Abstract
Osteotomies around the knee are well-recognized treatments for unloading the affected compartment in cases of lower limb malalignment. There are few papers in the literature describing the outcomes of distal femoral osteotomy (DFO), as compared with the studies reporting on high tibial osteotomy (HTO), probably because valgus malalignment is less common than the varus one. There is still debate as to what the correct indication is and which surgical techniques lead to the best outcomes in performing a DFO. Besides, it is still controversial whether patellofemoral arthritis should be considered as a contraindication to performing a DFO, as well as in HTO. In this article, we will summarize the indications for DFO, the surgical techniques reported in the literature, and their outcomes.
Keywords: Knee deformity, Malalignment, Valgus knee, Distal femoral osteotomy
Introduction
Osteotomies around the knee to unload the affected compartment and to allow correction of the underlying deformity are well-recognized treatments for symptomatic unicompartmental gonarthrosis in young and active patients [1••]. In the literature, there are many papers describing good results for high tibial osteotomy (HTO) in medial compartment arthosis associated with varus malalignment, with a survival rate of 98.7 % at 5 years and 75.9 % at 7.5 years [2••], but fewer papers have been published regarding distal femoral osteotomy (DFO). However, some issues are still debated for both HTO and DFO; these include the choice between opening and closing wedge osteotomy, the graft selection in the case of opening wedge osteotomy, the type of fixation, and the influence on the patellofemoral joint [3, 4]. Initial enthusiasm for a proximal tibial varus osteotomy to correct the valgus deformity diminished as data indicated unsatisfactory results [5, 6]. This is probably because a major valgus deformity of the knee is often associated with a joint line that slopes superolaterally in the anterior–posterior plane, and this abnormal plane cannot be corrected unless the osteotomy is done proximal to the joint [7••]. Bouillet and Van Gaver in 1961 [8] and Coventry in 1973 [9] established that if the valgus deformity is more than 12°–15° or if the joint plane deviates from the horizontal more than 140°, a DFO should be performed, rather than an HTO. The method is based on the fact that the normal tibiofemoral angle is 5°–8° of valgus; therefore, correction of alignment, so that the femur and tibia are anatomically collinear, will result in 5°–8° of mechanical varus and effectively unload the lateral compartment. Good results are reported in the literature about DFO [10], but there is still an open debate overall on the differences in terms of outcome between closing and opening wedge osteotomy [11•, 12•] and whether patellofemoral arthritis can be a potential contraindication to this surgery or the DFO can modify the patellofemoral alignment [13–15].
The purpose of this article is to analyze the literature about DFO, trying to clarify indications, functional outcomes, and survivorship of different surgical techniques described in the literature.
Indications
The correct selection of the patients undergoing DFO, as well as HTO, is mandatory for achieving good outcomes [16]. DFO can be performed to correct both congenital malalignment and posttraumatic deformity [17, 18••]. First of all, medical comorbidities should be addressed, as well as patients’ functional expectations. Obesity, evaluated as 1.32 times the normal weight or BMI greater than 30 kg/m2, has been associated with poorer outcomes [2••, 19]. Presence of inflammatory disorders should be addressed as well; in this population, valgus deformity is common, but osteotomies are normally contraindicated [16]. Patients considered for a DFO should be less than 65 years old, active, and affected only by lateral arthritis; however, not only the age, but also the activity level, lifestyle, and general health must be taken into consideration [18••].
DFO should be considered in the presence of isolated lateral compartment arthritis. However, it is still debated whether patellar osteoarthritis can influence clinical results. Performing a varus opening wedge, DFO probably reduces the Q angle and medializes the anterior tibial tubercle, unloading the patellofemoral compartment laterally; for these reasons, some authors have not reported a moderate patellofemoral arthritis as a contraindication to DFO [20••, 21]. In some cases, DFO, as well as HTO, can be considered in association with other procedures, such as cartilage procedures, in order to underload the affected compartment, with good midterm results [22, 23].
A complete knee examination should be assessed before surgery to localize joint-line tenderness, meniscal pathology, patellofemoral joint pain, or ligamentous instability. In the case of associated ligamentous instability, a concomitant or staged ligament reconstruction can be planned, or the osteotomy can be performed with the aim of partially solving the instability [24•, 25, 26]. Recently, Hetsroni et al. experimentally reproduced an Medial Collateral Ligament (MCL) deficiency and evaluated the compensation obtained with a varus lateral opening wedge DFO. In their cadaveric specimens, when the superficial MCL was transected, medial knee opening at 30° of flexion significantly decreased after lateral opening wedge DFO. When the superficial MCL, deep MCL, and ACL were all sectioned, medial knee opening in extension decreased after lateral opening wedge DFO, but this was not significant [27]. Preoperative knee range of motion (ROM) is another important factor to evaluate when considering a knee realignment procedure. There are few papers considering variables predicting poor outcomes in varus DFO, but some authors have described an ROM of less than 120° of flexion as a negative prognostic factor in HTO [2••]. Besides, the patient’s gait should be observed, as well as the lower limb deformity, on both sagittal and coronal planes (recurvatum).
Common contraindications to an osteotomy are the presence of an inflammatory disease and very unstable knees or valgus deformity greater than 20°, because it can be associated with severe ligamentous instability. Furthermore, severe bone loss and severe valgus deformity associated with tibial subluxation greater than 1 cm are other contraindications to osteotomies [18••], as well as severe articolar disruption (III or more according to Ahlbäck classification) [28].
Preoperative setting
Traditionally, diaphyseal deformity should be corrected through the identification of the center of rotation of angulation (CORA) [29], but the CORA is normally not calculated in the presence of a epiphyseal or articular deformity if a metaphyseal deformity is planned [30].
