More than three-quarters of the world’s population is exposed to air-pollution that exceeds WHO guidelines, and is a problem that children are particularly susceptible to. This extraordinary figure contributes to enormous health care-related costs for several conditions believed to be caused directly or indirectly by air pollution. This comprehensive review focused on the most recent epidemiological studies – published in the past 10 years − investigating outdoor air pollution and its effect on the respiratory health of children in this country.
Keywords: Air pollution, Asthma, Children, Health effects, Respiratory tract diseases
Abstract
BACKGROUND:
Outdoor air pollution is a global problem with serious effects on human health, and children are considered to be highly susceptible to the effects of air pollution.
OBJECTIVE:
To conduct a comprehensive and updated systematic review of the literature reporting the effects of outdoor air pollution on the respiratory health of children in Canada.
METHODS:
Searches of four electronic databases between January 2004 and November 2014 were conducted to identify epidemiological studies evaluating the effect of exposure to outdoor air pollutants on respiratory symptoms, lung function measurements and the use of health services due to respiratory conditions in Canadian children. The selection process and quality assessment, using the Newcastle-Ottawa Scale, were conducted independently by two reviewers.
RESULTS:
Twenty-seven studies that were heterogeneous with regard to study design, population, respiratory outcome and air pollution exposure were identified. Overall, the included studies reported adverse effects of outdoor air pollution at concentrations that were below Canadian and United States standards. Heterogeneous effects of air pollutants were reported according to city, sex, socioeconomic status and seasonality. The present review also describes trends in research related to the effect of air pollution on Canadian children over the past 25 years.
CONCLUSION:
The present study reconfirms the adverse effects of outdoor air pollution on the respiratory health of children in Canada. It will help researchers, clinicians and environmental health authorities identify the available evidence of the adverse effect of outdoor air pollution, research gaps and the limitations for further research.
Abstract
HISTORIQUE :
La pollution de l’air atmosphérique est un problème mondial qui a de graves effets sur la santé humaine. Les enfants sont considérés comme très vulnérables aux effets de ce type de pollution.
OBJECTIF :
Mener une analyse systématique complète et à jour des publications sur les effets de la pollution de l’air atmosphérique sur la santé respiratoire des enfants du Canada.
MÉTHODOLOGIE :
Les chercheurs ont effectué des recherches dans quatre bases de données électroniques entre janvier 2004 et novembre 2014 pour évaluer l’effet de l’exposition aux polluants atmosphériques sur les symptômes respiratoires, les mesures de la fonction pulmonaire et l’utilisation des services de santé en raison de maladies respiratoires chez les enfants canadiens. Deux analystes ont procédé à l’analyse indépendante du processus de sélection et de l’évaluation de la qualité, au moyen de l’échelle de Newcastle-Ottawa.
RÉSULTATS :
Les chercheurs ont colligé 27 études hétérogènes sur le plan de la méthodologie, de la population, des conséquences respiratoires et de l’exposition à la pollution atmosphérique. Dans l’ensemble, les études incluses portaient sur les effets indésirables de la pollution de l’air atmosphérique à des concentrations inférieures aux normes canadiennes et américaines. Les effets hétérogènes des polluants atmosphériques étaient déclarés selon la ville, le sexe, la situation socioéconomique et le caractère saisonnier du problème. La présente analyse décrit également les tendances de la recherche à l’égard de l’effet de la pollution atmosphérique sur les enfants canadiens depuis 25 ans.
CONCLUSION :
La présente étude confirme de nouveau les effets indésirables de la pollution de l’air atmosphérique sur la santé respiratoire des enfants canadiens. Elle aidera les chercheurs, les cliniciens et les autorités en santé environnementale à repérer les données probantes sur les effets négatifs de la pollution de l’air atmosphérique ainsi que les lacunes et les limites de la recherche, et ce, en prévision de prochaines recherches.
Outdoor air pollution is a global problem with serious effects on human health (1). In fact, it has been estimated that in 2011, approximately 80% of the world’s population was exposed to air pollution levels that exceeded WHO guidelines (2,3). Air pollution is a complex mixture of compounds that vary greatly depending on the emission sources. Typically, the so-called criteria air pollutants (CAP, which include particulate matter [PM], ozone [O3], lead [Pb], carbon monoxide [CO], sulphur oxides [SOx] and nitrogen oxides [NOx]), are monitored in surveillance air-quality networks. Interestingly, PM itself represents a complex mixture of particles of various sizes and concentrations of soil, metals, organics, inorganics, elemental carbon, ions and endotoxins, among other contaminants (4). Recently, the PM2.5 (PM size ≤2.5 μm in aerodynamic diameter) has been the focus of most outdoor air pollution and health studies due to its ability to penetrate the lung tissue and induce local and systemic effects (4).
