Abstract
Trochanteric valgus and varus correction osteotomies have been described with or without associated rotational correction. In the last decade, new techniques have been described, including femoral neck osteotomy, femoral head reorientation, relative neck lengthening, greater or lesser trochanter distalization, and femoral head reduction osteotomy. While the overall number of femoral osteotomies in the young patients has decreased because of the efficacy of primary total hip arthroplasties, those osteotomy techniques may expand the indications for femoral osteotomies in select patients who meet the indications.
Keywords: Osteotomy, Hip, Trochanteric, Perthes, Dysplasia, SCFE, Impingement, Surgical dislocation
Introduction
In the last 2 decades, advances in hip arthroplasty have led many surgeons to question the indications for osteotomies because of the described effectiveness of total hip arthroplasty (THA). However, the risk of multiple revisions in young patients reserves a role to the osteotomies of the proximal femur for treating deformities that may lead to the development of cartilage lesions or arthritis.
In the past, several osteotomies were described but the most frequently performed were trochanteric osteotomy (TO) valgus and varus correction, commonly associated with rotational correction. In the last decade, new techniques have been described including femoral neck osteotomy (FNO), femoral head reorientation (FHR), relative neck lengthening (RNL), greater or lesser trochanter distalization, and femoral head reduction osteotomy (FHRO). Although the overall number of femoral osteotomies has decreased, the addition of newer techniques may expand the indications for femoral osteotomies in young patients. Indications for proximal femoral osteotomies are shown in Table 1. The last 3 groups of procedures mentioned above, however, are routinely performed only by very select surgeons with extensive clinical experience. Consequently, the reported results may lack high evidence and the outcome may not be reproducible in widespread fashion.
Table 1.
Review of femoral osteotomies. (SCFE: slipped capital femoral epiphysis)
| Deformity | Procedure |
|---|---|
| Valgus femoral neck-diaphysis angle abnormality (ie, dysplasia) | Varus TO |
| Varus femoral neck-diaphysis angle abnormality (ie, subtrochanteric nonunion) | Valgus TO |
| Neck morphology abnormities (ie, SCFE or neck fracture consolidated in displaced position) | Surgical dislocation and neck osteotomies |
| Pelvitrochanteric impingement | Greater trochanter distalization with RNL |
| Ischiofemoral impingement | Lesser trochanter excision or distalization with RNL |
| Severe head deformity (ie, Perthes disease): | FHRO |
HRO femoral head reduction osteotomy, RNL relative neck lengthening, SCFE slipped capital femoral epiphysis, TO trochanteric osteotomy
Trochanteric osteotomies
Femoral osteotomies generally are classified as varus or valgus, referring to the aimed final geometry of the proximal femur. Corrections of rotation, length, and coronal plane abnormalities are usually associated with the varus/valgus correction to improve biomechanical forces, cartilage loading, and length inequalities.
Varus trochanteric osteotomies
Background
The most common indication for varus trochanteric osteotomies is hip dysplasia [1].
However, since previous studies suggested the acetabular deficiency as the major problem, femoral approaches were commonly performed if the reorientation of the entire acetabulum was not sufficient to obtain a complete correction of the deformity [2]. The femoral correction is mainly in varus but often is associated with a rotational change. Varus TO alone was described as successful in stopping minimal subluxation by some authors while other centers added a shelf plasty to the femoral osteotomy to improve results [3].
Indication and drawbacks
Although varus TO continues to be indicated as an additional correction to acetabular reorientation, isolated varus TO for dysplasia is currently rarely performed, with the exception of cases of combined high neck-shaft angle with an ipsilateral long leg in the face of mild dysplasia [4].
In general, the ideal candidate for a varus TO is a patient with a spherical femoral head, little or no acetabular dysplasia, with neck-shaft angle of more than 135° of valgus [4]. Also, an excessive anteversion is frequently associated with hip dysplasia and could be reduced with a subtrochanteric osteotomy.
