Abstract
Complications of the acromioclavicular joint injuries can occur as a result of the injury itself, conservative management, or surgical treatment. Fortunately, the majority of acromioclavicular surgeries utilizing modern techniques and instrumentation result in successful outcomes. However, clinical failures do occur with frequency. The ability to identify the causative factor of failures makes revision surgery more likely to be successful. The purposes of this review are to highlight common problems that can occur following acromioclavicular joint surgery and discuss techniques that can be utilized in revision surgery.
Keywords: Acromioclavicular joint injuries, Coracoclavicular reconstruction, Shoulder separation, Shoulder surgery complication
Introduction
Injuries to the acromioclavicular (AC) joint are common, particularly among the young and active population. AC joint dislocations represent ap proximately 12 % of all shoulder girdle dislocations, and 8 % of all joint dislocations throughout the body [1, 2]. Almost half of the AC joint injuries occur in patients in their 20s, with a predilection toward males versus females [3].
The management of AC dislocation is dependent on the severity of the injury. Lower grade AC injuries (types I and II) are initially treated nonoperatively. This typically consists of sling immobilization until pain subsides, ice, and rest. Operative treatment is recommended for more severe subtypes of AC separation (types IV, V, and VI injuries) due to the associated extensive soft tissue disruption and significant morbidity associated with persistently dislocated joints. Management of type III AC injuries remains controversial and a topic of debate.
Several different types of complications stemming from both operative and nonoperative treatment of AC injuries have been described. The underlying factors contributing to the failure of AC fixation are varied, which can be both patient and surgery dependent. There are a plethora of surgical techniques described to treat symptomatic AC joint dislocations. This is likely reflective of the inability of one technique to emerge as the “gold-standard.” As a result, most complications encountered following the surgical procedure are often times technique dependent. The objective of this manuscript is to review the common complications following acromioclavicular joint repair and reconstructions as well as potential salvage solutions.
Classification of acromioclavicular injuries
Accurate diagnosis and recognition of the pattern and displacement in AC injury is essential to successful treatment of acromioclavicular injuries. Critical to this process is obtaining adequate radiographic exams, which includes anteroposterior, axillary, and specific AC joint radiographs (Zanca view) of the injured shoulder. Comparison AC joint radiographs of the contralateral arm are also helpful to establish relative norms for patients. While it is relatively easy to assess vertical instability on radiographs, horizontal distal clavicle instability may be subtle but should be considered. Horizontal AC joint instability may occur independent of vertical instability [4, 5]. Residual horizontal instability can lead to pain and disability with lesser grade AC injuries. Additional special radiographic views (cross arm adduction views or functional axillary views) can assist in identifying horizontal instability in lesser grade AC injuries [6]. An AC width an index of ≥ 60 % measured on the bilateral Zanca view ([width of injured side − width of normal side / width of normal side] × 100 %) is highly accurate for posterior AC dislocation or horizontal instability [7].
Classification of AC injuries is based on the extent of involvement of the AC and coracoclavicular (CC) ligaments (Table 1) [2]. An understanding of this classification system will assist in guiding patient expectations, discussion of available treatment options, and formulating a proper surgical plan to address the associated injuries. While MRI examinations are not standard for all types of AC injuries, concomitant intraarticular glenohumeral pathologies have been shown to occur from 15 to 18.2 % of patients with type III or greater severity of AC joint injuries [8, 9]. Thus, MRI should be considered in patients presenting with high-grade AC injuries or clinical exam suspicious for intraarticular shoulder pathology.
Table 1.
Rockwood classification of acromioclavicular injuries
| Type | AC ligaments | CC ligaments | Deltopectoral fascia | X-ray CC distance | X-ray AC appearance |
|---|---|---|---|---|---|
| I | Sprained | Intact | Intact | Normal | Normal |
| II | Disrupted | Sprained | Intact | <25 % | Widened |
| III | Disrupted | Disrupted | Disrupted | 25–100 % | Widened |
| IV | Disrupted | Disrupted | Disrupted | Increased | Clavicle posteriorly displaced (axillary) |
| V | Disrupted | Disrupted | Disrupted | 100–300 % | N/A |
| VI | Disrupted | Disrupted | Disrupted | Decreased | Clavicle displaced inferior to coracoid |
Complication from nonoperative management of acromioclavicular injuries
While the focus of this review is to discuss complications associated with operative treatment of the AC joint, it is important to realize that complications stemming from nonoperative treatment have been described. Skin and wound complications can develop in patients treated nonoperatively for AC joint injuries. This includes abrasions or lacerations that may accompany AC joint injuries as well as skin tenting which may lead to local infection and skin necrosis, respectively. Iatrogenic skin complications, such as those associated with the Kenny-Howard device, are known to occur with frequency as well [1].
