Abstract
The incidence of both type 1 and type 2 diabetes (T1DM and T2DM) continues to rise within the pediatric population. However, T1DM remains the most prevalent form diagnosed in children. It is critical that health-care professionals understand the types of diabetes diagnosed in pediatrics, especially the distinguishing features between T1DM and T2DM, to ensure proper treatment. Similar to all individuals with T1DM, lifelong administration of exogenous insulin is necessary for survival. However, children have very distinct needs and challenges compared to those in the adult diabetes population. Accordingly, treatment, goals, and age-appropriate requirements must be individually addressed. The main objectives for the treatment of pediatric T1DM include maintaining glucose levels as close to normal as possible, avoiding acute complications, and preventing long-term complications. In addition, unique to pediatrics, facilitating normal growth and development is important to comprehensive care. To achieve these goals, a careful balance of insulin therapy, medical nutrition therapy, and exercise or activity is necessary. Pharmacological treatment options consist of various insulin products aimed at mimicking prior endogenous insulin secretion while minimizing adverse effects. This review focuses on the management of pediatric T1DM in the outpatient environment, highlighting pharmacotherapy management strategies.
INDEX TERMS: diabetes, medical management, pediatrics, type 1 diabetes
INTRODUCTION
Diabetes is a term used to describe a variety of metabolic diseases in which the pancreas either does not produce enough insulin or the cells in the body do not respond adequately, resulting in high blood glucose values. Although the 2 main types of pediatric diabetes are type 1 diabetes mellitus (T1DM) and type 2 DM (T2DM), the pediatric population is also affected by other types including neonatal diabetes, cystic fibrosis-related diabetes (CFRD), and secondary diabetes. It is critical that healthcare professionals understand the types of diabetes diagnosed in pediatric patients, especially the distinguishing features between type 1 and type 2, to ensure proper treatment. Chronic management strategies of the pediatric patient differ from those of the adult population, and these approaches will be reviewed. In addition, this review uses a patient case to highlight pharmacotherapy management.
TYPE 1 DIABETES IN PEDIATRICS
Incidence and Pathophysiology
The incidence of pediatric diabetes is increasing for both T1DM and T2DM diagnoses.1 Specific to T1DM, it has been estimated by the SEARCH for Diabetes in Youth study, that T1DM was diagnosed in more than 18,000 US youth in 2009.2 Pettitt et al3 estimated there are now almost 167,000 pediatric patients in the United States with T1DM.3
Type 1 Diabetes
T1DM is generally divided into 2 subgroups: autoimmune and idiopathic. A patient's risk for autoimmune diabetes is based on the combination of DR/DQ alleles in the histocompatibility locus of chromosome 6. It is necessary but not sufficient to be at high risk to develop the autoimmune form of diabetes. An environmental trigger is also required to begin the autoimmune process by which killer T cells destroy the pancreatic beta islet cells. Many times, the trigger is unknown; however, viral infections and early nutrition have been identified as potential triggers. The idiopathic subgroup of T1DM is diagnosed when there is no evidence of autoimmunity based on pancreatic or insulin antibodies. In either form, diabetes occurs when there is significant destruction of the insulin-producing beta cells. Consequently, there is an insufficient amount of insulin available to enable glucose to enter cells. Subsequently, increased concentrations of glucose remain in the blood, resulting in hyperglycemia and increased serum osmolality. In order for the kidneys to eliminate glucose, increased consumption of water is necessary to enable kidney filtration, resulting in a cycle of polydipsia and polyuria until insulin is finally administered. Due to the inability of glucose to enter the cells and provide energy secondary to the lack of insulin, other substrates such as fat and protein are metabolized via the tricarboxylic acid cycle. The byproducts of fatty acid metabolism result in ketone body formation. As ketones accumulate, the serum becomes acidic (pH<7.3), and diabetic ketoacidosis (DKA), a potentially life-threatening complication of diabetes, develops. The pulmonary compensatory mechanism attempts to neutralize the acidosis by increasing carbon dioxide production, and the physical signs of tachypnea and ketotic breath4 odor (acetone) are observed. As the acidosis worsens, the child becomes more critically ill, resulting in the possibility of death due to severe acidosis, dehydration, and cerebral edema if not treated rapidly with insulin. After treatment and resolution of DKA, subcutaneous insulin is initiated.
Classification
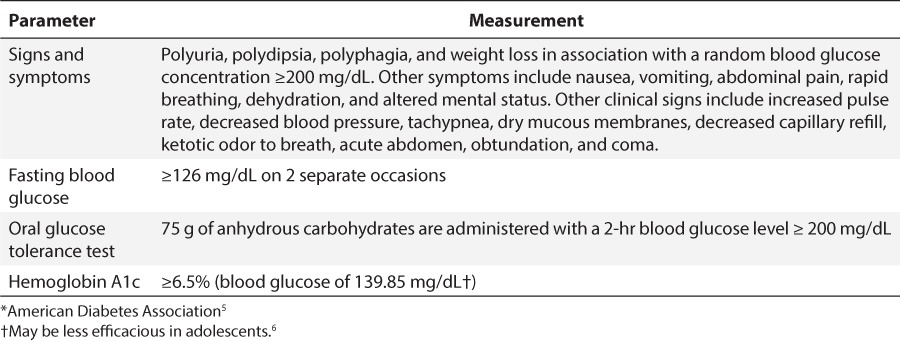
There are 4 criteria with which diabetes can be diagnosed (Table 1).5,6 Only 1 of the 4 criteria is necessary for the diagnosis. Historically, T1DM has been diagnosed based on the classic symptoms along with hyperglycemia. Although we focus on the pharmacological management of T1DM, a brief definition of other pediatric types of diabetes is included to aid the pediatric healthcare practitioners in distinguishing among the various forms.
Table 1.
Diagnostic Criteria for Diabetes *
Type 2 Diabetes
T2DM in children and adolescents share some features similar to those diagnosed in adults, such as a combination of peripheral and hepatic insulin resistance. In addition, there is progressive β-cell destruction leading to insulin deficiency.7 T2DM in children differs from T1DM as follows: insidious versus sudden onset, obese versus normal body mass index phenotype, physical sign of insulin resistance (acanthosis nigricans), versus insulin dependence, typically normal versus very low C-peptide levels, usual lack of pancreatic antibodies, and higher likelihood of a family history of diabetes. The prevalence of T2DM in children and adolescents has increased in the past few decades.1 Compared with adults with T2DM diagnoses, youth experience a much more rapid decline in β-cell function.8 Also atypical of the adult population, up to 25% of youth can present with DKA at the time of diagnosis rather than hyperglycemic hyperosmotic coma (which is rare in the pediatric population).9 In addition to lifestyle modifications, treatment of T2DM in children and adolescents may require insulin or a combination of both insulin (long-acting) and oral medications (such as metformin) or metformin alone.