Other rare indications are cases of osteonecrosis where flexion or flexion-varus TO may move the area of necrosis to a non-weight bearing area [5]. Varus TO presents also several drawbacks: the first is the residual deformity after bone union, which may be a problem for a future femoral stem placement [6].
This problem increases with the degree of displacement and excessive medial displacement of the distal fragment is contraindicated for these reasons [1].
Leg shortening is another drawback, especially if a full wedge is resected. This could be avoided with an opening wedge technique, but it is associated with longer time to bone union.
A Trendelenburg gait is common and may persist permanently in up to 30 % of patients [7, 8]. Cases of nonunion are also reported in literature [9•].
Furthermore, prominence of the greater trochanter because of varus positioning can predispose to bursitis over the plate and trochanter.
Results
Morscher’s summary of the large Swiss series reported the varus TO results separately, with nearly 90 % good to excellent long-term outcomes [10].
Iwase [11] followed 110 patients with hip dysplasia more than 20 years after TO, with nearly equal numbers of varus and valgus osteotomies. Varus osteotomy was performed for early hip arthritis. Using the endpoint of Harris hip score of less than 70 or a salvage surgery, the 10-year and 15-year survival rates for varus osteotomy were 89 %. The younger age (mean age 25 years) range in this series almost certainly was a factor in the excellent long-term outcomes, which included 82 % good to excellent 20-year results for their varus osteotomies. This compares favorably with the survivorship of primary THA in the young; in fact, the younger the patient, the better the short-term outcome and the worse the long-term outcome [12].
On the other hand, several parameters have been identified as negative predictors and are contraindications to a varus TO including age older than 40 years or obesity. Furthermore, a minimum of 15° of passive abduction preoperatively is an essential prerequisite to avoid complication [13].
Valgus osteotomies
Background
The most common current indication for valgus TO is subtrochanteric or neck nonunion. The latter has always been challenging for orthopedic surgeons since internal fixation was first proposed for femoral injuries in 1889, although early intervention and advancements in orthopedic technology have reduced the nonunion rate. In elderly patients, fracture nonunion is commonly treated with total joint replacement; while in younger patients without avascular necrosis, every effort should be made to preserve the native hip. A valgus TO performed with a blade plate is the most common technique used in those young patients. Correction could be obtained in the subtrochanteric region, as Schanz described, or in the trochanteric area, as proposed by Pauwels [14].
Indication and drawbacks
Pauwels’ [15] research on biomechanical forces affecting femoral neck fractures demonstrated that femoral neck nonunion was often a result of abnormal shear forces acting across the fracture site. By converting shear stresses into compressive forces, the osteotomy increases the likelihood of union and avoids a less desirable arthroplasty. Furthermore, the valgus TO partially corrects the proximal femoral deformity in nonunion of neck fracture extended to the subtrochanteric area [16].
Valgus trochanteric osteotomy has also been also used in adults for sequelae of Legg-Calvé-Perthes disease, SCFE [13], and in certain cases of osteonecrosis (flexion-valgus) [17]. In general, the goal is to move healthier articular cartilage into the weight-bearing zone of the acetabulum and to relieve impingement but the recently described techniques such as SCFE reorientation and femoral head reduction osteotomies have reduces its indications.
The major problem with valgus TO performed for neck nonunion is that the correction performed is not at the site of deformity, therefore restoring the anatomy and normalizing hip biomechanics could be achieved only indirectly. The alternative option is neck correction and fixation through a surgical dislocation; the latter directly corrects the deformity but presents with risks of avascular necrosis. This surgical option will be discussed in the next paragraph for malunited neck fracture.
At last, as described for varus TO in the previous section, THA after those realignment procedures could be challenging.
Results
Marti reviewed 50 nonunions of the femoral neck treated by valgus TO with a union rate of 94 % and a 12 % rate of conversion to THA at 7 year follow-up [18]. Weber and Cech reported the results of valgus ITO in 41 adult patients with femoral neck nonunion: 21 of 23 healed, with 61 % achieving normal function [19]. Maistrelli et al published the results of 277 valgus-extension osteotomies in adult patients. At 11–15 years of follow-up, they reported 67 % good or excellent results. Results were better when patients were younger than 40 years and if preoperative flexion was 60° or greater [7].
