a consequence, the index date for this subgroup could be falsely delayed in comparison to the time of diagnosis.
Related to the issue of index time definition and the possible delay in the time to diagnosis of type 2 diabetes is the risk of confounding by indication. As discussed later, it is commonly accepted that type 2 diabetes is a risk factor for certain infections. In addition, an increased susceptibility to infections has been demonstrated in obese patients (25). The prevalence of obesity is increased in patients with type 2 diabetes but also in patients with prediabetes. Any difference in susceptibility to infection between the case and the control group would bias our results. To minimize this bias, we first excluded all antibiotic prescriptions filled less than 6 months before the index date. When this period was extended to 3 years before the index date, it had limited effect on the OR (decreased from 1.52 [95% CI 1.50–1.55] to 1.43 [95% CI 1.41–1.46]). Finally, post hoc analyses revealed that the antibiotic exposure was increased among cases up to 15 years before the index date, which we find unlikely to be caused by increased susceptibility to infections resulting from, for example, prediabetes.
Recently, an observational study was published based on United Kingdom primary care patients. This study used a general practitioner-based database to study the antibiotic exposure in patients diagnosed with diabetes (n = 208 002) and matched controls (n = 815 576) free of diabetes between 1995 and 2013 with a median follow-up duration of 5.5 years (26). In this study, there was also an homogenously increased OR for diabetes (combined type 1 diabetes and type 2 diabetes in main analysis) risk with increasing exposure to any one of five commonly prescribed antibiotics: penicillins, cephalosporins, macrolides, quinolones, and tetracycline/sulfamethiazole (the latter two were analyzed as one group). The ORs for diabetes risk were similar to the ones observed in our study, although the OR with penicillin was lower than in our study: OR 1.23 (95% CI 1.05–1.11) with > 5 versus 0 prescriptions for penicillins.
Because different groups of bacteria may have either a positive or negative impact on host energy homeostasis and glucose metabolism, our primary aim of this study was to test the possibility that different antibiotic groups targeting specific gut bacteria classes could induce different effects on the risk for development of type 2 diabetes. Supporting this hypothesis, a previous interventional study found decreased insulin sensitivity following 1 week of treatment with vancomycin, but not ampicillin, in a group of obese males with the metabolic syndrome (27). In addition, increases in body weight were reported following exposure to vancomycin, but not following exposure to other antibiotics in an observational study. Unfortunately, because of very few redemptions on glycopeptides in our population, we were unable to assess the risk of type 2 diabetes associated with vancomycin exposure. However, the uniformly increased ORs for type 2 diabetes between groups of antibiotics in our study do not support the idea of one or a few antibiotics with particularly strong metabolic side effects.
There are two competing interpretations of our findings: 1) patients with type 2 diabetes are more prone to develop infections many years before they become diagnosed with type 2 diabetes and therefore have increased demand for antibiotics and 2) antibiotics increase the risk of type 2 diabetes.
In support for the first interpretation, we found an essentially unchanged exposure rate in cases versus controls before and after the type 2 diabetes index date. Boursi et al found higher incidence of urinary tract infections, skin infections, and respiratory tract infections in cases with type 2 diabetes compared with controls (26), and higher risk of infections has previously been reported in patients with uncontrolled diabetes compared with controls free of diabetes (28). Moreover, obesity, which often precedes development of type 2 diabetes, is suggested to increase risk of infection (25). Etiologically, complications of type 2 diabetes such as sensory peripheral neuropathy, vascular insufficiency, and autonomic neuropathy can all increase susceptibility to infection (29, 30), and hyperglycemia has been suggested to impair immune function (31). Because some of our patients may have had undiagnosed diabetes or hyperglycemia for an uncertain period before the index date and because the prevalence of obesity within the case group could be increased, we would expect a slightly increased demand for antibiotics treatment in the case group also prior to the index date.