Based on findings for lung and bladder cancer, the International Agency for Research on Cancer recently classified outdoor air pollution, as a whole, as a group 1 carcinogen (5). In addition, well-documented associations exist between outdoor air pollution and other health conditions including asthma, cardiovascular diseases, respiratory infections, adverse birth outcomes and additional cancers, such as leukemia (1,6,7). Children are considered to be highly susceptible to the effects of air pollution due to the immaturity of their immune system, the potential for developmental disruption, greater amount of time spent outdoors and, therefore, higher exposure levels, and a relatively high volume of air exchange relative to body mass (8,9). In fact, outdoor air pollution consistently shows an adverse effect on childhood respiratory health, especially on asthma outcomes, with a total estimated health care cost (among 34 countries, including Canada) of approximately US$1.7 trillion in 2010 (10,11).
Asthma is one of the top 10 causes of years lost due to disability in male children worldwide (12). The effects of outdoor air pollution on asthma and other respiratory conditions have been the subject of study involving many adult and children populations in Canada and elsewhere. Air pollution levels in Canada are relatively low and most Canadian cities experience extreme low temperatures. Thus, Canadian studies offer a unique opportunity to examine the effects of more moderate doses of air pollution compared with those experienced in many other nations (13). In addition, Canada boasts one of the highest percentage of foreign-born citizens (14), being a society of mixed languages, cultures and genetic diversity. Recent findings suggest that the influence of genetic diversity on the population’s susceptibility to air pollution is an important factor that should be considered in this field (15). In 2007, a systematic review of air pollution and children’s health in Canada analyzed the results of epidemiological studies published between January 1989 and December 2004 (16). From 11 studies over a 15-year period, the review identified associations between respiratory health effects and at least some CAP measurements. These associations were, however, often weaker than those reported in studies conducted in other countries. This was believed to be due to the lower levels of air pollution in Canada, the lower number of hours spent outdoors during the colder Canadian winters, as well as reduced levels of outdoor air pollution infiltrating into homes, which could act to reduce personal exposure to outdoor air pollution.
The objective of the present study was to conduct a comprehensive systematic review of the literature reporting the effects of outdoor air pollution on the respiratory health of children in Canada. We focused on the literature published during the past 10 years to update the previous review, identify new findings on types of associations between air pollutants and childhood respiratory health, and evaluate differences in those associations across Canadian cities.
METHODS
An a priori systematic literature review protocol was developed. The research question addressed in the present review was: what is the effect of outdoor air pollution exposure on respiratory conditions in Canadian children? Respiratory conditions included respiratory symptoms, lung function measurements and the use of health services due to respiratory disease.
Search strategy
To increase sensitivity, the search strategy used in the previous review (16) was modified. Specifically, four electronic bibliographic databases (MEDLINE, CINAHL, Scopus and CAB abstracts) were searched (Appendix 1). In general, databases were searched with a combination of terms and derived key words including variation to the following basic terms: “air pollution”, “outdoor air pollution”, “asthma”, “respiration disorders”, “respiratory health”, “respiratory symptoms”, “child”, “adolesc”, “youth” and “Canada”. In the MEDLINE search, the names of 16 specific Canadian cities were included to increase search sensitivity. The search strategy was not restricted by language or publication type. A Google Scholar web search was conducted and references of relevant studies were scanned and selected as a complementary search strategy.
Study selection and data extraction
The criteria for selecting studies included: any observational analytic design; publication date between January 1, 2004 and November 30, 2014; population included and reported data for children up to 18 years of age residing in Canada; exposure(s) included any nonbiological outdoor air pollutant whether measured directly or inferred (ie, by proximity to roadways), with special interest in the CAP (CO, NO2, SO2, O3, and PM10 and PM2.5); and outcomes included health services use (HSU), lung function measurement or self-reported respiratory symptoms. Studies that included a subset or cohort of Canadian children in which the data for the Canadians were not presented separately were excluded. Two reviewers (LR-V and AM) independently screened the identified articles’ titles and abstracts to select the articles for full review, and reviewed citations that were found to be potentially relevant for inclusion. A third reviewer (AO-V) resolved disagreement. Articles selected for full review were screened in a second round to confirm that the inclusion criteria were met. Agreement was measured using kappa (κ) statistics. Data extraction was performed by two reviewers (LR-V and AM) and summarized in standardized tables.
