Abstract
Background:
Penetrating nail-gun injuries to the head are rare, however, the incidence has been gradually rising over the last decade. While there is a large volume of case reports in the literature, there are only a few incidences of cerebrovascular injury. We present a case of a patient with a nail-gun injury to the brain, which compromised the cerebral vasculature. In this article, we present the case, incidence, pathology, and a brief literature review of penetrating nail-gun injuries to highlight the principles of management pertaining to penetration of cerebrovascular structures.
Case Description:
A 26-year-old male presented with a penetrating nail-gun injury to his head. There were no neurological deficits. Initial imaging revealed that the nail had penetrated the cranium and suggested the vasculature to be intact. However, due to the proximity of the nail to the circle of Willis the operative approach was tailored in anticipation of a vascular injury. Intraoperatively removal of the foreign body demonstrated a laceration to the M1 branch of the middle cerebral artery (MCA), which was successfully repaired.
Conclusion:
To our knowledge, this is the first reported case of a vascular arterial injury to the MCA from a nail-gun injury. It is imperative to have a high clinical suspicion for cerebrovascular compromise in penetrating nail-gun injuries even when conventional imaging suggests otherwise.
Keywords: Craniotomy, middle cerebral artery, nail-gun, trauma
INTRODUCTION
Intracranial nail-gun injuries are a rare but well-characterized cause of penetrating brain injury. The incidence of these injuries has been rising; the annual rate has almost tripled over the last decade.[7] As such, it is important for the clinician to be aware of these types of injuries. Despite the number of clinical challenges that they may present, a sound rational management strategy should permit most of these patients to be safely treated minimizing the risks of additional injury.
Here, we describe to our knowledge, the first reported case of a penetrating craniocerebral nail-gun injury causing vascular injury to the M1 branch of the middle cerebral artery (MCA). Technical considerations and challenges in the removal of the foreign body and in vascular repair are discussed as well. This report demonstrates that primary repair of a traumatic injury to the arterial vasculature can be associated with good radiographic and clinical outcome.
CASE HISTORY
History and physical examination
A 26-year-old male with no prior medical illnesses presented to hospital after apparently accidentally shooting himself with a nail-gun. He reportedly tripped while helping a friend with work on a deck, triggering the nail-gun during the fall. The patient denied any loss of consciousness, headaches, or seizure-like activity. He was initially assessed in a peripheral hospital Emergency Department where plain skull X-rays revealed a nail traversing the temporal bone [Figure 1]. Subsequently, he was transferred to our neurosurgical service for further evaluation and management.
Figure 1.
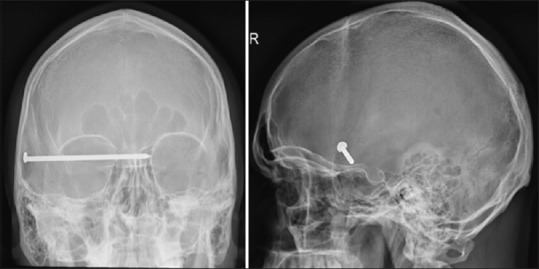
Anterior-Posterior and lateral skull X-rays showing an 8.7 cm nail projecting over the right temporal region, with apparent intracranial extension. No discrete calvarial fractures are detected
On presentation to our center, he was alert and oriented (Glasgow Coma Score 15). All cranial nerves were intact. There was no evidence of any motor, sensory or cerebellar dysfunction in his limbs. He was hemodynamically stable. The only abnormal laboratory finding was a mild leukocytosis. Computed tomography (CT) revealed a metallic foreign body is penetrating the right temporal bone. In addition, there was the presence of diffuse subarachnoid hemorrhage (SAH) within the basal cisterns and right sylvian fissure [Figure 2]. Evaluation of the surrounding brain parenchyma was limited due to scattered artifact caused by the foreign body. However, there was no clear evidence of intraparenchymal hemorrhage or edema noted. CT angiography (CTA) [Figures 2 and 3] revealed the foreign body to be within the vicinity of the circle of Willis. Artifact from the nail was present on this study too, but the luminal flow could be visualized throughout. Furthermore, there was no clear evidence of vessel perforation, dissection, thrombosis, or branch occlusion. Since there was still a possibility of vessel injury, and because we decided to forgo conventional angiography, we were prepared for a surgically corrective action if an injury to the vessel was encountered. To prepare for this, specialized vascular equipment including aneurysm clips and an operating microscope capable of intraoperative indocyanine green angiography was made available, and the neurovascular team was called. The patient was subsequently taken to the operating room on an emergent basis for removal of the foreign body.