In support of the second interpretation, there is now mounting evidence from rodent models suggesting that antibiotics may drive changes in insulin sensitivity, glucose tolerance, lipid deposition, and energy harvesting potential by altering the gut microbiota composition (32–38). In most of these studies, antibiotics have been shown to confer increased adiposity or weight gain independently of the type of antibiotics used (32, 36, 37), although antibiotic eradication or suppression of gut microbiota has also been shown to protect against diet-induced obesity or metabolic endotoxemia when the rodents where fed a high-fat diet (33, 34, 38). In line with a general growth promoting effect of antibiotics, they (several types) have been used in agriculture to achieve weight gain in livestock for decades (39) and exposure to antibiotics has been linked with development of obesity and increased body mass index in several observational studies (10–12). Finally, antibiotics could exert effects on glucose homeostasis or risk of type 2 diabetes independently of the gut microbiota (13). To our knowledge, however, no such mechanism has been documented in human intervention studies and the metabolic effects of antibiotics are abolished if animals are raised under sterile conditions (40).
Conclusions
Patients with type 2 diabetes, compared to control subjects free of type 2 diabetes, are overexposed to antibiotics before their diagnosis with type 2 diabetes as defined by the first redemption of a prescription on an oral glucose-lowering agent. This may represent an increased demand for antibiotics from an increased risk of infections in patients with yet-undiagnosed diabetes, prediabetes, or manifest type 2 diabetes. However, the possibility that antibiotics exposure increases diabetes risk cannot be excluded and deserves further investigation in interventional studies. Thus, our results call for new investigations of the long-term effect of antibiotics on lipid and glucose metabolism and body weight gain. In particular, we suggest investigation of commonly used narrow-spectrum penicillins because these drugs are frequently prescribed and showed the highest OR for type 2 diabetes risk.
Acknowledgments
We thank Morten Olesen for aid with data management and Reimar Thomsen for providing unpublished epidemiological data on the management of Danish patients with type 2 diabetes.
This work was supported by a grant from the Region of Southern Denmark.
Author contributions: All authors made substantial contributions to the study design and the acquisition and interpretation of the data. A.P. completed all analyses, which were validated by J.H. K.M. and A.P. drafted the manuscript. All authors contributed to the revision and completion of the article and provided their final approval of the version to be published.
Disclosure Summary: M. Frost has received fees for teaching from Amgen, Genzyme, and Eli Lilly. J.H. has participated in research projects funded by Novartis, Pfizer, Menarini, MSD, Nycomed, Astellas, and Alkabello with grants paid to the institution where he was employed; he has personally received fees for teaching or consulting from the Danish Association of Pharmaceutical Manufacturers and from Nycomed, Pfizer, Novartis, Astra Zeneca, Menarini, Leo Pharmaceuticals, and Ferring. A.P. has received funding from AstraZeneca, Astellas, Almirall, Servier, Boehringer Ingelheim, and Alcon, all with grants paid to the institution where he is employed. K.M.M. holds stocks in Chr. Hansen and Probi. F.K.K. reports not conflicts of interests for this publication.
Footnotes
- ATC
- Anatomical Therapeutic Chemical
- CI
- confidence interval
- DDD
- defined daily dose
- ICD
- International Classification of Diseases
- OR
- odds ratio.
