Abstract
Background:
Pneumocephalus (PNC) is the presence of air in the intracranial cavity. The most frequent cause is trauma, but there are many other etiological factors, such as surgical procedures. PNC with compression of frontal lobes and the widening of the interhemispheric space between the tips of the frontal lobes is a characteristic radiological finding of the “Mount Fuji sign.” In addition to presenting our own case, we reviewed the most relevant clinical features, diagnostic methods, and conservative management for this condition.
Case Description:
A 74-year-old male was diagnosed with meningioma of olfactory groove several years ago. After no improvement, surgery of the left frontal craniotomy keyhole type was conducted. A computed tomography (CT) scan of the skull performed 24 h later showed a neuroimaging that it is described as the silhouette of Mount Fuji. The treatment was conservative and used continuous oxygen for 5 days. Control CT scan demonstrated reduction of the intracranial air with normal brain parenchyma.
Conclusion:
The review of the literature, we did not find any cases of tension pneumocephalus documented previously through a supraorbital keyhole approach. There are a few cases reported of patients with Mount Fuji signs that do not require surgical procedures. The conservative treatment in our report leads to clinical and radiological improvement as well as a reduction in hospitalization time.
Keywords: Mount Fuji sign, olfactory meningioma, pneumocephalus, supraorbital keyhole approach, tension pneumocephalus
INTRODUCTION
The terms pneumocephalus (PNC) and tension pneumocephalus (TP) were created by Wolff[34] and Ectors,[8] respectively, even though TP has been described in the early literature.[6] PNC is the presence of air within the intracranial cavity. When this circumstance causes increased intracranial pressure that leads to neurological deterioration, it is known as TP. Ishiwata et al.[12] described the image produced by PNC in subdural collections that separated both frontal lobes as similar in appearance to the silhouette of the famous Fuji Volcano in Japan [Figure 1]. In this report, we present a case with a Mount Fuji sign after the evacuation of an olfactory groove meningioma through a supraorbital keyhole approach along with a short review of the literature.
Figure 1.

Fuji Volcano in Japan (available from internet)
CASE REPORT
A 74-year-old right-handed male was diagnosed with meningioma of olfactory groove several years ago. He presented with psychomotor agitation, confusion, and vertiginous crises. Among its antecedents, surgery for maxillary sinusitis, heart, and mesenteric thrombosis were mentioned. It more recently referred to a mild head injury. On neurological examination, motor or sensory deficits were not evidenced. The cranial nerve examination was normal. The patient underwent magnetic resonance imaging (MRI) that showed olfactory groove meningioma and significant perilesional edema around the tumor. He was initially treated with dexamethasone at a dosage of 4 mg every 6 h. After no improvement, surgery of the left frontal craniotomy keyhole type was conducted. The rigid endoscope was used to complete the resection. A computed tomography (CT) scan of the skull performed 24 h later showed bi-frontal subdural PNC with Mount Fuji sign with a slight shift to the right ventricular system and no frontal sinus breaches was identified [Figure 2]. At that time, the patient developed progressive decreased consciousness with a Glasgow coma score (GCS) between 12 and 13 points. He did not complain of a headache and did not have meningeal signs, such as vomiting or fever. Clinical examination revealed no neurological motor deficit. Additionally, no cerebrospinal fluid (CSF) leak or wound infection occurred.
Figure 2.
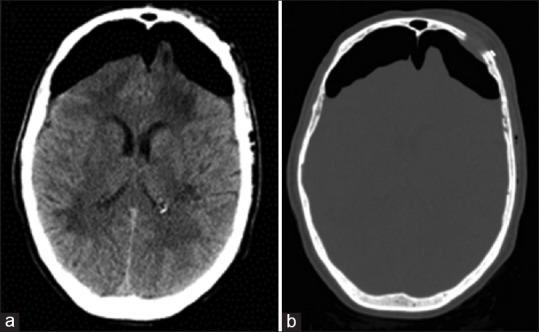
(a) Unenhanced axial computed tomography image of the brain demonstrates bilateral subdural areas of hypoattenuation with compression of both frontal lobes. (b) Postoperative computed tomography bone window image demonstrating the small supraorbital craniotomy
The family called for the transfer of the patient to a neighboring country, a request that was rejected because of the risk that implied. It was decided to observe the evolution of the patient with the use of antibiotics, acetazolamide, analgesics, and continuous oxygen at 5 L/min for 5 days. On 5th postoperative day, his level of consciousness improved. Control CT scan demonstrated reduction of the intracranial air with normal surface contours and parenchyma [Figure 3]. One week later, the patient was awake, had a GCS 15, and did not have cognitive or motor deficits.