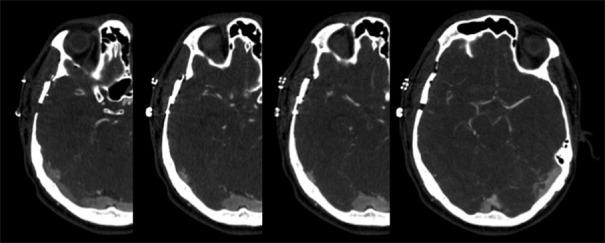
Figure 2.
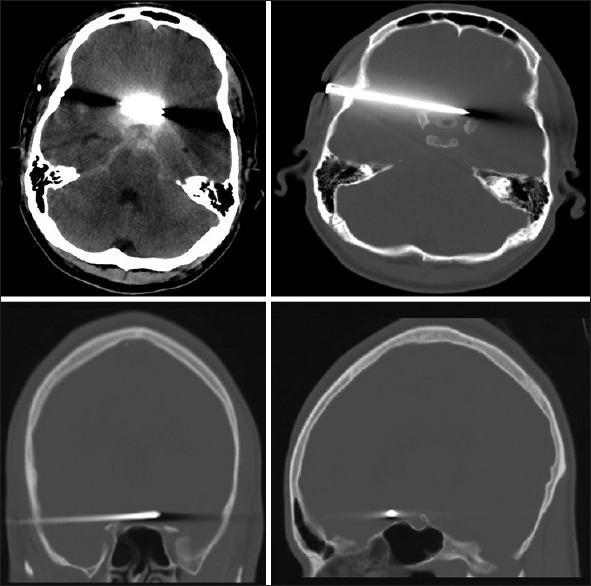
Sections of a noncontrast computed tomography head showing scattered subarachnoid hemorrhage in association with an intracranial nail penetrating the right temporal bone and projecting across midline, superior to the sphenoid sinus and anterior to the pituitary fossa, with evidence of obstructive hydrocephalus. Note the beam-hardening artifact
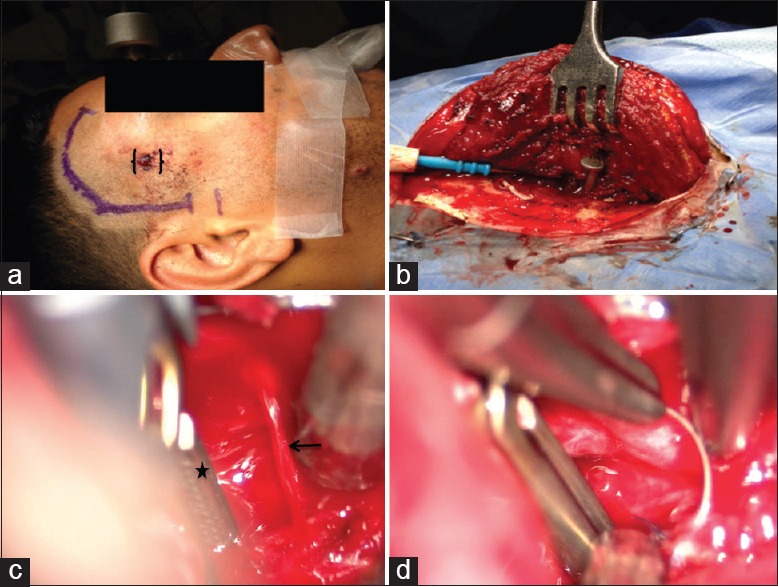
Figure 3.