Historically, a valgus-extension osteotomy was indicated with superolateral arthritis in young patients but literature shows a wide range of results: long-term studies reported good to excellent results between 6 % [11] and 86 % of patients at minimum follow-up of 10 years [20].
Neck osteotomies and neck reorientation
Background
Several pathologies may lead to neck deformities (eg, fractured neck malunion and SCFE). Literature has shown that, when a neck fracture consolidates in a displaced position, the deformity creates an impingement with the acetabulum and may progress to arthritis.
SCFE may results in a deformity of the neck that is dependent upon the severity of the slip and may lead to arthritis with the same mechanism. Literature has shown that SCFE develop osteoarthritis prematurely but may last for many decades without symptoms. This is confirmed by a the long-term study of Carney, the author showed significant differences between those SCFEs that were treated in situ compared with those treated with realignment. Other studies have also shown that the greater the deformity, the earlier is the onset of osteoarthritis.
Indication and drawbacks
Surgical dislocation [21] can be used as an approach for SCFE re-orientation and for neck osteotomy. Up to date, indication for surgical dislocation and epiphyseal realignment is limited to unstable or severe SCFE, while published data does not support this treatment for stable SCFE. Femoral neck osteotomies are indicated in select cases of malunited neck fracture in very young patients.
Neck osteotomy either in SCFE or malunited neck fracture may results in femoral head AVN (see below) or leg shortening as the most significant drawbacks of this procedures. In patients previously treated with several surgical procedures, the retinaculum with blood vessels supplying the head may not be easily identified and an iatrogenic injury may lead to AVN.
Results
For SCFE
Although femoral neck osteotomies outcomes have been analyzed in several studies such as these published by Rebello [22] Spencer [23], Leunig [24], no valid and reliable statistical analyses have been carried out. Only studies by Ziebarth [25] and Masse [26] published a statistical improvement in WOMAC or HHS results together with good radiographic results. Ziebarth et al [25], Slongo et al [27], and Huber et al [28] reported 2 cases of osteonecrosis after 92 surgical dislocations for stable and unstable SCFE, which is similar to the rates of osteonecrosis published by other authors using traditional treatment [29].
For femoral neck malunion
There is only 1 case series for the FNO published in the literature. Ganz et al treated 53 patients (aged from 9 to 34) and resulted in 2 cases of AVN and 5 cases of osteotomy failure [30•].
Relative neck lengthening and greater trochanter distalization
Background
RNL and greater trochanter distalization are commonly performed for pelvic trochanteric impingement. The morphologic appearance of those hips is frequently characterized by deformed epiphysis, short femoral neck, and a greater trochanter with a tip that is higher than the center of the femoral head. The majority of patients with such morphologies have had a history of disturbance of the epiphyseal blood perfusion during conservative treatment of hip dysplasia, with early closure of the head physis and undisturbed growth of the trochanteric physis. Other etiologies, such as trauma or as a sequelae of an osteotomy, are also possible [31]. The clinical problem in the majority of such hips may be characterized by weakness of the gluteus medius muscle, but there is often also substantial pain and limitation of motion from impingement. Impingement is extra-articular between the greater trochanter and the pelvis. In addition, more severe intra-articular impingement can be associated, because of an anterior flattening of the femoral head and a prominent anterolateral bony ridge of the short femoral neck.
Indications and drawbacks
If the greater trochanter deformity is not associated with other abnormality, an extra-articular advancement of the greater trochanter may be used to treat this problem, to addresses the muscle weakness and part of the extra-articular impingement [32].
If other abnormalities are present, RNL performed through surgical dislocation should be considered to treat extra-articular and intra-articular impingements caused by a high-riding greater trochanter and/or a short femoral neck. The procedure has 2 goals: the improvement of the muscular biomechanics and the resolution of the extra- and intra-articular impingement. The operation name is “relative lengthening” because only the superior part of the neck becomes longer [33].