In order to properly plan an osteotomy, a complete radiographic examination should be performed, including routine antero-posterior, lateral, and skyline views, to rule out multicompartmental arthritis and to assess the tibial slope [18••]. To assess the amount of the deformity and correction, an antero-posterior long-leg x-ray with the patient standing (including both the coxo-femoral and ankle joint), as well as a Rosenberg view, should be performed. The Rosenberg view facilitates the diagnosis of lateral (or medial) compartment cartilage wear. Besides, the Rosenberg view has a strong predictive value if the deformity is associated with a cruciate deficiency and the cartilage wear is located overall in the posterior tibial plateau [31]. Magnetic resonance imaging is helpful in assessing any chondral or ligamentous pathology and in evaluating the stress response of the subchondral bone [16, 18••].
Correct preoperative planning is mandatory for achieving a good malalignment correction. The method most commonly described in the literature is the one from Dugdale et al. [32]; the weight-bearing line (or mechanical axis) is placed at a selected position 48 %–50 % across the width of the tibial plateau from medial to lateral. The correction angle is formed by the angle between the line from the center of the femoral head to 50 % of the width of the tibial plateau and the line from the center of the talus to the same point on the tibial plateau. In HTO for varus malalignment, a slight overcorrection is usually suggested in order to obtain better results [2••]. Conversely, different authors have stated that varus overcorrection using DFO is absolutely contraindicated for optimal long-term results [18••]. Figure 1 shows a correct preoperative planning for a DFO.
Fig. 1.
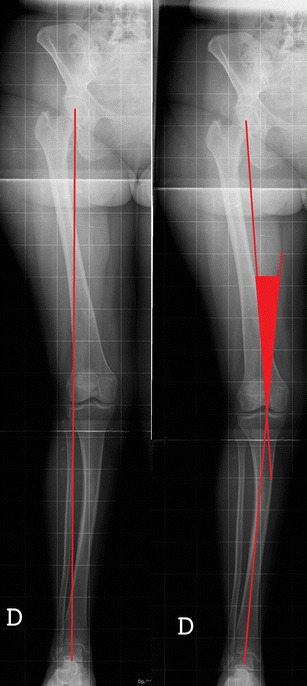
Preoperative planning on long-leg x-rays. a A valgus knee with the mechanical axis. b The correction angle is planned drawing two lines: one from the center of the hip to 50 % of the tibial plateau and one from the center of the talus to the same point
Surgical techniques and results
Different surgical techniques are reported in the literature about varus DFO, and these include (1) medial closing wedge DFO, (2) lateral opening wedge DFO, (3) dome osteotomy, and (4) other surgical techniques. In this section, we will briefly describe each technique and report the results in the literature.
Medial closing wedge
In the literature, there are more papers describing the results of medial closing wedge DFO than lateral opening wedge DFO. The most commonly performed technique was described by McDermott et al. using a 90° blade plate. The basis of this surgical technique is that if the 90° plate is placed parallel to the transcondylar axis and (after removing the medial wedge) to the medial part of the femoral cortex, the tibio-femoral angle will be 0°. Once the osteotomy was healed, the authors allowed progressive full weight-bearing; the resumption of full activities was allowed 3–6 months after the operation. Mc Dermott et al. reported satisfactory results in 20 out of 22 patients, mostly regarding pain improvement. The authors also suggested removing the plate 18–24 months after surgery to avoid soft tissue irritation and 6 months before performing a total knee arthroplasty [7••].
Different authors have reported good results with this technique, with a survival rate of 80 % at 40 months, but with a decrease to 45 % at 15 years. [10, 21, 33–37]. More recently Kosashvili et al. described their results with 33 consecutive DFOs performed with the same technique at a minimum follow-up of 10 years. The failure rate was 48.5 % at 10 years, and 58.8 % of the cases had good or excellent results. They compared the failed-group and the nonfailed one, and they stated that in the failed group, the average age was significantly higher [38]. On the other hand, Forkel et al. analyzed different variables potentially correlated with the outcome of DFO; they found that neither age nor presence of associated microfractures affected the result [39]. Afterward, different authors described their results with slight modification of the original surgical technique. Healy et al. in 1988 [40] described the results of 23 cases treated with closing wedge DFO. They planned an overcorrection of about 4° to unload the lateral compartment. They described a technique using three guide-pins: The first was positioned perpendicular to the long axis of the femoral shaft, 1–2 cm proximal to the medial epicondyle. The second pin was placed at the level of the distal cut and formed, with the first pin, an angle equivalent to the correction angle. The third pin was placed parallel to the second one, but distal and anterior to guide the saw and chisel used for the osteotomy. At the last follow-up, 93 % of the patients were rated as good or excellent according to the Hospital for Special Surgery (HSS) knee score and 86 % of them expressed satisfaction with the outcomes. Learmonth in 1990 [41] described a similar technique, with the addition of a special jig placed on the anterior tibial crest to allow double-checking of the final alignment.
Mathews et al. reported their results for 21 patients treated with a varus DFO using different types of fixation (plaster cast, staples, and blade plate). Thirty-three percent of the patients had satisfactory results using the HSS score, and 57 % had satisfactory results using the Knee Society Clinical Rating. Fifty-seven percent had a significant complication, including severe knee stiffness requiring manipulation under anesthesia (48 %), nonunion/delayed union (19 %), infection (10 %), and fixation failure (5 %). Five (19 %) knees required total knee replacement within 5 years of surgery [42].
Stähelin et al. reported on their results using an incomplete oblique DFO stabilized with a malleable semitubular plate bent as an angled plate and lag-screws, in 19 patients. Theoretical advantages of this technique were that (1) the descending direction of the osteotomy led to complete circumferential congruence and (2) the compression achieved with the lag screws on the entire contact area guaranteed a frictional force that increased the stability of the osteotomy. They reported a mean increase in the HSS score to 84 points, but 1 patient had an implant failure and 3 patients required a longer immobilization period to heal [43]. Table 1 summarizes the results in the literature about medial closing wedge DFO.
Table 1.