Differentiating Between Type 1 and Type 2 Diabetes
Differentiating between T1DM and T2DM is important and can be difficult, especially in overweight children. When the diagnosis of T1DM or T2DM is in question, insulin autoantibodies to glutamic acid decarboxylase (GAD-65), islet cell autoantibodies (ICA), and antibodies to tyrosine phosphatase (IC2A) should be obtained. Recently, a new enzyme-linked immunosorbent assay to detect ZnT8 autoantibody is being used. This test can help distinguish those with type 1 diabetes by detecting zinc transporter protein, which is not found in those with T2DM.
Type 1.5 Diabetes
Type 1.5 diabetes is associated with an obese phenotype and laboratory characteristics of both T1DM and T2DM. These children and adolescents may present with DKA and physical characteristics of T2DM (acanthosis nigricans and obesity), as well as positive GAD-65 antibodies. They may require insulin and/or oral agents at different times of the life cycle.
Permanent Neonatal Diabetes
Permanent neonatal diabetes (PNDM) is a rare form of diabetes with an estimated prevalence of 1 in 100,000 to 300,000 live births. In most children with a diagnosis of PNDM before 6 months of age, diabetes is likely to be nonautoimmune and caused by a mutation in 1 of a number of possible genes related to insulin receptors. As a result of deoxyribonucleic acid (DNA) analysis and uncovering the underlying genetic cause, patients with certain forms of PNDM may be treated with orally administered sulfonylureas, enabling the release of endogenous insulin that is associated with significant improvement in A1c and quality of life.10
Cystic Fibrosis-Related Diabetes
CFRD occurs in approximately 20% of adolescents and 40% to 50% of adults with cystic fibrosis.11 Despite sharing features of both T1DM and T2DM, CFRD is a distinct type of diabetes and is caused primarily by decreased insulin secretion from pancreatic islet cells in association with insulin resistance due to acute and chronic illnesses associated with cystic fibrosis. As such, people with CFRD require insulin due to the architectural derangement of the pancreatic islet cells secondary to the mucous plugging associated with cystic fibrosis.
Secondary Causes of Diabetes
Diabetes may also result from other diseases and treatments that decrease insulin secretion or increase insulin resistance. Examples of secondary diabetes include stress-induced hyperglycemia that may eventually result in T1DM or T2DM or medication-induced diabetes from medications such as steroids, antipsychotics, or chemotherapy treatment. The hyperglycemia may resolve once the secondary stress (e.g., illness) has resolved or the medication precipitating hyperglycemia is no longer being used.
MEDICAL MANAGEMENT OF TYPE 1 DIABETES
Pediatric patients, regardless of diabetes type, must be treated and educated differently from adults with diabetes. Diabetes is a lifelong disease that requires constant vigilance and adjustments as pediatric patients progress through childhood. Examples which can highly influence treatment strategies are age at diagnosis, ability of the child to communicate, infant and child eating patterns, sporadic play/activity, pubertal status and development, family dynamics, caregiver involvement in diabetes daily management, psychological adaptation to the diagnosis by both the patient and the caregiver(s), and daycare and school training. Goals of therapy are to maintain normal growth and development and avoid both short- and long-term complications. Striving for an A1c goal of less than 7.5% is currently recommended for all pediatric patients.12 However, individualization is critical, specifically minimizing risk of hypoglycemia or hyperglycemia based on the unique needs of the patient. Children with T1DM should be assessed initially and followed until adulthood by a comprehensive multidisciplinary team and center experienced in addressing the special needs of this population.13
Specific treatment and education for T1DM will vary based on the type of diabetes. However, for most children with diabetes, T1DM is the most prevalent form. There are 3 main components for the treatment of T1DM: medical nutrition therapy (MNT), exercise or activity, and medication management. Each component can influence overall outcomes. All 3 components must be evaluated by the healthcare practitioner when making medication changes.
Nonpharmacologic Management
MNT is a critical component of diabetes management regardless of type of diabetes. Overall goals of MNT are near normalization of glucose, blood pressure, lipids, and weight. Consultation with a registered dietician trained in pediatric diabetes, preferably a certified diabetes educator (CDE), is recommended. In T1DM, carbohydrates are the primary determinant of insulin needs. Depending on the insulin regimen prescribed, the MNT typically will be either carbohydrate counting with fixed, prescribed amounts of carbohydrates at each meal and snacks or carbohydrate counting using insulin-to-carbohydrate (I:C) ratios and correction factor (CF) or sensitivity factor (SF) calculations. Which insulin and corresponding MNT regimen is prescribed is determined by overall assessment of the patient and family, optimally by various diabetes team members. Factors to be assessed include how well the patient and caregivers are coping with the new diagnosis of diabetes, basic math abilities, anticipated adherence to the regimen, social factors, and diabetes support in managing the diabetes at home, school, or daycare. Once an insulin regimen and MNT are prescribed, the patients and their families are taught how to count carbohydrates using food labels, measurement of portion sizes, and other resource materials.14 MNT is an integral component of diabetes management in T1DM. In-depth recommendations can be found in the Academy of Nutrition and Dietetics Pediatric Weight Management Evidence-Based Nutrition Guidelines.15
Exercise or routine physical activity is the second treatment component. Regular exercise is important in all individuals with diabetes, regardless of age. Regular activity will improve insulin sensitivity and lipid levels, lower blood pressure, assist in weight loss, and affect the insulin and/or oral medication requirements. In addition, regular activity can reduce stress and enhance overall physiological well being. However, exercise can place individuals with T1DM at increased risk for hyperglycemia (if the patient has insufficient insulin present) or hypoglycemia (as muscles restore glycogen) during and after the exercise. It is common practice to recommend that patients check blood glucose values before, during (if prolonged activity), and after exercise. Increased testing of blood glucose values is critical when new sports activities begin for children. As a general guideline, blood glucose values should be ≥100 mg/dL prior to exercise and not over 300 mg/dL (especially if ketones are present). Testing supplies and quick-acting carbohydrates should always be available to check and treat any low blood glucose values as needed. As expected, activity and exercise will vary dramatically among age groups represented within the pediatric population, thus healthcare professionals should review the type, intensity and duration of activity with all patients to ensure blood glucose values are maintained within the target range.
