Abstract
Imaging modalities for the diagnosis of osteonecrosis (ON) of the femoral head have been studied extensively, but there have been few reports strictly addressing radiographic evaluation. The purpose of this report is to examine the use and role of (1) plain radiographs, (2) magnetic resonance imaging (MRI), (3) computerized tomography (CT), (4) bone scanning, and (5) positron emission topography (PET) for the diagnostic evaluation of ON. Plain radiographs are a mainstay in diagnosis but have very low sensitivity for early ON. MRI is the gold standard for diagnostic evaluation but may not identify subchondral fractures on collapse as well as CT scan or tomogram. Bone scanning should not be used for diagnosis due to its low sensitivity. PET scanning does not have a definitive role in diagnosis yet. Future research should focus on the role of new imaging technologies in evaluation.
Keywords: Osteonecrosis of hip, Diagnosis, Disease staging, Radiograph
Introduction
Detecting osteonecrosis (ON) is often challenging for clinicians and surgeons, which is why many imaging modalities are used to aid in diagnosis. Additionally, obtaining appropriate imaging is critical to correctly stage the disease [1, 2]. Plain radiographs are commonly obtained, but magnetic resonance imaging (MRI) is now considered the gold standard of diagnosis as it is highly specific (>99 %) and sensitive for the earliest stages of ON [3, 4••, 5]. Many recent studies have attempted to provide an improvement on the diagnostic abilities of plain radiographs and MRI with an emphasis on prognosis [6–10]. In addition, more recent literature has attempted to incorporate alternative imaging technologies that may improve upon the diagnostic evaluation of ON [6].
Imaging modalities for the diagnosis of ON have been previously studied individually [4••, 5, 11–14]. However, to our knowledge, there has not been a detailed literature review focusing extensively and specifically on the role of different imaging modalities in the diagnosis of ON. Therefore, the purpose of this review was to examine the use and role of (1) plain radiography, (2) MRI, (3) tomography, (4) bone scanning, and (5) positron emission tomography (PET) for the diagnostic evaluation of osteonecrosis of the femoral head. Our secondary purpose was to describe the common findings of ON associated with each imaging modality and how these findings may predict patient outcomes with the goal of assisting the practitioner with prognosis and treatment.
Plain radiographs
Plain radiographs have remained a mainstay for the diagnostic evaluation of any patient presenting with hip pain thought to be caused by ON. Radiographs have also been the foundation for many well-known classification systems (Fig. 1a–d). Kerboul et al. [15] developed one of the first systems widely used for measuring the extent of osteonecrosis. They measured the arc of the femoral surface involved in osteonecrosis using two different angles. The angles were calculated by drawing two lines from the center to the periphery of the femoral head containing the area of osteonecrosis on both the AP and lateral radiographs. These angles were then added together and if the sum of the angles was >200o, it was considered large. Although this has been primarily used with plain films, this technique has been applied to more advanced technologies such as MRI [16].
Fig. 1.
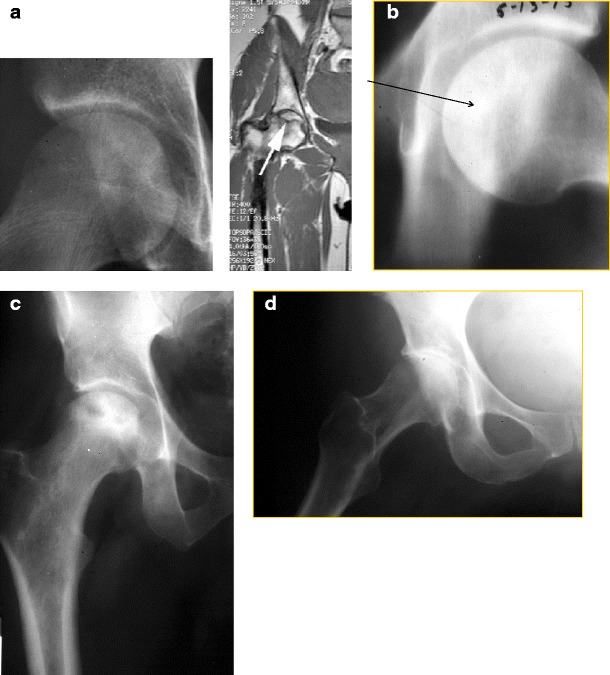
Plain radiographs showing different stages of disease. a Ficat Stage I ON patient with normal radiograph and abnormal MRI. b Ficat stage II ON patient with arrow pointing to sclerotic lesion. c Ficat stage III ON patient with evident femoral head collapse. d Ficat stage IV ON patient with acetabular involvement
When examining plain films, lesions may be classified as either sclerotic or cystic. This distinction may be critical to determining the risk of lesion progression. Takao et al. [17] followed a cohort of patients in pre-collapse or early post-collapse stages of the disease (n = 33 hips). After a mean follow-up of 14 years (range 10 to 23.4 years), they found an increase in sclerosis around the lesion was seen in the majority of hips that did not progress to collapse (n = 14 out of 17 hips). Hence, the authors concluded that sclerosis may be a positive prognostic sign. Furthermore, cystic lesions have been studied for a potential increased risk of failure of total hip resurfacings [18, 19]. Therefore, sclerotic lesions may indicate a better prognosis than their cystic counterparts.