Figure 3.
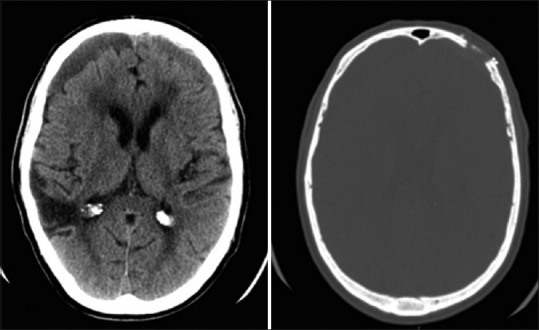
Control computed tomography scan demonstrating normal cerebral parenchyma surface
DISCUSSION
Pneumocephalus
The accumulation of intracranial air can be acute (<72 h) or delayed (≥72 h).[30] Others authors classified it as early PNC (<7 days) or late PNC (≥7 days).[28] It can be located in the epidural, subarachnoid, intraventricular, intracerebral, or subdural space, with the subdural space most frequent. The common site is frontal, followed by the occipital and temporal areas.[30]
At least two possible mechanisms for the development of PNC are described.[6] One is the effect of ball valve, where the air enters from the extracranial space through CSF leakage, which allows input but not output. When the intracranial pressure increases, the brain, and the dura plug the fistula tract and prevent air from going out. Another theory is known as the inverted soda bottle effect. Loss occurs when the CSF for a fistula or external drainage causes negative intracranial pressure. Air enters as bubbles, replacing the CSF as the pressure in the two cavities balance. A more unusual mechanism is the production of gas in situ due to infection by germs forming gas.[23]
A review of 295 patients with PNC indicates that trauma is the most common cause of PNC, accounting for 75% of cases. Infection, most common chronic otitis media, accounted for 9% of the cases reviewed.[15] Common causes of PNC are cranial or spinal surgery as well as some ENT operations, such as paranasal sinus surgery, nasal septum resection, or nasal polypectomy.[30] In some cases, the incidence of PNC after supratentorial craniotomy has been reported to be 100%. Sixty-six percent of these PNC were judged to be moderate or large, and the incidence decreased to 75% by postoperative day 7. Nonetheless, 11.8% of the scans obtained during the 2nd postoperative week had PNC that were judged to be moderate or large.[25] Several contributing factors have been implicated in the pathogenesis of TP, including nitrous oxide anesthesia, duration of surgery, hydrocephalus, a functional ventriculoperitoneal shunt, and intraoperative administration of mannitol.[29]
Clinically, PNC can cause headaches, nausea, vomiting, irritability, dizziness, and seizures. Sometimes the patient reported air entry intracranial space as a “gurgling” sensation in the head, based on the audible gas input.[3] When PNC causes intracranial hypertension and has a mass effect, it is called TP. If it is not diagnosed early and treated properly, TP can be fatal. An attempt was made to explain this effect based on the volume of gas, with one author using the value of 65 mL of air.[17] Others believe that about 25 mL of air can cause TP.[2] However, this method is hindered by the inherent difficulties in volume estimation in all CT scans.[16] In addition, Ishiwata et al. have found no substantial difference between the volume of air in TP and that in nontension PNC.[12]
Mount Fuji sign
CT is a golden standard for PNC or TP diagnostics. It only requires 0.55 mL of air to be detected, whereas a simple skull radiograph requires at least 2 mL.[13] Air between the frontal tips is a characteristic finding of the “Mount Fuji sign,” which means there is the greater pressure of air than the surface tension of cerebral fluid between the frontal lobes.[12] In anterior cranial fossa, the dura mater is thin and closely applied to bone and the arachnoids adherent to frontal lobes; therefore, the air is trapped in the subdural space of the anterior cranial fossa. When there is a bilateral compression of the frontal lobes without separation of the frontal tips, it is called “peaking sign,” which was previously linked to TP.[1] Blanco-Ulla and Villa Fernández do not believe that bridging veins that penetrate the superior sagittal sinus morphologically caused the shape of the tuned frontal lobes in the TP. They feel that this is more available to the arachnoid granulations of Pacchioni, located at some distance from the sagittal sinus.[4]
An MRI axial view of fluid-attenuated inversion recovery revealed the Mount Fuji sign with collapsed frontal lobes and widening of the interhemispheric space between the bilateral tips of the frontal lobes.[35] Nevertheless, MRI is not a technique that is, as sensitive as a CT scan.