Pharmacological Management
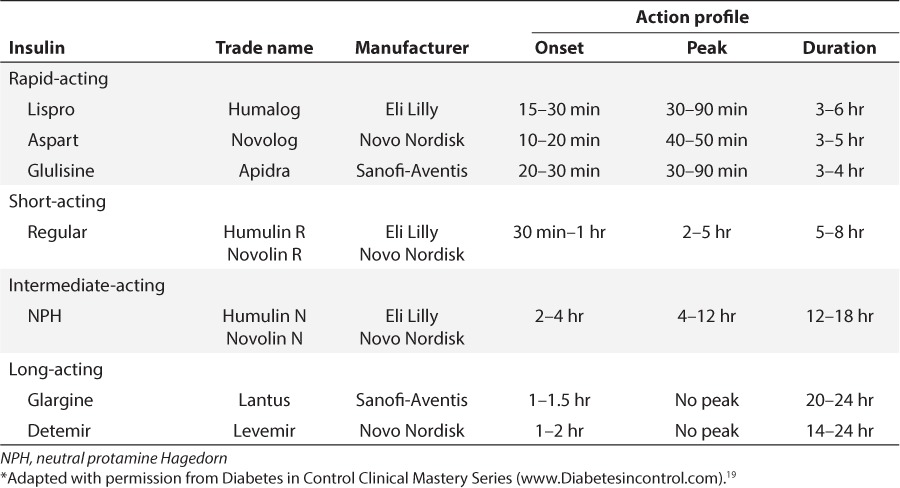
Insulin therapy in T1DM is essential for survival. Insulin therapy should most closely mimic normal physiological insulin secretion based on age, weight, and stage of growth and development. Insulin treatment recommendations can be achieved by using various insulin regimens from a variety of insulin products, pens, or pumps.16–18 Table 2 lists common insulin products available in the United States and their pharmacokinetic parameters for use in the management of pediatric patients.19 Premixed insulin products should not be recommended except in very limited situations, such as an adolescent who refuses injections and the parent/caregiver cannot mix insulin products despite rigorous diabetes team efforts to facilitate optimal diabetes care. Humulin R U-500 (concentrated), although approved for children with T1DM and able to improve glycemic control as an adjunct to diet and exercise, is rarely used in pediatric patients as few require over 200 units of insulin/day.
Table 2.
Pharmacokinetic Parameters of Insulin Commonly Used in Pediatrics in the United States *
In overweight adolescents with T1DM, studies evaluating the efficacy and safety of metformin as add-on therapy to insulin have been conducted and published.20–23 Some of these studies were limited by small numbers, short duration and low doses of metformin. Ongoing research is needed to further determine potential benefits vs. risk before routine use can be recommended in poorly controlled overweight adolescents with T1DM. Several other ongoing clinical trials are evaluating the use of other oral agents in children that are commonly used in the adult population.24
Insulin Requirements in T1DM
In children 9 months to 2 years of age, a reasonable total daily dose (TDD) would be 0.25 to 0.5 units/kg/day. Children between 1 and 6 years of age who do not present in DKA should receive approximately 0.5 to 0.6 units/kg/day insulin. For children presenting in DKA, it may be necessary to start at 1 unit/kg/day insulin, in view of glucose toxicity. From >7 years of age until the onset of puberty, children typically require 0.75 units/kg/day. A starting, estimated range from 0.75 to 1.5 units/kg/day of insulin (or more in some situations) may be necessary during puberty and during other times of stress and illness. Insulin dosage adjustments are based upon blood glucose values reviewed each day or every few days. This is often referred to as pattern management (i.e., evaluation of fasting pre-breakfast, pre-lunch, pre-dinnertime and bedtime blood glucose values). During the “honeymoon” phase, a period that can range from days to weeks after the initial diagnosis of T1DM, β cell function improves as shown by decreased exogenous insulin requirements. As such, insulin doses during this phase will vary tremendously and may need to be decreased quickly based upon blood glucose review. Data suggest that maintaining a very low dose of basal insulin (0.2 to 0.6 units/kg/day) during the honeymoon phase may preserve β-cell function.25 During the honeymoon phase, monitoring of blood glucose values must continue, although not necessarily 4 to 6 times per day. Once the honeymoon phase has ended, blood glucose values may abruptly increase (due to waning of the honeymoon phase), with insulin requirements going back to similar doses prescribed at diagnosis.
Common Insulin Regimens
Basal bolus therapy (also referred to as intensive insulin management [IIM] or multiple daily injections [MDI]) is currently considered the standard approach to the treatment of pediatric diabetes as a result of the Diabetes Complications and Control Trial (DCCT) and follow-up EDIC.26,27 The DCCT demonstrated that the earlier IIM was initiated (i.e., before chronic complications were evident), the more effective the therapy would be, resulting in positive and lasting benefits. This regimen, which most closely mimics normal physiological insulin production prior to diabetes, uses basal and bolus insulin products with I:C ratios and CF or SF. An I:C ratio describes how many units of rapid-acting insulin the patient should inject for a set amount (grams) of carbohydrates. SF or CF typically are used interchangeably. CF or SF is the estimated amount 1 unit of rapid-acting insulin will lower the blood glucose level (in milligrams per deciliter). Basal insulin maintains glucose levels within the desired target range when the patient is not eating and prevents hepatic gluconeogenesis. Bolus insulin prevents postprandial glucose elevations. In most pediatric patients, both long-acting insulins and all 3 rapid-acting insulin analogs have been demonstrated to be effective. The reader is referred to the specific manufacturers for detailed product information.
Continuous subcutaneous insulin infusion (CSII), also known as insulin pump therapy, is considered a form of intensive insulin therapy that uses one of the rapid-acting insulin analogs. CSII therapy has been shown to provide reductions in A1c.28 Examples of insulin pump products available include the Minimed Paradigm (Medtronic Diabetes, Northridge, CA), One Touch Ping (Animas Corporation, West Chester, PA), OmniPod (Insulet Corporation, Billerica, MA), ACCU-CHECK Combo (Roche Insulin Delivery Systems, Inc., Fishers, IN), and T-slim (Tandem Diabetes Care, San Diego, CA).16 Pumps can provide multiple doses of insulin without numerous injections. Typical bolus doses of insulin, as well as custom prandial insulin delivery (for high-protein/high-fat meals) can be programmed into the insulin pump. Typically the pump site (or infusion set) is changed every 2 to 3 days. Infusion sets consist of a cannula inserted into the body, plastic tubing (to carry the insulin from the pump to the cannula), and an adhesive which holds the cannula in place on the body. Infusion sets are available in many different designs and combinations of cannula and tubing lengths for different body types, lifestyles, and activity levels. CSII therapy can deliver numerous basal rates throughout the day and night, allow for insulin adjustments when the patient is ill and has increased insulin requirements, allow the user to reduce basal rates of insulin for anticipated low blood glucose values (i.e., after rigorous exercise), and suspend insulin in cases of low blood glucose.29 The decision to use CSII therapy should be determined by the patient, caregivers, and diabetes team. Multiple factors should be considered prior to starting a patient on CSII therapy. Key factors include patients who monitor blood glucose values 4 or more times/day, a strong foundation of diabetes knowledge, specifically the ability to count carbohydrates, and solve diabetes-related issues. Adequate family involvement, demonstrated adherence to previously prescribed diabetes self-care tasks, and appropriate communication and access to their diabetes care team are essential. Lastly, practical concerns such as sufficient health insurance or other financial resources to sustain CSII therapy must be considered (insurance coverage for all diabetes supplies, prescriptions, insulin pumps, and continuous glucose monitors will vary based on the insurance plan, state, and region in the United States). All patients and their parents/primary caregivers must be well trained to perform CSII. If CSII therapy is interrupted due to pump malfunction or improper use, high blood glucose values and ketonemia can develop rapidly.30 Part of CSII therapy is to always have basal and rapid-acting insulin readily accessible to switch to IIM therapy, if necessary, as well as round-the-clock telephone access to the child's diabetes team.
