Abstract
Osteonecrosis of the femoral head (ONFH) is a challenging diagnosis for the patient and treating surgeon. Though its cause is poorly understood, several methods of surgical treatment exist and are performed with variable success. Vascularized bone grafting is one such treatment that attempts to restore viable bone, structural support, and blood supply to the avascular portion of the femoral head. This review summarizes the various approaches to this technique that have been proposed and put into practice. The cost effectiveness of these procedures, both in time and resources, has been evaluated and found to be favorable. The use of revascularization procedures, along with the introduction of other potentiating factors, may signal an exciting future for this debilitating disease process.
Keywords: Osteonecrosis, Femoral, Head, Vascularized, Graft, Comparison
Introduction
Osteonecrosis of the femoral head (ONFH) is a challenging and often debilitating diagnosis. The process itself is multifactorial and not completely understood. As the disease progresses, patients experience increased pain and dysfunction, often resulting in severe disability [1]. Once articular surface collapse begins, rapid development of arthrosis is imminent, further limiting the patient [2].
The exact pathophysiology of the process has not been fully elucidated. Some patients have a history of direct insult to the bone, such as trauma (fracture or traumatic dislocation), radiation, and Caisson disease [3]. More indirect, non-traumatic, insults are also well studied. These include excessive alcohol use and the prolonged use of corticosteroids. Inherited coagulation disorders, as well as sickle cell disease, can increase a patient’s predilection towards AVN [4]. Recently, investigation into genetic predisposition outside of hematological causes has shown promise, with hopes to identify at-risk patients. However, all investigators conclude that the disease is multifactorial and likely a combination of inherent predisposition and external insult.
Treatment of the disease focuses on preservation or restoration of the femoral head blood supply and structural support within the femoral head. This in turn aims to arrest osteonecrosis and theoretically allow for return of normal bone metabolism. The goal of all forms of treatment is to maintain the patient’s anatomy as long as possible, delaying the need for arthroplasty in this young patient population [5]. Options for treatment are varied and include core decompression, osteotomy, and bone graft. When bone grafting, the surgeon can choose between vascularized and non-vascularized options [1]. The focus of this article will be placed on vascularized bone graft options in treatment of osteonecrosis of the femoral head.
Why vascularized bone graft?
The ultimate goal of any intervention in patients stricken with osteonecrosis of the femoral head (ONFH) is preservation of the hip joint. In ONFH, the articular surface of the femoral head loses the support of the subchondral bone. As the blood supply to the femoral head decreases, the subchondral bone dies. Though dead bone itself is hard and structurally sound, resorption of the dead bone by osteoclasts weakens its integrity. Without the underlying support of this bone, the arch of the femoral head can flatten and collapse, leading to disruption of the smooth gliding surface of the hip joint.
If left untreated, ONFH will almost invariably progress, though rate of progression is difficult to predict. In patients with unilateral disease, clinical progression may be punctuated with painless periods lasting months or even years. Patients with bilateral ONFH show more swift progression to significant disease within several years from the onset of symptoms. Radiographically, progression is more predictable. When patients with diagnosed ONFH are followed without intervention, about 22 % of patients will show collapse within the first year, with an increase to 37 % by 2 years. After 3 years, 75 % of patients show significant collapse [6].
Phemister first described the use of bone graft for treatment of femoral head osteonecrosis in 1930 [7]. Non-vascularized fibular bone graft was used to fill the space left behind after surgical removal of the necrotic bone. The hypothesis was that bone graft would act as support for the femoral head articular surface and scaffolding for influx of progenitor cells and the laying down of new bone. Multiple techniques have since been documented, allowing uncomplicated access to the area of bony necrosis and implantation of bone graft. Successful outcomes have been documented at 2–15 years [5, 8–13]. Improvement in outcome scores between vascularized and non-vascularized bone grafting is reported as 70 versus 35 %, and the rate of conversion to total hip replacement was nearly double in the non-vascularized group [14].
The theoretical advantage of vascularized bone graft is the inclusion of a new blood supply at the time of surgery and increasing the function of the graft beyond mere scaffolding for slow-moving creeping substitution. Direct revascularization of the bone allows for the invasion of osteoinductive progenitor cells, revitalizing the once necrotic zone, leading to restoration of a healthy subchondral plate (Fig. 1) [5]. Described methods of bone grafting with vascularized bone include iliac crest and greater trochanteric bone pedicle graft, as well as free vascularized fibular graft [8, 9, 11, 15–17].
Fig. 1.