The Mount Fuji sign indicates more severe PNC than the peaking sign and the necessity of emergent decompression,[31] although in some cases, as in our report, a patient with Mount Fuji sign sometimes does not need a surgical procedure. For Michel, the Mount Fuji sign on a CT scan of the brain can be useful in discriminating tension PNC from nontension PNC.[16] Some authors described neuroimaging simulating a sign of Mount Fuji.[24] This same image has also been described in pneumoperitoneum, and it is considered another indicator of an emergency condition.[10]
Treatment of pneumocephalus
Pneumocephalus usually gets absorbed without any clinical manifestations. The conservative treatment involves placing the patient in the Fowler position of 30°, avoiding Valsalva maneuver (coughing and sneezing), administering pain and antipyretic medications to prevent hyperthermia, and osmotic diuretics. With these measures, reabsorption was observed in 85% of cases after 2–3 weeks.[13] In other cases, different procedures have been used. For example, Paiva et al.[20] studied the effects of hyperbaric oxygenation (HBO2) therapy sessions on a group of 13 patients with PNC in comparison to a control group of 11 patients with normobaric oxygenation administered continuously at 5 L/min for 5 days, resulting in the reabsorption of nitrogen into the blood stream and a reduction in the volume of the intracranial air. Clinical improvement was seen in all patients. The treated group also experienced a lower rate of meningitis compared to the control group, and the length of the hospital stay was significantly higher in the control group compared to the treated group. Also, Webber-Jones[33] recommended the use of 100% oxygen with repair of the bony and dural defect. Pankaj's study concludes that the use of an oxygen mask increases the reabsorption of pneumocephalus compared to a nasal catheter.[22] On the other hand, González Tortosa et al.[9] reported a posttraumatic PNC, aggravated by hyperbaric chamber treatment.
When clinical signs appear, such as intracranial hypertension or impaired consciousness that endangers the life of the patient, treatment consists of emergent decompression to alleviate pressure on the brain parenchyma. Also, air is toxic to neurons, causing further damage to the already compromised parenchyma, and that leads to cerebral edema surrounding the air that evolves into encephalomalacia.[32]
Treatment options for TP include the drilling of burr holes, needle aspiration, and closure of the dural defect. If the frontal sinus is open during surgery, it is aggressively managed with exenteration of the mucosa, sinus packing with abdominal fat or a piece of temporal muscle and covered with frontal fascia.[21] There are a few cases reported of asymptomatic massive pneumocephalus[18] or patients with Mount Fuji signs that do not require surgical procedures.[31]
Pneumocephalus and air evacuation
Traveling by plane is considered high risk because as the height increases, atmospheric pressure decreases, and the gasses expand. Therefore, a pneumothorax could become hypertensive, a bulla could expand or break, and PNC could enlarge and produce more intracranial hypertension. However, Donovan et al.[7] reported the outcomes of a series of 21 patients with posttraumatic and/or postcraniotomy PNC, who underwent long-range air evacuation from a combat theater in military aircraft. The volumes of PNC ranged from 0.6 to 42.7 mL, with a mean volume of 9.3 mL and the median volume of 4.2 mL. No patient sustained a temporary or permanent neurologic decline as a result of air transportation. They concluded that PNC in patients with head injuries and craniotomies was not likely by itself to be an absolute contraindication to air evacuation.