The MiniMed 530G system (Medtronic Diabetes, Northridge, CA) is a first generation artificial pancreas system approved by the US Food and Drug Administration (FDA) in 2013 for the management of diabetes mellitus in persons 16 years of age and older. The system includes an external glucose sensor and insulin pump, transmitter, glucose meter, and therapy management software. Sensor signals are transmitted to the insulin pump and converted into glucose values every 5 minutes. The patient is required to continue testing blood glucose values for both device calibration and management decisions. The unique feature to this system is that it can be programmed to automatically suspend delivery of insulin when the sensor glucose value falls below a predefined threshold value between 60 and 90 mg/dL. The threshold suspend feature is optional; but if turned on, a sensor value below the programmed threshold will result in pump alarm, siren, and suspended insulin delivery. The system is not intended to treat hypoglycemia but rather reduce risk for severe hypoglycemia by alerting the user to immediately check a blood glucose value to determine treatment. During a threshold suspension event in which the pump siren is not heard or addressed by the user, the pump will automatically suspend for 2 hours. Upon completion of the 2-hour suspension, if still without user intervention, the pump will automatically resume basal insulin delivery for another 4 hours. The Automation to Stimulate Pancreatic Insulin Response (ASPIRE) study showed reduced nocturnal hypoglycemia without significant differences in glycated hemoglobin when using sensor augmented insulin pump therapy (SAPT) with threshold suspension compared to SAPT without threshold suspension.31
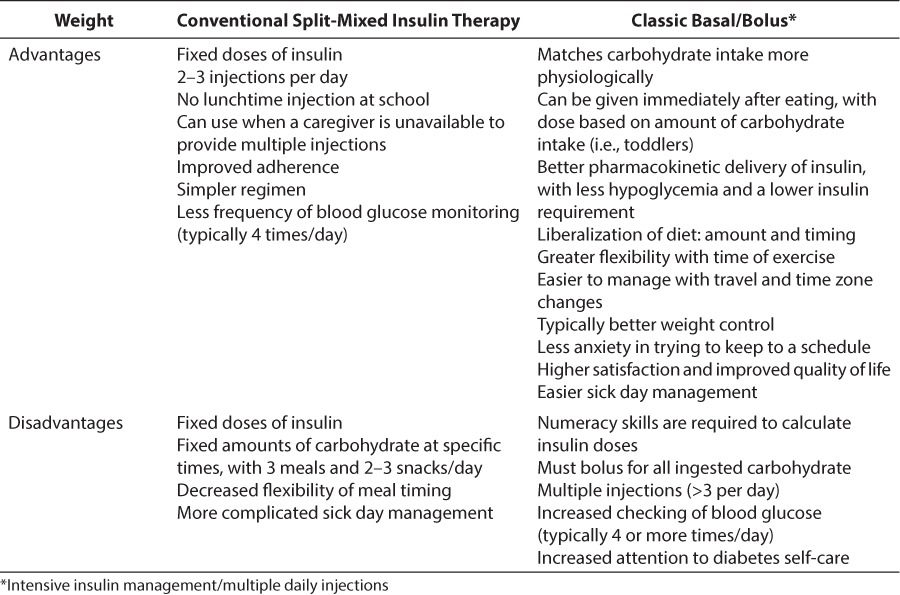
Conventional split-mixed insulin therapy (often referred to as conventional insulin management (CIM), although no longer considered the optimal form of therapy in pediatric T1DM, is still selected for some patients due to underlying unique family/social or economic circumstances that preclude giving insulin at school or the inability to perform intensive self-care skills. Due to these unique situations, healthcare professionals should be aware of this therapy and how to convert patients between various regimens. CIM typically consists of 2 doses of rapid-acting insulin in combination with an intermediate or basal insulin administered twice daily at set times. Insulin is given before breakfast and before dinner, usually 2/3 of the TDD in the morning and 1/3 of the TDD prior to the dinnertime meal. After the child has gone through the honeymoon phase, the dinnertime insulin may be split, with the rapid-acting insulin given at mealtime and the intermediate insulin moved to bedtime. This change moves the peak action of neutral protamine Hagedorn (NPH) to early morning, closer to when the patient is awake and ready to eat. It also correlates with the dawn phenomenon (a rise in the glucose level secondary to growth hormone). Meals and snacks should not be skipped or delayed on this regimen to avoid hypoglycemia. In pediatric practice, where dose adjustments are frequent due to anticipated normal growth and development, individual insulin products are preferred over premixed combination preparations. With this regimen, caregivers must be taught to mix the rapid-acting and intermediate or basal insulin prior to each insulin injection. Patients are instructed to draw up rapid-acting insulin prior to intermediate or basal insulin to avoid contamination of intermediate or basal in the rapid-acting vial, which could affect pharmacokinetic parameters of the insulin. Table 3 differentiates advantages and disadvantages between conventional and basal bolus therapy.
Table 3.
Comparison Between Conventional Split-Mixed Insulin Therapy and Classic Basal Bolus Therapy
Clinical Case Presentation Showing Insulin Dosing Calculations
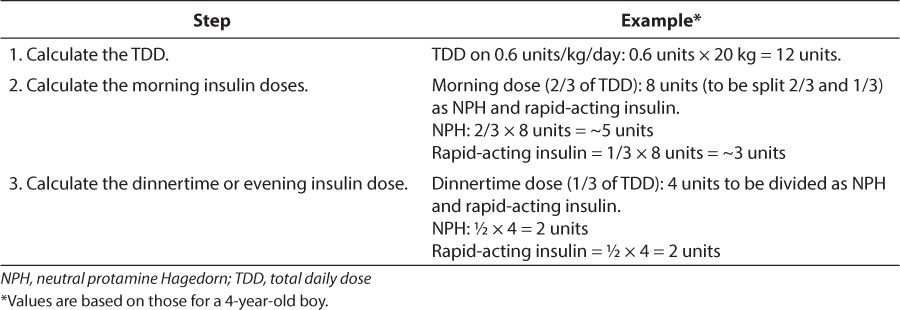
A 4-year-old boy weighing 20 kg presented to his primary care physician with a 2-week history of increased urination, increased drinking, and bedwetting. There was no vomiting. A urinalysis in the office revealed 4+ glucose and trace ketones. A random blood glucose was noted to be 450 mg/dL. His hemoglobin A1c was 10%, reflecting an approximate 3-month estimated blood glucose value of 240 mg/dL. T1DM was diagnosed, and the child was started on subcutaneous insulin. He was initially placed on 2 injections per day of split-mixed conventional insulin (NPH/rapid-acting at breakfast, NPH/rapid-acting at dinnertime), as there was no adult trained to provide insulin at lunch. His carbohydrate amounts were determined (Table 432) and his doses were calculated as follows in Table 5.
Table 4.
