Abstract
Bernese periacetabular osteotomy has become a secure and reproducible technique for treatment of hip dysplasia. It allows an adequate reorientation of the acetabulum and coverage of the femoral head improving biomechanical conditions of the hip joint. We present a review of literature and a modification of original technique that includes a smaller incision and preservation of the abductor muscles and rectus femoris tendon insertion.
Keywords: Hip dysplasia, Periacetabular osteotomy, Bernese periacetabular osteotomy
Introduction
Hip dysplasia is an alteration in normal development of constitutive elements of the hip. The natural history of the disease starts with acetabular dysplasia and progressively decreased femoral coverage and femoral anteversion, joint damage, labrum alterations, and secondary deformities with possible consequent dislocation and osteoarthritis. It has been estimated a frequency of 3 % of the population, with a ratio female/male = 7/1 approximately [1–3].
The etiology of hip dysplasia is multifactorial, including genetic (20 % with family history) and environmental factors, mechanical alterations mainly related to intrauterine primiparous dystocic presentation, multiple pregnancy, and macrosomia.
Patients with hip dysplasia show anatomic alterations of the acetabulum, proximal femur, and articular structures. These alterations produce unfavorable mechanical conditions with increased stress in the articular surface, ultimately leading to secondary osteoarthritis. In 1988, Reinhold Ganz, described a periacetabular osteotomy technique for management of patients with acetabular dysplasia and closure of triradiate cartilage called Bernese periacetabular osteotomy (PAO). With this technique, the reorientation of the acetabulum provides an adequate coverage of the femoral head, improving the biomechanical conditions of the joint without the risk of femoral head avascular necrosis [3–5] (Figs. 1, 2). The original technique was described with a modified Smith-Peterson approach and included partial detachment of the tensor fasciae latae from the ilium to the tubercle of the gluteus medius as well as the detachment of the rectus femoris muscle tendon in its direct and reflex portions.
Fig. 1–2.
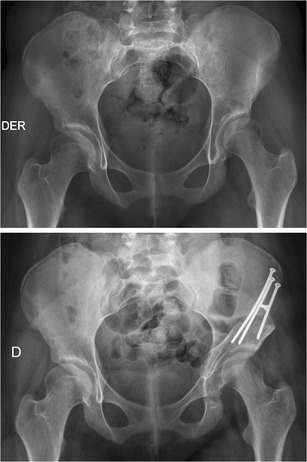
AP pelvis X-Ray pre- and postoperatory of a patient with hip dysplasia treated with Bernese periacetabular osteotomy
Different studies have been published over the years regarding the surgical technique, learning curve, results as well as intra- and postoperative complications [3, 6–12]. The 20-year survival rate of this technique is of 65 %, with 85 % of good and excellent results [9, 10•, 13, 14]. Prognostic factors such as age, degree of osteoarthritis, and articular congruence have been identified [10•, 15]. In terms of learning curve, a decreased rate of complications (from 20 % to 3 %) has been described after the first 50 surgeries [10•, 16–20]. These complications include overcorrection, lateralization of the hip, damage to the posterior pillar, dysesthesia in the lateral femoral cutaneous nerve distribution in 30 % of the cases [18–20], neurologic injury in less than 2 %–3 % [19], heterotopic ossification in 5 % [16], and nonunion [21•, 22].
The authors developed a modified technique, through a shorter anterior approach, with less damage to the soft tissues, no detachment of the tensor fasciae latae and the rectus femoris muscle in its direct and reflex portions. The technique was developed with the goal of reducing postoperative pain and recovery time, as well as increasing patient’s functional ability.
Surgical indications
PAO is indicated in patients with hip dysplasia, with mobility ranges in flexion >100°, internal rotation >20°, external rotation >20°, and abduction >30° and assessment of X-ray images with Wiberg angle <25°, anterior center-edge angle <25°, acetabular index >10°, percentage of femoral head coverage <80 %, Tönnis 0–1, and an adequate articular congruence. The radiographic study includes AP pelvis X-ray, false profile view, and AP pelvis with maximal abduction and internal rotation.
Surgical technique
With the patient in supine position over a radiolucent table, surgical field is prepared including the whole lower limb to allow movement during surgery. An adequate visualization of the pelvis should be verified under fluoroscope in anteroposterior and alar views.