Despite the fact that plain radiographs are routinely ordered when assessing patients who may have ON, they cannot be solely relied upon for multiple reasons. The first classification system of ON based on plain radiographs acknowledged that many small areas of osteonecrosis are not found using this modality [6]. Multiple studies and reviews have confirmed that plain radiographs are highly specific for advanced disease but exhibit very low sensitivity for the earliest stages of the disease [12, 14]. This is critical because early diagnosis and treatment is associated with a more favorable prognosis, while more advanced stages require aggressive management such as total hip arthroplasty [14, 20–22].
Although plain radiographs are a mainstay in diagnosis, it may be difficult to distinguish between ON and rapid onset osteoarthritis of the hip (ROOH) [4••, 7]. A recent literature review performed by Pivec et al. [4••] displayed the differences between ON, primary osteoarthritis (OA), and ROOH. Unlike primary OA and late-stage ON, respectively, plain films in cases of ROOH do not show acetabular bone loss or femoral head collapse (Table 1). In attempt to further distinguish between these different diagnoses, Nelson et al. [7] assessed whether the use of different imaging measures on plain radiograph could assist in distinguishing between these two diagnoses (n = 18 ON and 18 ROOH patients, respectively). They found that the Tonnis angle (p < 0.001) and the acetabular extrusion index (p = 0.044) were smaller in the ON cohort compared to the ROOH cohort. The authors concluded that using these different radiographic measures may reduce the misdiagnosis of these two conditions.
Table 1.
Radiographic findings differentiating between primary osteoarthritis, osteonecrosis, and rapidly progressive osteoarthritis [4••]
| Diagnosis | Plain radiographic findings |
|---|---|
| Primary OA | • Osteophyte formation • Subchondral cysts • Joint space narrowing • Sclerosis |
| Rapidly progressive OA | • Joint space narrowing without acetabular bone loss or femoral head collapse |
| ON | • Femoral head collapse • Subchondral fracture • Acetabular bone loss and degeneration in latest stages |
OA osteoarthritis, ON osteonecrosis
In summary, obtaining plain radiographs is fundamental in the work-up and follow-up of patients presenting with symptoms suspicious for ON. If femoral head collapse, acetabular changes, or advanced degeneration are apparent on X-ray, no further imaging is required (Fig. 2). However, they may not be as accurate as more recent technologies in identifying asymptomatic lesions. As such, more advanced imaging technologies may be required in the diagnostic evaluation of ON.
Fig. 2.