Determining Fixed Amounts of Carbohydrates when Using Conventional Split-Mixed Insulin Therapy
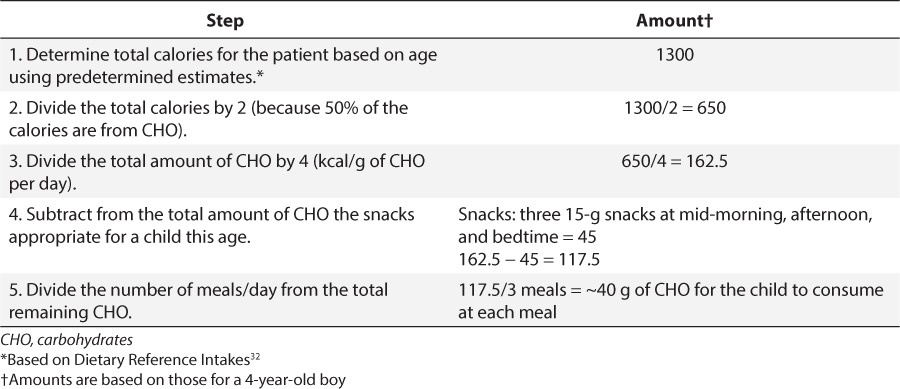
Table 5.
Determining Doses for Conventional Split-Mixed Insulin Therapy
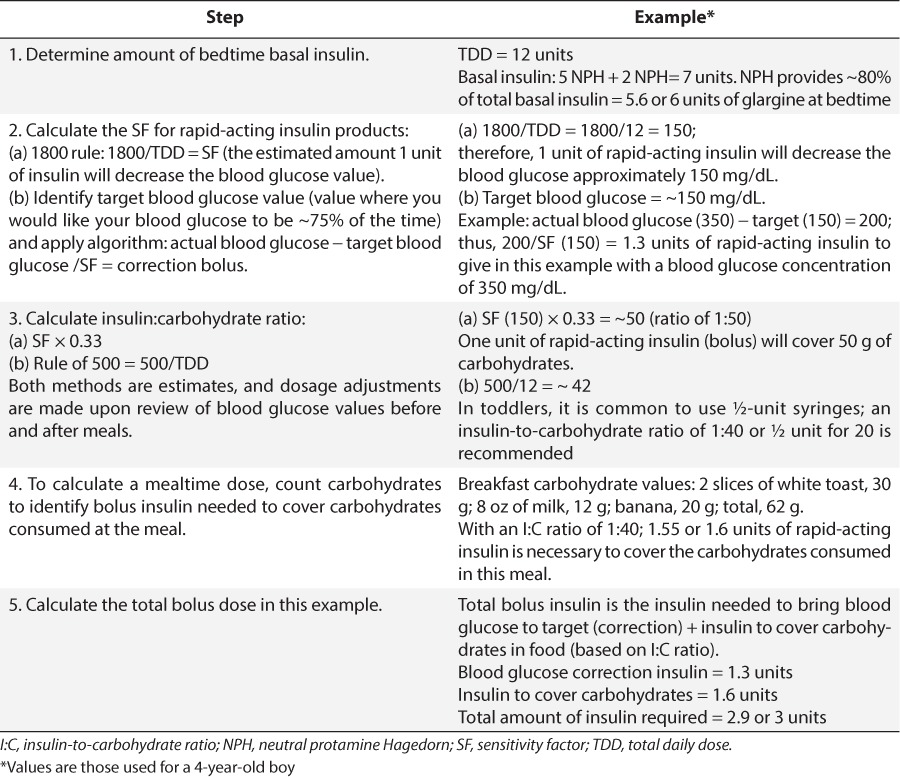
Four months after the diagnosis, the patient was transitioned to classic basal/bolus therapy, when lunchtime insulin administration was no longer an issue, as shown in Table 6. In this example, the I:C ratio was the same throughout the day. However, it is not uncommon for patients to have different I:C ratios for different meals due to hormonal changes (affecting an individual's insulin sensitivity) as well as varying amounts of activity.
Table 6.
Example of Insulin Calculations from Conventional Split-Mixed to Basal Bolus and a Mealtime Insulin Dose
After several months, the child attended diabetes camp and now asks to be transitioned to an insulin pump (CSII). As noted previously, transition to CSII requires increased diabetes self- care skills including frequent blood glucose monitoring, problem solving skills and manual dexterity. Changing the insulin regimen when transitioning from MDI to CSII is relatively easy. The patient's I:C ratio is now 1:30, and CF or SF is 90, both are simply programmed into the pump. To determine the basal rate of the insulin pump, which will now be provided by the rapid-acting insulin, one would take the TDD of glargine (Lantus) the patient injected while on MDI (6 units) and divide by 24 hours; thus programming the pump with a rate of 0.25 units per hour. Insulin dose adjustments can be made quickly based on blood glucose responses gathered from pattern management analysis.
Nonprescription Medications for Diabetes
Despite questions regarding their efficacy and safety, over-the-counter dietary supplements, herbal products, or vitamins are commonly used by the diabetes population.33 Supplements routinely used for diabetes include cinnamon, ginseng, chromium, aloe, bitter melon, Gymnema, fenugreek, and nopal.34 However, within the pediatric diabetes population, data are limited, with the prevalence of supplement use highly variable based on cultural beliefs, study location, and the definition of complementary and alternative medicine (e.g., some studies include prayer, massage, hypnosis).35 There can be tremendous variability in products, some of which have the potential for serious adverse effects or drug interactions.36 Healthcare professionals must routinely inquire about the use of such products and screen for drug interactions, adverse outcomes or negative influences on glycemic control in the pediatric patient where safety and efficacy data is scarce.
Monitoring
Blood glucose monitoring is the cornerstone of diabetes management as it is the only method to evaluate the interplay between the effects and safety of the prescribed insulin regimen, results of carbohydrate consumption and activity. Monitoring, for patients on CIM or IIM therapy, will usually be four or more times per day; pre-breakfast fasting, pre-lunch, pre-dinner and bedtime. In addition, patients will be asked to monitor blood glucose values for a few nights (e.g., 2–3 am) when changing basal insulin rates.
Common glucose monitors used in the pediatric population include the One Touch (Lifescan Inc., Wayne, PA), Freestyle (Abbott, Chicago, IL), Accuchek (Roche Diagnostics, Indianapolis, IN), and Bayer (Bayer Corp., Berkeley, CA) meters.37 These meters include various features that are advantageous for the pediatric population, including a low-blood volume requirement, lancet devices that allow the patient to adjust the depth of insertion, smaller meter size, no coding, and nonfingertip alternative testing options. Although alternate site testing is available, it should not be used when blood glucose values are fluctuating or are above or below target range as accuracy is not as reliable in these situations. Meter features frequently change, and the healthcare team members should ensure meter features best match the patient needs when making recommendations. The meter accuracy varies by about 20% to 30% from serum glucose levels. Therefore, for outpatient management, blood glucose results obtained by meters should be evaluated for patterns appropriate for the specific goals set for the patient.