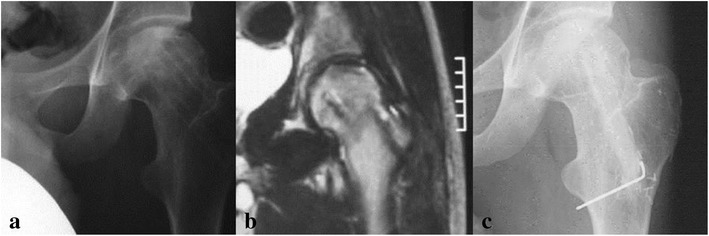
a Plain films of a 23-year-old male with ONFH after displaced subcapital fracture. b MRI of same patient. c Plain films 5 years postop from free vascularized fibular graft, revealing maintenance of the femoral head architecture
Comparison of non-vascularized and vascularized bone graft has yielded supportive results. Trousdale et al. compared free vascularized fibular graft with core decompression for patients with ONFH. He prospectively studied 34 patients (39 hips), 20 of which were treated with free vascularized fibular graft (FVFG) and 19 with core decompression. Postoperative follow-up ranged from 2 to 5 years, with definition of failure of surgery as conversion to total hip arthroplasty. Among the core decompression group, 58 % failed postoperatively, compared to a significantly lower 20 % in the FVFG group [14].
Kim et al. in 2005 compared 19 patients (23 hips) who underwent free vascularized fibular graft with 19 patients (23 hips) who underwent non-vascularized fibular graft. The patients’ preoperative lesions were evaluated via the Steinberg classifications, and the groups were matched according to lesion size and level of collapse. After a mean follow-up of 4 years, the vascularized patients enjoyed significantly better increase in outcome scores (70 % increase versus 35 % in the non-vascularized group), as well as significantly decreased postoperative dome depression and rate of collapse when compared to non-vascularized group [18].
Indications/contraindications
Vascularized grafting to the necrotic femoral head is a complex, multi-faceted procedure. Careful consideration must be applied to patient selection. In general, the procedure is considered ideal for young, active patients with ONFH [5]. The goal with this patient population is to avoid artificial joints as long as possible. Though there is no accepted absolute exclusion for age, patients’ greater than 50 years should be closely evaluated for total hip arthroplasty [15, 19]. As issues with fixation and wear continue to improve, the upper age limit in for the consideration of vascularized bone grafting continues to decrease.
Severity of lesion must also be considered, and this is typically defined by the size of the lesion and presence or absence of chondral collapse. In general, it is accepted that the ideal patient exhibits a small lesion, with no evidence of collapse of the articular surface on either plain films or advanced imaging [5, 15, 20]. There are different methods for defining lesion size. Kawate et al. in 2007 concluded that small lesions, defined as the sum of the encompassing angle of the lesion in the AP and lateral plain films being <300°, in patients with Steinberg stage I or II lesions, were ideal candidates for FVFG [20]. Patients with lesions >300° should be considered for total hip arthroplasty (THA) [20]. With the advent of cross sectional imaging, size has also been described in volumetric terms with <25 % of the femoral head by volume considered small and given a category of A by Urbaniak, 25–50 % categorized as B, and greater than 50 % as C [21].
For evaluation of the articular surface, classification systems such as Ficat, or the Steinberg Classification (a modified scale based on Ficat’s), can be employed. Aldridge et al. in 2006 recommend the Ficat classification in determining a patient’s fitness for FVFG. Recent studies have shown 88 % success rate with vascularized grafting in Ficat stage I and II (no collapse), with success rates decreasing in stage III and IV patients (Table 1) [22]. Ficat stages of osteonecrosis of the femoral head are delineated in Table 1. Outcomes in patients that are pre-collapse are more favorable than those with evidence of collapse, and literature suggests that this is a more telling preoperative factor than size [15, 21].
Table 1.
Ficat stages of osteonecrosis
| 0 | No findings on imaging (silent hip) |
| I | Possible slight abnormality with patchy/opaque areas. No collapse |
| IIA | Changes evident. Diffuse focal lesions |
| IIB | “Crescent sign” (subchondral fracture). Femoral head flattened in areas |
| III | Bone sequestrum. Edge of femoral head appears jagged/abnormal. Normal joint space |
| IV | Edge of femoral head completely flattened (collapsed). Reduced joint space. Acetabular degradation |
The effect of acetabular coverage has also been reviewed. Roush correlated the center-edge angle (CEA) with survivorship of vascularized graft in 200 hips [23]. He determined that patients with CEA >30 resulted in significantly less progression of collapse and eventual conversion to THA when compared to patients with CEA <30 [23].
Types of vascularized bone graft
Though the benefits of vascular grafts are well recognized, the treating surgeon must determine which graft is best suitable to the patient’s needs, as well as his or her own abilities and experience. There are several established options when addressing osteonecrosis of the femoral head.
Iliac crest vascularized graft
Iliac crest vascularized graft (ICVG) is a well-tested vascularized pedicle graft when treating ONFH. In order to harvest the graft, the patient is placed in the supine position, and a curvilinear incision is made along the iliac crest, continuing distally to the level of the lesser trochanter. The deep circumflex iliac artery is identified and dissected along the inguinal ligament until it enters the bony crest. The desired bony graft is then measured and removed. Cancellous bony graft can also be harvested from the crest at this time.
Though there is some variation, the next step involves exposure of the hip, usually via the Smith-Petersen approach. The capsule is then excised anteriorly, exposing the femoral neck and head/neck junction. A bony trough is then made at the head/neck junction, with placement altered slightly depending on the location of the lesion. The necrotic bone is then identified and removed under direct visualization.