Sections of a computed tomography angiogram are confirming intact internal carotids. The right M1 to the proximal M3 middle cerebral artery and anterior communicating artery regions are not visualized. However, there is normal distal filling of the right middle cerebral artery beyond the beam-hardening artifact, with no obvious vessel perforation, dissection, thrombosis, or branch occlusion
Operative note
Prior to positioning, the patient received 0.5 mg/kg of 20% IV mannitol. With the head secured in the 3-pin Mayfield fixation system, a curvilinear incision extending from the zygoma, and curving anterior to the ipsilateral hairline was performed. After cutting down to the temporalis fascia and reflecting the myocutaneous flap, a small craniotomy was performed, and the lateral sphenoid wing was drilled flat. The cranium surrounding the nail was left intact, and the dura was opened in a semi-circular fashion. The bone immediately surrounding the nail was then removed with a curved double-action bone rongeur. The nail was then slowly removed with a Leksell rongeur by using slight twist and pull out movements. Immediately after freeing the nail, the brain began to swell. Because of this, maneuvers to decrease the rising intracranial pressure, which included administration of a second dose of 0.5 mg/kg of 20% mannitol and elevation of the head of the operating table, were undertaken with good response. As the sylvian fissure was opened, a small amount of bleeding was noted; however, the bleeding became more brisk as the sylvian fissure was dissected more proximally. As we approached the M1 segment of the MCA vessel, an obvious vessel laceration was identified. Once the MCA was freed and dissected, a temporary clip was placed for proximal control. The laceration was repaired with 10.0 prolene sutures in an interrupted fashion [Figure 4]. Intraoperative Doppler ultrasound was then used to verify that proximal and distal flow in the vessel was maintained.
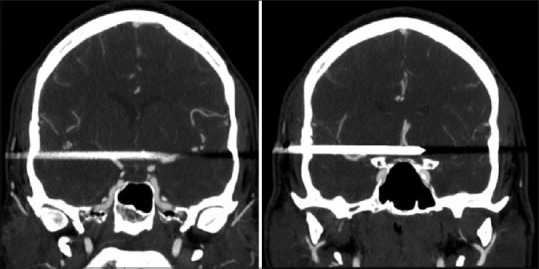
Figure 4.
Intraoperative images demonstrating the entry point of the nail (double brackets), proposed pterional incision (a) and temporalis reflection (b). A jet of blood (arrow) exsanguinating from the M1 vessel and application of a proximal temporary aneurysm clip (star) (c). Repair of the arteriotomy (d)
Postoperative management and outcome
On postoperative day (POD) 1, a CTA [Figure 5] revealed that the major intracranial arteries were patent with no pseudoaneurysm or vessel occlusion noted. A selective 2-vessel conventional digital subtraction angiogram (DSA) was performed on POD 3 that revealed normal cerebral vasculature, with no evidence of extravasation, pseudoaneurysm, and stenosis or thrombosis. There was good flow proximally and distally to the repair site [Figure 6]. The patient received a 7-day course of empiric antibiotic therapy. A psychiatric evaluation proved to be normal. He was discharged on POD 8 with no neurological deficits.
Figure 5.
Serial cuts of axial computed tomography angiogram obtained on postoperative day 1 after removal of the nail and closure of a breached middle cerebral artery, showing the visualized intracranial vasculature is normal in appearance
Figure 6.