In an effort to improve blood glucose monitoring by providing moment-to-moment evaluation, continuous glucose monitors using sensors have been developed (Guardian REAL-Time continuous glucose monitoring system (Medtronic Diabetes, Northridge, CA) and DexCom G4 (Dexcom, Inc., San Diego, CA) to measure trends in interstitial glucose. A major benefit of sensors is the ability to observe trends (vs. single points in time) in blood glucose values and make adjustments as needed. Limitations to continuous glucose monitoring are that interstitial glucose readings lag serum blood glucose levels by approximately 20 minutes and calibrations are necessary with routine fingerstick blood glucose readings. New technologies incorporating CSII and glucose sensors are forthcoming. The previously discussed MiniMed 530G with Enlite (Medtronic Diabetes) can suspend insulin delivery when the glucose sensor detects a preset low threshold and the patient does not respond. The ultimate goal of the continuous sensor is to work seamlessly as a closed-loop system with an insulin pump (otherwise known as the artificial pancreas).
In insulin-treated patients, it is essential to understand pattern management strategies, which involve the analysis of blood glucose measurements. In addition to medications, food, and activity, other factors can also influence optimal blood glucose control. A few examples include stress from an infection, surgery/trauma, alcohol, various medications, and hormonal changes such as puberty, menstruation, or pregnancy. It is important to teach patients, along with their parents or caregivers, to review blood glucose values for daily problem solving, especially if values are out of the patient's desired target range. The reader is referred to Cryer who provides expanded guidance on pattern management strategies.38 Basic concepts are to correct hypoglycemia first, followed by fasting blood glucose readings and finally postprandial values.
The A1c level, used to measure glycemic status, represents an approximate 3 month estimated blood glucose average, with 50% weighted toward the last month. Hemoglobinopathies, anemias, and other diseases with rapid blood cell turnover such as CFRD can influence A1c results, typically lowering them, and thus not providing an accurate 3-month estimated blood glucose level. However, in CFRD, based on technology available, although the A1c results do not truly reflect average blood glucose levels, they are obtained to follow the trend of glycemic control.39
Prevention of Complications
Hypoglycemia is of great concern, especially in the pediatric population, and is a major hindrance to obtaining optimal blood glucose control.13 Hypoglycemia is typically considered a blood glucose of ≤ 70 mg/dL.5 Patients may or may not have symptoms. Symptoms may be difficult to detect, especially in the very young; thus, checking the blood glucose level is critical when hypoglycemia is suspected. Parents and children often fear hypoglycemia, especially if the child has had a seizure in the past due to a low blood glucose level. Even mild hypoglycemia can result in altered cognitive function.13 Detailed instruction must be provided to educate the patient, family and other caregivers on classic signs of hypoglycemia and its treatment. Symptoms can include: shaking, sweating, excessive hunger, irritability, headache, dizziness, sudden outbursts or mental status changes. Nocturnal symptoms may include nightmares, restless sleep, profuse sweating, and morning headache. The “Rule of 15” is a commonly taught method to treat low blood glucose values.40 The guidelines instruct that if a low blood glucose value is obtained, treat with 15 g of quick-acting carbohydrate (CHO), that is 4 oz. (1/2 cup) of fruit juice, regular soda or 3 to 4 glucose tablets. Recheck the blood glucose in 15 minutes and repeat treatment if the blood glucose is below target. Continue this process until the blood glucose is above target. Once above target, if the patient will not be eating a meal in the next few hours, have another ~15–20 g of complex CHO with protein (e.g., peanut butter crackers, ½ a meat sandwich). The goal of this additional CHO and protein snack is to avoid another low blood glucose value prior to the next meal. In cases of severe hypoglycemia with loss of consciousness or seizure, glucagon should be administered. Once any hypoglycemic event is resolved, the patient, parents, and/or healthcare practitioners should employ problem-solving skills to determine the cause of the low blood glucose value(s) (e.g., gave excess insulin, additional vigorous activity, did not consume enough CHO).
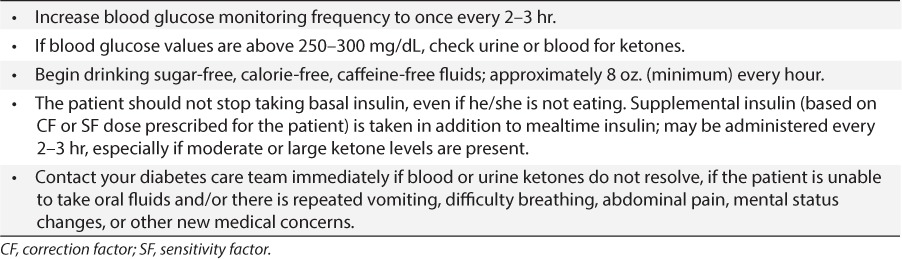
Hyperglycemia, which can quickly lead to DKA, is also an acute complication of T1DM. Guidelines for home management of elevated blood glucose value are summarized in Table 7. Urine ketone strips (foil wrapped) as well as blood ketone meters (Precision Extra; Abbott, Chicago, IL) and Nova Max Plus (Nova Diabetes Care, Waltham, MA) are available to measure ketones to help recognize the beginning of DKA.
Table 7.
Typical Guidelines for the Home Management of Elevated Blood Glucose
Elimination and/or minimization of long-term complications of diabetes (hypertension, dyslipidemia, retinopathy, and nephropathy) should be addressed at routine clinic visits for all patients.5 In addition; associated autoimmune conditions such as thyroid disease and celiac disease should be screened at diagnosis and periodically thereafter based on standards of practice. Ophthalmological screening should be conducted in children 10 and older or 3 to 5 years after T1DM diagnosis; annually thereafter.13 Yearly screening for microalbuminuria should start at age 10 and in those who have had diabetes for 5 years.
Education
Regardless of the type of therapy prescribed, education with subsequent implementation of the diabetes care plan is paramount to the long-term success of pediatric diabetes management and outcomes. While education can be delivered in a variety of ways, the optimal approach involves multidisciplinary pediatric teams, including CDE, experienced in the treatment and care of this population. The presentation of information must be tailored to the cognitive and developmental abilities of the child or adolescent and at least one parent/caregiver, but ideally incorporates the entire family.12,13 Education should follow a comprehensive curriculum that is age and diagnosis appropriate.40 Each curriculum should include the following content areas: disease process, MNT, the importance of exercise, proper use of medications, proper procedures for monitoring devices, pattern management analysis for home use as appropriate, prevention and detection of acute and chronic complications, psychosocial issues, and behavioral change strategies.41
Transition Issues
As young adults with T1DM get ready to transition from pediatric diabetes care providers to adult care providers, numerous challenges arise where healthcare professional can provide assistance. Young adults in general, regardless of diabetes, may participate in risky behaviors during adolescence and young adulthood. Such behaviors may include the use of tobacco, recreational drugs, unprotected sexual intercourse, and the use of alcohol. High-risk behaviors can be of particular concern in individuals with diabetes and should be addressed starting in the pediatric clinical care environment. In addition, conversations about insurance, finances, how to obtain critical diabetes prescriptions, and safety concerns with driving and hypoglycemia must be addressed in young adults with diabetes.42
Future Possibilities for Management
Exciting research for the management of T1DM is ongoing. At this time, the closed-loop artificial pancreas appears promising.43 Stem cell-derived cells have been recently designed to replace lost insulin-producing ability.44 Lastly, continued efforts are being made to improve existing devices and products (e.g., blood glucose meters, sensors, size of needles for injecting insulin) that patients use each day in their diabetes management.