Summary of the results described in the literature on medial closing wedge DFVO
| Author | Year | Number | Median Age (range) | Median F-UP | Type of Fixation | Results |
|---|---|---|---|---|---|---|
| McDermott [7••] | 1988 | 22 | Not reported | Not reported | 90° blade plate | 20/22 good results. 1 plate failure and 1 conversion to TKA. Greatest improvement in pain. |
| Healy [39] | 1988 | 23 | 56 years (19–70) | 4 years | 90° blade plate | 93 % were rated as good or excellent (Hospital for Special Surgery Knee Score [HSS]), and 86 % were satisfied with the outcome. |
| Edgerton [36] | 1993 | 23 | Not reported | 8.3 years | 90° blade plate | 71 % rate of satisfactory results |
| Finkelstein [33] | 1996 | 21/24 | 56.3 years (27–77) | 133 months | 90° blade plate | 13 not failed: average improvement in the score of 30 points, greatest improvement in pain. 7 failed osteotomies with subsequent TKA. The survival rate was 83 % (95%CI 65 %–98 %) at 40 months and 64 % (95%CI 48 %–80 %) at the final follow-up. |
| Mathews [41] | 1998 | 21 | Not reported | 1–8 years | 10 knees plaster cast, 5 had 2 staples with a plaster cast, and 6 knees had rigid internal fixation with an AO blade plate. | 33 % of patients had a satisfactory result using the HSS score, and 57 % had a satisfactory result using the Knee Society Clinical Rating. 57 % percent had a significant complication, 19 % knees required TKA. Positive prognostic factors were: grades I to III osteoarthritis, adequate correction of valgus deformity and rigid internal fixation to permit postoperative early mobilization. |
| Stahelin [42] | 2000 | 19 | 56 years (39–71) | 5 years | Malleable semitubular plate | Average HSS score increased: 84 points. 11 knees rated as excellent. 1 implant failure. |
| Aglietti [35] | 2000 | 18 | 54 years (38–75) | 9 years | 90° blade plate | 77 % good or excellent results according to the Knee Society rating system. No patients had nonunion or infection. 1 patient converted to TKA. |
| Marin Morales [37] | 2000 | 17 | 55 years (50–72) | 6.5 years | 95° AO blade-plate and straight blade-plate | 75 % good or excellent results. 1 deep infection. |
| Wang [21] | 2005 | 30 | 53 years (31–64) | 99 months | 90° blade plate | 83 % had a satisfactory result, two had a fair result, and three had conversion to a total knee arthroplasty. The mean knee score improved from 46 points (range, 20–63 points) preoperatively to 88 points (range, 65–99 points) at the time of the most recent follow-up. The survival rate at 10 years was 87 % (95 % CI, 69 %–100 %). |
| Backstein [10] | 2007 | 38 | 44.1 years (20–67) | 123 months | 90° blade plate | Radiographic analysis demonstrated an average tibiofemoral angle 11.68 of valgus preoperatively and 1.28 of varus postoperatively. 60 % had good or excellent results, 7.5 % had a fair result, and 7.5 % had poor results. 230 % converted to TKA. The 10-year survival rate was 82 % (95 % CI, 75 %–89 %), and the 15-year one was 45 % (95 % CI, 33 %–57 %). |
| Omidi-Kashani [34] | 2009 | 25 | 23.3 years (17–41) | 16.3 months | 90° blade plate | The mean knee score improved from 90.7 points (range, 77–96 points) preoperatively to 98.13 points (range, 93–100 points) at the time of the most recent follow-up. |
| Kosashvili [38] | 2010 | 33 | 45.5 years (24–63) | 15.1 years | 90° blade plate | 15 patients converted to TKA, so the failure rate was 48.5 % at 15.6 years. Of the remaining, 58.8 % had good or excellent results. The average age in the failed group was significantly higher than in the non-failed one (47.6 vs. 45.6) |
| Forkel [39] | 2014 | 23 | 47 years (25–55) | 3.5 years | Angle-stable locking plate | All KOOS subitems increased significantly. No significant difference in the subgroup analysis of KOOS subitems for patients with and without microfracture or age (<50 vs. >50 years). 1 case of revision because of nonunion |
Note. F-UP, follow-up; TKA, total knee arthroplasty; CI, confidential interval; KOOS, knee osteoarthritis outcome
Lateral opening wedge
Due to the good results reported with opening wedge HTO [2••, 3, 4] and the small amount of correction achievable with the medial closing wedge DFO, recently, different techniques for lateral opening wedge DFO have been described.
Puddu et al. developed a complete system similar to the medial opening wedge HTO, to perform varus lateral opening wedge DFO [18••]. The designed T-shaped tooth plate had four holes proximal and three holes distal to the tooth. More recently, a new version of the plate has been developed. This is a locking plate made of titanium alloy and allows some freedom in screw orientation. With this technique, a 12-cm straight lateral incision that starts from the epicondyle and is extended proximally is used. After careful dissection, leaving the joint capsule intact, the lateral cortex of the femur is exposed. Retractors are placed to avoid vessels damage, and, with the knee in extension and under fluoroscopy, a guide wire is drilled free-hand with an oblique direction of about 20° from three fingers above the lateral epicondyle to few millimeters proximal to the medial epicondyle. The surgeon should start the osteotomy with the oscillating saw and then advance using osteotomes, preserving 1 cm of the medial hinge. Then the osteotomy can be opened with the wedge gradually, until the desired correction is obtained. The osteotomy is stabilized with the proper plate with the “tooth” of the same size of the wedge and is fixed with screws. In addition, a lateral plate also acts as a tension band, with proven mechanical advantages, as compared with a medial plate. The authors suggested a postoperative protocol, with the knee immobilized in full extension or 10° of flexion when standing, starting CPM immediately and allowing no weight-bearing ROM exercises with the brace unlocked. The patients are kept non-weight-bearing for 6 weeks; then partial weight-bearing is allowed for 2 weeks, and full weight-bearing at 8 weeks [18••].
In the literature, good outcomes have been reported using this technique, and most of the authors have agreed that the lateral opening wedge technique allows a more precise correction, with a survival rate of around 80 % at 7 years, and less plate intolerance, as compared with other systems [12•, 18••, 44]. Other authors have reported their results using a similar opening wedge technique stabilized with another method of fixation, instead of the Puddu Plate® [18••].