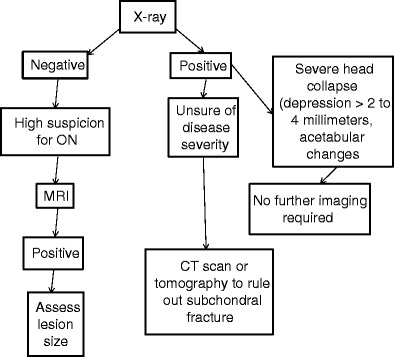
Algorithm for diagnosis of osteonecrosis
Magnetic resonance imaging
Magnetic resonance imaging (MRI) is the gold standard for detecting the earliest stages of ON, due to multiple studies displaying >99 % specificity and sensitivity (Table 2) [23–32]. A band-like lesion showing a low intensity signal on T1-weighted images is usually pathognomonic for this disease [3, 6, 14, 24, 28, 33]. In addition to the pathognomonic band-like lesion, bone marrow edema has been discussed as a potential early finding indicative of ischemia. Ragab et al. [34] evaluated a group of patients who had an MRI after presenting with hip pain, 29 % of whom were diagnosed with ON (n = 10 hips). Of the ON patients, all had bone marrow edema identified on their MRI. Additionally, bone marrow edema has been reported to correlate with symptomatic ON. Koo et al. [35] conducted a study on 37 hips, of which 14 were symptomatic, to determine whether bone marrow edema on MRI had any association with pain in the earliest stages of the disease process. Of the symptomatic hips, 7 showed marrow edema, with 6 of the 7 complaining of moderate to severe pain. The authors found that when the marrow edema resolved, it usually accompanied the resolution of the pain. Similarly, Huang et al. [36] evaluated the association of bone marrow edema with pain (n = 110 total hips with 31 asymptomatic hips). They found a strong correlation between bone marrow edema and the presentation of hip pain (p < 0.0001), with those with edema being nearly 25 times more likely to complain of pain than those without edema. Although each of these studies found an association between bone marrow edema and ON, each of these authors clearly states that bone marrow edema is not pathognomonic for ON.
Table 2.
Studies displaying MRI sensitivity and specificity >99 %
In conjunction with bone marrow edema, approximately 50 % of patients with ON will have a joint effusion visualized on MRI [37, 38]. In the previously mentioned study performed by Huang et al. [36] (n = 110 hips), about 90 % of their patients with ON also had joint effusions. Specifically, they noted that Steinberg stage III ON or higher was associated with the presence of a joint effusion (p < 0.003). Moreover, joint effusions may assist in staging the disease. Liu et al. [39••] evaluated the relationship between hip joint effusion volume and staging using the Association Research Circulation Osseous (ARCO) classification scheme (n = 185 hips). They found that there was a significant difference in effusion volume between ON stages I and III (p < 0.01). However, the effusion volume was comparable between stages I and II as well as within sub-stages (A, B, and C) (p > 0.05).
Magnetic resonance imaging is typically not used to follow lesions once the femoral head has collapsed [12]; however, it has been used to follow the progression of small asymptomatic lesions. Zhao et al. [40] evaluated the changes of lesion size within a cohort of pre-collapse ON (ARCO I and II) patients caused by corticosteroid administration (n = 84 hips). After a 5-year follow-up, 80 hips (95 %) experienced a decrease in lesion size. Therefore, the authors concluded that MRI may be helpful in following small asymptomatic lesions, but they did not recommend that it should be used in routine follow-up.
Despite MRI being widely accepted as paramount for diagnosis of ON, it is not infallible. In the more advanced stages of osteonecrosis (Steinberg III or IV), MRI may not be sensitive or specific for diagnosing subchondral fractures. Yeh et al. [41] and Stevens et al. [42] performed studies that demonstrated that computerized tomography (CT) was more sensitive and specific for identifying subchondral fractures than MRI in separate studies. These will be discussed in detail in the CT section of this report.
In an attempt to improve upon the sensitivity and specificity of MRI when diagnosing and staging ON, researchers have explored the use of different technologies such as diffuse weight imaging (DWI) [10] and magnetic resonance spectroscopy (MRS) [8]. Oner et al. [10] evaluated the use of DWI in conjunction with conventional MRI in a cohort of patients with ON (n = 35 femoral heads). However, they found that DWI did not aid in distinguishing between the various stages of ON. As such, the authors concluded that DWI has limited value in assessing patients with ON of the femoral head. Similarly, Hou et al. [8] evaluated patients with ON in a matched control trial using MRI and MRS (n = 110 patients total). The authors found that the measured lipid and water content differed significantly on MRS between those with ON and the control cohort (p < 0.001 and 0.05, respectively). Thus, they concluded that using MRS may be beneficial when predicting ON in the earliest stages of its development.
In summary, MRI remains the gold standard of diagnosis and staging and should be obtained in the event that plain radiographs do not definitively identify a lesion (Fig. 2). It may not be as effective in identifying subchondral fractures as tomography or CT scanning. Furthermore, it has yet to be shown as an effective tool for following the routine progression of disease aside from small asymptomatic lesions. Therefore, although its diagnostic utility cannot be improved upon, its role in identifying subchondral fractures and following the course of the disease is not always optimal. Future improvements in MRI technology may improve further upon its prognostic sensitivity.