CONCLUSIONS
T1DM management in the pediatric population is complex. Providing the best care to a patient living with diabetes requires a collaborative model involving various healthcare professionals. All healthcare professionals should embrace participation in the pediatric multidisciplinary team for therapy management as well as the ongoing education and training of patients and their families with T1DM.
ACKNOWLEDGMENT
The authors acknowledge the editorial assistance of Cindy Orticio, freelance editor, Dallas, Texas.
ABBREVIATIONS
- ASPIRE
Automation to Stimulate Pancreatic Insulin Response
- CDE
certified diabetes educator
- CF
correction factor
- CFRD
cystic fibrosis–related diabetes
- CHO
carbohydrate
- CIM
conventional insulin management
- CSII
continuous subcutaneous insulin infusion
- DCCT
Diabetes Complications and Control Trial
- DNA
deoxyribonucleic acid
- DKA
diabetic ketoacidosis
- EDIC
Epidemiology of Diabetes Interventions and Complications Trial
- FDA
Food and Drug Administration
- GAD-65
glutamic acid decarboxylase
- A1c
hemoglobin A1c
- IAA
insulin autoantibodies
- I:C
insulin-to-carbohydrate ratio
- ICA
islet cell autoantibodies
- ICA2
antibodies to tyrosine phosphatase
- IIM
intensive insulin management
- MDI
multiple daily injections
- MNT
medical nutrition therapy
- NPH
isophane protamine Hagedorn
- PNDM
permanent neonatal diabetes
- SAPT
sensor augmented insulin pump therapy
- SF
sensitivity factor
- T1DM
type 1 diabetes mellitus
- T2DM
type 2 diabetes mellitus
- TDD
total daily dose
Footnotes
Disclosures Drs. Beck and Cogen declare no conflicts or financial interest in any product or service mentioned in the manuscript, including grants, equipment, medications, employment, gifts, and honoraria.
REFERENCES
- 1.Dabelea D, Mayer-Davis E, Saydah S et al. SEARCH for Diabetes in Youth study. JAMA. 2014;311:1778–1786. [Google Scholar]
- 2.Lawrence JM, Imperatore G, Pettitt DJ. Incidence of diabetes in US youth by type, race/ethnicity, and age, 2008–2009. Diabetes. 2014;63(suppl.1):A407. et al.; SEARCH for Diabetes in Youth Study Group. [Google Scholar]
- 3.Pettitt DJ, Talton J, Dabelea D et al. SEARCH for Diabetes in Youth Study Group. Prevalence of diabetes in US youth in 2009: the SEARCH for Diabetes in Youth Study. Diabetes Care. 2014;37:402–408. doi: 10.2337/dc13-1838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nelson DL, Lehninger AL, Cox MM. Lehninger principles of biochemistry. 4th ed. New York: WW Freeman; 2005. The Henderson-Hasselbalch equation relates pH, p K a, and buffer concentration; pp. 66–67. p. [Google Scholar]
- 5.American Diabetes Association. Standards of medical care in diabetes. Diabetes Care. 2014;37(suppl 1):S14–S80. doi: 10.2337/dc14-S014. [DOI] [PubMed] [Google Scholar]
- 6.Lee JM, Wu EL, Tarini B et al. Diagnosis of diabetes using hemoglobin A1c: should recommendations in adults be extrapolated to adolescents? J Pediatr. 2011;158:947–952. e1–3. doi: 10.1016/j.jpeds.2010.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Copeland KC, Silverstein J, Moore KR et al. Management of newly diagnosed type 2 diabetes mellitus (T2DM) in children and adolescents. Pediatrics. 2013;131:364–382. doi: 10.1542/peds.2012-3494. [DOI] [PubMed] [Google Scholar]
- 8.Bacha F, Gungor N, Lee S et al. Progressive deterioration of β-cell function in obese youth with type 2 diabetes. Pediatr Diabetes. 2013;14:106–111. doi: 10.1111/j.1399-5448.2012.00915.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gungor N, Hannon T, Libman I et al. Type 2 diabetes mellitus in youth: the complete picture to date. Pediatr Clin North Am. 2005;52:1579–1609. doi: 10.1016/j.pcl.2005.07.009. [DOI] [PubMed] [Google Scholar]
- 10.Støy J, Greeley SA, Paz VP et al. Diagnosis and treatment of neonatal diabetes: a United States experience. Pediatr Diabetes. 2008;9:450–459. doi: 10.1111/j.1399-5448.2008.00433.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moran A, Dunitz J, Nathan B et al. Cystic fibrosis-related diabetes: current trends in prevalence, incidence, and mortality. Diabetes Care. 2009;32:1626–1631. doi: 10.2337/dc09-0586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chiang JL, Kirkman MS, Laffel LMB. Type 1 diabetes through the life span: a position statement of the American Diabetes Association. Diabetes Care. 2014;37:2034–2054. doi: 10.2337/dc14-1140. et al.; Type 1 Diabetes Sourcebook Authors. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Silverstein J, Klingensmith G, Copeland K et al. Care of children and adolescents with type 1 diabetes: a statement of the American Diabetes Association. Diabetes Care. 2005;28:186–212. doi: 10.2337/diacare.28.1.186. [DOI] [PubMed] [Google Scholar]
- 14.Borushek A. CalorieKing calorie, fat and carbohydrate counter. 2013 ed. Hudsonville, MI: Family Health Publications; 2012. [Google Scholar]
- 15.American Dietetic Association. Pediatric Weight Management Evidence-Based Nutrition Practice Guideline. Chicago: American Dietetic Association; 2007. [Google Scholar]
- 16.Bangstad HJ, Danne T, Deeb LC et al. International Society for Pediatric and Adolescent Diabetes. ISPAD clinical practice consensus guidelines 2006–2007. Insulin treatment. Pediatr Diabetes. 2007;8:88–102. doi: 10.1111/j.1399-5448.2007.00233.x. [DOI] [PubMed] [Google Scholar]
- 17.Neithercott T. The basics of insulin pumps. Diabetes Forecast. 2014;67:58–63. [PubMed] [Google Scholar]
- 18.Berg E. Insulin pens. These devices bring grab-and-go convenience to taking shots. Diabetes Forecast. 2014;67:68–69. [PubMed] [Google Scholar]
- 19.Medication, insulin, diabetes clinical mastery series issue. http://www.diabetesin-control.com/articles/56-/16551-updated-comprehensive-list-of-insulins Assessed October 30, 2014.