Jacobi et al. in 2010 described their technique using a Tomofix® plate (Synthes), encouraged from the good results obtained with the same system in the proximal tibia [45, 46]. This fixation should be more stable, allowing earlier total weight-bearing. They reported on 14 patients in which they frequentlyobserved a delayed osteotomy healing; however, outcomes were satisfactory once the osteotomy was healed, and also if 86 % of the patients complained about plate intolerance [11•].
Recently Saithna et al. described their results on 22 patients in which they performed a DFO using the technique described by Puddu [18••] and 1 performed with the Tomofix® (Synthes) plate. They used bone graft only if the gap was greater than 12 mm. They reported a cumulative survival rate of 79 % at 5 years, with a significant improvement in all the outcomes evaluated [47•]. Biomechanical studies have demonstrated greater axial and torsional stability with the TomoFix® plate (Synthes, Switzerland), when compared with the Puddu® plate (Arthrex Inc., Naples) [48•], but no clinical trials confirmed better outcomes with one fixation system as compared with the other.
Finally, Zarrouk et al. described their results on 22 patients in which they performed an opening wedge DFO using a 95° blade plate and without any bone graft. They reported a survival rate of 91 % at 8 years, with 80 % good and excellent results [20••]. Table 2 summarizes the results from literature on lateral opening wedge DFO.
Table 2.
Summary of the results described in the literature on lateral opening wedge DFVO
| Author | Year | Number | Median Age (range) | Median F-UP | Type of Fixation | Results |
|---|---|---|---|---|---|---|
| Puddu [18••] | 2010 | 21 | 54 years | 4–14 years | Puddu® plate | Improving in both International Knee Committe Documentation Committee (IKDC) rating scale and the HSS system at 4–14 years of follow-up. |
| Jacobi [46] | 2010 | 14 | 46 years (28–63) | 45 months | Tomofix® plate | 50 % of osteotomies healed at 3 months, 14 % at 6 months and the other at 9 months. 86 % required plate removal. Mean satisfaction index was 78 %. |
| Zarrouk [20••] | 2010 | 22 | 53 years (27–66) | 54 months | 95 ° blade plate | 80 % had good or excellent results, 9.5 % had fair results, and 9.5 % had poor results. The 8-year survival rate was 91 % (confidence interval, 69—100 %). |
| Thein [4] | 2012 | 6 | 46.7 years | 6.5 years | Puddu® plate | The mean Oxford Knee Score improved from 13.1 ± 8.6 to 26 ± 12.5. The average subjective satisfaction rate at the last follow-up was 6.6 ± 2.8 points. conversion to TKA at the final follow-up |
| Dewilde [44] | 2012 | 19 | Not reported | 68 months | Puddu® plate | The average knee score improved significantly from 43 ± 8 preoperatively to 78 ± 23 at final follow-up. The Kellgren–Lawrence osteoarthritis score remained unchanged. Kaplan–Meier analysis using revision surgery or conversion to TKA as an endpoint demonstrated an 82 % successful survivorship at 7 years of follow-up. |
| Saithna [47•] | 2014 | 22 | 41 years (28–58) | 4.5 years | Puddu® plate and Tomofix® plate | 4 patients underwent TKA. The cumulative survival rate of 79 % at 5 years, with a significant improvement in all the outcomes evaluated. |
Note. F-UP, follow-up; TKA, total knee arthroplasty; CI, confidential interval
There is still a debate as to which is the best “graft” to fill the gap, as well as in medial opening wedge HTO. Different authors have suggested using bone filler for defects greater than 7.5–0 mm [3, 18••]. Many methods have been described for both HTO and DFO: bone grafts (allograft or autograft), synthetic bone substitutes (hydroxyapatite, β-tricalcium phosphate, a combination of both, bone cement) with or without platelet-rich-plasma (PRP), growth factors, and bone marrow stromal cells [28]. Iliac crest autograft are considered the “gold standard,” but considering the donor site morbidity, bone substitutes can be a good choice because of their osteoconductive, osteoinductive, and osteogenic properties, and also if there is still some concern about their mechanical property and biological degradability [49, 50]. Encouraging results have been reported with the use of PRP and marrow stromal cells in association both with bone grafting and bone substitute augmentation, although they are still experimental [51].
Other surgical techniques
There are few reports in the literature regarding a dome femoral osteotomy to correct a valgus knee, reporting on different methods of fixation of the osteotomy [52, 53]. Some of them stabilize the dome DFO using an external fixator, with the main advantage being the ability to perform a combination of angulation and translation to correct the deformity with a lower soft tissue dissection. The main advantages to using a dome osteotomy instead of an oblique one are the following: (1) It allows deformity correction without leg length change; (2) it is performed in the metaphysis, and it facilitates the bone union; (3) it allows for simultaneous correction of valgus and varus or flexion/extension deformity; and (4) the dome-shaped osteotomy creates a larger contact surface [52, 54].
Brinkman et al. stated that, even though the medial closing-wedge DFO offers superior initial stability, an important disadvantage of this single-plane osteotomy is its position relative to the throclea and the patellofemoral joint. They supposed that this type of osteotomy disrupts the soft tissue gliding mechanism, slowing the rehabilitation process. To avoid this inconvenience, they described a new biplane technique, in which the saw cuts for the closing-wedge are made only in the posterior three fourths of the femur, after which an ascending oblique saw cut is performed on the anterior surface of the femur to complete the osteotomy. Through biomechanical tests, they confirmed an improvement in axial stability but with an associated decreased stability in torsion [55].
DFO and patella
The anatomic and physiologic function of the extensor mechanism may be altered during a varus DFO. The theoretical changes in the patella mechanics after DFO are a decrease in quadriceps tendon length and a decrease in Q angle. The typical closing wedge osteotomy on the distal medial femur effectively shortens only the medial side and only a fractional portion of the overall length. This minimal change would equally apply to the Q angle [13]. Theoretically, after a varus DFO, the lateral subluxatiuon of the patella can be reduced, and the patella may be recentered into the groove. In the literature, some authors have stated that the outcome of the DFO seems not to be associated with the presence of severe patellofemoral arthritis [21]. Other authors have described a combined tibial tuberosity osteotomy in cases of severe patellofemoral osteoarthritis, or a combined lateral release, with good clinical outcome [20••].