The iliac crest and anterosuperior iliac spine (ASIS) are identified and marked. A shortened incision is done, starting from the ASIS and extending 8 cm distal following the lower limb longitudinal axis. To expose structures proximal to ASIS, it is possible to apply the mobile-window concept, in which free mobilization of the skin and subcutaneous tissue over the iliac crest allows a complete and adequate visualization. The fascia over the tensor fasciae latae muscle is split, protecting the femoral cutaneous nerve and displacing it medially along with the sartorius muscle (Fig. 3). The tensor fasciae latae is retracted laterally to expose the rectus femoris muscle, tendon, and psoas muscle.
Fig. 3.
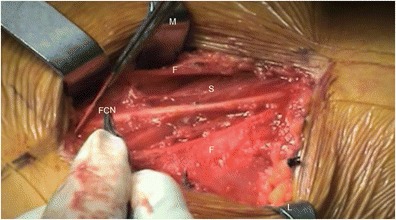
Surgical approach: fascia (F), sartorius muscle (S), and femoral cutaneous nerve (FCN). L lateral retractor, M medial retractor
Using the mobile-window concept, the subcutaneous tissue and skin are displaced proximally, exposing the ASIS and insertion of the sartorius muscle. An osteotomy of 1.5 × 2 cm is performed on the ASIS with an oscillating saw and straight osteotome, in order to move the insertion of the sartorius muscle medially and expose the region between the ASIS and anterior inferior iliac spine (AIIS). The interval between the rectus femoris muscle and the psoas is then dissected, retracting the rectus femoris muscle laterally in its direct and reflex portion and retracting the psoas muscle medially. Iliocapsularis muscle is retracted medially, exposing the articular capsule, by retracting the iliocapsularis muscles and the psoas, the ascending branch of the rectus femoris muscle and of the lateral femoral circumflex artery are protected. From now on the surgery is as described in the original technique; the bone structures are identified and the corresponding osteotomies performed. First, once the medial and inferior region of the extracapsular femoral neck is identified, the curved osteotome is located over the ischium just below the acetabulum and the osteotomy is performed under fluoroscopic AP view. This osteotomy is an incomplete cut, preserving intact the posterior column (Fig. 4). The following is a complete osteotomy of the superior pubic ramus, taking care not to damage the posterior structures and medial psoas muscle with the osteotome (Fig. 5). The third osteotomy is the iliac wing osteotomy, performed in the top of the acetabular area with an oscillating saw. It is very important not to exceed the medial border of posterior pillar (±1–2 cm), with the aim to maintain the integrity of pelvic ring (Fig. 6). The final osteotomy is performed under radioscopic joining previous osteotomies and preserving the posterior pillar (Figs. 7, 8).
Fig. 4.

First osteotomy in a radioscopic intra-operatory view
Fig. 5.
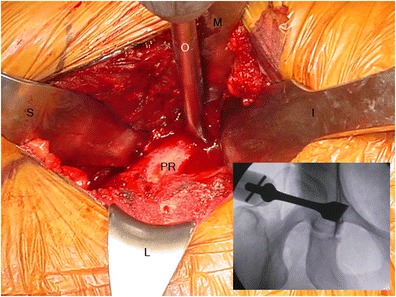
Second osteotomy. Direct vision and the corresponding fluoroscopic vision with the osteotome in the right position. I inferior retractor, L lateral retractor, M medial retractor, O osteotome, PR superior pubic ramus, S superior retractor
Fig. 6.

Third osteotomy in a radioscopic intra-operatory view
Fig. 7.

Fourth osteotomy in a radioscopic intra-operatory view
Fig. 8.

Periacetabular osteotomy in a radioscopic intra-operatory view
With placement of acetabular Schanz pins, the acetabulum is mobilized and the anterolateral coverage of the femoral head, together with the acetabular index, are corrected. The osteotomy is temporarily fixed with Kirschner wires, before intra-operative radiographic control. If this is satisfactory, definitive fixation is performed using 3 long 3.5-mm cortical screws using a transverse fixation [23]. Finally, reduction and osteosynthesis of the ASIS is performed with 1 short 3.5-mm cortical screw. The closing is done in layers and protecting the lateral femoral cutaneous nerve [3, 9, 13, 14].