CT axial and tomography technologies
Although computerized tomography (CT) scanning is not commonly used for diagnosing patients suspected of having ON, it may have value in detecting the presence of, and describing the characteristics of subchondral fractures. Alternatively, a tomogram can be obtained if a CT scan is unavailable. In 1986, Mitchell et al. [43] described the appearance of ON of the femoral head on CT scan in comparison with MRI (n = 21 hips). The authors found that CT scans more clearly depicted areas of bony changes than MRI. In contrast, MRI more accurately depicted alterations to the bone marrow commonly seen in ON.
Similarly, Yeh et al. [41] assessed the accuracy of MRI and CT in diagnosing subchondral fractures in patients who have ON (n = 28 hips). All images were evaluated by a blinded musculoskeletal radiologist and a general radiologist, and substantial inter-observer variability was found in the staging of the disease (k = 0.01 with value <0.2 considered poor) and identification of subchondral fractures with MRI. The authors concluded that although MRI is highly sensitive for the earliest stages of ON, sole reliance on it may lead to inaccurate staging in the later stages (Steinberg II to IV). Additionally, Stevens et al. [42] compared the ability of CT to MRI in diagnosing subchondral fractures (Steinberg III). After a 12-month follow-up, they found very low sensitivity and specificity of MRI for the diagnosing of subchondral fractures when compared to CT (38 and 100 % versus 100 and 100 %, respectively). Therefore, the authors concluded that CT allows for good visualization of the cortical surface of bones, while MRI cannot image this area in such a detailed manner.
However, there have been inconsistencies in the diagnostic ability of CT scanning. Recently, Barille et al. [44•] evaluated the incidence of missed ON in those with MRI-proven ON (n = 33 hips). They found that 89 % of all hips with osteonecrosis were not diagnosed on CT. They speculated that this may be because many radiologists were not implementing a routine visual checklist when examining the hip. Therefore, the authors concluded that if CT was to aid in the diagnosis of ON, it could only do so if a routine search pattern was implemented with each pelvic CT by the interpreting radiologist.
In summary, although we do not recommend CT in the routine radiographic evaluation of ON, it can be helpful in patients who are suspected to have a subchondral fracture or when there is suspicion for head collapse that is not detected on MRI (Fig. 2).
99-Technetium bone scan
Multiple attempts have been carried out to investigate if bone scanning has a role in early diagnosis. By injecting 99mTc-methylene diphosphonate, osteoblastic activity and the presence of blood flow may be identified, thus, suspected areas of early stage (Steinberg I) osteonecrosis would display a reactive interface around the suspected lesions [23, 43, 45]. A case series of 5 patients published by Alavi et al. [46] first described the use of bone scanning in osteonecrosis, and the authors were able to identify areas of osteonecrosis 2 to 5 months before plain radiographs, leading them to believe that this could be a potential diagnostic tool for high-risk patients.
However, studies have determined that bone scanning may not be particularly effective in ON diagnosis. In 2008, Mont et al. [47] compared the sensitivity and specificity of MRI to bone scintigraphy when evaluating a group of patients who had suspected osteonecrotic lesions (n = 163 lesions among 48 patients). All of the patients underwent simultaneous bone scans and MRI studies and had histological confirmation of the diagnosis. The authors found 100 % sensitivity for MRI studies compared to 56 % sensitivity for bone scans. Hence, they concluded that although bone scanning may be useful as a screening tool, it shows the least utility in the earliest stages of the disease. In summary, the utility of bone scanning in staging and diagnosing ON remains an area of investigation; however, routine bone scanning is not recommended [6, 47].
New technologies
Positron emission tomography
Recently, studies have investigated positron emission tomography (PET) for the diagnosis of ONFH; however, there is currently a paucity of reports to validate its routine use. Using 18 F as a radio-labeled marker, it accumulates in high glucose metabolizing cells, such as inflammatory cells that are present within osteonecrotic lesions [48–50]. In one of these studies, Dasa et al. [51] evaluated 17 hips with ON, in which all patients underwent PET scanning, SPECT, MRI with T1 and T2 imaging, and bone scanning. It was concluded that the PET scans identified 9 hips with areas of increased acetabular uptake suspicious for osteonecrosis that were not seen on MRI, SPECT, or bone scanning. The authors concluded that PET scans may have more diagnostic value in identifying early stage (Steinberg I) ON than other imaging modalities. Despite studies showing the benefits of PET scans, its use in the diagnosis of ON is not common practice due to its high cost and time-consuming nature [6]. Further studies are needed highlighting the advantages of PET scans in ON to justify the disadvantages of this imaging modality.
