Abstract
Healthcare professionals can be confronted with a wide range of ethical and regulatory issues in today’s ever-changing practice environments. While achieving best practice standards, physical therapists may need to compromise what is best for patients due to fiscally driven rules, regulations, and limited benefits. Scenarios may surface where ethical issues and associated dilemmas become paramount between what is versus what should be. A challenge that should be in the forefront of professional endeavors is staying current with published rules, regulations, and conditions of participation, as applied to various practice models and environments while still adhering to ethical codes. Knowing and utilizing available resources especially American Physical Therapy Association (APTA), websites, documents, and references can strengthen practice patterns and treatment options.
Keywords: Ethical issues, Physical therapy, Practice dilemmas, Physical therapy, Avoiding regulatory fraud/abuse, Physical therapy, Billing practices, Practice scenarios, Patients with limited benefits
Introduction
Healthcare professionals are confronted with a range of ethical and regulatory issues in today’s ever-changing practice environments. Doing what is best for the patient is often influenced and, at times, compromised by external factors, including rules and regulations associated with third party payment systems. Medicare, Medicaid, and commercial carriers have established conditions of participation and fiscally driven regulations, such as payment caps that often direct practice parameters and may affect patient care outcomes. Providing optimal care for a given patient may be compromised by limited benefits. Physical therapists need to know available options and develop strategies that consider best practice within the confines of contemporary payment systems. Ethical issues may confront practitioners that can create dilemmas between what is and what should be.
Where the rubber hits the road
Physical therapists follow the Guide to Physical Therapist Practice [1], American Physical Therapy Association (APTA), and state-directed practice laws in their quest to provide best care for patients. Physical therapists are also team members in a delivery model for patients with rheumatic diseases and musculoskeletal conditions. Other team members may include rheumatologists, orthopedic surgeons, nurses, occupational therapists, social workers, pharmacists, and psychologists just to name a few. In addition, physical therapists practice in a wide range of delivery system models including academic, hospital-based, home health, and private office practices. Rules, expected behaviors, and priorities often vary across these systems and cultures and are subject to change.
Altering established practice patterns to accommodate changing rules and regulations can be challenging and may raise ethical questions. For example, is it acceptable to implement a plan of care that falls outside limits allowed by fiscal intermediaries? If a patient requires intensive physical therapy for an “impending” frozen shoulder, but has inadequate insurance to cover the cost, how can his physical therapist uphold a core principle of APTA’s code of ethics that states “Physical Therapists shall adhere to the core values of the profession and shall act in the best interests of patients/clients over the interests of the physical therapist” [2]? Does this imply that such a patient should be treated without charge or at a reduced charge? While that might be a tempting solution (and while the APTA’s code of ethics encourages pro bono care for patients who cannot afford care), Medicare regulations [3] require that all patients shall be billed in accordance to the Centers for Medicare and Medicaid Services (CMS) fee methodology without consideration to patients’ ability to pay.
Changing rules and regulations
Examples of major changes in health care delivery in physical therapy followed the startup of Medicare and Medicaid in 1965 and in 1982 with diagnostic-related group (DRG) payment systems. More recently, physical therapists are experiencing another layer of regulations that require Physician Quality Reporting System (PQRS) [4] within a capped payment system. Understanding the rules and regulations and avoiding mistakes that might be considered “fraud” are paramount.
What are the driving forces, principles, and guidelines that shape professional behaviors and ethical standards? “Right” and “wrong” behaviors are at the forefront of current and future professional endeavors. In physical therapy, the literature is rich with texts and publications [5–8] that address “ethics in physical therapy” Purtillo et al. [5] emphasize that “the goal of professional ethics is to arrive at a caring response in situations you encounter in the course of carrying out your professional role and its functions.” Gabard et al. [8] states, “Ethics is the heart of professionalism. Just as much as technical skills, moral commitment enables physical therapists to provide quality services for patients, work effectively with colleagues, and maintain the trust of the public.” The APTA is also a preferred resource for members to understand the profession’s position on sound ethical behavior, such as core documents and publications [1, 2] Meeting behavioral standards and doing the right thing are also based upon the moral fabric that each of us brings to our individual profession and patient encounter. Not knowing the laws, rules, and ethical codes is not an excuse for a lapse. Knowing their scope and associated relationships build confidence in taking the right course of action.