Quality assessment
Study quality was assessed using the Newcastle-Ottawa Scale (NOS), which uses an eight-item rating system to evaluate the method of selection of participants, the exposure/outcome assessment, and comparability among study groups (17). Comparability was evaluated by controlling for potential confounders in terms of study design and the type of health effects under evaluation. The Cochrane Non-Randomized Studies Methods Working Group recommends the use of the NOS, although the study of its psychometric properties remains in progress (18). The NOS quality scores range from 0 to 9 (0 to 4 = poor quality; 5 to 7 = moderate quality; 8 to 9 = high quality). The NOS has specific formats for cohort and case-control studies only. The cohort study form was used to evaluate noncohort longitudinal studies and the case control form to evaluate case-crossover and cross-sectional studies. Two reviewers (LR-V and AM) independently performed the quality assessment of the included studies and disagreements were discussed and resolved by consensus.
Data analysis
Descriptive results of the included studies are provided. While quantitative analyses using pooled measures and random effect models were planned, they could not be conducted due to heterogeneity among study populations (children’s age), outcomes and study designs. Kappa statistics and 95% CIs were generated using Stata version 11.1 (StataCorp, USA).
RESULTS
Search results
The present review follows the PRISMA recommendations (19). As indicated in Figure 1, the systematic search identified 162 studies. After removing duplicates, initial screening with inclusion/exclusion criteria and full-text review, 27 studies were included. Studies were excluded for a variety of reasons, primarily because they did not report results on Canadian children. Reviewer agreement was substantial for identifying potentially relevant studies (disagreement 22%; κ=0.73 [95% CI 0.70 to 0.75]) and excellent for identifying included/excluded studies in full-text review (κ=0.91 [95% CI 0.78 to 1.00]).
Figure 1).
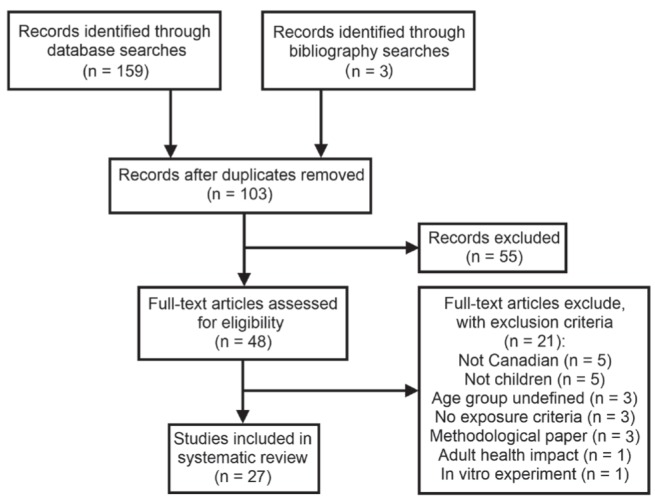
PRISMA flow diagram for selection of studies
Study characteristics
The 27 studies that met the selection criteria varied in design, study location, number and type of air pollutants considered, age of children population and respiratory outcome. Tables 1 and 2 summarize the main characteristics and results of the individual studies grouped according to respiratory outcome examined (20–46).
TABLE 1.
Characteristics and results of included studies with health services use outcomes
| Reference; study location; and study period | Study design; study population and size | Pollutants (mean or median levels*) and methods assessing exposure | Respiratory outcome | Study findings | Adjustment for confounding factors |
|---|---|---|---|---|---|
| Lin et al, 2004 (34); Vancouver area; 1987–1998 | Time series study; hospitalizations of 6–12 year olds; from BC Linked Health Dataset (n=3822) | Mean CO (960), SO2 (4.77), NO2 (18.65), O3 (28.02), PM10 (NS), PM2.5 (NS) from 1995–1998; from monitoring stations | Hospitalizations for asthma | RR of asthma hospitalizations in low SES group associated with: NO2 (male, 1-day lag): 1.16 (95% CI 1.06–1.28), NO2 (male 4-day lag): 1.18 (95% CI 1.03–1.34), SO2 (female 4-day lag): 1.17 (95% CI 1–1.37), and SO2 (female 6-day lag): 1.19 (95% CI 1–1.42) | Sex, temperature, relative humidity, SES, day of the week |