Conclusion
In conclusion, multiple imaging strategies are currently available for the appropriate diagnosis and staging of ON of the femoral head. Some of these modalities, such as plain radiographs and MRI, have a proven and well-defined role in the clinical assessment of this disease process. However, other imaging technologies require further investigation before obtaining a definitive role in diagnostic evaluation of patients.
When encountering a patient who is at high risk for ON, plain radiographs are a necessary first step in diagnosis. In addition, an MRI should be obtained if suspicion is high but radiographs are negative. However, in advanced stages of the disease involving a minimal subchondral fracture, CT scanning may be useful in accurately identifying the presence of subchondral collapse where MRI is often insufficient (Fig. 2). We do not recommend the use of bone scans in radiographic evaluation, and PET scanning has yet to gain a clearly defined role in radiographic evaluation. Future research should focus on improving the diagnostic capabilities of current imaging technologies. Furthermore, as new technologies continue to develop, investigations should focus on how these technologies can be used as adjuncts to current technologies for evaluating ON.
Compliance with Ethics Guidelines
Conflict of Interest
Todd P. Pierce, Julio J. Jauregui, Jeffrey J. Cherian, and Randa K. Elmallah declare that they have no conflict of interest.
Michael A. Mont has received grants and personal fees from Stryker, Wright Medical Technology, Inc., DJ Orthopaedics, Joint Active Systems, Sage Products, Inc., and TissueGene. Dr. Mont has also received personal fees from Janssen, Medical Compression Systems, Medtronic, and grants from the National Institutes of Health (NIAMS & NICHD). Dr. Mont also serves on the editorial/governing board of the American Journal of Orthopedics, Journal of Arthroplasty, Journal of Bone and Joint Surgery (American), Journal of Knee Surgery, Orthopedics, and Surgical Techniques International and is also a board member/committee appointment for the AAOS Society.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Modern Surgical Treatment of Hip Avascular Necrosis
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Arlet J, Ficat P. Non-traumatic avascular femur head necrosis. New methods of examination and new concepts. Chir Narzadow Ruchu Ortop Pol. 1977;42(3):269. [PubMed] [Google Scholar]
- 2.Steinberg ME, Hayken GD, Steinberg DR. A quantitative system for staging avascular necrosis. J Bone Joint Surg Br. 1995;77(1):34. [PubMed] [Google Scholar]
- 3.Lieberman JR, Berry DJ, Mont MA, Aaron RK, Callaghan JJ, Rajadhyaksha AD, et al. Osteonecrosis of the hip: management in the 21st century. Instr Course Lect. 2003;52:337. [PubMed] [Google Scholar]
- 4.••.Pivec R, Johnson AJ, Harwin SF, Mont MA. Differentiation, diagnosis, and treatment of osteoarthritis, osteonecrosis, and rapidly progressive osteoarthritis. Orthopedics. 2013;36(2):118. doi: 10.3928/01477447-20130122-04. [DOI] [PubMed] [Google Scholar]
- 5.Zalavras CG, Lieberman JR. Osteonecrosis of the femoral head: evaluation and treatment. J Am Acad Orthop Surg. 2014;22(7):455. doi: 10.5435/JAAOS-22-07-455. [DOI] [PubMed] [Google Scholar]
- 6.Zhao DW, Hu YC. Chinese experts' consensus on the diagnosis and treatment of osteonecrosis of the femoral head in adults. Orthop Surg. 2012;4(3):125. doi: 10.1111/j.1757-7861.2012.00192.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nelson FR, Bhandarkar VS, Woods TA. Using hip measures to avoid misdiagnosing early rapid onset osteoarthritis for osteonecrosis. J Arthroplast. 2014;29(6):1243. doi: 10.1016/j.arth.2013.11.010. [DOI] [PubMed] [Google Scholar]