The morbidity of the greater trochanter distalization and relative lengthening procedures is quite small, including healing problems of the greater trochanter.
Relative neck lengthening morbidity is not higher than for surgical dislocation alone; this aspect may increase the biomechanical value of the procedure. Lateral displacement of the greater trochanter has been described as the most important component of the trochanteric transfer [34, 35]. Those authors suggested that distal displacement alone does not increase the lever arm of the abductors and distal transfer alone increases the pressure over a reduced area of the joint, possibly accelerating the development of osteoarthritis [36]. Furthermore, the intra-articular component of impingement is not addressed by this procedure, and this component is the clinically more important in the long-term [31].
Results
Published results are not easily comparable because of the different rage of indications between authors. For example, a wide range [31] of improvement in hip abductors’ insufficiency has been reported in the literature. This wide range is probably attributable to the variability of indications for surgery and to the etiology of deformity.
Several studies evaluated the improvement of hip function but did not use a validated tool and only few studies have shown improvement of hip function in the majority of patients treated greater trochanter distalization, either based on a validated hip score or only from gait improvement. According to Sun Young Joo [37], trochanteric advancement alone does little to relieve pain and improve limping in patients with relative overgrowth of the greater trochanter and Legg-Calvé-Perthes (LCPD) disease underlying the importance of intra-articular deformity treatment.
Lesser trochanter distalization or excision
Background
Lesser trochanter distalization or excision is commonly performed for ischiofemoral impingement (IFI); this is defined as a contact between the ischium and the lesser trochanter. Ischiofemoral impingement is not common and is often related to trauma or prior hip surgery (eg, as a result of fractures of the proximal femur or in patients with intertrochanteric osteotomy) [38–40]. Both congenital and acquired impingements have been reported in cases without a history of prior surgery [38, 41, 42].
Ischiofemoral impingement is characterized by a narrowed space between the ischial tuberosity and the lesser trochanter, with intermittent compression of the quadratus femoris muscle between the ischium and the lesser trochanter, and associated edema or fatty replacement of the quadratus femoris muscle [38, 40].
Ischiofemoral impingement is related to sex, being more common in women and bilateral in up to one-third of patients [38, 40]. The predominance of ischiofemoral impingement might be due to the shape of the female pelvis [38, 40].
The diagnosis is mainly done through an MRI, because there are no specific tests for ischiofemoral impingement, and it is often confused with intra-articular hip pain [40].
In patients with ischiofemoral impingement, the distance between the ischial tuberosity and the lesser trochanter (also known as the ischiofemoral distance) is reduced, with mean (±SD) measurements of 13 ± 5 mm in patients vs 23 ± 8 mm in control subjects [38]. Some caution is advised when measuring this distance in daily practice, because the measurements are dependent on the degree of internal or external rotation of the hip during image acquisition. So far, to our knowledge, no prospective study exists on ischiofemoral impingement; therefore, inconsistencies in patient positioning cannot be excluded in the reported studies [38, 40].
Indications and drawbacks
Although most reports recommend conservative treatment or CT-guided injection of steroids [38, 39, 43], some authors suggest surgical resection or distalization of the lesser trochanter. Resection could be arthroscopically performed after psoas tendon detachment as described by Safran [44•], while open distalization may be performed associated with other osteotomies through a surgical dislocation (Fig. 1) [43]. The preferred treatment of IFI is still debated in the orthopedic community. While the 2 cases of IFI following total hip arthroplasty were successfully treated with open excision of the lesser trochanter, definitive treatment has yet to be determined, especially for the nonarthritic hip without previous surgery.
Fig. 1.
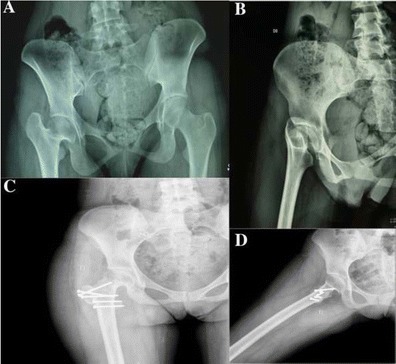
A 22-year-old woman presenting a pelvitrochanteric and an ischiofemoral impingement (a and b), treated with relative neck lengthening and lesser trochanter distalization (c and d)
Results
Published results of those techniques are promising but only few cases have been described, therefore, the actual evidence is not sufficient to support a routine use of those procedures outside selected centers.