| Yang et al, 2004 (46); Greater Vancouver; 1995–1999 | Case-crossover, case-control and time-series analyses; first hospital admissions of 0–3 year olds, excluding birth-related admissions (n=1610) | Mean CO (700), O3 (14.3), NO2 (16.8), SO2 (3.5), PM10 (13.3) and PM2.5 (7.7); from local monitors | Hospitalizations for respiratory disease (including asthma) | OR of respiratory hospitalizations associated with 3-day lag mean and max PM10-2.5: 1.22 (95% CI 1.02–1.48) and 1.14 (95% CI 0.99–1.32), respectively; time-series analysis gave weaker associations | Sex, SES, day of the week, season, study year, season and influenza hospitalizations |
| Lin et al, 2005 (35); Toronto; 1998–2001 | Case-crossover design; hospitalizations of 0–14 year olds (n=6782) | Mean PM10 (20.41), PM2.5 (9.59), PM10-2.5 (10.86), CO (1160), SO2 (4.73), NO2 (24.54), O3 (38.06); from monitoring stations | Hospitalization for respiratory infections | OR of hospitalizations for 6-day average exposure to: PM10-2.5: boys 1.15 (95% CI 1.02–1.3), girls 1.18 (95% CI 1.01–1.36); PM10: boys 1.25 (95% CI 1.01–1.54); NO2: girls 1.31 (95% CI 1.05–1.63); PM2.5, O3 and SO2 showed no associations | Sex, temperature, pollutant interactions and seasonality |
| Luginaah et al, 2005 (37); Windsor; 1995–2000 | Time series and case-crossover design; hospitalizations 0–14 year olds (n=1602) | Mean NO2 (38.9), SO2 (27.5), CO (1300), PM10 (50.6), TRS (8), and coefficient of haze (0.5); from monitoring stations | Hospitalizations for respiratory disease | Time Series RR: NO2: female 2-day lag: 1.19 (95% CI 1.002–1.411); SO2: female Current-Day: 1.11 (95% CI 1.011–1.221); CO: female 2-day lag: 1.07 (95% CI 1.001–1.139); Cross-over design OR: CO: female current day, 2-day lag and 3-day lag: 1.15 (95% CI 1.006–1.307), 1.19 (95% CI 1.020–1.379) and 1.22 (95% CI 1.022–1.459) | Temperature, sex, humidity, barometric pressure, seasonality |
| Dales et al, 2006 (25); 11 of the largest Canadian cities; 1986–2000 | Time series study; hospitalizations of 0–27 day olds (n=8586) | Mean NO2 (21.8), SO2 (4.3), CO (1.0), O3 (17.0), and PM10 (NS); from monitoring stations (population weighted average) | Hospitalizations for respiratory disease | The percentage of variation for IQR increase for all gasses combined was 9.61% (95% CI 4.52–14.7); individually: O3: 2.67 (95% CI 0.98–4.39); NO2 2.48 (95% CI 1.18–3.8); SO2: 1.41 (95% CI 0.35–2.47); CO: 1.3 (95% CI 0.13–2.49) | Long-term temporal trends, day of week effects, weather variables, other gases and PM10 |
| Villeneuve et al, 2007 (45); Edmonton; 1992–2002 | Case-crossover design (time stratified); ED visits of 2–14 year olds (n=20,392) | Summer/winter median PM10 (22.0/19.0), PM2.5 (7.0/7.3), CO (600/900), SO2 (2.0/3.0), NO2 (17.5/28.5), O3 (38.0/24.3); from monitoring stations | ED visits for asthma | Positive association were observed in warm season and higher in 2–4 years: OR 5-day average: NO2 1.50 (95% CI 1.31–1.71), CO 1.48 (95% CI 1.27–1.72), PM2.5: 1.16 (95% CI 1.04–1.28) and PM10: 1.16 (95% CI 1.05–1.28); For 5–14 years: OR 5-day average: NO2: 1.13 (95% CI 1.02–1.24), O3: 1.14 (95% CI 1.05–1.24), PM2.5: 1.10 (95% CI 1.02–1.17), PM10: 1.14 (95% CI 1.06–1.22); many of the 1- and 3-day lags were also significant during the warm season for various pollutants | Temperature, relative humidity, season, aeroallergens, and ED visits for influenza |
| Szyszkowicz et al, 2008 (43); Edmonton; 1992–2002 | Longitudinal study; 0–10 years ED visits (n=18,891) | Mean/median CO (700/600), NO2 (21.9/19.7), SO2 (2.6/2.2), O3 (18.6/17.8), PM10 (22.6/19.4), PM2.5 (8.5/6.2); from monitoring stations | ED visits for asthma | Many positive associations were observed in the warm season; the higher percentage increase for each pollutant was: CO (2-day lag) male: 17.7% (95% CI 10.2–25.6), NO2 (2-day lag) male: 19.2% (95% CI 11.4–27.6), O3 (same day) female: 17.8% (95% CI 7.1–29.5), PM10 (2-day lag) male: 7.4% (95% CI 3.1–11.9), PM2.5 (same-day) female: 7.7% (95% CI 5.2–10.3), O3 (1-day lag), PM10 (same-day), and PM2.5 (2-day lag) showed positive variations for some age/sex/season combinations | Sex, temperature, relative humidity, day of the week |