- 8.Hou CH, Shih TT, Liu CY, Li YD, Enright T. Proton MR spectroscopy of the femoral head—evaluation of patients at risk for avascular necrosis. J Magn Reson Imaging : JMRI. 2006;24(2):409. doi: 10.1002/jmri.20653. [DOI] [PubMed] [Google Scholar]
- 9.Ikemura S, Yamamoto T, Motomura G, Nakashima Y, Mawatari T, Iwamoto Y. MRI evaluation of collapsed femoral heads in patients 60 years old or older: differentiation of subchondral insufficiency fracture from osteonecrosis of the femoral head. AJR Am J Roentgenol. 2010;195(1):W63. doi: 10.2214/AJR.09.3271. [DOI] [PubMed] [Google Scholar]
- 10.Oner AY, Aggunlu L, Akpek S, Celik A, Le Roux P, Tali T, et al. Staging of hip avascular necrosis: is there a need for DWI? Acta Radiol. 2011;52(1):111. doi: 10.1258/ar.2010.100231. [DOI] [PubMed] [Google Scholar]
- 11.Petrigliano FA, Lieberman JR. Osteonecrosis of the hip: novel approaches to evaluation and treatment. Clin Orthop Relat Res. 2007;465:53. doi: 10.1097/BLO.0b013e3181591c92. [DOI] [PubMed] [Google Scholar]
- 12.Karantanas AH. Accuracy and limitations of diagnostic methods for avascular necrosis of the hip. Expert Opin Med Diagn. 2013;7(2):179. doi: 10.1517/17530059.2013.757592. [DOI] [PubMed] [Google Scholar]
- 13.Lavernia CJ, Sierra RJ, Grieco FR. Osteonecrosis of the femoral head. J Am Acad Orthop Surg. 1999;7(4):250. doi: 10.5435/00124635-199907000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Malizos KN, Karantanas AH, Varitimidis SE, Dailiana ZH, Bargiotas K, Maris T. Osteonecrosis of the femoral head: etiology, imaging and treatment. Eur J Radiol. 2007;63(1):16. doi: 10.1016/j.ejrad.2007.03.019. [DOI] [PubMed] [Google Scholar]
- 15.Kerboul M, Thomine J, Postel M, Merle d'Aubigne R. The conservative surgical treatment of idiopathic aseptic necrosis of the femoral head. J Bone Joint Surg Br. 1974;56(2):291. [PubMed] [Google Scholar]
- 16.Ha YC, Jung WH, Kim JR, Seong NH, Kim SY, Koo KH. Prediction of collapse in femoral head osteonecrosis: a modified Kerboul method with use of magnetic resonance images. J Bone Joint Surg Am. 2006;88(Suppl 3):35. doi: 10.2106/JBJS.F.00535. [DOI] [PubMed] [Google Scholar]
- 17.Takao M, Nishii T, Sakai T, Yoshikawa H, Sugano N. Repair in osteonecrosis of the femoral head: MR imaging features at long-term follow-up. Clin Rheumatol. 2010;29(8):841. doi: 10.1007/s10067-010-1404-8. [DOI] [PubMed] [Google Scholar]
- 18.Gross TP, Liu F. Is there added risk in resurfacing a femoral head with cysts? J Orthop Surg Res. 2011;6:55. doi: 10.1186/1749-799X-6-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mont MA, Seyler TM, Ulrich SD, Beaule PE, Boyd HS, Grecula MJ, et al. Effect of changing indications and techniques on total hip resurfacing. Clin Orthop Relat Res. 2007;465:63. doi: 10.1097/BLO.0b013e318159dd60. [DOI] [PubMed] [Google Scholar]
- 20.Lee GC, Khoury V, Steinberg D, Kim W, Dalinka M, Steinberg M. How do radiologists evaluate osteonecrosis? Skelet Radiol. 2014;43(5):607. doi: 10.1007/s00256-013-1803-4. [DOI] [PubMed] [Google Scholar]
- 21.Mont MA, Jones LC, Pacheco I, Hungerford DS. Radiographic predictors of outcome of core decompression for hips with osteonecrosis stage III. Clin Orthop Relat Res. 1998;354:159. doi: 10.1097/00003086-199809000-00019. [DOI] [PubMed] [Google Scholar]