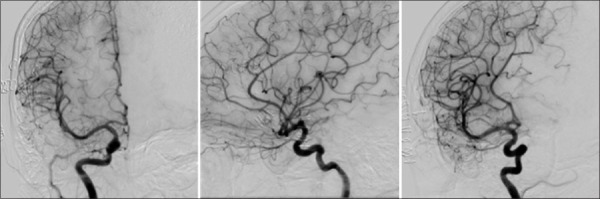
Right internal carotid AP (left), lateral (middle), and oblique (right) projections of a digital subtraction angiogram obtained on postoperative day 3, showing no evidence of extravasation, stenosis or occlusion after middle cerebral artery repair
DISCUSSION
With the growing use of pneumatic nail-guns both in the construction industry and by consumers for home use, penetrating craniofacial injuries caused by these devices are on the rise. Most of these injuries are primarily work-related accidents but are also commonly reported as intentionally self-inflicted.[10,15,17]
While the literature is filled with case reports and several series of penetrating intracranial nail-gun injuries, to our knowledge this is the first reported case of a nail-gun injury to the M1 branch of the MCA. In fact, a review of the literature shows few reported cases involving the cerebral vascular system at all. Sani et al. described the successful repair of an intracranial nail-gun injury involving the superior sagittal sinus.[14] Weil et al. also described a low-velocity nail injury of the petrous internal carotid artery (ICA).[19] Selvanathan et al. described a case series with one patient having a nail impinging on the petrous segment of the ICA, who subsequently developed a traumatic pseudoaneurysm of the ICA.[15] More recently, an intracranial nail penetrating the distal basilar artery was successfully removed and treated by surgical clipping.[7]
Posttraumatic pseudoaneurysms are rare but commonly described the occurrence, representing <1% of intracranial aneurysms. They occur when there is the complete disruption of all the three arterial wall layers, and the organizing hematoma or gliotic brain tissue forms the wall of an aneurysm. Posttraumatic pseudoaneurysms occur most commonly in the periphery of the brain where vessels are closely apposed to the dura.[3] The interval between penetrating injury and the detection of a traumatic aneurysm varies from immediately after penetrating injury to years, with a mean time of 2–3 weeks.[2] Posttraumatic aneurysms are associated with fatal outcomes, with a reported mortality up to 41%.[3] There are four high-risk situations for development of these fatal aneurysms: (1) Missile or bone fragments close to the skull base (2) large hematoma at the entry site (3) multiple fragments passing in various directions (4) high clinical suspicion by the surgeon.[8] Additionally, some recommend that routine angiography should be performed in all patients within 1–2 weeks after the injury to rule out the occurrence of pseudoaneurysms.[6] Despite the multitude of reports of traumatic pseudoaneurysms, there have only been four reported cases of traumatic pseudoaneurysms from intracranial nail penetration.[15]
The significance of a nail-gun associated M1 injury despite a seemingly normal CTA makes several important learning points regarding the management of these patients. Firstly, CTA cannot definitively rule out a vessel injury due to the large amount of metal artifact created by the nail. It can, however, indicate whether the vessel is patent, especially when considered together with the patient's symptomatology. In our case, the patient was neurologically intact and had a CTA suggesting continued patency of the parent vessel. It should, however, be noted that despite the CTA showing no vessel injury, our patient clearly had traumatic disruption of the wall of the M1 vessel from the nail. Nevertheless, because preservation of vessel patency was paramount in our case, we decided to forgo conventional angiography and to be prepared for a surgically corrective action. In hindsight, considering our intraoperative finding of a breached major vessel, we do recommend consideration of conventional angiography if there is any clinical suspicion of potential vascular compromise. If a vascular compromise is detected on angiography, obtaining proximal vascular control prior to the removal of the nail is imperative. In addition, if there is flow compromise within the vessel or an obvious pseudoaneurysm, yet no neurological deficit is present, then a conventional angiography with possible endovascular sacrifice of the vessel or pseudoaneurysm repair prior to surgical removal of the foreign body is strongly recommended. On the other hand, if a neurological deficit is present, and in the absence of a significant infarct, immediate surgical exploration with preparation for intraoperative vessel repair may be warranted in order to perfuse the ischemic brain tissue.