Complications
There are few reports in the literature about complication rate after DFO, as compared with the reports on HTO, and they are normally divided into intraoperative and postoperative complications.
Regarding the possible intraoperative complications occurring during a DFO, the surgeon must be careful about the propagation of a fracture, either through the far cortex or to the articular joint. If the pin is placed too close to the joint, there will be a little metaphyseal bone between the osteotomy and the articular surface, and this will lead to a greater risk of intraarticular fracture. On the other hand, if the surgeon does not leave enough bone on the medial hinge, the risk of osteotomy subluxation is greater. To avoid both of these complications, the surgeon must carefully select the pin guide position and osteotomy level. When medial hinge disruption and osteotomy displacement occur, the surgeon can fix the problem with a contralateral staple or screw [18••]. The surgeon should be careful not to leave residual bone at the osteotomy level, to improve the compression of the osteotomy and the rate of healing. Theoretically, there is a risk of neurovascular injury performing a DFO; to avoid this complication, a correct position of the blunt retractor is mandatory [56]. In a cadaveric study by Visser et al., the relationship between the vascular structures and the distal femur closing wedge osteotomy performed using a less invasive approach were evaluated. After a 3-D reconstruction, the authors concluded that damages to the vastus medialis and the neurovascular structures (femoral and saphenous nerve and distal geniculate artery that supplies the vastus medialis muscle) are minimized using this less invasive approach [57].
With respet to postoperative complications, the rate of deep venous trombosis has been reported to be as great as that of total knee arthroplasty. Fatal pulmonary embolism is rare, but it has been reported. The risk of compartment syndrome is greater in HTO, as compared with DFO, as well as the risk of patella baja [56]. Postoperative infection is more common if the DFO is stabilized with an external fixator, because of the superficial pin tract infection (25 %–50 %). The rate of nonunion is similar to the one reported for HTO, and it is less common after closing wedge DFO than after opening wedge DFO [56]. Willey et al. reported their complication rate after both HTO and DFO with concomitant significant additional knee reconstruction (cartilage resurfacing requiring an arthrotomy, ligament reconstruction, meniscal transplantation, or extensor mechanism realignment). They described major complications as intraarticular fracture, deep venous thrombosis, deep infection, extension loss, arthrofibrosis, valgus or varus overcorrection, nonunion, and neurovascular injury. On the other hand, complications that were considered minor included hardware pain, superficial infection, anterior knee pain, hematoma, delayed union, and tendonitis. They reported 20 % of major complications and 25.7 % of minor complications, with a higher complication rate for HTO, as compared with DFO, in association with other procedures [58].
Conclusion
In the literature, there are few reports describing the results of DFO, as compared with HTO, probably because valgus malalignment is less common. A correct indication is mandatory to obtain good results. Increased BMI and a presence of an inflammatory disorder have been associated with a poor outcome in HTO and, theoretically, in DFO as well [2••, 16].
Historically, the DFO has most often been performed using a closing wedge technique, with different outcomes reported in the literature, with success rates varying between 82 % at 4 years and less than 50 % at 15 years [10, 21, 33–36]. Consequently, because of the success of opening wedge HTO [2••, 3, 4, 28] and because of the technical difficulties in precisely correcting a large amount of valgus malalignment performing a closing wedge osteotomy, different authors have reported their results performing a lateral opening wedge DFO [12•, 18••, 44]. As compared with the closing wedge technique, an open wedge technique has the advantage of being easier and more precise in adjusting the amount of correction intraoperatively, but despite its precision in deformity correction, lateral wedge osteotomy may have an increased rate of nonunion because of the bone gap [11•].
One of the topics regarding DFO is the method of fixation, which appears to have a great influence on the outcome of this procedure. Mathews et al. described their results with 21 patients in whom they performed a DFO using different type of stabilization (plaster casts, staples, or internal fixation). Satisfactory results were obtained only in those patients who had less severe degrees of osteoarthritis confined to the lateral compartment (grades I to III), adequate correction of valgus deformity (the anatomical axis within 2° from zero), and rigid internal fixation to permit postoperative early mobilization. Besides, the authors concluded that the blade plate is associated with higher healing rates and better outcomes [42].
Metal plates are effective in obtaining a rigid stable fixation, with the disadvantages of extensive soft tissue damage, impossible correction adjustments after surgery, and metal failure. On the contrary, external fixation allows for gradual correction of the deformity, also after surgery, but pin site infection, restriction on ROM and discomfort are common. Intramedullary nails are less invasive than metal plates, but a rigid fixation cannot be obtained in cases of metaphyseal osteotomy. Seah et al. retrospectively evaluated 26 patients in which they performed a DFO stabilized with either fixator-assisted plating or a unilateral frame, and they evaluated the accuracy of correction. The authors concluded that an accurate correction was obtained with both techniques, so the method of fixation should be left to the discretion of the surgeon and needs of the patient [59].
Another important issue is the necessity of filling the bone gap during a lateral opening wedge DFO. Puddu et al. stated that any gap greater than 7.5 mm should be filled with autologous, allogenic, or synthetic bone, while gaps smaller than that may be left unfilled [18••]. There is no study in the literature comparing the healing rate using autograft, allograft, or bone substitute. The main advantage to using a bone substitute is the possibility of obtaining a large amount, with a specific shape reproducing the gap.
There is no consensus in the literature about the postoperative program after a DFO, with either a closing wedge or an opening wedge technique. Normally, patients are kept non-weight-bearing or partial weight-bearing depending on the stability of the fixation, until the osteotomy healing is demonstrated [18••].
In painful genu valgum with association of lateral compartment arthritis in young or middle-aged patients, the varus DFO in an effective treatment.
There are no proofs of the superiority of one surgical technique over the other. Closing wedge DFO guarantees a higher healing rate, but it is more demanding to obtain a precise correction for medium to large amounts of malalignment. On the contrary, opening wedge DFO allows a more precise and gradual correction of the deformity, so it is probably a better choice for deformity greater than 10° of valgus.