References
- 1. Xu J, Gordon JI. Honor thy symbionts. Proc Natl Acad Sci. 2003;100(18):10452–10459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Qin J, Li Y, Cai Z, et al. A metagenome-wide association study of gut microbiota in type 2 diabetes. Nature. 2012;490(7418):55–60. [DOI] [PubMed] [Google Scholar]
- 3. Karlsson FH, Tremaroli V, Nookaew I, et al. Gut metagenome in European women with normal, impaired and diabetic glucose control. Nature. 2013;498(7452):99–103. [DOI] [PubMed] [Google Scholar]
- 4. Ridaura VK, Faith JJ, Rey FE, et al. Gut microbiota from twins discordant for obesity modulate metabolism in mice. Science. 2013;341(6150):1241214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Vrieze A, Van Nood E, Holleman F, et al. Transfer of intestinal microbiota from lean donors increases insulin sensitivity in individuals with metabolic syndrome. Gastroenterology. 2012;143(4):913–916.e7. [DOI] [PubMed] [Google Scholar]
- 6. Bäckhed F, Ding H, Wang T, et al. The gut microbiota as an environmental factor that regulates fat storage. Proc Natl Acad Sci U S A. 2004;101(44):15718–15723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Jernberg C, Löfmark S, Edlund C, Jansson JK. Long-term ecological impacts of antibiotic administration on the human intestinal microbiota. ISME J. 2007;1(1):56–66. [DOI] [PubMed] [Google Scholar]
- 8. Dethlefsen L, Relman DA. Incomplete recovery and individualized responses of the human distal gut microbiota to repeated antibiotic perturbation. Proc Natl Acad Sci. 2010;108(Suppl 1):4554–4561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Jakobsson HE, Jernberg C, Andersson AF, Sjölund-Karlsson M, Jansson JK, Engstrand L. Short-term antibiotic treatment has differing long-term impacts on the human throat and gut microbiome. PLoS ONE. 2010;5(3):e9836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Thuny F, Richet H, Casalta J-P, Angelakis E, Habib G, Raoult D. Vancomycin treatment of infective endocarditis is linked with recently acquired obesity. PLoS One. 2010;5(2):e9074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Trasande L, Blustein J, Liu M, Corwin E, Cox LM, Blaser MJ. Infant antibiotic exposures and early-life body mass. Int J Obes. 2013;37(1):16–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bailey LC, Forrest CB, Zhang P, Richards TM, Livshits A, DeRusso PA. Association of antibiotics in infancy with early childhood obesity. JAMA Pediatr. 2014;168(11):1063–1069. [DOI] [PubMed] [Google Scholar]
- 13. Chou H-W, Wang J-L, Chang C-H, Lee J-J, Shau W-Y, Lai M-S. Risk of severe dysglycemia among diabetic patients receiving levofloxacin, ciprofloxacin, or moxifloxacin in Taiwan. Clin Infect Dis. 2013;57(7):971–980. [DOI] [PubMed] [Google Scholar]
- 14. Lynge E, Sandegaard JL, Rebolj M. The Danish National Patient Register. Scand J Public Health. 2011;39(7 Suppl):30–33. [DOI] [PubMed] [Google Scholar]
- 15. Kildemoes HW, Sørensen HT, Hallas J. The Danish National Prescription Registry. Scand J Public Health. 2011;39(7 Suppl):38–41. [DOI] [PubMed] [Google Scholar]
- 16. WHO. Collaborating Centre for Drug Statistics Methodology. Guidelines for ATC classification and DDD assignment 2011. Oslo, Norway; 2010. [Google Scholar]
- 17. Pedersen CB. The Danish Civil Registration System. Scand J Public Health. 2011;39(7 Suppl):22–25. [DOI] [PubMed] [Google Scholar]
- 18. Sortsø C, Thygesen LC, Brønnum-Hansen H. Database on Danish population-based registers for public health and welfare research. Scand J Public Health. 2011;39(7 Suppl):17–19. [DOI] [PubMed] [Google Scholar]
- 19. Mor A, Berencsi K, Svensson E, et al. Prescribing practices and clinical predictors of glucose-lowering therapy within the first year in people with newly diagnosed type 2 diabetes. Diabet Med. 2015. doi:10.1111/dme.12819. [DOI] [PubMed] [Google Scholar]
- 20. Rothman KJ, Greenland S, Lash TL. Modern Epidemiology. 3rd ed Philadelphia, PA: Lippincott, Williams & Wilkins; 2012. [Google Scholar]
- 21. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. [DOI] [PubMed] [Google Scholar]