Finally, the medical guideline recommends waiting at least 7 days to fly after a transcranial or spinal surgery that could introduce gas into the skull. Neurosurgical procedures could be a cause of residual intracranial air and could create a dormant fistulous tract that opens when the cabin pressure changes. Although it is difficult to make one guideline to apply to all cases, the concern for possible problems during air travel could lead to a consensus among consultant neurosurgeons.[11]
Supraorbital keyhole craniotomy
The supraorbital craniotomy offers equal surgical possibilities with fewer approach-related morbidity due to limited exposure of the cerebral surface and minimal brain retraction. The short skin incision within the eyebrow and careful soft tissue dissection result in a pleasing cosmetic outcome.[26]
According to Ormond and Hadjipanayis,[19] MEDLINE search revealed a total of 81 cases of olfactory groove meningioma reported in the literature. Complications reported included eight CSF leaks (9.9%). Because the recessed cribriform plate is difficult to visualize with a microscope during a supraorbital keyhole approach, some authors have recommended an endoscopic endonasal route. A recent study compared both procedures and concluded that better resections and lower CSF leak rates were possible through the open rather than the endoscopic approach,[14] but the use of the endoscope for assisting the cribriform plate allows a better resection of olfactory groove meningiomas while helping with skull base reconstruction to prevent CSF leakage.[19]
The main complication reported with the superciliary craniotomy was CSF rhinorrhea. Several papers showed different ranges. In 66 patients operated on using the lateral supraorbital approach applied to olfactory meningiomas, Romani et al.[27] found 6 patients (9%) with CSF leakage. Four of the 6 patients were treated with lumbar drainage for a few days. The other 2 patients required a fascia lata graft. Paiva-Neto and Tella[21] reported 2 cases (8%) with CSF rhinorrhea that were successfully treated by lumbar external drainage, and there was 1 case of meningitis and one mortality. Reisch and Perneczky[26] described CSF leak in 12 patients (2.6%), 7 cases through the frontal sinus and 5 cases through the deep paranasal sinuses after removal of the anterior clinoid process. Of these patients, five underwent surgical reconstruction, and in 7 cases, the fistula was closed after lumbar drainage. On the other hand, among 302 patients operated on using a supraorbital eyebrow approach, Czirják and Szeifert[5] evaluated 76 frontolateral keyhole craniotomies performed for supratentorial intracranial tumors. They did not have any craniotomy-related complications. In our revision, we did not find any cases of Mount Fuji sign with this approach.
CONCLUSIONS
The review of the literature, we did not find any cases of TP documented previously through a supraorbital keyhole approach.
TP must be treated by surgical revision when it causes intracranial hypertension and/or deterioration of consciousness. There are a few cases reported of patients with Mount Fuji signs that do not require surgical procedures. The conservative treatment in these patients with HBO2 therapy sessions in a monoplace hyperbaric chamber with 100% oxygen concentration or normobaric oxygenation administered continuously at 5 L/min at least for 5 days, may lead to clinical and radiological improvement as well as a reduction in hospitalization time.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Contributor Information
Carlos B. Dabdoub, Email: carlosdabdoub@hotmail.com.
Gueider Salas, Email: gueidersalas@gmail.com.
Elisabeth do N. Silveira, Email: betinha_nurse@hotmail.com.
Carlos F. Dabdoub, Email: cdabdoub45@hotmail.com.