Acknowledgments
Conflict of interest
Federica Rosso declares that she has no conflict of interest.
Fabrizio Margheritini declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
ᅟ
No human or animal studies performed by the authors
This article does not contain any studies with human or animal subjects performed by any of the authors.
Human studies done by authors (but no animal studies)
This article does not contain any studies with animal subjects performed by any of the authors. With regard to the authors’ research cited in this paper, all procedures were followed in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 2000 and 2008.
Animal studies done by authors (but no human studies)
This article does not contain any studies with human subjects performed by any of the authors.
With regard to the authors’ research cited in this paper, all institutional and national guidelines for the care and use of laboratory animals were followed.
Contributor Information
Federica Rosso, Phone: 011/5085014, Email: federica.rosso@yahoo.it.
Fabrizio Margheritini, Email: fabrizio.margheritini@uniroma4.it.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.••.Saithna A, Kundra R, Modi CS, Getgood A, Spalding T. Distal femoral varus osteotomy for lateral compartment osteoarthritis in the valgus knee. A systematic review of the literature. Open Orthop J. 2012;6:313–9. doi: 10.2174/1874325001206010313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.••.Bonasia DE, Dettoni F, Sito G, Blonna D, Marmotti A, Bruzzone M, et al. Medial opening wedge high tibial osteotomy for medial compartment overload/arthritis in the varus knee: prognostic factors. Am J Sports Med. 2014;42(3):690–8. doi: 10.1177/0363546513516577. [DOI] [PubMed] [Google Scholar]
- 3.Rossi R, Bonasia DE, Amendola A. The role of high tibial osteotomy in the varus knee. J Am Acad Orthop Surg. 2011;19(10):590–9. doi: 10.5435/00124635-201110000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Dettoni F, Bonasia DE, Castoldi F, Bruzzone M, Blonna D, Rossi R. High tibial osteotomy versus unicompartmental knee arthroplasty for medial compartment arthrosis of the knee: a review of the literature. Iowa Orthop J. 2010;30:131–40. [PMC free article] [PubMed] [Google Scholar]
- 5.Shoji H, Insall J. High tibial osteotomy for osteoarthritis of the knee with valgus deformity. J Bone Joint Surg Am. 1973;55(5):963–73. [PubMed] [Google Scholar]
- 6.Coventry MB. Proximal tibial varus osteotomy for osteoarthritis of the lateral compartment of the knee. J Bone Joint Surg Am. 1987;69(1):32–8. [PubMed] [Google Scholar]
- 7.••.McDermott AG, Finklestein JA, Farine I, Boynton EL, MacIntosh DL, Gross A. Distal femoral varus osteotomy for valgus deformity of the knee. J Bone Joint Surg Am. 1988;70(1):110–6. [PubMed] [Google Scholar]
- 8.Bouillet H VGP. Knee arthritis. Pathogenesis and treatment. L’arthrose du genou. Etude pathogenique et traitement. . Acta Orthop Belg. 1961(27):6.
- 9.Coventry MB. Osteotomy about the knee for degenerative and rheumatoid arthritis. J Bone Joint Surg Am. 1973;55(1):23–48. [PubMed] [Google Scholar]
- 10.Backstein D, Morag G, Hanna S, Safir O, Gross A. Long-term follow-up of distal femoral varus osteotomy of the knee. J Arthroplasty. 2007;22(4 Suppl 1):2–6. doi: 10.1016/j.arth.2007.01.026. [DOI] [PubMed] [Google Scholar]
- 11.•.Jacobi M, Wahl P, Bouaicha S, Jakob RP, Gautier E. Distal femoral varus osteotomy: problems associated with the lateral open-wedge technique. Arch Orthop Trauma Surg. 2011;131(6):725–8. doi: 10.1007/s00402-010-1193-1. [DOI] [PubMed] [Google Scholar]
- 12.•.Dewilde TR, Dauw J, Vandenneucker H, Bellemans J. Opening wedge distal femoral varus osteotomy using the puddu plate and calcium phosphate bone cement. Knee Surg Sports Traumatol Arthrosc. 2013;21(1):249–54. doi: 10.1007/s00167-012-2156-6. [DOI] [PubMed] [Google Scholar]
- 13.Closkey RF, Windsor RE. Alterations in the patella after a high tibial or distal femoral osteotomy. Clin Orthop Relat Res. 2001;389:51–6. doi: 10.1097/00003086-200108000-00009. [DOI] [PubMed] [Google Scholar]
- 14.Purushothaman B, Agarwal A, Dawson M. Posttraumatic chronic patellar dislocation treated by distal femoral osteotomy and medial patellofemoral ligament reconstruction. Orthopedics. 2012;35(11):e1668–72. doi: 10.3928/01477447-20121023-30. [DOI] [PubMed] [Google Scholar]
- 15.Kwon JH, Kim JI, Seo DH, Kang KW, Nam JH, Nha KW. Patellar dislocation with genu valgum treated by DFO. Orthopedics. 2013;36(6):840–3. doi: 10.3928/01477447-20130523-35. [DOI] [PubMed] [Google Scholar]
- 16.Preston CF, Fulkerson EW, Meislin R, Di Cesare PE. Osteotomy about the knee: applications, techniques, and results. J Knee Surg. 2005;18(4):258–72. doi: 10.1055/s-0030-1248190. [DOI] [PubMed] [Google Scholar]
- 17.Lustig S, Khiami F, Boyer P, Catonne Y, Deschamps G, Massin P, et al. Post-traumatic knee osteoarthritis treated by osteotomy only. Orthop Traumatol Surg Res. 2010;96(8):856–60. doi: 10.1016/j.otsr.2010.06.012. [DOI] [PubMed] [Google Scholar]
