Abstract
Chikungunya virus (CHIKV) is an emerging alphaviral disease and a public health problem in South Asia including Nepal in recent years. In this study, sera were collected from patients presenting with fever, headache, muscular pain, fatigue, and joint pain of both upper and lower extremities. A total of 169 serum samples were tested for CHIKV and dengue virus (DENV) by using Immunoglobulin M (IgM) and Immunoglobulin G (IgG) antibody using enzyme-linked immunosorbent assay (ELISA) method during August to November 2013. Results showed that 3.6% and 27.8% samples were positive for CHIKV and DENV IgM positive, respectively. Similarly, results of IgG showed 3.0% samples were positive for CHIKV IgG and 29.0% were for DENV IgG positive. Further, a 50% focal reduction neutralization test (FRNT50) was performed to confirm the presence of CHIKV, which demonstrated that 8.9% of CHIKV IgM and/or IgG ELISA positive possessed neutralizing anti-CHIK antibodies. To our knowledge, this is the first report in which the presence of CHIKV is confirmed in Nepalese patients by FRNT50. Basic scientists and clinicians need to consider CHIKV as a differential diagnosis in febrile Nepalese patients, and policy makers should consider appropriate surveillance and actions for control strategies.
Chikungunya virus (CHIKV) is a mosquito-borne febrile illness that is transmitted to humans through the bite of infected Aedes aegypti and Ae. albopictus mosquitoes.1 CHIKV belongs to the Alphavirus genus of the Togaviridae family whereas dengue viruses (DENVs) belong to genus Flavivirus of the family Flaviviridae. Both CHIKV and DENV are transmitted by the same mosquito vectors. The CHIKV was first isolated and characterized in humans and mosquitoes during an outbreak in Tanzania and Mozambique in 1955.2 Afterwards, several outbreaks of CHIKV occurred and affected millions of people in eastern, southern, central Africa and Asia.3 CHIKV was introduced in the Americas in October 2013. As of April 2015, over 1,322,893 cases have been suspected and 30,309 confirmed to be CHIKV in the Americas.4 It generally causes mild illness but sometimes can lead to severe and life-threatening complications. The disease is characterized by an acute illness with fever, chills, headache, nausea, vomiting, joint pain with or without swelling, low back pain, and skin rash. DENV can progress to dengue hemorrhagic fever and dengue shock syndrome while CHIKV causes arthralgia, which may persist for months.5 There is similarity in signs and symptoms of CHIK and DEN, which increases risks for misdiagnosis and underreporting of CHIKV infection in DEN-endemic areas.5 The incubation period of CHIKV is usually 2–10 days, with constitutional symptoms lasting up to 7 days. The symptoms usually resolve within days to a few weeks; but in severe cases, these symptoms may last for months. Herein, we report a serological study of possible CHIKV infection with confirmation by 50% focal reduction neutralization test (FRNT50) among febrile patients for the first time in Nepal.
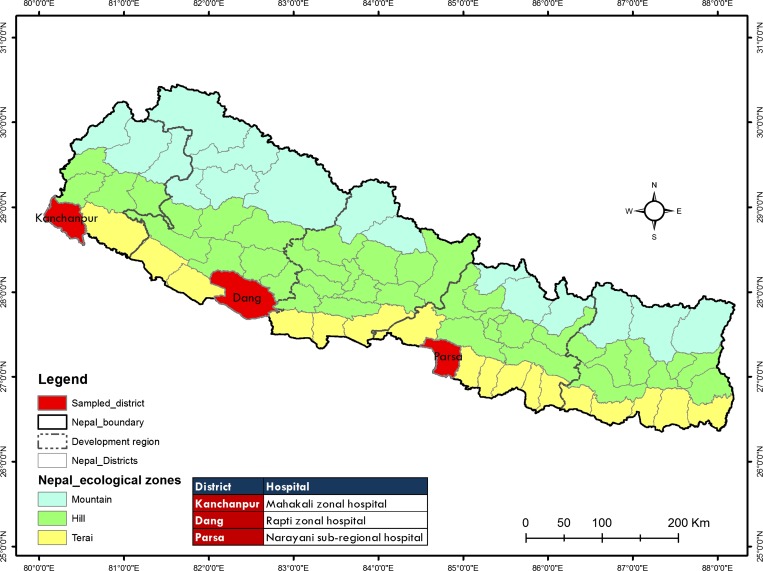
During August to November 2013, physicians observed more patients presenting with fever and joint pain in three large hospitals of Terai region of Nepal namely Narayani Sub-Regional Hospital, Birgunj, Parsa; Rapti Zonal Hospital, Ghorahi, Dang; and Mahakali Zonal Hospital, Mahendranagar, Kanchanpur (Figure 1 ). The clinical features of those patients were consistent with DEN fever and included fever, rashes, and thrombocytopenia. These patients were initially diagnosed clinically as DEN and managed accordingly. A blood sample was collected from all febrile patients at the time of admission to the hospitals (1–7 days after onset of fever). Samples were centrifuged and maintained at 4°C until they arrived in our research center at Kathmandu. The sera were stored at − 70°C until assayed.