The long-term sequelae of nonoperative treatment of AC joint injuries remain a topic of debate. Persistent pain and disability can occur even with low-grade AC injuries (types I and II) managed conservatively [4, 10]. The success of conservative treatment may be different depending on the activity demand of the patient. Bergfeld et al. found up to 9 % (9/97—type I) and 23 % (7/31—type II) of the higher demand naval academy patients reported severe pain with limitation of activities at follow-up between 6 months and 3.5 years [10]. Management of type III injuries remains controversial. While nonoperative treatment can be successful, studies have shown that residual functional deficits may persist, including scapulothoracic dyskinesis, which may require further therapeutic intervention [11, 12].
Other causes of pain following nonoperative management of AC injuries may be degenerative in nature. Studies have shown that the rate of posttraumatic arthritis can be significant [10, 13–15]. Cox reported a 36 % rate of symptomatic arthritis after grade I injuries and a 48 % rate after grade II injuries [14]. Taft et al. reported posttraumatic arthritis in 43 % of patient who had type III AC injuries treated nonsurgically [15]. In addition to posttraumatic arthritis, distal clavicular osteolysis is also a recognized sequela of nonoperative management. The treatment of both posttraumatic arthritis and osteolysis is similar. Treatment consisting of activity modification, a course of anti-inflammatory medication, and intraarticular injection is generally the mainstay of nonoperative measures. Patients who are refractory to conservative management are candidates for resection of the distal clavicle. In patients with higher grade of AC injuries (type III, IV, or V), careful preoperative evaluation of AC stability is advised in order to determine if concomitant stabilization of the coracoclavicular ligament with reconstruction would be warranted at the time of distal clavicle resection.
Complications from operative treatment of acromioclavicular injuries
There are over 60 described procedures for surgical treatment of AC joint injuries [16], which is likely reflective of the limited evidence available to dictate the best strategy for operative treatment. There is even less evidence available to dictate the best strategy for revision following failed AC joint fixation. Revision surgery for failed AC joint repairs and reconstruction is therefore a challenge to the surgeon and a burden to the patient. Milewski et al. reviewed the complications related to newer techniques of anatomic CC ligament reconstruction with three fellowship-trained orthopedic surgeons. The authors reported an 80 % complication rate in the coracoid tunnel group and a 35 % complication rate in the coracoid loop group [17•]. More patients in the coracoid tunnel group had loss of reduction and coracoid base fractures; however, clavicle fractures were seen more often in the group with the loop around the coracoid base [17•]. In contrast, Martetschlager et al. reported an overall complication rate of 27 % in patients after CC ligament reconstruction and no difference between a cortical fixation versus tendon graft loop procedure [18]. In their series, the overall construct survivorship without complications was 86 and 83 % at 12 and 24 months, respectively [18].
Complications stemming from AC joint surgery are varied and at times unique to the implant and fixation method used during the index procedure. Essential to the planning process in revision scenarios is understanding the contributing factors to failure and the type of surgery performed at the index procedure. This may include reviewing preinjury and postsurgical films, previous operative reports, a detailed physical exam, and obtaining advanced imaging. The objective should be to identify a source or mode of failure from the prior procedure, such as pain from residual horizontal instability or loss of fixation due to coracoid or clavicle fracture. The ability to identify a clear source of failure increases the likelihood of success following the revision surgery.
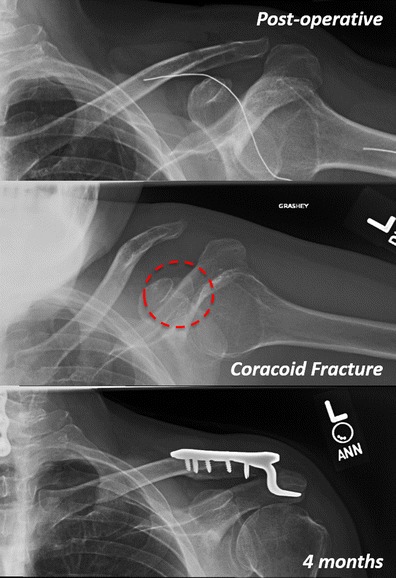
The most common complication following AC joint repair or reconstruction is loss of reduction. Loss of reduction in clinical series ranges between 15 and 80 % [19–22]. Not all patients are symptomatic, and the decision for revision should be based on patient’s symptoms and not on radiographic findings. Patients who have minimal symptoms with the loss of reduction can be successfully managed conservatively (Fig. 1). The status of the coracoid and clavicle should also be evaluated closely in cases where loss of reduction has occurred. In revision cases, an intact coracoid affords the surgeon multiple options to secure alternate CC graft fixation (Fig. 2). Likewise, an intact clavicle provides a stable structure by which fixation and a graft can be secured. If the coracoid base or the clavicle is compromised, then revision options will be limited and challenging.