Various surgical approaches to removal of these foreign bodies have been proposed. If the calvaria is not penetrated extraction under local anesthetic may be effective and is associated with minimal complications.[15] In contrast, reports of devastating complications such as subdural or intraparenchymal hematoma following the blind removal of foreign bodies entering the dura suggests that direct visualization during removal is imperative.[12,18] Attempts should also be made to preserve an adequate length of the superficial temporal artery (STA) during the craniotomy, should distal anastomosis become necessary. As such, we performed a modified pterional craniotomy, which allowed us to preserve the STA, yet provided us with an adequate corridor to manage any suspected vascular injury. As described by Shenoy et al., blind removal using gentle traction with the rotatory movement was attempted in our case.[16] Serious hemorrhage is unusual even when the nail has transfixed a major vessel such as the sagittal sinus.[11,13] Endovascular embolization as an adjunct has also been described as a less invasive, effective and safe alternative.[9]
Complications of penetrating head trauma include local wound infection, meningitis, and formation of a brain abscess. Cerebrospinal fluid leaks and air sinus wounds increase the risk of infection.[5] Currently, there are no established guidelines for the use of prophylactic antibiotics, although it is recommended.[1] The risks of seizures following traumatic brain injury occur in about 30–50% of cases.[5] As such, prophylactic anti-seizure medications should be started after an injury to decrease the incidence of early posttraumatic seizures.[4] Finally, a thorough neuropsychiatric assessment should be undertaken in all situations, especially with a possibility of suicide attempt cannot be excluded. Psychotic illnesses such as depression and schizophrenia have been associated with these types of injuries.[17]
CONCLUSION
Penetrating vascular injuries from nail-gun injuries are exceedingly rare. Despite impressive clinical and radiological presentations, this type of low-velocity trauma usually produces very limited collateral injury. The first step in management involves careful neurological and radiographic assessments. The cornerstone of imaging should be CT with and without angiographic sequences. In the event that vascular compromise is suspected, a formal cerebral angiogram may be considered. However, it is also reasonable to proceed to surgery prepared for vascular disruption. Removal of a penetrating foreign object should be undertaken only with direct visualization and after preparations for vascular control have been made. This case demonstrates that despite a benign-looking preoperative vascular imaging study a high-level of suspicion for vessel injury should be maintained, and preparations for the corrective action undertaken.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
Daniel Fok, MD. Division of Neurology, University of Calgary, Calgary, Alberta
Roberto Diaz, MD PhD. Division of Neurosurgery, University of Calgary, Calgary, Alberta.
Footnotes
Contributor Information
Albert M. Isaacs, Email: akm.isaacs@gmail.com.
Sung-Joo Yuh, Email: syuh071@gmail.com.
R. John Hurlbert, Email: jhurlber@ucalgary.ca.
Alim P. Mitha, Email: alimmitha@gmail.com.