Our experience
We started performing PAO in 1996. In the beginning, we performed a long Smith Petersen surgical approach as described by Dr. Ganz. During the next years, with more than 300 PAOs done, we developed a modification of the PAO original surgical technique with a shorter anterior approach. This technique was presented on the American Academy Annual Meeting 2011(see appendix). At present, other publications use this technique [24, 25]. In the original technique the direct head of the rectus femoris was detached from the anterior inferior iliac spine (AIIS) and a protected rehabilitation was needed of at least 6 weeks to allow for rectus femoris healing. The modification included preservation of the rectus femoris direct head tendon, not releasing it, but retracting it laterally and preserving the abductor insertion at the lateral iliac wing. The rehabilitation protocol is much faster with this modification, since no restriction of the quadriceps is needed. A cadaveric study was done in the Anatomy Laboratory. Dissection of the anatomic pieces was performed through an anterior approach to the hip. Insertion of the tensor fasciae latae was respected as well as rectus femoris tendon in its direct and reflex portions. By dissecting the intramuscular plane between rectus femoris and psoas, an adequate exposure of joint capsule and iliocapsularis muscle was achieved, causing no interference in the partial osteotomy of the ischium when it is medially displaced and presenting no risk of neurovascular injury, specially the ascending motor branch of the rectus femoris muscle and the lateral femoral circumflex artery are protected by retracting medially the iliocapsularis and psoas muscles.
Fifty-one patients (48 hips) with dysplasia sequelae underwent surgery with the modified technique. With a follow-up of 39.35 months (12–76) on average, 48 hips (92.15 %) were operated in female patients. The mean age was 23.24 (12–48). The length of the anterior incision was on average 8.52 cm (6–13 cm). The hospitalization time was 4.1 days (3–7 days) on average. Preoperative modified Harris Hip Score (HHS) was on average 84.36 (79–96) and postoperative was 96.72 (91–100). There was an HHS improvement of 12.36 points on average during the complete follow-up period, with good and excellent results in all patients treated. Imaging studies presented a normalization of radiological parameters. Preoperative X-Ray and postoperative images at 3 and 6 months and after each year were evaluated. Radiological parameters were measured in all images considering the radiological consolidation of osteotomies. An average improvement of Wiberg angle from 15.3 (8–24) degrees preoperatively to 31.2 (24–35) degrees postoperatively was described. Acetabular index improved from 26.2 (18–41) degrees preoperative to 9.8 (3–13) degrees postoperative on average. Percentage of femoral head coverage improved from 62.4 % (50–73) to 77.6 % (70–87) postoperative on average.
A shorter incision is preferred by patients specially women. Aside from this, any type of approach could cause early and late problems with skin healing, like dehiscence and wider, displeasing scars. In the attempt to improve this, in 2013 we introduced a new modification of skin incision, following skin tension lines. An oblique inguinal incision is performed between the inguinal crease and a projected line from the ASIS to the pubis, as shown in Figure 9. An aesthetical scar was obtained, along with better satisfaction results from patients.
Fig. 9.
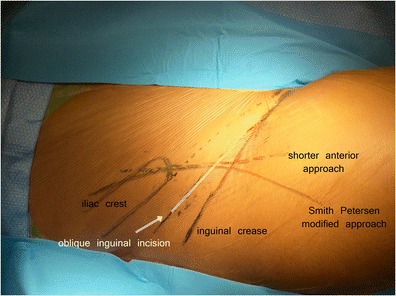
Surgical incisions drawings in a patient for PAO
Postoperative and rehabilitation
Preservation of muscles insertions and lesser damage to soft tissues allow patients to start an active rehabilitation process from the first postoperative day, by preserving their walking strength, decreasing the claudication period, and allowing them to begin their normal activities sooner.