Figure 1.
Map of Nepal showing three ecological zones, five development regions, 75 districts, and study sites.
Initially, serum samples were screened for the presence of Immunoglobulin G (IgG) and Immunoglobulin M (IgM) antibodies against DENV using a microtiter plate enzyme-linked immunosorbent assay (ELISA) (Standard Diagnostics Inc., Korea) at Kathmandu, Nepal. The ELISA test was performed according to the manufacture's protocol and interpreted either positive or negative on the basis of absorbance with respect to cutoff values. A sample was considered positive if the absorbance was greater than the cutoff value (0.3 + average of negative value).
The serum samples were shipped to Institute of Tropical Medicine, Nagasaki University, Nagasaki, Japan to perform IgG, IgM ELISA and FRNT50 for CHIKV. In-house IgM-capture ELISA was carried out using the protocol described by Bundo and Igarashi6 with minor modifications. Ninety-six-well microplates were coated with 100 μL (5.5 μg/100 μL) of anti-human IgM and incubated at 37°C for 1 hour. Wells were blocked with Block Ace and were incubated at room temperature (RT) for 1 hour. After incubation, wells were washed with phosphate buffer saline (PBS) containing 0.05% Tween 20 (PBS-T) three times. Test samples, positive and negative controls were diluted 1:100 in PBS-T and 100 μL aliquots were distributed into duplicate wells. The plate was incubated at 37°C for 1 hour and then washed as described above. CHIKV (strain: S-27 African prototype) antigen (128 ELISA units) was added 100 μL/well and incubated at 37°C for 1 hour. After washing, 100 μL/well of 1:150 dilution of HRP-conjugated anti-CHIKV rabbit polyclonal antibody was added and incubated at 37°C for 1 hour. In case of DENV IgM ELISA, tetravalent DENV antigen and 1:2,500 dilution of HRP-conjugated anti-flavi mouse monoclonal antibody was used.7 After washing, 100 μL/well of o-Phenylenediamine dihydrochloride substrate was added and was kept in the dark at RT for 1 hour. To terminate the reaction, 100 μL/well of 1 N sulfuric acid was added to each well, and then the optical density (OD) was read at 492 nm (Multiscan JX, model no. 353; Thermolab System, Tokyo, Japan). A positive control OD492 (or sample)/negative control OD492 ratio greater than or equal to 2.0 was considered positive. In-house indirect IgG ELISA, purified CHIKV (strain: S-27 African prototype) and was used as assay antigen for CHIK indirect ELISA. For DENV IgG indirect ELISA, was carried out following the protocol described previously.8 The protocol for CHIK IgG detection was the same as the IgM detection method except in, assay antigen purified was used for coating plate, dilution of the samples were 1:1,000 and HRP-conjugated anti-human IgG dilution was 1:30,000. A standard curve was prepared using the OD492 values of the CHIKV-positive control sera starting with a 1,000-fold dilution, followed by serial 2-fold dilutions. A sample titer equal to or greater than 1:3,000 was considered to be positive.