Head reduction osteotomies
Background
Head reduction osteotomies are commonly performed for Legg-Calvé-Perthes disease. Etiology of LCPD is an idiopathic osteonecrosis of the femoral epiphysis probably because of its tenuous blood supply. This process created an asphericity of the femoral head and this causes hip pain and dysfunction either in childhood either in adulthood. Stulberg et al [45] and McElwain et al [46] demonstrated a clear correlation between femoral head sphericity and radiographic and long-term functional outcome.
A recent meta-analysis [47] suggested that children older than 8 years would be the best candidate for surgery. The Level IIa and IIIa studies revealed patients undergoing surgery during or before the fragmentation phase have better femoral head sphericity at the end stage of LCPD than those undergoing nonoperative treatment.
Several treatments were proposed for LCPD but their effects on the natural history of the disease are unclear and the best treatment of LCPD remains unknown.
Recently femoral head reduction osteotomy has been proposed to treat those deformities. The rationale of this procedure is to address the disease directly on the site of deformity. A peri-acetabular osteotomy may be added when the acetabulum is dysplastic.
Indication and drawbacks
Femoral head reduction osteotomy has a rare but distinct indication in older children and adolescents. It is a direct approach to morphology of the femoral head and it does not have a true alternative option. Femoral head osteotomy is always combined with relative lengthening of the neck. However, it may be performed without an additional joint-stabilizing procedure if secondary deformation of the acetabulum is absent or only minimal.
Finally, an excessive resection of the femoral head can cause hip instability and subluxation and may lead to an early osteoarthritis. The remaining subluxation tendency may be limited with a varus intertrochanteric osteotomy and a reorientation of the acetabulum at a later stage.
Results
Unfortunately there is only 1 case series of femoral head reduction osteotomies reported [33]. The authors described the procedures for 13 patients Perthes or Perthes-like deformities. Patients’ ages ranged between 9 and 21 years. Eight hips had a peri-acetabular osteotomy, together with the reduction osteotomy. All osteotomies healed within 6 to 8 weeks, and none developed osteonecrosis at a minimum follow-up of 3 years. All patients reported improved motion, without substantial pain.
With the longest follow-up at 9 years, intra-capital osteotomy has promising radiographic and clinical results and seems to be a good choice in selected cases but further study, in hands other than the technique describers, will be necessary to confirm this statement.
Conclusions
Although the use of femoral osteotomies is decreased due to the effectiveness of THA, they may still play a role in young patients with major deformities of the proximal femur before cartilage lesions are developed. Classic osteotomies, such as valgus and varus correction, should be considered when patients meet the limited indications.
Select cases may benefit from new techniques, such as femoral neck osteotomy, femoral head reorientation, relative neck lengthening (RNL), greater or lesser trochanter distalization and femoral head reduction osteotomy (FHRO).
The last 3 groups of procedures, however, are routinely performed only by surgeons with extensive clinical experience and may not offer the same rates of success if adopted in a widespread fashion.