Once the donor site is prepared, the graft is then passed under the inguinal ligament, through the belly of the iliacus and above the reflected head of the biceps femoris. The lesion is then packed with cancellous graft, and the vascularized pedicle is inserted in such as fashion that the pedicle is unimpeded, and the distal portion of the graft is abutting the subchondral plate (Fig. 3b).
Fig. 3.
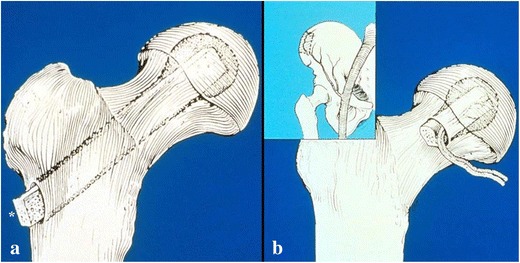
a Fibular strut graft (of note, in free vascularized fibular grafts, the pedicle will exit the distal end of the decompression tunnel (asterisk). b Iliac crest vascularized bone graft at harvest site (inset) and placed after decompression
Results of vascularized iliac crest have been extensively studied. Eisenschenk reviewed 80 patients who underwent ICVG for ONFH, with mean follow-up of 5 years. Harris Hip Scores (HHS) were 86.8 % good or excellent for his patients, with over half of the patients exhibiting no radiographic progression of disease at final follow-up [12]. Hasegawa et al. compared ICVG to core decompression and non-vascularized fibular graft for treatment of ONFH. He also employed HHS, with average follow-up of 8 years. While 63 % reported good-excellent results postop, the results were only “slightly” better than core decompression and revealed no significant difference when compared to non-vascularized fibular graft. Of note, the authors also state technical difficulty in removing in entirety the necrotic bone within the femoral head beneath the subchondral bone, and with evaluating and restoring femoral head sphericity, making treatment of advanced lesions difficult [16]. Pavlocic’s data supports this conclusion. He used ICVG to treat 24 patients with Ficat II and III lesions, and determined ICVG to be most valuable in patients with pre-collapse lesions, or very mild Ficat III disease [24].
Some surgeons have combined the use of ICVG with rotation osteotomy in the treatment of ONFH to address advanced lesions. Matsusaki reported on 14 patients (17 hips) treated with ICVG and transtrochanteric anterior rotational osteotomy for ONFH with >2/3 of the weight-bearing surface involved [17] According to the authors, the osteotomy relieved the involved surface of its weight-bearing, while revascularizing the subchondral plate. Average postoperative follow-up was over 4 years. Patients showed an average improvement of over 10 points in their Japanese Orthopedic Association (JOA) score, which measures pain, gait, range of motion, and ability to perform ADLs effectively. The JOA score has been widely used in Japan, and found to correlate closely with outcome, suggesting substantial improvement in Matsusaki’s patients [25]. Matsusaki also reported that 71 % of patients showed no progression of their disease [17].
Noguchi reported his results comparing ICVG versus ICVG with simultaneous rotational osteotomy in the treatment of lesions >2/3 of the femoral head [25, 26]. He studied 18 hips, with stage II and III lesions according to the Japanese Investigation Committee (JIC), a modification of the well-known Ficat classification. The authors focused on the stage II patients, 4 of which underwent ICVG only, and 10 of whom underwent ICVG with rotational osteotomy. Of the ICVG-only group, there was about a 5-point increase in the JOA score, with 75 % of patients showing progression of their disease on imaging. The patients who underwent ICVG with osteotomy had an average 13-point increase in JOA scores, with only 20 % showing disease progression on imaging at a mean 1 year postoperatively [26]. Specific complications include lateral thigh paresthesias, superficial infection, and inguinal hernia.
Free vascularized fibular graft
With the advent of advanced operative microscopy in the 1970s, the development of harvest and free transfer of a vascularized fibular graft was developed simultaneously, but separately, at several institutions [5]. The technique consists of harvesting the fibula and preparation of the graft site, either by two teams in concert, or by a single team in a stepwise fashion. The patient is placed in the lateral decubitus position, and the hip is approached via a curved, anterolateral incision (Fig. 2a) [27]. The fascia lata is incised longitudinally, extending proximally between the gluteus maximus and tensor fascia lata, exposing the proximolateral femur. Deep dissection continues deep to the abductors and rectus femoris, permitting the dissection of the donor vessels, which are usually the ascending branches of the lateral femoral circumflex artery and its accompanying veins [28]. A Steinmann pin is inserted from the lateral femur through the neck into the femoral head lesion under fluoroscopic guidance. Sequential reamers are introduced over the pin, and reaming continues until a tunnel of sufficient diameter to allow placement of the fibula strut is achieved, with reaming continuing proximally to within about 5 mm from the articular surface of the femoral head. Remaining necrotic bone is then removed with a curette, while using fluoroscopy to evaluate the borders of the lesion. Contrast dye can be injected into the tunnel to further appreciate its characteristics [5]. Viable cancellous reamings and autograft harvested from the greater trochanter are packed into the tunnel once the necrotic bone is removed.