Fig. 1.
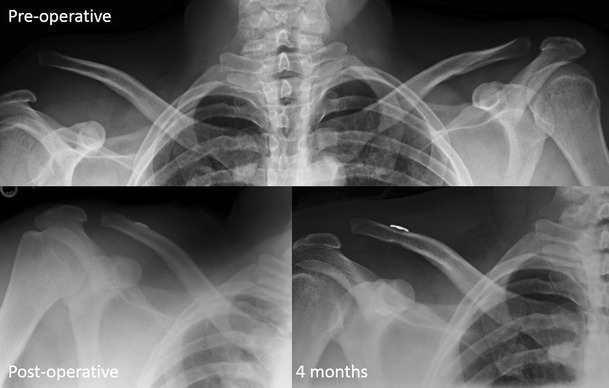
Acute type V AC joint injury after motorcycle accident. Patient underwent AC repair with suture button device with good reduction of deformity. There was partial loss of reduction at 4 months after surgery. Contour of the shoulder was maintained and patient was satisfied and pain free
Fig. 2.
Patient with failed right shoulder allograft CC joint reconstruction. On MRI, the trapezoid limb of the allograft had pulled out underneath the clavicle (circle). The clavicle and coracoid overall were intact. A revision allograft CC reconstruction was performed with a hook plate placed for additional stabilization and protection of allograft reconstruction. AC joint was stable and reduced after hook plate removal
Failed Weaver-Dunn procedure
Weaver and Dunn published their description of distal clavicle resection and CC ligament reconstruction in 1972 [23]. In this procedure, 7–8 mm of bone is removed from the distal clavicle and 2–3 mm is removed from the acromion. The coracoacromial ligament is then transferred and secured to the distal clavicle. Modification of the original procedure has included the use of variety of materials including suture or tissue to supplement the coracoclavicular fixation.
Failures of Weaver-Dunn AC reconstruction typically occur with both the clavicle and coracoid being intact and can be successfully revised with tendon autograft (semitendinosus) or allograft reconstruction. From a biomechanical point of view, an anatomic reconstruction using a free tendon graft imitating the double bundle of the CC ligament complex provides improved stability as compared with AC stabilization using the Weaver-Dunn procedure [24, 25]. Recurrent AC joint subluxation and dislocation can be minimized, decreasing the incidence of postoperative pain secondary to residual anterior-posterior instability and compromised clinical outcomes that have been observed with the modified Weaver-Dunn procedure [25]. Tauber et al. reported their experience revising failed Weaver-Dunn procedure with anatomic AC reconstruction with semitendinosus autograft [26]. Significant reduction in pain, improvement in functional scores, and improved radiographic parameters were achieved in their series of revision AC reconstruction cases.
Coracoid fracture after acromioclavicular repair or reconstruction
Techniques that involve drill holes through the coracoid for graft placement and fixation as part of anatomic CC ligament reconstruction or acute repair (synthetic sutures and button) increase the potential for coracoid fracture and cutout [17•, 27]. Milewski et al. reported a 20 % prevalence of coracoid fracture with CC ligament reconstruction using coracoid tunneling [17•]. This risk can be minimized by passage of the graft and/or suture around and under the coracoid without drilling. Newer generation arthroscopic instrumentation also has reduced the diameter needed to pass and secure the suture-button construct through the coracoid. Furthermore, adequate visualization of the entire base of the coracoid is essential. Accurate coracoid tunnel placement particularly in the center-center or medial-center position in the coracoid minimizes bony failure risk [28]. The combination of minimization of the tunnel diameter in the coracoid and appropriate visualization are therefore recommended to help prevent coracoid fracture or cutout in techniques using transcoracoid fixation.