The following schematic can be valuable when confronted with ethical and legal questions. In addition to these helpful references, fiscal intermediaries publish rules and regulations with associated payment criteria that need to be a component of the therapist’s playbook. The playbook changes often and staying current is a hallmark of professionalism. Note that the patient is at the center of focus.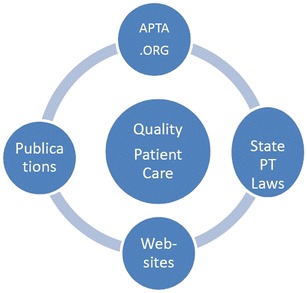
APTA members can use APTA.org as a valuable resource. The following documents are helpful toward avoiding “fraud, waste, and abuse” and gaining understanding of the changes and opportunities associated with the Affordable Care Act.
Core documents www.apta.org/Policies/CoreDocuments/—This site features links to APTA code of ethics, Guide to Physical Therapist Practice, and Guide for Conduct and Professionalism.
Coding and billing www.apta.org/Payment/CodingBilling/—This site includes links to courses (see http://learningcenter.apta.org and http://www.apta.org/Courses/Online/NavigatingCompliance/ for examples).
Compliance www.apta.org/Compliance/—This site offers information on fraud and abuse and Medicare audits.
Managed care contracting tool kit www.apta.org/Payment/Privateinsurance/ManagedCareContractingToolkit/.
PT in motion www.apta.org/PTinMotion/2014—A number of articles are available regarding ethical, compliance, and documentation issues.
The federal government’s websites and the Federal Registry also publish changes in rules and regulations that affect physical therapy. For example, the US Department of Health and Human Services CMS publishes documents [9] that provide an overview of facts and laws regarding Medicare and Medicaid conditions of participation.
Even when clinicians are diligent in learning and staying abreast of changing rules that affect practice, circumstances may present that create the need for legal counsel and services. This is especially true when engaging in contracts with agencies and fiscal intermediaries. Professionally designed contracts that are clear and that capture the intended terms and conditions of both parties promote understanding and may avoid further legal action.
In addition to knowing and following preferred practice guidelines, physical therapists can face Medicare audits and compliance issues associated with documentation, coding, and billing procedures. This is particularly difficult to reconcile as regulatory changes are seemingly based on pressures to cut costs, measure efficiencies, and with demands to prove the value of treatment interventions. Consequently, changes in regulations without ethical content complicate the way healthcare is now being organized and financed. This changing environment places the patient and service provider in a difficult position as illustrated by the following scenario:
A 56 year-old man is referred to physical therapy for sciatica, degenerative disc disease, and degenerative joint disease. He is the sole caretaker for his disabled wife. Over the last month he has lost his capacity to bend, lift and carry during activities of daily living and work. While registering at the Outpatient Rehabilitation Center he learns that his Medicaid benefits only provide for a PT evaluation but without any follow up services.
Upon completing the initial examination, the physical therapist considers treatment options given the identified impairments and loss of function, including manual therapy for the lower lumbar spine, stabilization and strengthening exercises for the low back and trunk, and instruction in a home exercise program and proper body mechanics. The physical therapist recommends follow-up twice a week for 4 weeks. However, given the limitations of the patient’s insurance benefits, these additional treatments will not be covered.
How should the physical therapist proceed? Should the patient be asked to pay out of pocket for optimal care or proceed with only the evaluation that is covered? Should the patient be offered free or discounted services because it “seems like the right thing to do”?