- 18.••.Puddu GCM, Cerullo G, Franco V, Giannì E. Which osteotomy for a valgus knee? Int Orthop. 2010;34(2):239–47. doi: 10.1007/s00264-009-0820-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Coventry MBID, Wallrichs SL. Proximal tibial osteotomy. A critical long-term study of 87 cases. J Bone Joint Surg Am. 1993;75:196–201. doi: 10.2106/00004623-199302000-00006. [DOI] [PubMed] [Google Scholar]
- 20.••.Zarrouk A, Bouzidi R, Karray B, Kammoun S, Mourali S, Kooli M. Distal femoral varus osteotomy outcome: is associated femoropatellar osteoarthritis consequential? Orthop Traumatol Surg Res. 2010;96(6):632–6. doi: 10.1016/j.otsr.2010.04.009. [DOI] [PubMed] [Google Scholar]
- 21.Wang JW, Hsu CC. Distal femoral varus osteotomy for osteoarthritis of the knee. J Bone Joint Surg Am. 2005;87(1):127–33. doi: 10.2106/JBJS.C.01559. [DOI] [PubMed] [Google Scholar]
- 22.Drexler M, Gross A, Dwyer T, Safir O, Backstein D, Chaudhry H, et al. Distal femoral varus osteotomy combined with tibial plateau fresh osteochondral allograft for post-traumatic osteoarthritis of the knee. Knee Surg Sports Traumatol Arthrosc. 2014 doi: 10.1007/s00167-013-2828-x. [DOI] [PubMed] [Google Scholar]
- 23.Bonasia DE, Amendola A. Combined medial meniscal transplantation and high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2010;18(7):870–3. doi: 10.1007/s00167-009-0999-2. [DOI] [PubMed] [Google Scholar]
- 24.•.Phisitkul P, Wolf BR, Amendola A. Role of high tibial and distal femoral osteotomies in the treatment of lateral-posterolateral and medial instabilities of the knee. Sports Med Arthrosc. 2006;14(2):96–104. doi: 10.1097/01.jsa.0000212306.47323.83. [DOI] [PubMed] [Google Scholar]
- 25.Cameron JC, Saha S. Management of medial collateral ligament laxity. Orthop Clin North Am. 1994;25(3):527–32. [PubMed] [Google Scholar]
- 26.Paley D, Bhatnagar J, Herzenberg JE, Bhave A. New procedures for tightening knee collateral ligaments in conjunction with knee realignment osteotomy. Orthop Clin North Am. 1994;25(3):533–55. [PubMed] [Google Scholar]
- 27.Hetsroni I, Lyman S, Pearle AD, Marx RG. The effect of lateral opening wedge distal femoral osteotomy on medial knee opening: clinical and biomechanical factors. Knee Surg Sports Traumatol Arthrosc. 2013 doi: 10.1007/s00167-013-2405-3. [DOI] [PubMed] [Google Scholar]
- 28.Amendola A, Bonasia DE. Results of high tibial osteotomy: review of the literature. Int Orthop. 2010;34(2):155–60. doi: 10.1007/s00264-009-0889-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Paley D, Herzenberg JE, Tetsworth K, McKie J, Bhave A. Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am. 1994;25(3):425–65. [PubMed] [Google Scholar]
- 30.Fabricant PD, Camara JM, Rozbruch SR. Femoral deformity planning: intentional placement of the apex of deformity. Orthopedics. 2013;36(5):e533–7. doi: 10.3928/01477447-20130426-11. [DOI] [PubMed] [Google Scholar]
- 31.Rosenberg TD, Paulos LE, Parker RD, Coward DB, Scott SM. The forty-five-degree posteroanterior flexion weight-bearing radiograph of the knee. J Bone Joint Surg Am. 1988;70(10):1479–83. [PubMed] [Google Scholar]
- 32.Dugdale TW, Noyes FR, Styer D. Preoperative planning for high tibial osteotomy. The effect of lateral tibiofemoral separation and tibiofemoral length. Clin Orthop Relat Res. 1992;274:248–64. [PubMed] [Google Scholar]
- 33.Finkelstein JA, Gross AE, Davis A. Varus osteotomy of the distal part of the femur. A survivorship analysis. J Bone Joint Surg Am. 1996;78(9):1348–52. doi: 10.2106/00004623-199609000-00008. [DOI] [PubMed] [Google Scholar]
- 34.Omidi-Kashani F, Hasankhani IG, Mazlumi M, Ebrahimzadeh MH. Varus distal femoral osteotomy in young adults with valgus knee. J Orthop Surg Res. 2009;4:15. doi: 10.1186/1749-799X-4-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Aglietti P, Menchetti PP. Distal femoral varus osteotomy in the valgus osteoarthritic knee. Am J Knee Surg. 2000;13(2):89–95. [PubMed] [Google Scholar]
- 36.Edgerton BC, Mariani EM, Morrey BF. Distal femoral varus osteotomy for painful genu valgum. A five-to-11-year follow-up study. Clin Orthop Relat Res. 1993;288:263–9. [PubMed] [Google Scholar]
- 37.Marin Morales LA, Gomez Navalon LA, Zorrilla Ribot P, Salido Valle JA. Treatment of osteoarthritis of the knee with valgus deformity by means of varus osteotomy. Acta Orthop Belg. 2000;66(3):272–8. [PubMed] [Google Scholar]
- 38.Kosashvili Y, Safir O, Gross A, Morag G, Lakstein D, Backstein D. Distal femoral varus osteotomy for lateral osteoarthritis of the knee: a minimum ten-year follow-up. Int Orthop. 2010;34(2):249–54. doi: 10.1007/s00264-009-0807-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Forkel P, Achtnich A, Metzlaff S, Zantop T, Petersen W. Midterm results following medial closed wedge distal femoral osteotomy stabilized with a locking internal fixation device. Knee Surg Sports Traumatol Arthrosc. 2014 doi: 10.1007/s00167-014-2953-1. [DOI] [PubMed] [Google Scholar]
- 40.Healy WL, Anglen JO, Wasilewski SA, Krackow KA. Distal femoral varus osteotomy. J Bone Joint Surg Am. 1988;70(1):102–9. [PubMed] [Google Scholar]