There is limited literature to guide optimal treatment of coracoid fracture following AC joint repairs and reconstructions. Most of the available literature are expert opinion and case reports [17•, 29]. Coracoid fractures that are recognized intraoperatively can be managed with hook-plate stabilization, particularly in cases of acute AC joint repairs. Open reduction and internal fixation of the coracoid fragment can be performed depending on the displacement and size of the distal fragment. Management of coracoid fractures that occur during the postoperative period is also challenging. Assessment of the AC reduction as well as coracoid fracture fragment should be performed. The use of CT scan with reconstructions is helpful for assessment of the coracoid fracture and the bone quality for preoperative planning. The base of the coracoid in the long and short axes is 13.9 ± 2.0 and 10.5 ± 2.2 mm, respectively [30]. The minimal axes diameter was 6.6 mm in this particular study, which suggests that any coracoid base will accept a 4.5-mm-diameter screw. Kawasaki et al. described a perfect circle technique of using intraoperative fluoroscopy with the patient in supine position for coracoid fracture fixation after a hook plating of the AC joint injury [30]. Depending on the stability of the coracoid fixation, repassage of a graft under the coracoid following fixation can be considered in revision scenarios with or without utilization of a hook plate to “off load” the revision CC ligament reconstruction and coracoid fixation (Fig. 3) [17•, 29]. Alternatively, the proximal lateral half of the conjoined tendon can be transferred to the distal clavicle to reconstruct the CC ligament and reduce the interval depending on the stability of the coracoid fixation [31–33].
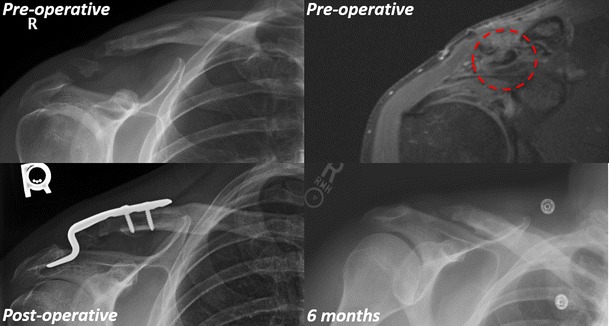
Fig. 3.
Patient underwent a left shoulder anatomic CC allograft reconstruction for a chronic type III injury. Patient had an accident resulting in acute loss of reduction with a coracoid fracture 1 month after surgery (circle). Patient redeveloped pain over the AC joint over the next couple of visits. He was revised with repeat reconstruction with hook plate with decreased pain and improved function
Clavicle fracture after acromioclavicular repair or reconstruction
Clavicular fractures following acromioclavicular joint reconstruction have been reported [17•, 34]. Similar to coracoid fractures, the popularity of anatomic CC ligament reconstruction and drilling of the clavicle raises the risk of clavicle fractures during the postoperative period. Minimization of the clavicular tunnel diameter along with adequate tunnel spacing of 20 to 25 mm between clavicular tunnels and 10 to 15 mm between the lateral tunnel and the distal edge of the clavicle may reduce the incidence of clavicle fracture [35•]. In a cadaver model, Spiegl et al. found a significant reduction of the clavicle strength after CC ligament reconstruction using hamstring and 6 mm tunnels comparing to a cortical button device and drilling 2.4 mm tunnels in the clavicle [36]. The addition of a tenodesis screw into the clavicular tunnel does not seem to increase the strength or decrease the ultimate failure of the clavicle [37]. Depending on the size of the clavicle in the AP plane, a tunnel diameter greater than 7 mm will reduce the clavicle strength and may increase risk of fracture. Accurate placement of the conoid tunnel at 25 % of the clavicular length from the lateral border of the clavicle has also been associated with lower rate of loss of reduction and higher rate of return among the active military population [38].
Minimally displaced clavicular fractures after anatomic CC reconstruction can be serially monitored and successfully treated nonoperatively [34]. Displaced clavicle fractures with loss of AC joint reduction typically are addressed with open reduction and internal fixation. Usage of plate constructs such as clavicle plates or hook plates is often dictated by the size and location of the clavicle fracture. Large distal clavicle osteolysis after CC ligament reconstruction with allograft is a complex and challenging problem to manage (Fig. 4). This may be attributed to immune reaction to the allograft tissue. Although not described in the literature, using a vascularized fibular graft with a hook plate and revision CC ligament reconstruction using semitendinosus autograft tissue may be an option [39]. Iliac crest bone graft can also provide an option for reconstruction depending on the size of the bone loss. Alternatively, total claviculectomy may provide a final salvage option for patients that present with massive distal clavicle lysis after failed CC ligament reconstruction [40].
Fig. 4.