REFERENCES
- 1.Antibiotic prophylaxis for penetrating brain injury. J Trauma. 2001;51(2 Suppl):S34–40. [PubMed] [Google Scholar]
- 2.Blankenship BA, Baxter AB, McKahn GM., 2nd Delayed cerebral artery pseudoaneurysm after nail gun injury. AJR Am J Roentgenol. 1999;172:541–2. doi: 10.2214/ajr.172.2.9930820. [DOI] [PubMed] [Google Scholar]
- 3.Bula WI, Loes DJ. Trauma to the cerebrovascular system. Neuroimaging Clin N Am. 1994;4:753–72. [PubMed] [Google Scholar]
- 4.Carey M. Moderate and severe traumatic brain injury. In: Marshall LF, Grady MS, editors. Youmans Neurological Surgery. 5th ed. Vol. 4. Philadelphia: Bullet Wounds to the Brain Among Civilians; 2004. [Google Scholar]
- 5.Cemil B, Tun K, Yigenoglu O, Kaptanoglu E. Attempted suicide with screw penetration into the cranium. Ulus Travma Acil Cerrahi Derg. 2009;15:624–7. [PubMed] [Google Scholar]
- 6.du Trevou MD, van Dellen JR. Penetrating stab wounds to the brain: The timing of angiography in patients presenting with the weapon already removed. Neurosurgery. 1992;31:905–11. doi: 10.1227/00006123-199211000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Englot DJ, Laurans MS, Abbed K, Bulsara KR. Removal of nail penetrating the basilar artery. Neurosurg Rev. 2010;33:501–4. doi: 10.1007/s10143-010-0268-3. [DOI] [PubMed] [Google Scholar]
- 8.Guyot LL, Kazmierczak CD, Diaz FG. Vascular injury in neurotrauma. Neurol Res. 2001;23:291–6. doi: 10.1179/016164101101198442. [DOI] [PubMed] [Google Scholar]
- 9.Hiraishi T, Kawaguchi T, Kobayashi T, Tomikawa M, Ito Y, Fujii Y. Unstable stenosis of the internal carotid artery caused by a craniofacial nail-gun injury-case report. Neurol Med Chir (Tokyo) 2009;49:590–3. doi: 10.2176/nmc.49.590. [DOI] [PubMed] [Google Scholar]
- 10.Litvack ZN, Hunt MA, Weinstein JS, West GA. Self-inflicted nail-gun injury with 12 cranial penetrations and associated cerebral trauma. Case report and review of the literature. J Neurosurg. 2006;104:828–34. doi: 10.3171/jns.2006.104.5.828. [DOI] [PubMed] [Google Scholar]
- 11.Olumide AA, Adeloye A. Unusual cranio-cerebral injuries: Report of two cases in Nigerians. Surg Neurol. 1976;6:306–8. [PubMed] [Google Scholar]
- 12.Ravelli V, Forli C, Parenti G. Unusual penetrating craniocerebral injuries. Report of three cases. J Neurosurg Sci. 1987;31:153–6. [PubMed] [Google Scholar]
- 13.Reeves DL. Penetrating craniocerebral injuries. Report of two unusual cases. J Neurosurg. 1965;23:204–5. doi: 10.3171/jns.1965.23.2.0204. [DOI] [PubMed] [Google Scholar]
- 14.Sani S, Jobe KW, Byrne RW. Successful repair of an intracranial nail-gun injury involving the parietal region and the superior sagittal sinus. Case report. J Neurosurg. 2005;103:567–9. doi: 10.3171/jns.2005.103.3.0567. [DOI] [PubMed] [Google Scholar]
- 15.Selvanathan S, Goldschlager T, McMillen J, Campbell S. Penetrating craniocerebral injuries from nail-gun use. J Clin Neurosci. 2007;14:678–83. doi: 10.1016/j.jocn.2006.02.017. [DOI] [PubMed] [Google Scholar]
- 16.Shenoy SN, Raja A. Unusual self-inflicted penetrating craniocerebral injury by a nail. Neurol India. 2003;51:411–3. [PubMed] [Google Scholar]
- 17.Son S, Kang DH, Kim BH, Choi NC. Incidentally discovered a self-inflicted a nail in the brain of schizophrenia patient. Psychiatry Investig. 2011;8:272–4. doi: 10.4306/pi.2011.8.3.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Spennato P, Bocchetti A, Mirone G, Savarese L, Squillante D, Rotondo M, et al. Double concentric craniotomy for a craniocerebral penetrating nail. Case report and technical note. Surg Neurol. 2005;64:368–71. doi: 10.1016/j.surneu.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 19.Weil AG, Weill A, Li M, Shédid D. Low-energy penetrating nail injury through the petrous segment of the ICA. Can J Neurol Sci. 2011;38:649–51. doi: 10.1017/s0317167100012208. [DOI] [PubMed] [Google Scholar]