Compliance with Ethics Guidelines
Conflict of Interest
Alessandro Aprato, Pietro Pellegrino, Michael S.H. Kain, and Alessandro Masse declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Turgeon TR, Phillips W, Kantor SR, Santore RF. The role of acetabular and femoral osteotomies in reconstructive surgery of the hip: 2005 and beyond. Clin Orthop. 2005;441:188–199. doi: 10.1097/01.blo.0000193541.72443.73. [DOI] [PubMed] [Google Scholar]
- 2.Turchetto L, Massè A, Aprato A, Barbuio A, Ganz R, Turchetto L, et al. Developmental dysplasia of hip: joint preserving surgeon in the adolescent and young adult. Minerva Ortopedica e Traumatol. 2013;64:41–52. [Google Scholar]
- 3.Mubarak SJ, Valencia FG, Wenger DR. One-stage correction of the spastic dislocated hip. Use of pericapsular acetabuloplasty to improve coverage. J Bone Joint Surg Am. 1992;74:1347–1357. [PubMed] [Google Scholar]
- 4.Pogliacomi F, De Filippo M, Costantino C, Wallensten R, Soncini G. 2006: the value of pelvic and femoral osteotomies in hip surgery. Acta Bio-Med Atenei Parm. 2007;78:60–70. [PubMed] [Google Scholar]
- 5.Millis MB, Murphy SB, Poss R. Osteotomies about the hip for the prevention and treatment of osteoarthrosis. Instr Course Lect. 1996;45:209–226. [PubMed] [Google Scholar]
- 6.Ferguson GM, Cabanela ME, Ilstrup DM. Total hip arthroplasty after failed intertrochanteric osteotomy. J Bone Joint Surg (Br) 1994;76:252–257. [PubMed] [Google Scholar]
- 7.Maistrelli GL, Gerundini M, Fusco U, Bombelli R, Bombelli M, Avai A. Valgus-extension osteotomy for osteoarthritis of the hip. Indications and long-term results. J Bone Joint Surg (Br) 1990;72:653–657. doi: 10.1302/0301-620X.72B4.2380222. [DOI] [PubMed] [Google Scholar]
- 8.Santore R, Bombelli M. Long-term follow-up of the Bombelli experience with osteotomy for osteoarthritis: results at 11 years. In Hungerford DS, editor. The Hip: Proceedings of the Eleventh Open Scientific Meeting of the Hip Society, St. Louis: Mosby; 1983. p. 106–28. [PubMed]
- 9.•.Louahem M’sabah D, Assi C, Cottalorda J. Proximal femoral osteotomies in children. Orthop Traumatol Surg Res. 2013;99:S171–S186. doi: 10.1016/j.otsr.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 10.Morscher E. Intertrochanteric osteotomy in osteoarthritis of the hip. In: Riley L, editor. The hip: proceedings of the Eighth Open Scientific Meeting of the Hip Society. St. Louis: Mosby; 1980. p. 24–46.
- 11.Iwase T, Hasegawa Y, Kawamoto K, Iwasada S, Yamada K, Iwata H. Twenty years’ follow-up of intertrochanteric osteotomy for treatment of the dysplastic hip. Clin Orthop. 1996;331:245–255. doi: 10.1097/00003086-199610000-00035. [DOI] [PubMed] [Google Scholar]
- 12.Dorr LD, Takei GK, Conaty JP. Total hip arthroplasties in patients less than forty-five years old. J Bone Joint Surg Am. 1983;65:474–479. [PubMed] [Google Scholar]
- 13.Santore RF, Kantor SR. Intertrochanteric femoral osteotomies for developmental and posttraumatic conditions. J Bone Jt Surg. 2004;86:2542–2553. [PubMed] [Google Scholar]
- 14.Schoenfeld AJ, Vrabec GA. Valgus osteotomy of the proximal femur with sliding hip screw for the treatment of femoral neck nonunions: the technique, a case series, and literature review. J Orthop Trauma. 2006;20:485–491. doi: 10.1097/00005131-200608000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Pauwels F. Biomechanics of the normal and diseased hip: theoretical foundation, technique and results of treatment: an atlas. New York: Springer; 1976. Osteoarthritis; pp. 129–271. [Google Scholar]
- 16.Blount WP. Proximal osteotomies of the femur. Instr Course Lect. Sept 1, 1952.
- 17.Santore RF. Intertrochanteric osteotomy for osteonecrosis. Semin Arthroplast. 1991;2:208–213. [PubMed] [Google Scholar]
- 18.Marti RK, Schüller HM, Raaymakers EL. Intertrochanteric osteotomy for non-union of the femoral neck. J Bone Joint Surg (Br) 1989;71:782–787. doi: 10.1302/0301-620X.71B5.2584247. [DOI] [PubMed] [Google Scholar]
- 19.Weber B, Cech O. Pseudoarthrosis. Bern: Hans Huber; 1976.