Failed anatomic CC ligament reconstruction with significant distal clavicle osteolysis
Other general complications after acromioclavicular repair or reconstruction
Hardware migration has long been associated with AC joint surgery. The frequency and location of pin migration and potential serious complications that may arise have prompted most clinicians to abandon their use, particularly smooth pins (Fig. 5). Clinicians who still utilize pins should bend the pins distally to prevent migration, check their position with frequent radiographs, and remove them after initial interval healing. Pin migration from AC joint surgery into various vital structures such as the pleural space, spinal canal, carotid sheath, and nearby vascular structures has all been reported in the literature [41, 42].
Fig. 5.

Migrated k-wire into the axilla from AC joint fixation
Postoperative infection following AC joint surgery is not uncommon. Reported rates of infection range from 0 to 9 % [43••]. Fortunately, most postoperative infections are superficial in nature and therefore respond to medical therapy alone. Deep infection involving fixation or augmentation devices however does occur. Neault et al. reported on three cases in which deep postoperative infection occurred after the use of nonabsorbable tape [44]. All patients responded with removal of the foreign materials, debridement, and antibiotic therapy. Colosimo et al. similarly reported two cases of aseptic foreign body reaction to Dacron graft, which responded to removal of the synthetic material [45]. Most authors therefore recommend aggressive debridement with removal of all synthetic materials in suspected cases of deep infection along with appropriate antibiotic coverage when an infection is confirmed. Staged reconstruction can be carried out in a delayed fashion once the infection is eradicated. If the failure is found to be aseptic in nature, primary revision can be considered [46].
Authors’ preferred treatment
While many surgical repairs or reconstruction techniques have been described, the authors currently prefer an anatomic reconstruction. Studies in the literature that directly compare anatomic and nonanatomic techniques show improved results with the anatomic technique [26, 47]. Because of the reconstruction technique, repair can be performed in a subacute fashion. Assuming there is no skin tenting or compromise, waiting 2–4 weeks from injury allows abrasions to heal and can minimize skin-related complications. Further, in the case of type III injuries, a brief recovery period may allow symptoms to improve and allow select patients to choose nonoperative management. While there may be no biomechanical advantage [48], we do not routinely resect any distal clavicle unless reduction is prohibited as in some chronic cases. If resection of the clavicle is required, minimal bone (5–7 mm) should be removed. The graft is augmented with a strong braided polyester suture that is also passed under the coracoid and through the clavicular tunnels. This suture is tied over the clavicle for initial reduction and augmented fixation. We routinely reconstruct the AC ligaments with the lateral graft. If the graft length is insufficient, or in the case of types IV and V injuries, we further reconstruct the AC ligaments with strong braided suture through drill tunnels in the clavicle and acromion [49]. Finally, the delto-trapezeal fascia is reefed over the repair and the graft is incorporated into the fascial closure [35•]. Patients are immobilized with a supportive abduction sling postoperatively for 4–6 weeks.
Conclusion
Successful outcomes following AC joint surgery are dependent on several factors including accurate diagnosis and recognition of the severity of the injury. Having a full comprehensive knowledge of available surgical options is essential. The ability of the treating clinician to anticipate potential pitfalls during surgery as well as the technical aspects to avoid complications is critical to the success of the procedure and outcome. Even with all this knowledge, complications related to acromioclavicular surgery still may occur. The ability to identify the relevant culprit of a failed acromioclavicular procedure and having knowledge of reconstructive options makes revision surgery more likely to be successful.
Compliance with Ethics Guidelines
Conflict of Interest
Richard Ma declares that he has no conflict of interest.
Patrick A. Smith have no conflicts to disclose relevant to this manuscript.
Matthew J. Smith reports personal fees from Arthrex, Zimmer, and DePuy, outside the submitted work.
Seth L. Sherman has received consultant/research support from Arthrex and RTI.
David Flood have no conflicts to disclose relevant to this manuscript.
Xinning Li has received consultation fees from Tornier and Mitek Sports Medicine, outside the submitted work.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Shoulder Surgery: Complications
Contributor Information
Richard Ma, Email: RichardMaMD@Gmail.com.