- 22. Thygesen LC, Daasnes C, Thaulow I, Brønnum-Hansen H. Introduction to Danish (nationwide) registers on health and social issues: structure, access, legislation, and archiving. Scand J Public Health. 2011;39(7 Suppl):12–16. [DOI] [PubMed] [Google Scholar]
- 23. Carstensen B, Kristensen JK, Ottosen P, Borch-Johnsen K, on behalf of the steering group of the National Diabetes Register. The Danish National Diabetes Register: trends in incidence, prevalence and mortality. Diabetologia. 2008;51(12):2187–2196. [DOI] [PubMed] [Google Scholar]
- 24. de Vegt F, Dekker JM, Jager A, et al. Relation of impaired fasting and postload glucose with incident type 2 diabetes in a dutch population: The Hoorn study. JAMA. 2001;285(16):2109–2113. [DOI] [PubMed] [Google Scholar]
- 25. Falagas ME, Kompoti M. Obesity and infection. Lancet Infect Dis. 2006;6(7):438–446. [DOI] [PubMed] [Google Scholar]
- 26. Boursi B, Mamtani R, Haynes K, Yang Y-X. The effect of past antibiotic exposure on diabetes risk. Eur J Endocrinol. 2015;172(6):639–648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Vrieze A, Out C, Fuentes S, et al. Impact of oral vancomycin on gut microbiota, bile acid metabolism, and insulin sensitivity. J Hepatol. 2014;60(4):824–831. [DOI] [PubMed] [Google Scholar]
- 28. Marchant MH, Viens NA, Cook C, Vail TP, Bolognesi MP. The impact of glycemic control and diabetes mellitus on perioperative outcomes after total joint arthroplasty. J Bone Joint Surg Am. 2009;91(7):1621–1629. [DOI] [PubMed] [Google Scholar]
- 29. Nitzan O, Elias M, Chazan B, Saliba W. Urinary tract infections in patients with type 2 diabetes mellitus: review of prevalence, diagnosis, and management. Diabetes Metab Syndr Obes. 2015;8:129–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Wukich DK, Crim BE, Frykberg RG, Rosario BL. Neuropathy and poorly controlled diabetes increase the rate of surgical site infection after foot and ankle surgery. J Bone Joint Surg Am. 2014;96(10):832–839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Delamaire M, Maugendre D, Moreno M, Le Goff MC, Allannic H, Genetet B. Impaired leucocyte functions in diabetic patients. Diabet Med. 1997;14(1):29–34. [DOI] [PubMed] [Google Scholar]
- 32. Cho I, Yamanishi S, Cox L, et al. Antibiotics in early life alter the murine colonic microbiome and adiposity. Nature. 2012;488(7413):621–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Carvalho BM, Guadagnini D, Tsukumo DML, et al. Modulation of gut microbiota by antibiotics improves insulin signalling in high-fat fed mice. Diabetologia. 2012;55(10):2823–2834. [DOI] [PubMed] [Google Scholar]
- 34. Membrez M, Blancher F, Jaquet M, et al. Gut microbiota modulation with norfloxacin and ampicillin enhances glucose tolerance in mice. FASEB J. 2008;22(7):2416–2426. [DOI] [PubMed] [Google Scholar]
- 35. Wichmann A, Allahyar A, Greiner TU, et al. Microbial modulation of energy availability in the colon regulates intestinal transit. Cell Host Microbe. 2013;14(5):582–590. [DOI] [PubMed] [Google Scholar]
- 36. De Sá Del Fiol F, Tardelli Ferreira ACM, Marciano JJ, Marques MC, Sant'Ana LL. Obesity and the use of antibiotics and probiotics in rats. Chemotherapy. 2015;60(3):162–167. [DOI] [PubMed] [Google Scholar]
- 37. Cox LM, Yamanishi S, Sohn J, et al. Altering the intestinal microbiota during a critical developmental window has lasting metabolic consequences. Cell. 2014;158(4):705–721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hwang I, Park YJ, Kim Y-R, et al. Alteration of gut microbiota by vancomycin and bacitracin improves insulin resistance via glucagon-like peptide 1 in diet-induced obesity. FASEB J. 2015;29(6):2397–2411. [DOI] [PubMed] [Google Scholar]
- 39. Blaser MJ. The Jeremiah Metzger Lecture: Global warming redux: the disappearing microbiota and epidemic obesity. Trans Am Clin Climatol Assoc. 2012;123:230–241. [PMC free article] [PubMed] [Google Scholar]
- 40. Dibner JJ, Richards JD. Antibiotic growth promoters in agriculture: history and mode of action. Poult Sci. 2005;84(4):634–643. [DOI] [PubMed] [Google Scholar]