- 20.Hamilton J, Cummings E, Zdravkovic V et al. Metformin as an adjunct therapy in adolescents with type 1 diabetes and insulin resistance: a randomized controlled trial. Diabetes Care. 2003;26:138–143. doi: 10.2337/diacare.26.1.138. [DOI] [PubMed] [Google Scholar]
- 21.Sarnblad S, KIroon M, Aman J. Metformin as additional therapy in adolescents with poorly controlled type 1 diabetes: randomized placebo-controlled trial with aspects on insulin sensitivity. Eur J Endocrinol. 2003;149:323–329. doi: 10.1530/eje.0.1490323. [DOI] [PubMed] [Google Scholar]
- 22.Nadeau KJ, Chow K, Alam S et al. Effects of low dose metformin in adolescents with type 1 diabetes mellitus: a randomized, double-blinded placebo-controlled study. Pediatr Diabetes. 2015;16:196–203. doi: 10.1111/pedi.12140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Konrad K, Datz N, Engelsberger I for the German/Austrian DPV Initiative. Current use of metformin in addition to insulin in pediatric patients with type 1 diabetes mellitus: an analysis based on a large diabetes registry in Germany and Austria. Pediatr Diabetes. 2014. doi:10.1111/pedi.12203. [DOI] [PubMed]
- 24.Vaidyanathan J, Choe S, Sahajwalla CG. Type 2 diabetes in pediatrics and adults: thoughts from a clinical pharmacology perspective. J Pharm Sci. 2012;101:1659–1671. doi: 10.1002/jps.23085. [DOI] [PubMed] [Google Scholar]
- 25.Aly H, Gottlieb P. The honeymoon phase: intersection of metabolism and immunology. Curr Opin Endocrinol Diabetes Obes. 2009;16:286–92. doi: 10.1097/MED.0b013e32832e0693. [DOI] [PubMed] [Google Scholar]
- 26.Diabetes Control and Complications Trial Research Group. Effect of intensive diabetes treatment on the development and progression of long-term complications in adolescents with insulin-dependent diabetes mellitus: Diabetes Control and Complications Trial. J Pediatr. 1994;125:177–188. doi: 10.1016/s0022-3476(94)70190-3. [DOI] [PubMed] [Google Scholar]
- 27.White NH, Cleary PA, Dahms W et al. Beneficial effects of intensive therapy of diabetes during adolescence: outcomes after the conclusion of the Diabetes Control and Complications Trial (DCCT) J Pediatr. 2001;139:804–812. doi: 10.1067/mpd.2001.118887. [DOI] [PubMed] [Google Scholar]
- 28.Beck RW, Tamborlane WV, Bergenstal RM et al. The T1D Exchange Clinic Registry. J Clin Endocrinol Metab. 2012;97:4383–4389. doi: 10.1210/jc.2012-1561. [DOI] [PubMed] [Google Scholar]
- 29.Choudhary P, Shin J, Evans ML et al. Insulin pump therapy with automated insulin suspension in response to hypoglycemia. Diabetes Care. 2011;34:2023–2025. doi: 10.2337/dc10-2411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Orsini-Federici M, Akwi JA, Canonico V et al. Early detection of insulin deprivation in continuous subcutaneous insulin infusion-treated patients with type 1 diabetes. Diabetes Technology Ther. 2006;8:67–75. doi: 10.1089/dia.2006.8.67. [DOI] [PubMed] [Google Scholar]
- 31.Bergenstal RM, Klonoff DC, Garg SK. Threshold-based insulin-pump interruption for reduction of hypoglycemia. N Engl J Med. 2013;369:224–232. doi: 10.1056/NEJMoa1303576. et al. for the ASPIRE In-Home Study Group. [DOI] [PubMed] [Google Scholar]
- 32.Institute of Medicine, Food and Nutrition Board. Dietary Reference Intakes for Energy, Carbohydrates, Fiber, Fat, Fatty Acids, Cholesterol, Protein and Amino Acids. Washington DC: National Academies Press; 2005. [Google Scholar]
- 33.Yeh GY, Eisenberg DM, Davis RB et al. Use of complementary and alternative medicine among persons with diabetes mellitus: results of a national survey. Am J Public Health. 2002;92:1648–1652. doi: 10.2105/ajph.92.10.1648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Geil P, Shane-McWhorter L. Dietary supplements in the management of diabetes: potential risks and benefits. J Am Diet Assoc. 2008;108(suppl 1):S59–S65. doi: 10.1016/j.jada.2008.01.020. [DOI] [PubMed] [Google Scholar]
- 35.Miller JL, Dingcai C, Miller JG et al. Correlates of complementary and alternative medicine use in Chicago area children with diabetes. Prim Care Diabetes. 2009;3:149–156. doi: 10.1016/j.pcd.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 36.Kessler RC, Davis RB, Foster DF et al. Long-term trends in the use of complementary and alternative medical therapies in the United States. Ann Intern Med. 2001;135:262–268. doi: 10.7326/0003-4819-135-4-200108210-00011. [DOI] [PubMed] [Google Scholar]
- 37.Wahowiak L. Blood glucose meters. What to look for—and what to know. Diabetes Forecast. 2014;67:42–52. [PubMed] [Google Scholar]
- 38.Cryer PE. Hypoglycemia in Diabetes: Patho-physiology, Prevalence, and Prevention. 1st ed. Alexandria, VA: American Diabetes Association; 2009. p. 171. [Google Scholar]
- 39.Moran A, Brunzell C, Cohen RC et al. Clinical care guidelines for cystic fibrosis-related diabetes: a position statement of the American Diabetes Association and a clinical practice guideline of the Cystic Fibrosis Foundation, endorsed by the Pediatric Endocrine Society. Diabetes Care. 2010;33:2697–2708. doi: 10.2337/dc10-1768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chase HP. Understanding Diabetes: a Handbook for People Who Are Living With Diabetes. Denver, CO: Paros; 2006. [Google Scholar]
- 41.Haas L, Maryniuk M, Beck J et al. National standards for diabetes self-management education and support. Diabetes Care. 2012;35:2393–2401. doi: 10.2337/dc12-1707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Peters A, Laffel L, American Diabetes Association Transitions Working Group Diabetes care for emerging adults: recommendations for transition from pediatric to adult diabetes care systems: A position statement of the American Diabetes Association. Diabetes Care. 2011;34:2477–2485. doi: 10.2337/dc11-1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Thabit H, Hovorka R. Closed-loop insulin delivery in type 1 diabetes. Endocrinol Metab Clin N Am. 2012;41:105–117. doi: 10.1016/j.ecl.2011.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Krishnan R, Alexander M, Robles L et al. Islet and stem cell encapsulation for clinical transplantation. Rev Diabet Stud. 2014;11:84–101. doi: 10.1900/RDS.2014.11.84. [DOI] [PMC free article] [PubMed] [Google Scholar]