Matthew J. Smith, Email: smithmj@health.missouri.edu
Seth L. Sherman, Email: dr.seth.sherman@gmail.com
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Allman FL., Jr Fractures and ligamentous injuries of the clavicle and its articulation. J Bone Joint Surg Am. 1967;49:774–784. [PubMed] [Google Scholar]
- 2.Rockwood C, Williams G, Young D. Disorders of the acromioclavicular joint. Philadelphia: WB Saunders; 2004. [Google Scholar]
- 3.Lemos MJ. The evaluation and treatment of the injured acromioclavicular joint in athletes. Am J Sports Med. 1998;26:137–144. doi: 10.1177/03635465980260010801. [DOI] [PubMed] [Google Scholar]
- 4.Mouhsine E, Garofalo R, Crevoisier X, et al. Grade I and II acromioclavicular dislocations: results of conservative treatment. J Shoulder Elbow Surg. 2003;12:599–602. doi: 10.1016/S1058-2746(03)00215-5. [DOI] [PubMed] [Google Scholar]
- 5.Wellmann M, da Silva G, Lichtenberg S, et al. Instability pattern of acromioclavicular joint dislocations type Rockwood III: relevance of horizontal instability. Orthopade. 2013;42:271–277. doi: 10.1007/s00132-013-2085-1. [DOI] [PubMed] [Google Scholar]
- 6.Tauber M, Koller H, Hitzl W, et al. Dynamic radiologic evaluation of horizontal instability in acute acromioclavicular joint dislocations. Am J Sports Med. 2010;38:1188–1195. doi: 10.1177/0363546510361951. [DOI] [PubMed] [Google Scholar]
- 7.Vaisman A, Villalon Montenegro IE, Tuca De Diego MJ, et al. A novel radiographic index for the diagnosis of posterior acromioclavicular joint dislocations. Am J Sports Med. 2014;42:112–116. doi: 10.1177/0363546513506849. [DOI] [PubMed] [Google Scholar]
- 8.Pauly S, Gerhardt C, Haas NP, et al. Prevalence of concomitant intraarticular lesions in patients treated operatively for high-grade acromioclavicular joint separations. Knee Surg Sports Traumatol Arthrosc. 2009;17:513–517. doi: 10.1007/s00167-008-0666-z. [DOI] [PubMed] [Google Scholar]
- 9.Tischer T, Salzmann GM, El-Azab H, et al. Incidence of associated injuries with acute acromioclavicular joint dislocations types III through V. Am J Sports Med. 2009;37:136–139. doi: 10.1177/0363546508322891. [DOI] [PubMed] [Google Scholar]
- 10.Bergfeld JA, Andrish JT, Clancy WG. Evaluation of the acromioclavicular joint following first- and second-degree sprains. Am J Sports Med. 1978;6:153–159. doi: 10.1177/036354657800600402. [DOI] [PubMed] [Google Scholar]
- 11.Gumina S, Carbone S, Postacchini F. Scapular dyskinesis and SICK scapula syndrome in patients with chronic type III acromioclavicular dislocation. Arthrosc. 2009;25:40–45. doi: 10.1016/j.arthro.2008.08.019. [DOI] [PubMed] [Google Scholar]
- 12.Schlegel TF, Burks RT, Marcus RL, et al. A prospective evaluation of untreated acute grade III acromioclavicular separations. Am J Sports Med. 2001;29:699–703. doi: 10.1177/03635465010290060401. [DOI] [PubMed] [Google Scholar]
- 13.Cook DA, Heiner JP. Acromioclavicular joint injuries. Orthop Rev. 1990;19:510–516. [PubMed] [Google Scholar]
- 14.Cox JS. The fate of the acromioclavicular joint in athletic injuries. Am J Sports Med. 1981;9:50–53. doi: 10.1177/036354658100900111. [DOI] [PubMed] [Google Scholar]
- 15.Taft TN, Wilson FC, Oglesby JW. Dislocation of the acromioclavicular joint. An end-result study. J Bone Joint Surg Am. 1987;69:1045–1051. [PubMed] [Google Scholar]
- 16.Geaney LE, Miller MD, Ticker JB, et al. Management of the failed AC joint reconstruction: causation and treatment. Sports Med Arthrosc Rev. 2010;18:167–172. doi: 10.1097/JSA.0b013e3181eaf6f7. [DOI] [PubMed] [Google Scholar]
- 17.•.Milewski MD, Tompkins M, Giugale JM, et al. Complications related to anatomic reconstruction of the coracoclavicular ligaments. Am J Sports Med. 2012;40:1628–1634. doi: 10.1177/0363546512445273. [DOI] [PubMed] [Google Scholar]
- 18.Martetschlager F, Horan MP, Warth RJ, et al. Complications after anatomic fixation and reconstruction of the coracoclavicular ligaments. Am J Sports Med. 2013;41:2896–2903. doi: 10.1177/0363546513502459. [DOI] [PubMed] [Google Scholar]