- 22.Cherian SF, Laorr A, Saleh KJ, Kuskowski MA, Bailey RF, Cheng EY. Quantifying the extent of femoral head involvement in osteonecrosis. J Bone Joint Surg Am. 2003;85-A(2):309. doi: 10.2106/00004623-200302000-00019. [DOI] [PubMed] [Google Scholar]
- 23.Beltran J, Herman LJ, Burk JM, Zuelzer WA, Clark RN, Lucas JG, et al. Femoral head avascular necrosis: MR imaging with clinical-pathologic and radionuclide correlation. Radiology. 1988;166(1 Pt 1):215. doi: 10.1148/radiology.166.1.3336682. [DOI] [PubMed] [Google Scholar]
- 24.Coleman BG, Kressel HY, Dalinka MK, Scheibler ML, Burk DL, Cohen EK. Radiographically negative avascular necrosis: detection with MR imaging. Radiology. 1988;168(2):525. doi: 10.1148/radiology.168.2.3393676. [DOI] [PubMed] [Google Scholar]
- 25.Hauzeur JP, Pasteels JL, Schoutens A, Hinsenkamp M, Appelboom T, Chochrad I, et al. The diagnostic value of magnetic resonance imaging in non-traumatic osteonecrosis of the femoral head. J Bone Joint Surg Am. 1989;71(5):641. [PubMed] [Google Scholar]
- 26.Thickman D, Axel L, Kressel HY, Steinberg M, Chen H, Velchick M, et al. Magnetic resonance imaging of avascular necrosis of the femoral head. Skelet Radiol. 1986;15(2):133. doi: 10.1007/BF00350207. [DOI] [PubMed] [Google Scholar]
- 27.Markisz JA, Knowles RJ, Altchek DW, Schneider R, Whalen JP, Cahill PT. Segmental patterns of avascular necrosis of the femoral heads: early detection with MR imaging. Radiology. 1987;162(3):717. doi: 10.1148/radiology.162.3.3809485. [DOI] [PubMed] [Google Scholar]
- 28.Fordyce MJ, Solomon L. Early detection of avascular necrosis of the femoral head by MRI. J Bone Joint Surg Br. 1993;75(3):365. doi: 10.1302/0301-620X.75B3.8496201. [DOI] [PubMed] [Google Scholar]
- 29.Wu Z, Yan X, Liu Z, Pan S, Cao X. Avascular necrosis of the femoral head: MR imaging with radiological and histological correlation. Chin Med J. 1998;111(7):599. [PubMed] [Google Scholar]
- 30.Zibis AH, Karantanas AH, Roidis NT, Hantes ME, Argiri P, Moraitis T, et al. The role of MR imaging in staging femoral head osteonecrosis. Eur J Radiol. 2007;63(1):3. doi: 10.1016/j.ejrad.2007.03.029. [DOI] [PubMed] [Google Scholar]
- 31.Miller IL, Savory CG, Polly DW, Jr., Graham GD, McCabe JM, Callaghan JJ. Femoral head osteonecrosis. Detection by magnetic resonance imaging versus single-photon emission computed tomography. Clin Orthop Relat Res. 1989;247:152–162. [PubMed]
- 32.Bassett LW, Gold RH, Reicher M, Bennett LR, Tooke SM. Magnetic resonance imaging in the early diagnosis of ischemic necrosis of the femoral head. Preliminary results. Clin Orthop Relat Res. 1987;214:237. [PubMed] [Google Scholar]
- 33.Lang P, Genant HK, Jergesen HE, Murray WR. Imaging of the hip joint. Computed tomography versus magnetic resonance imaging. Clin Orthop Relat Res. 1992;274:135. [PubMed] [Google Scholar]
- 34.Ragab Y, Emad Y, Abou-Zeid A. Bone marrow edema syndromes of the hip: MRI features in different hip disorders. Clin Rheumatol. 2008;27(4):475. doi: 10.1007/s10067-007-0731-x. [DOI] [PubMed] [Google Scholar]
- 35.Koo KH, Ahn IO, Kim R, Song HR, Jeong ST, Na JB, et al. Bone marrow edema and associated pain in early stage osteonecrosis of the femoral head: prospective study with serial MR images. Radiology. 1999;213(3):715. doi: 10.1148/radiology.213.3.r99dc06715. [DOI] [PubMed] [Google Scholar]
- 36.Huang GS, Chan WP, Chang YC, Chang CY, Chen CY, Yu JS. MR imaging of bone marrow edema and joint effusion in patients with osteonecrosis of the femoral head: relationship to pain. AJR Am J Roentgenol. 2003;181(2):545. doi: 10.2214/ajr.181.2.1810545. [DOI] [PubMed] [Google Scholar]