Fig. 2.
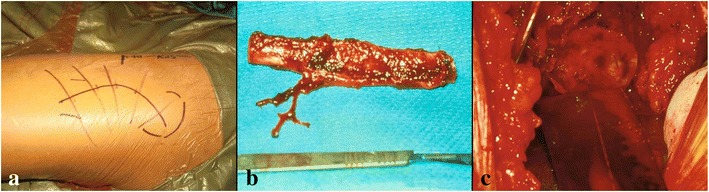
a The hip is approached via a curved, anterolateral incision while the patient is in the lateral decubitus position. b The harvested fibula, with the peroneal artery and vein dissected. c The fibular graft in place, with resultant bleeding from within the fibular canal
The ipsilateral fibula is approached via a lateral incision, described by Judet [29]. The peroneal vessel pedicle is identified and freed from surrounding soft tissue. Proximal and distal osteotomies are performed, and the graft is freed. The final steps of this portion of the case can be delayed if needed until the femur is prepared to accept the graft [28].
Once the fibula is prepared and the tunnel is complete, the graft can be released from the donor site and introduced into the femoral tunnel (Fig. 2b). The graft is placed such that the pedicle is unimpeded and patent, and so the fibular graft is abutting the subchondral plate and newly introduced cancellous graft (Fig. 3a). The graft is then secured with a Kirschner wire, and the arterial and venous anastomoses are performed with the aid of microscopy. Blood flow into the graft is confirmed by seeing endosteal bleeding inside the fibular canal (Fig. 2c) [5].
Several studies have closely analyzed the outcomes of FVFG in the treatment of ONFH. Yoo et al. in 1992 reported on 81 patients with a mean follow-up of 5 years, 2 months [30]. The patient population consisted of 59 patients with Ficat II lesions and 22 with Ficat III lesions. Patient outcomes were assessed with HHS. Ninety-one percent of patients reported good to excellent results (56 Ficat II patients, 18 Ficat III patients). Radiographic evaluation showed improved or unchanged disease postoperatively in 89 % of patients [30].
Judet et al. reported on 60 patients (68 hips) status post FVFG of ONFH, with impressive 18-year average follow-up (range 15–22 years) [31]. Of these patients, 52 % reported good results. Though this number seems disappointing, further examination of the data reveals good results obtained in 80 % of patients under 40 years of age at time of surgery, and 80 % good results in patients with stage II or III disease, even if the lesion involved the majority of the head. The authors also postulate that, because their data spanned the entirety of their experience with the procedure, early patients were not as well selected as later patients, resulting in lower results [31].
This thought is echoed by Urbaniak et al., who has multiple large volume reports on the use of FVFG for the treatment of ONFH. In 1995, Urbaniak reported on 103 hips in 89 patients, with minimum follow-up of 4.5 years [32]. The population consisted of patients with stage II through stage V disease, according to the criteria of Marcus et al. [33]. Patients have significant improvements in their Harris Hip Scores across all stages, as well as decrease in pain medication usage in 86 % of the population. Eighty-one percent ultimately were satisfied in their decision to undergo FVFG [32].
The author returned to this subject in 2004 for an updated review. Of the 224 FVFG performed, an 88 % success rate, as defined by an absence of conversion to total hip arthroplasty, was reported in patients with Ficat stage I and II disease. For patients with stage III or IV disease, success rates drop to 78 %. As predicted by Judet, patient selection was refined, as at the time of review, the procedure was only offered to patients under the age of 50, with stage II, III, or IV disease. For patients under 20 years of age, stage V (a patient that according to authors has collapse with arthrosis) disease is thought to be acceptable. The development of this treatment protocol from the “experimental procedure” described by Judet to that employed by Urbaniak suggests the continued refinement necessary for this complex but effective surgery [5, 9, 31]. Complications of FVFG include subtrochanteric fractures (1 %), surgical site infection (0.03 %), and great toe plantar flexion contracture (3 %) [5].
Greater trochanter vascularized graft
Though less commonly employed, the greater trochanter vascularized graft (GTVG) has been described in the literature [34, 35]. The patient is placed supine with the operative ilium elevated to sixty degrees. A skin incision is made 4 cm distal to the crest, and extended distally to the level of the greater trochanter, then vertically along the anterior aspect of the trochanter. Dissection continues until the transverse branch of the lateral femoral circumflex artery is identified. The vessels are followed to the point where they enter the greater trochanter. From this point, a 3 cm × 2 cm vascularized block is excised from the bone of the greater trochanter, taking care not to release more than 30 % of the insertion of the gluteus medius. Cancellous autograft can also be harvested at this time from the remaining greater trochanter. A T-type capsulotomy is then performed, and a “partial dislocation” is employed, in order to evaluate the cartilage of the acetabulum and femoral head by direct visualization. A 2 cm × 2 cm bony window in this made at the head/neck junction, and the necrotic bone is removed. The lesion is then packed with cancellous graft, and the GTVG is placed via the bony window, taking care not to place undue pressure on the soft tissue pedicle [34, 35].