- 41.Learmonth ID. A simple technique for varus supracondylar osteotomy in genu valgum. J Bone Joint Surg (Br) 1990;72(2):235–7. doi: 10.1302/0301-620X.72B2.2312562. [DOI] [PubMed] [Google Scholar]
- 42.Mathews J, Cobb AG, Richardson S, Bentley G. Distal femoral osteotomy for lateral compartment osteoarthritis of the knee. Orthopedics. 1998;21(4):437–40. doi: 10.3928/0147-7447-19980401-08. [DOI] [PubMed] [Google Scholar]
- 43.Stahelin T, Hardegger F, Ward JC. Supracondylar osteotomy of the femur with use of compression. Osteosynthesis with a malleable implant. J Bone Joint Surg Am. 2000;82(5):712–22. doi: 10.2106/00004623-200005000-00012. [DOI] [PubMed] [Google Scholar]
- 44.Thein R, Bronak S, Thein R, Haviv B. Distal femoral osteotomy for valgus arthritic knees. J Orthop Sci. 2012;17(6):745–9. doi: 10.1007/s00776-012-0273-1. [DOI] [PubMed] [Google Scholar]
- 45.Staubli AE, De Simoni C, Babst R, Lobenhoffer P. TomoFix: a new LCP-concept for open wedge osteotomy of the medial proximal tibia–early results in 92 cases. Injury. 2003;34(Suppl 2):B55–62. doi: 10.1016/j.injury.2003.09.025. [DOI] [PubMed] [Google Scholar]
- 46.Jacobi MJR. Open wedge osteotomy in the treatmen of medial osteoarthritis of the knee. Tech Knee Surg. 2005;4(2):70–8. doi: 10.1097/01.btk.0000164755.04528.da. [DOI] [Google Scholar]
- 47.•.Saithna A, Kundra R, Getgood A, Spalding T. Opening wedge distal femoral varus osteotomy for lateral compartment osteoarthritis in the valgus knee. Knee. 2014;21(1):172–5. doi: 10.1016/j.knee.2013.08.014. [DOI] [PubMed] [Google Scholar]
- 48.•.Stoffel K, Stachowiak G, Kuster M. Open wedge high tibial osteotomy: biomechanical investigation of the modified arthrex osteotomy plate (puddu plate) and the TomoFix plate. Clin Biomech (Bristol, Avon) 2004;19(9):944–50. doi: 10.1016/j.clinbiomech.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 49.Gaasbeek RD, Toonen HG, van Heerwaarden RJ, Buma P. Mechanism of bone incorporation of beta-TCP bone substitute in open wedge tibial osteotomy in patients. Biomaterials. 2005;26(33):6713–9. doi: 10.1016/j.biomaterials.2005.04.056. [DOI] [PubMed] [Google Scholar]
- 50.Aryee S, Imhoff AB, Rose T, Tischer T. Do we need synthetic osteotomy augmentation materials for opening-wedge high tibial osteotomy. Biomaterials. 2008;29(26):3497–502. doi: 10.1016/j.biomaterials.2008.05.027. [DOI] [PubMed] [Google Scholar]
- 51.Dallari D, Savarino L, Stagni C, Cenni E, Cenacchi A, Fornasari PM, et al. Enhanced tibial osteotomy healing with use of bone grafts supplemented with platelet gel or platelet gel and bone marrow stromal cells. J Bone Joint Surg Am. 2007;89(11):2413–20. doi: 10.2106/JBJS.F.01026. [DOI] [PubMed] [Google Scholar]
- 52.Gugenheim JJ, Jr, Brinker MR. Bone realignment with use of temporary external fixation for distal femoral valgus and varus deformities. J Bone Joint Surg Am. 2003;85-A(7):1229–37. doi: 10.2106/00004623-200307000-00008. [DOI] [PubMed] [Google Scholar]
- 53.Luna-Pizarro D, Moreno-Delgado F, De la Fuente-Zuno JC, Meraz-Lares G. Distal femoral dome varus osteotomy: surgical technique with minimal dissection and external fixation. Knee. 2012;19(2):99–102. doi: 10.1016/j.knee.2011.01.005. [DOI] [PubMed] [Google Scholar]
- 54.Yoo MJ, Yoo JS, Lee JY, Hwang CH. Deformity correction by femoral supracondylar dome osteotomy with retrograde intramedullary nailing in varus deformity of the distal femur after pathologic fracture of giant cell tumor. Knee Surg Relat Res. 2013;25(4):220–4. doi: 10.5792/ksrr.2013.25.4.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Brinkman JM, Hurschler C, Staubli AE, van Heerwaarden RJ. Axial and torsional stability of an improved single-plane and a new bi-plane osteotomy technique for supracondylar femur osteotomies. Knee Surg Sports Traumatol Arthrosc. 2011;19(7):1090–8. doi: 10.1007/s00167-010-1349-0. [DOI] [PubMed] [Google Scholar]
- 56.Koyonos L, Slenker N, Cohen S. Complications in brief: osteotomy for lower extremity malalignment. Clin Orthop Relat Res. 2012;470(12):3630–6. doi: 10.1007/s11999-012-2392-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Visser J, Brinkman JM, Bleys RL, Castelein RM, van Heerwaarden RJ. The safety and feasibility of a less invasive distal femur closing wedge osteotomy technique: a cadaveric dissection study of the medial aspect of the distal femur. Knee Surg Sports Traumatol Arthrosc. 2013;21(1):220–7. doi: 10.1007/s00167-012-2133-0. [DOI] [PubMed] [Google Scholar]
- 58.Willey M, Wolf BR, Kocaglu B, Amendola A. Complications associated with realignment osteotomy of the knee performed simultaneously with additional reconstructive procedures. Iowa Orthop J. 2010;30:55–60. [PMC free article] [PubMed] [Google Scholar]
- 59.Seah KT, Shafi R, Fragomen AT, Rozbruch SR. Distal femoral osteotomy: is internal fixation better than external? Clin Orthop Relat Res. 2011;469(7):2003–11. doi: 10.1007/s11999-010-1755-0. [DOI] [PMC free article] [PubMed] [Google Scholar]