- 37.Mitchell DG, Rao V, Dalinka M, Spritzer CE, Gefter WB, Axel L, et al. MRI of joint fluid in the normal and ischemic hip. AJR Am J Roentgenol. 1986;146(6):1215. doi: 10.2214/ajr.146.6.1215. [DOI] [PubMed] [Google Scholar]
- 38.Bluemke DA, Zerhouni EA. MRI of avascular necrosis of bone. Top Magn Reson Imaging : TMRI. 1996;8(4):231. doi: 10.1097/00002142-199608000-00003. [DOI] [PubMed] [Google Scholar]
- 39.••.Liu B, Yi H, Zhang Z, Li Z, Yue D, Sun W. Association of hip joint effusion volume with early osteonecrosis of the femoral head. Hip Int : J Clin Exp Res Hip Pathol Ther. 2012;22(2):179. doi: 10.5301/HIP.2012.9237. [DOI] [PubMed] [Google Scholar]
- 40.Zhao FC, Li ZR, Zhang NF, Wang BL, Sun W, Cheng LM, et al. Lesion size changes in osteonecrosis of the femoral head: a long-term prospective study using MRI. Int Orthop. 2010;34(6):799. doi: 10.1007/s00264-009-0829-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yeh LR, Chen CK, Huang YL, Pan HB, Yang CF. Diagnostic performance of MR imaging in the assessment of subchondral fractures in avascular necrosis of the femoral head. Skelet Radiol. 2009;38(6):559. doi: 10.1007/s00256-009-0659-0. [DOI] [PubMed] [Google Scholar]
- 42.Stevens K, Tao C, Lee SU, Salem N, Vandevenne J, Cheng C, et al. Subchondral fractures in osteonecrosis of the femoral head: comparison of radiography, CT, and MR imaging. AJR Am J Roentgenol. 2003;180(2):363. doi: 10.2214/ajr.180.2.1800363. [DOI] [PubMed] [Google Scholar]
- 43.Mitchell DG, Kressel HY, Arger PH, Dalinka M, Spritzer CE, Steinberg ME. Avascular necrosis of the femoral head: morphologic assessment by MR imaging, with CT correlation. Radiology. 1986;161(3):739. doi: 10.1148/radiology.161.3.3786725. [DOI] [PubMed] [Google Scholar]
- 44.•.Barille MF, Wu JS, McMahon CJ. Femoral head avascular necrosis: a frequently missed incidental finding on multidetector CT. Clin Radiol. 2014;69(3):280. doi: 10.1016/j.crad.2013.10.012. [DOI] [PubMed] [Google Scholar]
- 45.Sedonja I, Jevtic V, Milcinski M. Bone scintigraphy as a prognostic indicator for bone collapse in the early phases of femoral head osteonecrosis. Ann Nucl Med. 2007;21(3):167. doi: 10.1007/s12149-007-0001-7. [DOI] [PubMed] [Google Scholar]
- 46.Alavi A, McCloskey JR, Steinberg ME. Early detection of avascular necrosis of the femoral head by 99m technetium diphosphonate bone scan: a preliminary report. Clin Orthop Relat Res. 1977;127:137–141. [PubMed]
- 47.Mont MA, Ulrich SD, Seyler TM, Smith JM, Marker DR, McGrath MS, et al. Bone scanning of limited value for diagnosis of symptomatic oligofocal and multifocal osteonecrosis. J Rheumatol. 2008;35(8):1629. [PubMed] [Google Scholar]
- 48.Schiepers C, Broos P, Miserez M, Bormans G, De Roo M. Measurement of skeletal flow with positron emission tomography and 18F-fluoride in femoral head osteonecrosis. Arch Orthop Trauma Surg. 1998;118(3):131. doi: 10.1007/s004020050332. [DOI] [PubMed] [Google Scholar]
- 49.Mont MA, Jones LC, Sotereanos DG, Amstutz HC, Hungerford DS. Understanding and treating osteonecrosis of the femoral head. Instr Course Lect. 2000;49:169. [PubMed] [Google Scholar]
- 50.Nguyen BD, Roarke MC. F-18 FDG PET/CT incidental finding of large ischiogluteal bursitis. Clin Nucl Med. 2007;32(7):535. doi: 10.1097/RLU.0b013e3180646ad3. [DOI] [PubMed] [Google Scholar]
- 51.Dasa V, Adbel-Nabi H, Anders MJ, Mihalko WM. F-18 fluoride positron emission tomography of the hip for osteonecrosis. Clin Orthop Relat Res. 2008;466(5):1081. doi: 10.1007/s11999-008-0219-2. [DOI] [PMC free article] [PubMed] [Google Scholar]