Zhao et al. reported on 191 patients (195) hips treated with GTVG for ONFH, with mean follow-up of 8 years [34]. The patients had Ficat stage II–IV lesions. Twenty-three patients ultimately had conversion to THA. On average, the patient population who did not receive THA increased their HHS from 53 to 88 points. A survival analysis revealed no significant difference between the survival of a patient with stage II disease versus stage III disease at 11 years. One hundred eighteen of the patients showed no progression of disease at final postop follow-up [34]. Reported complications to surgery included chronic donor pain (11 %), deep vein thrombosis (4 %), and complications in wound healing (3 %) [34].
Comparison
As summarized above, there are multiple choices available to the surgeon wishing to treat ONFH with a vascularized graft. Though the literature abounds with studies dissecting every detail of these procedures independently, there are few that compare them side by side. Of those that do exist, the comparisons are limited to ICVG and FVFG, which are the two most often performed and studied.
The most direct comparison study was performed by Yen et al. in 2006. Here, the author compared 33 patients with ONFH treated with ICVG to 22 patients with the same condition, treated with FVFG [36•]. All patients had minimum follow-up of 3 years. Six parameters were evaluated: postoperative functional score, patient self-evaluation score, radiographs, rate of THA conversion, average OR time, and complications. Of the six parameters studied, functional score, patient score, radiographs, and conversion rate showed no significant difference. However, significant differences were found in OR time and complication rate. Average OR time for FVFG was found to be 7 h, versus the average 3.5 h for ICVG. However, complications were found to be significantly higher in the ICVG group (20.5 versus 4.5 %) [36•]. Complications for ICVG included lateral paresthesias, inguinal protrusion, and wound edge necrosis. Complications in the FVFG group included one patient with claw toe deformity [36•].
Though the author’s results seem clear, several factors must be considered. As discussed above, the OR time for FVFG can be shortened considerably if two surgical teams are operating concomitantly, decreasing the significance of the main point standing against the procedure in this study. Operative time for FVFG at our home institution is presently about 4 h. Furthermore, the complication rates of both FVFG and ICVG can be reduced by experienced surgeons operating at high volume centers.
Complications
There are several well-documented complications to vascularized bone grafting for the treatment of ONFH. Most large institutions report a low incident of infection. Aldridge et al. reported a total infection rate of only 0.2 %, noting that the resulting increased bleeding at the surgical site, combined with limited foreign body introduction, likely played a role. Contracture of the great toe is also commonly seen, though usually subclinical and easily improved with focused physical therapy in the early postoperative period [5, 37]. Motor weakness distal to the graft harvest site is a rare complication (less than 1 %) and usually resolved with time postoperatively. Injury/irritation of the peroneal nerve and its branches is seen during graft harvest but usually resolves without intervention. A review of 1270 FVFG revealed only one case of return to the OR for neurolysis of the peroneal nerve [7].
Specific to free vascularized fibular grafting is the complication of postoperative femoral fracture. Fracture occurs in the intertrochanteric or subtrochanteric region, usually 6 to 8 weeks postoperative as patients begin to increase their weight-bearing. Large institutions report this complication occurring between 0.7 to 1 %, with rates of fracture decreasing with experience and with limited cancellous bone harvest distal to the greater trochanter [5, 37].
Graft failure is a complication that must be considered when evaluating a patient for vascularized graft. Failure can be difficult to evaluate and predict postoperatively. A definition of failure can also be elusive, as in the case of vascularized grafting, the graft itself still provides mechanical support even if it is no longer vascularized. In a review of 16 patients s/p FVFG, Malizos et al. found 88 % of grafts to still be viable at time of conversion to total hip [38]. All 16 grafts showed some degree of bony union, with 3 of the 16 exhibiting complete union. The samples with partial healing exhibiting thick scarring between the end of the graft and the subchondral plate, leading Malizos to conclude that improved graft placement would result in increased buttressing effect, as well as encouraging more robust graft/host union [38].
Cost effectiveness
One criticism of the use of vascularized bone grafts in the treatment of ONFH is the cost. The complexity of these operations often implies the perception of high cost. This argument lead Watters et al. to compare the “cost effectiveness of free vascularized fibular graft (FVFG) to total hip arthroplasty for the treatment of symptomatic Ficat stage II and III osteonecrosis of the femoral head” [39•]. This was performed using a theoretical cohort of patients aged 30 years, with goals of comparing both average lifetime cost and collective Quality Adjusted Life Years gained from each procedure.
The results revealed a both a decrease in cost and an increase in QALY gained ($16,725 versus 22,657 and 22.23 versus 22.08 for FVFG versus THA, respectively). Though the study is limited by the relatively few cases in the literature, and is published out of an institution in which a high volume of both procedures are regularly performed, the results reveal that, in an age where cost of various procedures must be considered, vascularized bone grafting is an economically feasible option [39•].