- 19.Cook JB, Shaha JS, Rowles DJ, et al. Early failures with single clavicular transosseous coracoclavicular ligament reconstruction. J Shoulder Elbow Surg. 2012;21:1746–1752. doi: 10.1016/j.jse.2012.01.018. [DOI] [PubMed] [Google Scholar]
- 20.Salzmann GM, Walz L, Schoettle PB, et al. Arthroscopic anatomical reconstruction of the acromioclavicular joint. Acta Orthop Belg. 2008;74:397–400. [PubMed] [Google Scholar]
- 21.Weinstein DM, McCann PD, McIlveen SJ, et al. Surgical treatment of complete acromioclavicular dislocations. Am J Sports Med. 1995;23:324–331. doi: 10.1177/036354659502300313. [DOI] [PubMed] [Google Scholar]
- 22.Yoo JC, Ahn JH, Yoon JR, et al. Clinical results of single-tunnel coracoclavicular ligament reconstruction using autogenous semitendinosus tendon. Am J Sports Med. 2010;38:950–957. doi: 10.1177/0363546509356976. [DOI] [PubMed] [Google Scholar]
- 23.Weaver JK, Dunn HK. Treatment of acromioclavicular injuries, especially complete acromioclavicular separation. J Bone Joint Surg Am. 1972;54:1187–1194. [PubMed] [Google Scholar]
- 24.Grutter PW, Petersen SA. Anatomical acromioclavicular ligament reconstruction: a biomechanical comparison of reconstructive techniques of the acromioclavicular joint. Am J Sports Med. 2005;33:1723–1728. doi: 10.1177/0363546505275646. [DOI] [PubMed] [Google Scholar]
- 25.Mazzocca AD, Santangelo SA, Johnson ST, et al. A biomechanical evaluation of an anatomical coracoclavicular ligament reconstruction. Am J Sports Med. 2006;34:236–246. doi: 10.1177/0363546505281795. [DOI] [PubMed] [Google Scholar]
- 26.Tauber M, Gordon K, Koller H, et al. Semitendinosus tendon graft versus a modified Weaver-Dunn procedure for acromioclavicular joint reconstruction in chronic cases: a prospective comparative study. Am J Sports Med. 2009;37:181–190. doi: 10.1177/0363546508323255. [DOI] [PubMed] [Google Scholar]
- 27.Gerhardt DC, VanDerWerf JD, Rylander LS, et al. Postoperative coracoid fracture after transcoracoid acromioclavicular joint reconstruction. J Shoulder Elbow Surg Ame Shoulder Elbow Surg. 2011;20:e6–10. doi: 10.1016/j.jse.2011.01.017. [DOI] [PubMed] [Google Scholar]
- 28.Ferreira JV, Chowaniec D, Obopilwe E, et al. Biomechanical evaluation of effect of coracoid tunnel placement on load to failure of fixation during repair of acromioclavicular joint dislocations. Arthrosc. 2012;28:1230–1236. doi: 10.1016/j.arthro.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 29.Wiesel BB, Gartsman GM, Press CM, et al. What went wrong and what was done about it: pitfalls in the treatment of common shoulder surgery. J Bone Joint Surg Am. 2013;95:2061–2070. doi: 10.2106/JBJS.9522icl. [DOI] [PubMed] [Google Scholar]
- 30.Kawasaki Y, Hirano T, Miyatake K, et al. Safety screw fixation technique in a case of coracoid base fracture with acromioclavicular dislocation and coracoid base cross-sectional size data from a computed axial tomography study. Arch Orthop Trauma Surg. 2014;134:913–918. doi: 10.1007/s00402-014-1995-7. [DOI] [PubMed] [Google Scholar]
- 31.Jiang C, Wang M, Rong G. Proximally based conjoined tendon transfer for coracoclavicular reconstruction in the treatment of acromioclavicular dislocation. J Bone Joint Surg Am. 2007;89:2408–2412. doi: 10.2106/JBJS.F.01586. [DOI] [PubMed] [Google Scholar]
- 32.Jiang C, Wang M, Rong G. Proximally based conjoined tendon transfer for coracoclavicular reconstruction in the treatment of acromioclavicular dislocation. Surgical technique. J Bone Joint Surg Am. 2008;90(Suppl 2 Pt 2):299–308. doi: 10.2106/JBJS.H.00438. [DOI] [PubMed] [Google Scholar]
- 33.Kim SH, Lee YH, Shin SH, et al. Outcome of conjoined tendon and coracoacromial ligament transfer for the treatment of chronic type V acromioclavicular joint separation. Injury. 2012;43:213–218. doi: 10.1016/j.injury.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 34.Turman KA, Miller CD, Miller MD. Clavicular fractures following coracoclavicular ligament reconstruction with tendon graft: a report of three cases. J Bone Joint Surg Am. 2010;92:1526–1532. doi: 10.2106/JBJS.I.00410. [DOI] [PubMed] [Google Scholar]