- 20.Boos N, Krushell R, Ganz R, Müller ME. Total hip arthroplasty after previous proximal femoral osteotomy. J Bone Joint Surg (Br) 1997;79:247–253. doi: 10.1302/0301-620X.79B2.6982. [DOI] [PubMed] [Google Scholar]
- 21.Ganz R, Gill TJ, Gautier E, Ganz K, Krügel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg (Br) 2001;83:1119–1124. doi: 10.1302/0301-620X.83B8.11964. [DOI] [PubMed] [Google Scholar]
- 22.Rebello G, Spencer S, Millis MB, Kim Y-J. Surgical dislocation in the management of pediatric and adolescent hip deformity. Clin Orthop. 2009;467:724–731. doi: 10.1007/s11999-008-0591-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Spencer S, Millis MB, Kim Y-J. Early results of treatment of hip impingement syndrome in slipped capital femoral epiphysis and pistol grip deformity of the femoral head-neck junction using the surgical dislocation technique. J Pediatr Orthop. 2006;26:281–285. doi: 10.1097/01.bpo.0000217726.16417.74. [DOI] [PubMed] [Google Scholar]
- 24.Leunig M, Slongo T, Kleinschmidt M, Ganz R. Subcapital correction osteotomy in slipped capital femoral epiphysis by means of surgical hip dislocation. Oper Orthop Traumatol. 2007;19:389–410. doi: 10.1007/s00064-007-1213-7. [DOI] [PubMed] [Google Scholar]
- 25.Ziebarth K, Zilkens C, Spencer S, Leunig M, Ganz R, Kim Y-J. Capital realignment for moderate and severe SCFE using a modified Dunn procedure. Clin Orthop. 2009;467:704–716. doi: 10.1007/s11999-008-0687-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Massè A, Aprato A, Grappiolo G, Turchetto L, Campacci A, Ganz R. Surgical hip dislocation for anatomic reorientation of slipped capital femoral epiphysis: preliminary results. Hip Int J Clin Exp Res Hip Pathol Ther. 2012;22:137–144. doi: 10.5301/HIP.2012.9208. [DOI] [PubMed] [Google Scholar]
- 27.Slongo T, Kakaty D, Krause F, Ziebarth K. Treatment of slipped capital femoral epiphysis with a modified Dunn procedure. J Bone Joint Surg Am. 2010;92:2898–2908. doi: 10.2106/JBJS.I.01385. [DOI] [PubMed] [Google Scholar]
- 28.Huber H, Dora C, Ramseier LE, Buck F, Dierauer S. Adolescent slipped capital femoral epiphysis treated by a modified Dunn osteotomy with surgical hip dislocation. J Bone Joint Surg (Br) 2011;93:833–838. doi: 10.1302/0301-620X.93B6.25849. [DOI] [PubMed] [Google Scholar]
- 29.Loder RT, Richards BS, Shapiro PS, Reznick LR, Aronson DD. Acute slipped capital femoral epiphysis: the importance of physeal stability. J Bone Joint Surg Am. 1993;75:1134–1140. doi: 10.2106/00004623-199308000-00002. [DOI] [PubMed] [Google Scholar]
- 30.•.Ganz R, Horowitz K, Leunig M. Algorithm for femoral and periacetabular osteotomies in complex hip deformities. Clin Orthop Relat Res. 2010;468:3168–3180. doi: 10.1007/s11999-010-1489-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Garcia FL, Picado CHF, Cardinali LP. Does trochanteric transfer eliminate the Trendelenburg sign in adults? Clin Orthop Relat Res. 2011;469:1984–1990. doi: 10.1007/s11999-010-1676-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kelikian AS, Tachdjian MO, Askew MJ, Jasty M. Greater trochanteric advancement of the proximal femur: a clinical and biomechanical study. Hip. 1983;77–105. [PubMed]