Rehabilitation starts in the same day with active hip mobilization exercises. Quadriceps, glutei, and hamstring muscles exercises are begun immediately. In our series, rehabilitation process started with active movements from first postoperative day in 92 % of the patients. Only 1 patient started physical rehabilitation on the 4th day—because of a manifestation of symptomatic anemia in his postoperative—and required a transfusion of filtered red blood cells. Support with a walker and partial load started on the second and third postoperative day. Eighty-nine percent of patients started using a cane between the third and fourth day postoperative. The average hospitalization time was of 4.1 days (3–7 days). Eighty-one percent of the patients started their rehabilitation on the first postoperative day with active muscle exercises and walking with partial weight bearing using support from the second postoperative day. Eighty-seven percent of the patients walked within the third postoperative day. Patients walked with protected weight bearing with 2 crutches the first 6 weeks and then with 1 crutch the following 4 weeks.
Complications and follow-up
Complications reported in our experience do not differ from what has been reported in literature. Ten patients (19.6 %) had temporary dysesthesia of the femoral cutaneous nerve area, 2 patients (3.92 %) showed suture dehiscence, and 2 patients needed hardware removal. In this series, there was no evidence of infection, vascular injury, sciatic nerve injury, or femoral nerve injury. There was no evidence of heterotopic ossification.
Summary
The surgical technique of anterior approach modified from the Bernese periacetabular osteotomy is a secure and reproducible technique that allows an adequate reorientation of the acetabulum, improving the coverage of the femoral head in patients with hip dysplasia. The modified incision presents a better-looking and is smaller with less aggressiveness on soft tissues. Moreover, we preserve abductor muscles and no detachment of rectus femoris tendon. The modified technique allows an early and active rehabilitation starting the first postoperative day. It decreases the length of physiotherapy and speeds up the reintegration to the daily activities of young patients with hip dysplasia.
Compliance with Ethics Guidelines
Conflict of Interest
Javier Besomi and Carlos Tobar declare that they have no conflict of interest. Joaquín Lara is a consultant for Stryker.
Human and Animal Rights and Informed Consent
Human studies done by authors (but no animal studies). This article does not contain any studies with animal subjects performed by any of the authors. With regard to the authors’ research cited in this paper, all procedures were followed in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 2000 and 2008.
Appendix
A multimedia video detailing this modified technique is available on web site at aaos.org (http://www3.aaos.org/product/productpage.cfm?code=V11001).
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Weinstein SL. Natural history of congenital hip dislocation (CDH) and hip dysplasia. Clin Orthop Relat Res. 1987;225:62–8. [PubMed] [Google Scholar]
- 2.Fujii M, Nakashima Y, et al. Intraarticular findings in symptomatic developmental dysplasia of the hip. J Pediatr Orthop. 2009;29:9–13. doi: 10.1097/BPO.0b013e318190a0be. [DOI] [PubMed] [Google Scholar]
- 3.Ganz R, Klaue K, Vinh T, Mast J. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop. 1988;232:26–36. [PubMed] [Google Scholar]
- 4.Beck M, Leuning M, Ellis T, Sledge JB, Ganz R. The acetabular blood supply: implications for periacetabular osteotomies. Sur Anat. 2003;25:361–7. doi: 10.1007/s00276-003-0149-3. [DOI] [PubMed] [Google Scholar]
- 5.Gautier E, Ganz K. Anatomy of the medial circumflex artery and its surgical implications. J Bone Joint Surg Br. 2000;82(5):679–83. [DOI] [PubMed]
- 6.Troelsen A, Elmengaard B, Soballe K. A new minimally invasive transsartorial approach for periacetabular osteotomy. J Bone Joint Surg. 2008;90:493–8. doi: 10.2106/JBJS.F.01399. [DOI] [PubMed] [Google Scholar]