- 35.•.Carofino BC, Mazzocca AD. The anatomic coracoclavicular ligament reconstruction: surgical technique and indications. J Shoulder Elbow Surg. 2010;19:37–46. doi: 10.1016/j.jse.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 36.Spiegl UJ, Smith SD, Euler SA, et al. Biomechanical consequences of coracoclavicular reconstruction techniques on clavicle strength. Am J Sports Med. 2014;42:1724–1730. doi: 10.1177/0363546514524159. [DOI] [PubMed] [Google Scholar]
- 37.Dumont GD, Russell RD, Knight JR, et al. Impact of tunnels and tenodesis screws on clavicle fracture: a biomechanical study of varying coracoclavicular ligament reconstruction techniques. Arthrosc. 2013;29:1604–1607. doi: 10.1016/j.arthro.2013.07.257. [DOI] [PubMed] [Google Scholar]
- 38.Cook JB, Shaha JS, Rowles DJ, et al. Clavicular bone tunnel malposition leads to early failures in coracoclavicular ligament reconstructions. Am J Sports Med. 2013;41:142–148. doi: 10.1177/0363546512465591. [DOI] [PubMed] [Google Scholar]
- 39.Momberger NG, Smith J, Coleman DA. Vascularized fibular grafts for salvage reconstruction of clavicle nonunion. J Shoulder Elbow Surg Am Shoulder Elbow Surg. 2000;9:389–394. doi: 10.1067/mse.2000.107090. [DOI] [PubMed] [Google Scholar]
- 40.Krishnan SG, Schiffern SC, Pennington SD, et al. Functional outcomes after total claviculectomy as a salvage procedure. A series of six cases. J Bone Joint Surg Am. 2007;89:1215–1219. doi: 10.2106/JBJS.E.01436. [DOI] [PubMed] [Google Scholar]
- 41.Grauthoff H, Klammer HL. Complications due to migration of a Kirschner wire from the clavicle (author’s transl) RoFo Fortschr Geb Rontgenstrahlen Nuklearmedizin. 1978;128:591–594. doi: 10.1055/s-0029-1230910. [DOI] [PubMed] [Google Scholar]
- 42.Norrell H, Jr., Llewellyn RC. Migration of a threaded Steinmann pin from an acromioclavicular joint into the spinal canal. A case report. J Bone Joint Surg. [PubMed]
- 43.••.Provencher M, Leclere L, Romeo A et al. Avoiding and managing complications of surgery of the acromioclavicular joint: Springer; 2009. This book chapter provides a good summary on acromioclavicuar joint injury diagnosis and surgical management. Furthermore, technical aspects of acromioclavicular surgery including measures to avoid and solve intraoperative complications are provided.
- 44.Neault MA, Nuber GW, Marymont JV. Infections after surgical repair of acromioclavicular separations with nonabsorbable tape or suture. J Shoulder Elbow Surg. 1996;5:477–478. doi: 10.1016/S1058-2746(96)80021-8. [DOI] [PubMed] [Google Scholar]
- 45.Colosimo AJ, Hummer CD, 3rd, Heidt RS., Jr Aseptic foreign body reaction to Dacron graft material used for coracoclavicular ligament reconstruction after type III acromioclavicular dislocation. Am J Sports Med. 1996;24:561–563. doi: 10.1177/036354659602400424. [DOI] [PubMed] [Google Scholar]
- 46.Lemos MJ, Tolo ET. Complications of the treatment of the acromioclavicular and sternoclavicular joint injuries, including instability. Clin Sports Med. 2003;22:371–385. doi: 10.1016/S0278-5919(02)00102-3. [DOI] [PubMed] [Google Scholar]
- 47.Beitzel K, Cote MP, Apostolakos J, et al. Current concepts in the treatment of acromioclavicular joint dislocations. Arthrosc. 2013;29:387–397. doi: 10.1016/j.arthro.2012.11.023. [DOI] [PubMed] [Google Scholar]
- 48.Beaver AB, Parks BG, Hinton RY. Biomechanical analysis of distal clavicle excision with acromioclavicular joint reconstruction. Am J Sports Med. 2013;41:1684–1688. doi: 10.1177/0363546513488750. [DOI] [PubMed] [Google Scholar]
- 49.Nuchtern JV, Sellenschloh K, Bishop N, et al. Biomechanical evaluation of 3 stabilization methods on acromioclavicular joint dislocations. Am J Sports Med. 2013;41:1387–1394. doi: 10.1177/0363546513484892. [DOI] [PubMed] [Google Scholar]