For FRNT50, 150 μL of each dilution of the serum samples were mixed with an equal volume of CHIKV, which contained 60 focus-forming units, followed by incubation at 37°C for 1 hour for a virus-antibody neutralization reaction. The virus and serum mixture was inoculated into vero cell monolayer in a 96-well plate at 37°C for 1 hour. After incubation, the infected cells were overlaid with 1.25% methylcellulose 4,000 in 2% fetal calf serum (FCS) minimun essential medium (MEM). The plates were then incubated at 37°C for 30 hours. The plates were washed with PBS, fixed with 4% paraformaldehyde phosphate buffer solution for 30 minutes at RT, rinsed, and permeabilized with 1% NP-40 solution in PBS per well for 30 minutes at RT. After washing, the plates were blocked with Block Ace for 30 minutes at RT. In-house anti-CHIKV rabbit IgG (diluted 1:3,000), was then added, incubated at 37°C for 1 hour and washed. Subsequently, 1:1,000 diluted HRP-conjugated goat anti-rabbit IgG were added to the plates and incubated at 37°C for 1 hour. The staining was visualized by the addition of a 0.5 mg/mL solution of substrate 3, 3′-diaminobenzidine tetrahydrochloride in PBS with 0.03% of H2O2 added at RT for 10 minutes, and the staining reaction was allowed to proceed. After washing the stained cells, the number of foci per well were counted by using a microscope. The reciprocal of the end point serum dilution that provided a 50%, or greater, reduction in the mean number of foci relative to the control wells that contained no serum was considered to be the FRNT50 titer.
A total of 169 serum samples were tested for IgM and IgG against CHIKV and DENV by using IgM capture ELISAs and IgG ELISAs.8 Results of IgM capture ELISAs showed that six (3.6%) samples were positive for CHIKV IgM only, 47 (27.8%) for DENV IgM only, and three (1.8%) for both CHIKV and DENV IgM positive (Table 1). Similarly, results of IgG indirect ELISA showed five (3.0%) samples were positive for CHIKV IgG only, 49 (29.0%) for DENV IgG only, and two (1.2%) for both CHIKV and DENV IgG positive (Table 1). Further, FRNT50 was performed to confirm the presence of CHIKV among anti-CHIKV IgM and/or IgG positive samples. Fifteen samples (8.9%) of CHIKV IgM and/or IgG ELISA positive possessed neutralizing anti-CHIK antibodies. In this study, 83 (49.1%) clinically suspected febrile cases were negative for both DENV and CHIKV. There is a possibility of other tropical and infectious diseases in this area. Typhoid fever and malaria are the other common causes of fever in low land Terai.
Table 1.
Serological results of the 169 febrile patients suspected for chikungunya virus and dengue virus infection
| Profile | CHIK IgM | CHIK IgG | DEN IgM | DEN IgG | Total number of patients | Number of patients (%) |
|---|---|---|---|---|---|---|
| A | (+) | (+) | (−) | (−) | 1 | 0.6 |
| B | (+) | (−) | (−) | (+) | 1 | 0.6 |
| C | (+) | (−) | (−) | (−) | 4 | 2.4 |
| D | (+) | (−) | (+) | (−) | 2 | 1.2 |
| E | (+) | (−) | (+) | (+) | 1 | 0.6 |
| F | (−) | (+) | (+) | (−) | 3 | 1.8 |
| G | (−) | (+) | (+) | (+) | 1 | 0.6 |
| H | (−) | (+) | (−) | (−) | 1 | 0.6 |
| I | (−) | (+) | (−) | (+) | 1 | 0.6 |
| J | (−) | (−) | (+) | (−) | 24 | 14.2 |
| K | (−) | (−) | (+) | (+) | 19 | 11.2 |
| L | (−) | (−) | (−) | (+) | 28 | 16.5 |
| M | (−) | (−) | (−) | (−) | 83 | 49.1 |
CHIK = chikungunya; DEN = dengue; IgG = Immunoglobulin G; IgM = Immunoglobulin M; − = negative; + = positive.
Some of the patients showed positive IgM results for both CHIKV and DENV, suggesting sequential infection by the two viruses in a short period or by concurrent infection with both viruses. A concurrent CHIKV and DENV infection was reported in India,9 Srilanka,11 Singapore,12 and other countries.10 Although a single case report of CHIKV in Nepal has been published,13 no molecular confirmation by polymerase chain reaction has been reported in Nepal. In this study, the detection of anti-CHIKV IgM and/or IgG indicate recent and past infection of CHIKV in Nepal. It also shows that CHIKV has been circulating in this country. The data herein provide the first reported CHIKV infections in Nepalese patients confirmed by neutralization assay among the CHIKV IgM and/or IgG positives. As CHIKV was detected among clinically suspect DEN Nepalese isolates, results indicate a need for improved differential diagnosis in febrile patients in DEN-endemic areas as well as consideration in disease control strategies.