REFERENCES
- 1.Agrawal A, Singh BR. Mount Fuji sign with concavo-convex appearance of epidural haematoma in a patient with tension pneumocephalus. Radiol Case. 2009;3:10–2. doi: 10.3941/jrcr.v3i1.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aoki N, Sakai T. Computed tomography features immediately after replacement of haematoma with oxygen through percutaneous subdural tapping for the treatment of chronic subdural haematoma in adults. Acta Neurochir (Wien) 1993;120:44–6. doi: 10.1007/BF02001468. [DOI] [PubMed] [Google Scholar]
- 3.Bernstein AL, Cassidy J, Duchynski R, Eisenberg SS. Atypical headache after prolonged treatment with nasal continuous positive airway pressure. Headache. 2005;45:609–11. doi: 10.1111/j.1526-4610.2005.05117_3.x. [DOI] [PubMed] [Google Scholar]
- 4.Blanco-Ulla M, Villa Fernández J. Anatomical basis of the sign of Mount Fuji. Rev Argent Radiol. 2014;78:242–4. [Google Scholar]
- 5.Czirják S, Szeifert GT. The role of the superciliary approach in the surgical management of intracranial neoplasms. Neurol Res. 2006;28:131–7. doi: 10.1179/016164106X97991. [DOI] [PubMed] [Google Scholar]
- 6.Dandy WE. Pneumocepahlus (intracranial pneumatocele or aerocele) Arch Surg. 1926;132:949–82. [Google Scholar]
- 7.Donovan DJ, Iskandar JI, Dunn CJ, King JA. Aeromedical evacuation of patients with pneumocephalus: Outcomes in 21 cases. Aviat Space Environ Med. 2008;79:30–5. doi: 10.3357/asem.1893.2008. [DOI] [PubMed] [Google Scholar]
- 8.Ectors L. Chronic subdural hematoma. Surgical treatment. (article in French) Acta Chir Belg. 1962;6:570–606. [Google Scholar]
- 9.González Tortosa J, Mendoza Roca A, Poza Poza M. Post-traumatic pneumocephalus, aggravated by hyperbaric chamber treatment.(article in Spanish) Neurocirugía. 1996;7:126–8. [Google Scholar]
- 10.Hokama A, Yara S, Fujita J, Nakamura S, Nakaema M, Kuniyoshi Y. The Mount Fuji sign of the pneumoperitoneum. Emerg Med J. 2009;26:300. doi: 10.1136/emj.2008.062125. [DOI] [PubMed] [Google Scholar]
- 11.Huh J. Barotrauma-induced pneumocephalus experienced by a high risk patient after commercial air travel. J Korean Neurosurg Soc. 2013;54:142–4. doi: 10.3340/jkns.2013.54.2.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ishiwata Y, Fujitsu K, Sekino T, Fujino H, Kubokura T, Tsubone K, et al. Subdural tension pneumocephalus following surgery for chronic subdural hematoma. J Neurosurg. 1988;68:58–61. doi: 10.3171/jns.1988.68.1.0058. [DOI] [PubMed] [Google Scholar]
- 13.Karavelioglu E, Eser O, Haktanir A. Pneumocephalus and pneumorrhachis after spinal surgery: Case report and review of the literature. Neurol Med Chir (Tokyo) 2014;54:405–7. doi: 10.2176/nmc.cr2013-0118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Komotar RJ, Starke RM, Raper DM, Anand VK, Schwartz TH. Endoscopic endonasal versus open transcranial resection of anterior midline skull base meningiomas. World Neurosurg. 2012;77:713–24. doi: 10.1016/j.wneu.2011.08.025. [DOI] [PubMed] [Google Scholar]
- 15.Markham JW. The clinical features of pneumocephalus based upon a survey of 284 cases with report of 11 additional cases. Acta Neurochir (Wien) 1967;16:1–78. doi: 10.1007/BF01401900. [DOI] [PubMed] [Google Scholar]
- 16.Michel SJ. The Mount Fuji sign. Radiology. 2004;232:449–50. doi: 10.1148/radiol.2322021556. [DOI] [PubMed] [Google Scholar]
- 17.Monajati A, Cotanch WW. Subdural tension pneumocephalus following surgery. J Comput Assist Tomogr. 1982;6:902–6. doi: 10.1097/00004728-198210000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Ogando-Rivas E, Navarro-Ramírez PA, Benítez-Gasca PA, Lorenzo-Ruiz M, Ramos-Sandoval F. Asymptomatic massive neumoencephalus (article in Spanish) Rev Med Hosp Gen Méx. 2014;77:74–8. [Google Scholar]