The future
Vascularized bone grafts of all types are proven to provide multiple advantages in the treatment of ONFH. The next step in the development of these techniques appears to be the addition of new and exciting factors to their already effective characteristics. Aoyama et al. examined the addition of multipotent mesenchymal stem cells (MSCs) and β-tricalcium phosphate (β-TCP) to ICVG at time of operation in 10 patients with stage III ONFH [40•]. The patients were followed for a minimum of 2 years, and radiographic and outcome scores (JOA) were assessed. Nine patients completed the protocol. The average JOA score across all patients improved from 65.6 points to 87.9 points. Of the nine, 7 remained at stage III at final follow-up, where 2 advanced to stage IV [40•].
Similar, small studies have been completed with FVFG, exhibiting signs of potential in this multimodal therapy [41]. It remains to be seen whether the addition of stem cells to vascularized grafts will create a significant difference in objective and subjective outcomes.
Conclusions
Osteonecrosis of the femoral head is a complex, too often debilitating disease suffered by patients of all types. Preservation of the native hip is the goal of treatment for young and active patients, and the vascularized bone graft plays an integral part in returning them to normal activity. With experience and proper patient selection, any of these grafts can produce improved outcomes in this complex patient population. Careful considerations of the risks and benefits of each technique, as well as associated complications, must be employed before the surgeon enters the operating theater. Though well established as meaningful parts of the treatment of ONFH, vascular bone grafts will undoubtedly continue to improve as new technology evolves and refines these procedures for years to come.
Compliance with Ethics Guidelines
Conflict of Interest
Patrick D. Millikan and Vasili Karas declare that they have no conflict of interest. Samuel S. Wellman reports grants from Stryker, Zimmer, Biomet, and DePuy and personal fees from TJO.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Modern Surgical Treatment of Hip Avascular Necrosis
Contributor Information
Patrick D. Millikan, Phone: 8127602602, Email: patrick.millikan@dm.duke.edu
Vasili Karas, Phone: 8479031971, Email: vasili.karas@dm.duke.edu.
Samuel S. Wellman, Phone: 9196846166, Email: samuel.wellman@dm.duke.edu
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Zalavras CG, Lieberman JR. Osteonecrosis of the femoral head: evaluation and treatment. J Am Acad Orthop Surg. 2014;22(7):455–464. doi: 10.5435/JAAOS-22-07-455. [DOI] [PubMed] [Google Scholar]
- 2.Merle D’Aubigne R, Postel M, Mazabraud A, Massias P, Gueguen J, France P. Idiopathic necrosis of the femoral head in adults. J Bone Joint Surg (Br) 1965;47(4):612–633. [PubMed] [Google Scholar]
- 3.Mont MA, Jones LC, Hungerford DS. Nontraumatic osteonecrosis of the femoral head: ten years later. J Bone Joint Surg. 2006;88(5):1117–1132. doi: 10.2106/JBJS.E.01041. [DOI] [PubMed] [Google Scholar]
- 4.Hernigou P, Bachir D, Galacteros F. The natural history of symptomatic osteonecrosis in adults with sickle-cell disease. J Bone Joint Surg. 2003;85(3):500–504. doi: 10.2106/00004623-200303000-00016. [DOI] [PubMed] [Google Scholar]
- 5.Aldridge JM, III, Urbaniak JR. Avascular necrosis of the femoral head: role of vascularized bone grafts. Orthop Clin N Am. 2007;38(1):13–22. doi: 10.1016/j.ocl.2006.10.012. [DOI] [PubMed] [Google Scholar]
- 6.Marciniak D, Furey C, Shaffer JW. Osteonecrosis of the femoral head. A study of 101 hips treated with vascularized fibular grafting. J Bone Joint Surg Am. 2005;87(4):742–747. doi: 10.2106/JBJS.D.02004. [DOI] [PubMed] [Google Scholar]
- 7.Phemister DB. Treatment of the necrotic head of the femur in adults. J Bone Joint Surg. 1949;31(1):55–66. [PubMed] [Google Scholar]
- 8.Aldridge JM, 3rd, Berend KR, Gunneson EE, Urbaniak JR. Free vascularized fibular grafting for the treatment of postcollapse osteonecrosis of the femoral head. Surgical technique. J Bone Joint Surg Am. 2004;86-A(Suppl 1):87–101. doi: 10.2106/00004623-200403001-00012. [DOI] [PubMed] [Google Scholar]