The CHIKV and DENV vectors Ae. aegypti and Ae. albopictus were already established in the Terai region of southern Nepal.14 Most of the health workers in Nepal may be unfamiliar with CHIKV since there is no orientation program or surveillance system for CHIKV in Nepal. The initial signs and symptoms of both DEN and CHIK are quite similar, which may lead to difficulties in making an appropriate provisional diagnosis. Laboratory diagnosis plays a vital role for differential diagnosis between CHIK fevers and other febrile illness. To perform accurate diagnosis, there is an urgent need for sensitive and specific rapid diagnostics tests, which can be used at hospitals in peripheral health settings. Although previous observations suggested that CHIKV does not progress to fatal hemorrhagic fever syndrome and is considered a relatively benign self-limiting illness, neurological manifestations along with other complications have been reported more frequently.15,16 A recent study suggested that CHIKV may induce transient immune suppression that allows opportunistic infections to cause disease in patients.17 There have been frequent outbreaks of CHIKV in India,9 and a potential threat of transmission between Nepal and India exists. Nepal borders with India in the south, east, and west parts; and the two countries share similar climates and population movement. We recommend surveillance for CHIKV, its vectors and preparedness to prevent future outbreaks of CHIKV infection in Terai region of Nepal.
ACKNOWLEDGMENTS
We thank Sujan Shrestha, La Jolla Institute for Allergy and Immunology and Deanna Hagge, Anandaban Hospital for critically reading this manuscript. We also thank all staff of Everest International Clinic and Research Center, for their technical support. We are extremely grateful to the Medical Superintendents, doctors, nurses, staffs, and patients of the respective hospitals for their kind support during the study. We would also like to thank Rojina Shrestha, Srinivas Thapa, and Shrawan Kumar Singh for their assistance in samples collection.
Disclaimer: Institutional review board approval with informed consent procedures was not required in Nepal for this project as samples were diagnostic for suspected DEN patients reportable to the government and undergoing treatment at different hospitals under the Ministry of Health and Population, Nepal. Through this hospital, the government not only helps in providing medical care for patients, but also gathers data from patients as part of Health Management and Information System for health surveillance duties.
Footnotes
Authors' addresses: Basu Dev Pandey, Leprosy Control Division, Department of Health Services, Ministry of Health and Population, Kathmandu, Nepal, E-mail: drbasupandey@gmail.com. Biswas Neupane and Kishor Pandey, Everest International Clinic and Research Center, Virology, Kathmandu, Nepal, E-mails: biswasneupane11@gmail.com and pandey_kishor@hotmail.com. Mya Myat Ngwe Tun and Kouichi Morita, Institute of Tropical Medicine, Virology, Nagasaki, Japan, E-mails: myamyat@tm.nagasaki-u.ac.jp and moritak@nagasaki-u.ac.jp.
References
- 1.Hochedez P, Jaureguiberry S, Debruyne M, Bossi P, Hausfater P, Brucker G, Bricaire F, Caumes E. Chikungunya infection in travellers. Emerg Infect Dis. 2006;12:1565–1567. doi: 10.3201/eid1210.060495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lumsden WHR. An epidemic of virus disease in southern province, Tanganyika territory, in 1952–53: II. General description and epidemiology. Trans R Soc Trop Med Hyg. 1995;49:33–57. doi: 10.1016/0035-9203(55)90081-x. [DOI] [PubMed] [Google Scholar]
- 3.Economopoulou A, Dominguez M, Helynck B, Sissoko D, Wichmann O, Quenel P, Germonneau P, Quatresous I. A typical chikungunya virus infections: clinical manifestations, mortality and risk factors for severe disease during the 2005–2006 outbreak on Reunion. Epidemiol Infect. 2009;137:534–541. doi: 10.1017/S0950268808001167. [DOI] [PubMed] [Google Scholar]
- 4.PAHO Number of Reported Cases of Chikungunya Fever in the Americas—EW 13. 2015. http://www.paho.org/hq/ Available at. Accessed April 4, 2015.