- 7.López-Durán L, Zarzoso R, Cardoso Z, Molina M, Junyent E, Ibarzabal A, et al. Osteotomía periacetabular tipo Ganz en la displasia de cadera del adulto. Rev Ortop Traumatol. 2002;46(Suppl 1):38–45. [Google Scholar]
- 8.Matheney T, Kim Y-J, Zurakowski D, Matero C, Millis M. Intermediate to long-term results following the bernese periacetabular osteotomy and predictors of clinical outcome. J Bone Joint Surg Am. 2009;91:2113–23. doi: 10.2106/JBJS.G.00143. [DOI] [PubMed] [Google Scholar]
- 9.Clohisy JC, Barrett SE, Gordon JE, Delgado ED, Schoenecker PL. Periacetabular osteotomy for the treatment of severe acetabular dysplasia. J Bone Joint Surg Am. 2005;87:254–9. doi: 10.2106/JBJS.D.02093. [DOI] [PubMed] [Google Scholar]
- 10.•.Steppacher S, Tannast M, Ganz R, Siebenrock A. Mean 20-year follow-up of Bernese periacetabular osteotomy. Clin Orthop Relat Res. 2008;466:1633–44. doi: 10.1007/s11999-008-0242-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kralj M, Mavcic B, Antolic V, Iglic A. The Bernese periacetabular osteotomy: clinical, radiographic and mechanical 7–15 year follow-up of 26 hips. Acta Orthop. 2005;76:833–40. doi: 10.1080/17453670510045453. [DOI] [PubMed] [Google Scholar]
- 12.Siebenrock KA, Scholl E. Bernese periacetabular osteotomy. Clin Orthop Relat Res. 1999;363:9–20. [PubMed]
- 13.Clohisy JC, Barrett SE, Gordon JE, Delgado ED, Schoenecker PL. Periacetabular osteotomy in the treatment of severe acetabular dysplasia. Surgical technique. J Bone Joint Surg Am. 2006;88(Suppl 1):65–83. doi: 10.2106/JBJS.E.00887. [DOI] [PubMed] [Google Scholar]
- 14.Siebenrock KA, Leuning M, Ganz R. Periacetabular osteotomy: the Bernese experience. Inst Course Lect. 2001;50:239–45. [PubMed] [Google Scholar]
- 15.Badra MI, Anand A, Straight JJ, Sala DA. Functional outcome in adult patients following Bernese periacetabular osteotomy. Orthopedics. 2008;31:69. doi: 10.3928/01477447-20080101-03. [DOI] [PubMed] [Google Scholar]
- 16.Crockarell J, Trousdale R, Cabanela M, Berry D. Early experience and results with the periacetabular osteotomy. Clin Orthop Relat Res. 1999;363:45–63. doi: 10.1097/00003086-199906000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Peters CL, Erickson JA, Hines JL. Early results of the Bernese periacetabular osteotomy: the learning curve at an academic medical center. J Bone Joint Surg Am. 2006;88:1920–6. doi: 10.2106/JBJS.E.00515. [DOI] [PubMed] [Google Scholar]
- 18.Hussel JG, Mast JW, Mayo KA, Howie DW, Ganz R. A comparison of different surgical approaches for the periacetabular osteotomy. Clin Orthop Relat Res. 1999;636:64–72. [PubMed] [Google Scholar]
- 19.Davey JP, Santore RF. Complications of periacetabular osteotomy. Clin Orthop Relat Res. 1999;363:33–7. doi: 10.1097/00003086-199906000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Hussell J, Rodríguez J, Ganz R. Technical complications of the Bernese periacetabular osteotomy. Clin Orthop. 1999;363:81–92. [PubMed] [Google Scholar]
- 21.•.Clohisy JC, Schutz AL, St John L, Schoenecker PL, Wright RW. Periacetabular osteotomy: a systematic literature review. Clin Orthop Relat Res. 2009;467:2041–52. doi: 10.1007/s11999-009-0842-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tibor LM, Sink EL. Periacetabular osteotomy for hip preservation. Orthop Clin North Am. 2012;43:343–57. doi: 10.1016/j.ocl.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 23.Babis GC, Trousdale RT, Jenkyn TR, Kaufman K. Comparison of two methods of screw fixation in periacetabular osteotomy. Clin Orthop Relat Res. 2002;403:221–7. doi: 10.1097/00003086-200210000-00032. [DOI] [PubMed] [Google Scholar]
- 24.Peters CL, Erickson JA, Anderson MB, Anderson LA. Preservation of the rectus femoris origin during periacetabular osteotomy does not compromise acetabular reorientation. Clin Orthop Relat Res. 2014. doi:10.1007/s11999-014-3837-x. [DOI] [PMC free article] [PubMed]
- 25.Novais EN, Kim YJ, Carry PM, Millis MB. The Bernese periacetabular osteotomy: is transaction of the rectus femoris tendon essential?. Clin Orthop Relat Res. 2014;472(10):3142–9. [DOI] [PMC free article] [PubMed]