In the future, physical therapists will need to use alternatives to traditional duration and frequency care models to address changing rules. Educating patients and gaining their compliance with home exercises are necessary yet challenging for clients who have limited rehabilitation benefits. Physical therapists are currently looking to non-traditional initiatives such as TeleHealth and promoting the use of technology including smartphones and electronic communications. However, payment for such services is currently variable and usage is limited. Going forward, practitioners will need to provide links to quality educational resources and develop user-friendly educational tools basic to achieving success for disadvantaged patients without adequate rehabilitation benefits.
In today’s practice environments there are a variety of stakeholders with differing and sometimes conflicting values and priorities. Physical therapists often identify high-quality patient care, professional values, and self-fulfillment as motivators toward professional growth and satisfaction. Conversely, an organization managing or paying for healthcare services may prioritize fiscal viability, institutional efficiency, and competitive positioning in the marketplace. If management directs or encourages double booking to increase profitability, the physical therapist should not double book (treat two patients within the same timeframe), especially for Medicare patients to avoid a breach of federal regulations. As described by Scott in his text defining “situational ethics” [6] by doing so, the physical therapist raises the question, does violating federal law in this case also carry over to a breach of APTA ethics? Is this a special situation of blending a violation of billing standards via Medicare and APTA’s code of ethics that states in principle 2 “Physical Therapists comply with the laws and regulations governing the practice of physical therapy” [2]? In conclusion, this is but one example of where conflicting values and priorities present practice dilemmas and the need for knowledge and sound judgment.
Hence, when it comes to providing rehabilitation services (and many other healthcare services), this version of the Golden Rule often applies: those with the gold make the rules. While this may be the unfortunate reality, exploring practical alternatives while balancing priorities and the needs of various stakeholders is essential.
Compliance with Ethics Guidelines
Conflict of Interest
Robert W. Richardson declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Ethics
Sidebar resources
APTA.org and CMS.gov are valuable resources for physical therapists. The following documents and publications can help you avoid fraud, waste, and abuse and gain an understanding of the changing regulations [1–4, 9]
• APTA core documents www.apta.org/Policies/CoreDocuments—This site features links to the code of ethics, Guide to Physical Therapist Practice and Guide for Conduct and Professionalism.
• APTA coding and billing www.apta.org/Payment/CodingBilling—This site includes links to courses (also see http://learningcenter.apta.org and http://www.apta.org/Courses/Online/NavigatingCompliance).
• Compliance http://www.apta.org/Compliance—This site offers information on fraud and abuse and Medicare audits.
• The federal government’s websites and the Federal Registry publish changes in rules and regulations that affect physical therapy. For example, the U.S. Department of Health and Human Services Centers for Medicare and publishes documents that provide an overview of facts and laws regarding Medicare fraud and abuse. Changes are also published in other forms in the public record. Government websites can be useful, but be forewarned that most will induce sleep with a full dose.
References
- 1.Guide to physical therapist practice 3.0. American Physical Therapy Association. http://www.apta.org.
- 2.Code of ethics for the physical therapist. American Physical Therapy Association. http://www.apta.org.
- 3.Medicare claims processing manual. Chapter 5 part B outpatient rehabilitation and CORF/OPT services, http:www.cms.gov/Medicare/Billing/TherapyServices/downloads/clm104c05.pdf
- 4.Final 2015 Physician Fee Schedule and Physician Quality Reporting System (PQRS) Measures. APTA Inf Bull. October 2014.
- 5.Purtillo RB, Doherty RF. Ethical dimensions in the health professions, fifth ed. Saunders, an imprint of Elsevier: 2010, p26.
- 6.Scott R. Professional ethics: a guide for rehabilitation professionals. Mosby: 1998, p12-14.
- 7.Richardson JK. The challenging roles facing physical therapists. Healthc Trends and Transit. 1993;5(1):34. [Google Scholar]
- 8.Gabard DL, Martin, ML. Physical therapy ethics, FA Davis: 2003, p vii(Preface)
- 9.Centers for Medicare and Medicaid Services. http://www.cms.gov/RegulationsandGuidance/RegulationsandGuidance.html.