- 19.Ormond DR, Hadjipanayis CG. The supraorbital keyhole craniotomy through an eyebrow incision: Its origins and evolution. Minim Invasive Surg 2013. 2013 doi: 10.1155/2013/296469. 296469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Paiva WS, de Andrade AF, Figueiredo EG, Amorim RL, Prudente M, Teixeira MJ. Effects of hyperbaric oxygenation therapy on symptomatic pneumocephalus. Ther Clin Risk Manag. 2014;10:769–73. doi: 10.2147/TCRM.S45220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Paiva-Neto MA, Tella OI., Jr Supra-orbital keyhole removal of anterior fossa and parasellar meningiomas. Arq Neuropsiquiatr. 2010;68:418–23. doi: 10.1590/s0004-282x2010000300018. [DOI] [PubMed] [Google Scholar]
- 22.Pankaj G. Normobaric oxygen therapy strategies in the treatment of postcraniotomy pneumocephalus. J Neurosurg. 2008;108:926–9. doi: 10.3171/JNS/2008/108/5/0926. [DOI] [PubMed] [Google Scholar]
- 23.Penrose-Stevens A, Ibrahim A, Redfern RM. Localized pneumocephalus caused by Clostridium perfringens meningitis. Br J Neurosurg. 1999;13:85–6. doi: 10.1080/02688699944285. [DOI] [PubMed] [Google Scholar]
- 24.Prakash B, Pranesh MB, Parimalam N, Harish Kumar R. Hyperostosis frontalis interna mimicking Mount Fuji sign. J Assoc Physicians India. 2011;59:181–3. [PubMed] [Google Scholar]
- 25.Reasoner DK, Todd MM, Scamman FL, Warner DS. The incidence of pneumocephalus after supratentorial craniotomy. Observations on the disappearance of intracranial air. Anesthesiology. 1994;80:1008–12. doi: 10.1097/00000542-199405000-00009. [DOI] [PubMed] [Google Scholar]
- 26.Reisch R, Perneczky A. Ten-year experience with the supraorbital subfrontal approach through an eyebrow skin incision. Neurosurgery. 2005;57(4 Suppl):242–55. doi: 10.1227/01.neu.0000178353.42777.2c. [DOI] [PubMed] [Google Scholar]
- 27.Romani R, Lehecka M, Gaal E, Toninelli S, Celik O, Niemelä M, et al. Lateral supraorbital approach applied to olfactory groove meningiomas: Experience with 66 consecutive patients. Neurosurgery. 2009;65:39–52. doi: 10.1227/01.NEU.0000346266.69493.88. [DOI] [PubMed] [Google Scholar]
- 28.Ruiz-Juretschke F, Mateo-Sierra O, Iza-Vallejo B, Carrillo-Yagüe R. Intraventricular tension pneumocephalus after transsphenoidal surgery: A case report and literature review. Neurocirugia (Astur) 2007;18:134–7. [PubMed] [Google Scholar]
- 29.Satapathy GC, Dash HH. Tension pneumocephalus after neurosurgery in the supine position. Br J Anaesth. 2000;84:115–7. doi: 10.1093/oxfordjournals.bja.a013368. [DOI] [PubMed] [Google Scholar]
- 30.Solomiichuk VO, Lebed VO, Drizhdov KI. Posttraumatic delayed subdural tension pneumocephalus. Surg Neurol Int. 2013;4:37. doi: 10.4103/2152-7806.109537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tazón-Varela MA, Hernández-Herrero M, Alonso-Vega L, Pérez-Mier LA, Gallastegui Menéndez A. Severe head injury: The Mount Fuji sign.(article in Spanish) Emergencias. 2011;23:415. [Google Scholar]
- 32.Venkatesh SK, Bhargava V. Clinics in diagnostic imaging (119). Post-traumatic intracerebral pneumatocele. Singapore Med J. 2007;48:1055–9. [PubMed] [Google Scholar]
- 33.Webber-Jones JE. Tension pneumocephalus. J Neurosci Nurs. 2005;37:272–6. doi: 10.1097/01376517-200510000-00007. [DOI] [PubMed] [Google Scholar]
- 34.Wolff E. Air accumulation in the right lateral ventricle of the brain (Pneumocephalus) (article in German) Münch Med Wochenschr. 1914;61:899. [Google Scholar]
- 35.Yamashita S, Tsuchimochi W, Yonekawa T, Kyoraku I, Shiomi K, Nakazato M. The Mount Fuji sign on MRI. Intern Med. 2009;48:1567–8. doi: 10.2169/internalmedicine.48.2511. [DOI] [PubMed] [Google Scholar]