- 9.Berend KR, Gunneson EE, Urbaniak JR. Free vascularized fibular grafting for the treatment of postcollapse osteonecrosis of the femoral head. J Bone Joint Surg Am. 2003;85-A(6):987–993. doi: 10.2106/00004623-200306000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Beris AE, Lykissas MG, Payatakes A, Kontogeorgakos VA, Mavrodontidis A, Korompilias AV. Free vascularized fibular graft for treatment of pathological femoral neck fracture and osteonecrosis of the femoral head: a case report with a long-term follow-up. Microsurgery. 2009;29(3):240–243. doi: 10.1002/micr.20598. [DOI] [PubMed] [Google Scholar]
- 11.Chen CC, Lin CL, Chen WC, Shih HN, Ueng SW, Lee MS. Vascularized iliac bone-grafting for osteonecrosis with segmental collapse of the femoral head. J Bone Joint Surg Am. 2009;91(10):2390–2394. doi: 10.2106/JBJS.H.01814. [DOI] [PubMed] [Google Scholar]
- 12.Eisenschenk A, Lautenbach M, Schwetlick G, Weber U. Treatment of femoral head necrosis with vascularized iliac crest transplants. Clin Orthop Relat Res. 2001;386:100–105. doi: 10.1097/00003086-200105000-00013. [DOI] [PubMed] [Google Scholar]
- 13.Jun X, Chang-Qing Z, Kai-Gang Z, Hong-Shuai L, Jia-Gen S. Modified free vascularized fibular grafting for the treatment of femoral neck nonunion. J Orthop Trauma. 2010;24(4):230–235. doi: 10.1097/BOT.0b013e3181be3ec3. [DOI] [PubMed] [Google Scholar]
- 14.Trousdale RT. Vascularized free fibula graft vs core decompression. Orthopedics. 1997;20(4):359. doi: 10.3928/0147-7447-19970401-20. [DOI] [PubMed] [Google Scholar]
- 15.Urbaniak JR, Harvey EJ. Revascularization of the femoral head in osteonecrosis. J Am Acad Orthop Surg. 1998;6(1):44–54. doi: 10.5435/00124635-199801000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Hasegawa Y, Iwata H, Torii S, Iwase T, Kawamoto K, Iwasada S. Vascularized pedicle bone-grafting for nontraumatic avascular necrosis of the femoral head. A 5- to 11-year follow-up. Arch Orthop Trauma Surg. 1997;116(5):251–258. doi: 10.1007/BF00390047. [DOI] [PubMed] [Google Scholar]
- 17.Matsusaki H, Noguchi M, Kawakami T, Tani T. Use of vascularized pedicle iliac bone graft combined with transtrochanteric rotational osteotomy in the treatment of avascular necrosis of the femoral head. Arch Orthop Trauma Surg. 2005;125(2):95–101. doi: 10.1007/s00402-004-0777-z. [DOI] [PubMed] [Google Scholar]
- 18.Kim SY, Kim YG, Kim PT, Ihn JC, Cho BC, Koo KH. Vascularized compared with nonvascularized fibular grafts for large osteonecrotic lesions of the femoral head. J Bone Joint Surg Am. 2005;87(9):2012–2018. doi: 10.2106/JBJS.D.02593. [DOI] [PubMed] [Google Scholar]
- 19.Dewei Z, Xiaobing Y. A retrospective analysis of the use of cannulated compression screws and a vascularised iliac bone graft in the treatment of displaced fracture of the femoral neck in patients aged < 50 years. Bone Joint J. 2014;96-B(8):1024–1028. doi: 10.1302/0301-620X.96B8.33002. [DOI] [PubMed] [Google Scholar]
- 20.Kawate K, Yajima H, Sugimoto K, Ono H, Ohmura T, Kobata Y, et al. Indications for free vascularized fibular grafting for the treatment of osteonecrosis of the femoral head. BMC Musculoskelet Disord. 2007;8:78. doi: 10.1186/1471-2474-8-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Eward WC, Rineer CA, Urbaniak JR, Richard MJ, Ruch DS. The vascularized fibular graft in precollapse osteonecrosis: is long-term hip preservation possible? Clin Orthop Relat Res. 2012;470(10):2819–2826. doi: 10.1007/s11999-012-2429-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lieberman JR, Berry DJ, Mont MA, Aaron RK, Callaghan JJ, Rajadhyaksha AD, et al. Osteonecrosis of the hip: management in the 21st century. Instr Course Lect. 2003;52:337–355. [PubMed] [Google Scholar]
- 23.Roush TF, Olson SA, Pietrobon R, Braga L, Urbaniak JR. Influence of acetabular coverage on hip survival after free vascularized fibular grafting for femoral head osteonecrosis. J Bone Joint Surg Am. 2006;88(10):2152–2158. doi: 10.2106/JBJS.E.00469. [DOI] [PubMed] [Google Scholar]
- 24.Pavlovcic V, Dolinar D, Arnez Z. Femoral head necrosis treated with vascularized iliac crest graft. Int Orthop. 1999;23(3):150–153. doi: 10.1007/s002640050334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kuribayashi M, Takahashi KA, Fujioka M, Ueshima K, Inoue S, Kubo T. Reliability and validity of the Japanese Orthopaedic Association hip score. J Orthop Sci. 2010;15(4):452–458. doi: 10.1007/s00776-010-1490-0. [DOI] [PubMed] [Google Scholar]