- 33.Leunig M, Ganz R. Relative neck lengthening and intracapital osteotomy for severe Perthes and Perthes-like deformities. Bull NYU Hosp Jt Dis. 2011;69(Suppl 1):S62–S67. [PubMed] [Google Scholar]
- 34.Takata K, Maniwa S, Ochi M. Surgical treatment of high-standing greater trochanter. Arch Orthop Trauma Surg. 1999;119:461–463. doi: 10.1007/s004020050021. [DOI] [PubMed] [Google Scholar]
- 35.Maquet PGJ. Biomechanics of the hip: as applied to Osteoarthritis and related conditions. New York: Springer; 1985. Lateral displacement of the greater trochanter; pp. 134–149. [Google Scholar]
- 36.Wagner H. Transplantation of the greater trochanter. In: Weil UH, editor. Acetabular dysplasia: skeletal dysplasias in childhood. Berlin: Springer; 1978. pp. 99–102. [Google Scholar]
- 37.Joo SY, Lee KS, Koh IH, Park HW, Kim HW. Trochanteric advancement in patients with Legg-Calvé-Perthes disease does not improve pain or limp. Clin Orthop. 2008;466:927–934. doi: 10.1007/s11999-008-0128-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Torriani M, Souto SCL, Thomas BJ, Ouellette H, Bredella MA. Ischiofemoral impingement syndrome: an entity with hip pain and abnormalities of the quadratus femoris muscle. Am J Roentgenol. 2009;193:186–190. doi: 10.2214/AJR.08.2090. [DOI] [PubMed] [Google Scholar]
- 39.Johnson KA. Impingement of the lesser trochanter on the ischial ramus after total hip arthroplasty. Report of three cases. J Bone Joint Surg Am. 1977;59:268–269. [PubMed] [Google Scholar]
- 40.Tosun O, Algin O, Yalcin N, Cay N, Ocakoglu G, Karaoglanoglu M. Ischiofemoral impingement: evaluation with new MRI parameters and assessment of their reliability. Skelet Radiol. 2012;41:575–587. doi: 10.1007/s00256-011-1257-5. [DOI] [PubMed] [Google Scholar]
- 41.Patti JW, Ouellette H, Bredella MA, Torriani M. Impingement of lesser trochanter on ischium as a potential cause for hip pain. Skelet Radiol. 2008;37:939–941. doi: 10.1007/s00256-008-0551-3. [DOI] [PubMed] [Google Scholar]
- 42.Stafford GH, Villar RN. Ischiofemoral impingement. J Bone Joint Surg (Br) 2011;93:1300–1302. doi: 10.1302/0301-620X.93B10.26714. [DOI] [PubMed] [Google Scholar]
- 43.Ali AM, Whitwell D, Ostlere SJ. Case report: imaging and surgical treatment of a snapping hip due to ischiofemoral impingement. Skelet Radiol. 2011;40:653–656. doi: 10.1007/s00256-010-1085-z. [DOI] [PubMed] [Google Scholar]
- 44.•.Safran M, Ryu J. Ischiofemoral impingement of the hip: a novel approach to treatment. Knee Surg Sports Traumatol Arthrosc. 2014;22:781–785. doi: 10.1007/s00167-013-2801-8. [DOI] [PubMed] [Google Scholar]
- 45.Stulberg SD, Cooperman DR, Wallensten R. The natural history of Legg-Calvé-Perthes disease. J Bone Joint Surg Am. 1981;63:1095–1108. [PubMed] [Google Scholar]
- 46.McElwain JP, Regan BF, Dowling F, Fogarty E. Derotation varus osteotomy in Perthes disease. J Pediatr Orthop. 1985;5:195–198. doi: 10.1097/01241398-198505020-00013. [DOI] [PubMed] [Google Scholar]
- 47.Saran N, Varghese R, Mulpuri K. Do femoral or salter innominate osteotomies improve femoral head sphericity in Legg-Calvé-Perthes disease? A meta-analysis. Clin Orthop Relat Res. 2012;470:2383–2393. doi: 10.1007/s11999-012-2326-3. [DOI] [PMC free article] [PubMed] [Google Scholar]