- 5.Carey DE. Chikungunya and dengue: a case of mistaken identity? J Hist Med Allied Sci. 1971;26:243–262. doi: 10.1093/jhmas/xxvi.3.243. [DOI] [PubMed] [Google Scholar]
- 6.Bundo K, Igarashi A. Antibody-capture ELISA for detection of immunoglobulin M antibodies in sera from Japanese encephalitis and dengue hemorrhagic fever patients. J Virol Methods. 1985;11:15–22. doi: 10.1016/0166-0934(85)90120-x. [DOI] [PubMed] [Google Scholar]
- 7.Inoue S, Alonzo MT, Kurosawa Y, Mapua CA, Reyes JD, Dimaano EM, Alera MT, Saito M, Oishi K, Hasebe F, Matias RR, Natividad FF, Morita K. Evaluation of a dengue IgG indirect enzyme-linked immunosorbent assay and a Japanese encephalitis IgG indirect enzyme-linked immunosorbent assay for diagnosis of secondary dengue virus infection. Vector Borne Zoonotic Dis. 2010;10:143–150. doi: 10.1089/vbz.2008.0153. [DOI] [PubMed] [Google Scholar]
- 8.Ngwe Tun MM, Thant KZ, Inoue S, Nabeshima T, Aoki K, Kyaw AK, Myint T, Tar T, Maung KT, Hayasaka D, Morita K. Detection of East Central South African genotype of chikungunya virus in Myanmar, 2010. Emerg Infect Dis. 2010;20:1378–1381. doi: 10.3201/eid2008.131431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chahar HS, Bharai P, Dar L, Guleria R, Kabra SK, Broor S. Co-infection with chikungunya virus and dengue virus in Delhi, India. Emerg Infect Dis. 2009;15:1077–1080. doi: 10.3201/eid1507.080638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Caron M, Paupy C, Grard G, Becquart P, Mombo I, Nso BB, Kassa Kassa F, Nkoghe D, Leroy EM. Recent introduction and rapid dissemination of chikungunya virus and dengue virus serotype 2 associated with human and mosquito coinfections in Gabon, central Africa. Clin Infect Dis. 2012;55:e45–e53. doi: 10.1093/cid/cis530. [DOI] [PubMed] [Google Scholar]
- 11.Kularatne SA, Gihan MC, Weerasinghe SC, Gunasena S. Concurrent outbreaks of chikungunya and dengue fever in Kandy, Sri Lanka, 2006–07: a comparative analysis of clinical and laboratory features. Postgrad Med J. 2009;85:342–346. doi: 10.1136/pgmj.2007.066746. [DOI] [PubMed] [Google Scholar]
- 12.Chang SF, Su C, Shu PY, Yang CF, Liao TL, Cheng CH, Hu HC, Huang JH. Concurrent isolation of chikungunya virus and dengue virus from a patient with co-infection resulting from a trip to Singapore. J Clin Microbiol. 2010;48:4586–4589. doi: 10.1128/JCM.01228-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pun SB, Bastola A, Shah R. Case report: first report of chikungunya virus in Nepal. J Infect Dev Ctries. 2014;8:790–792. doi: 10.3855/jidc.3701. [DOI] [PubMed] [Google Scholar]
- 14.Dhimal M, Gautam I, Kreß A, Müller R, Kuch U. Spatio-temporal distribution of dengue and lymphatic filariasis vectors along an altitudinal transect in central Nepal. PLoS Negl Trop Dis. 2014;8:e3035. doi: 10.1371/journal.pntd.0003035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Powers AM, Loque CH. Changing patterns of chikungunya virus-emergence of a zoonotic arbovirus. J Gen Virol. 2007;88:2363–2377. doi: 10.1099/vir.0.82858-0. [DOI] [PubMed] [Google Scholar]
- 16.Singh SS, Manimunda SP, Sugunan AP, Sahina Vijayachari P. Four cases of acute flaccid paralysis associated with chikungunya virus infection. Epidemiol Infect. 2008;136:1277–1280. doi: 10.1017/S0950268807009739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kumar JC, Vivek Y, Sudhindra P, Dhananjaya B, Kumar AT, Guru K, Kumar A, Heqde MB. Oral candidiasis in chikungunya viral fever: a case report. Cases J. 2010;3:6. doi: 10.1186/1757-1626-3-6. [DOI] [PMC free article] [PubMed] [Google Scholar]