- 26.Noguchi M, Kawakami T, Yamamoto H. Use of vascularized pedicle iliac bone graft in the treatment of avascular necrosis of the femoral head. Arch Orthop Trauma Surg. 2001;121(8):437–442. doi: 10.1007/s004020100263. [DOI] [PubMed] [Google Scholar]
- 27.Marchant MH, Jr, Zura RD, Urbaniak JR, Aldridge JM., 3rd Hip incision planning for free vascularized fibular grafting of the proximal femur: a handy tip. J Surg Orthop Adv. 2007;16(4):204–206. [PubMed] [Google Scholar]
- 28.Soucacos PN, Beris AE, Malizos K, Koropilias A, Zalavras H, Dailiana Z. Treatment of avascular necrosis of the femoral head with vascularized fibular transplant. Clin Orthop Relat Res. 2001;386:120–130. doi: 10.1097/00003086-200105000-00016. [DOI] [PubMed] [Google Scholar]
- 29.Judet H, Judet J, Gilbert A. Vascular microsurgery in orthopaedics. Int Orthop. 1981;5(2):61–68. doi: 10.1007/BF00267835. [DOI] [PubMed] [Google Scholar]
- 30.Yoo MC, Chung DW, Hahn CS. Free vascularized fibula grafting for the treatment of osteonecrosis of the femoral head. Clin Orthop Relat Res. 1992;277:128–138. [PubMed] [Google Scholar]
- 31.Judet H, Gilbert A. Long-term results of free vascularized fibular grafting for femoral head necrosis. Clin Orthop Relat Res. 2001;386:114–119. doi: 10.1097/00003086-200105000-00015. [DOI] [PubMed] [Google Scholar]
- 32.Urbaniak JR, Coogan PG, Gunneson EB, Nunley JA. Treatment of osteonecrosis of the femoral head with free vascularized fibular grafting. A long-term follow-up study of one hundred and three hips. J Bone Joint Surg Am. 1995;77(5):681–694. doi: 10.2106/00004623-199505000-00004. [DOI] [PubMed] [Google Scholar]
- 33.Marcus ND, Enneking W, Massam RA. The silent hip in idiopathic aseptic necrosis. J Bone Joint Surg Am. 1973;55:1351–1366. [PubMed] [Google Scholar]
- 34.Zhao D, Wang B, Guo L, Yang L, Tian F. Will a vascularized greater trochanter graft preserve the necrotic femoral head? Clin Orthop Relat Res. 2010;468(5):1316–1324. doi: 10.1007/s11999-009-1159-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zeng YR, He S, Feng WJ, Li FL, Li J, Jian LY, et al. Vascularised greater trochanter bone graft, combined free iliac flap and impaction bone grafting for osteonecrosis of the femoral head. Int Orthop. 2013;37(3):391–398. doi: 10.1007/s00264-012-1773-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.•.Yen CY, Tu YK, Ma CH, Yu SW, Kao FC, Lee MS. Osteonecrosis of the femoral head: comparison of clinical results for vascularized iliac and fibula bone grafting. J Reconstr Microsurg. 2006;22(1):21–24. doi: 10.1055/s-2006-931902. [DOI] [PubMed] [Google Scholar]
- 37.Gaskill TR, Urbaniak JR, Aldridge JM., 3rd Free vascularized fibular transfer for femoral head osteonecrosis: donor and graft site morbidity. J Bone Joint Surg Am. 2009;91(8):1861–1867. doi: 10.2106/JBJS.H.01105. [DOI] [PubMed] [Google Scholar]
- 38.Malizos KN, Quarles LD, Dailiana ZH, Rizk WS, Seaber AV, Urbaniak JR. Analysis of failures after vascularized fibular grafting in femoral head necrosis. Orthop Clin N Am. 2004;35(3):305–314. doi: 10.1016/j.ocl.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 39.•.Watters TS, Browne JA, Orlando LA, Wellman SS, Urbaniak JR, Bolognesi MP. Cost-effectiveness analysis of free vascularized fibular grafting for osteonecrosis of the femoral head. J Surg Orthop Adv. 2011;20(3):158–167. [PubMed] [Google Scholar]
- 40.•.Aoyama T, Goto K, Kakinoki R, Ikeguchi R, Ueda M, Kasai Y, et al. An exploratory clinical trial for idiopathic osteonecrosis of femoral head by cultured autologous multipotent mesenchymal stromal cells augmented with vascularized bone grafts. Tissue Eng B Rev. 2014;20(4):233–242. doi: 10.1089/ten.teb.2014.0090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kawate K, Yajima H, Ohgushi H, Kotobuki N, Sugimoto K, Ohmura T, et al. Tissue-engineered approach for the treatment of steroid-induced osteonecrosis of the femoral head: transplantation of autologous mesenchymal stem cells cultured with beta-tricalcium phosphate ceramics and free vascularized fibula. Artif Organs. 2006;30(12):960–962. doi: 10.1111/j.1525-1594.2006.00333.x. [DOI] [PubMed] [Google Scholar]