| Burra et al, 2009 (20); Toronto; 1992–2001 | Longitudinal study; family physician and specialists service claim records for 1–17 year olds (n=1,146,215) | Mean SO2 (9.7), NO2 (39.2), O3 (33.3) and PM2.5 (17.9); from monitoring stations | Asthma physician visits | RR for pollutants by SES quintiles (Q1/Q5) were: SO2: 1.005 (95% CI 1.000–1.010), NO2: 1.002 (95% CI 0.995–1.008), and PM2.5: 1.006 (95% CI 0.997–1.015); low SES groups had higher RR in SO2 and PM2.5 models | SES, temperature, barometric pressure, 24 h mean relative humidity, day of the week |
| Smargiassi et al, 2009 (41); Montreal (Quebec); 1996–2004 | Case-crossover design (time stratified); 2–4 year olds living near a refinery (n=1579) | Daily peak mean SO2 (east/southwest of refineries) using monitoring stations (23.8/12.8); and AERMOD dispersion model (19.2/16.0) | Asthma ED visits or hospital admissions | OR for same-day ED visits: 1.10 (95% CI 1.00–1.22), and hospital admissions: 1.42 (95% CI 1.10–1.82) | Temperature, relative humidity, regional/background air pollutant levels |
| Henderson et al, 2011 (30); Southeast corner of BC 92 days: July to September 2003 | Cohort study; Residents at the southeast area of BC with a reliable geocodable residential address in health databases; included newborns (n=281,711; 21.6% <20 years old) | Mean PM10 during days of smoke coverage from forest fires; Comparison of two methods: TEOM monitoring stations (45.9); and CALPUFF dispersion model (44.2) | Respiratory or cardiovascular physician visits and hospital admissions | OR change due to 10 μg/m3 increase in total PM10 (TEOM) in respiratory hospital admissions: 1.05 (95% CI 1.00–1.10), and cardiovascular admissions: 1.00 (95% CI 0.96–1.05) | Age, sex, SES |
| Lavigne et al, 2012 (32); Windsor (Ontario); 2002–2009 | Case-crossover design (time stratified); 2–14 year olds hospitalized for asthma (n=3728) | Mean summer/winter SO (2.1/1.7), NO2 (9.8/7.4), CO (400/300), PM2.5 (7.1/7.4), O3 (13.2/26.0); from monitoring stations | Asthma ED visits | Increased risk of warm season asthma ED visit of 19%, 25% and 36% associated with increases in IQR of 1-day lagged exposure to SO2, NO2 and CO levels, respectively | Daily number of influenza ED visits, temperature and relative humidity. |
| Lewin et al, 2013 (33); Shawiningan (Quebec); 1999–2008 | Case-crossover design (time stratified); hospitalized 0–4 year olds living near aluminium smelter (n=396) | Exposure calculated by: % of hours/day each residence was downwind of the smelter; and daily mean SO2 (6.3) and PM2.5 (13.5) from monitoring station | Hospitalization for asthma or bronchiolitis | OR of hours downwind of a smelter on same-day hospitalization of 2–4-year-old children: 1.27 (95% CI 1.03–1.56), and PM2.5 exposure: 1.22 (95% CI 1.03–1.11) | Average daily wind direction and speed |
| To et al, 2013 (44); Ontario; 2003–2006 | Longitudinal study; All Ontario residents with asthma registered at the (OASIS) database | Canada 2003/2004/2005/2006) mean AQHI (3.87/3.64/3.83/3.34), NO2 (NS), O3 (NS), and PM2.5 (NS) measures; from monitoring stations | Asthma-attributed hospitalizations, ED and outpatient visits | RR for 1-unit increase in the AQHI by same-day outpatient visits: 1.056 (95% CI 1.053–1.058) and hospitalization: 1.0256 (95% CI 1.053–1.058), and 2-day lag ED visits: 1.013 (95% CI 1.010–1.017) | Age group, season, residence area, and year |
| Szyszkowicz et al, 2014 (42); Windsor (Ontario); 2004–2010 | Case-crossover design (time stratified); ED visits for 2–14 year olds; (n=2151) | AQHI for Canada; hourly AQHI calculations, NO2, O3, and PM2.5 measures from two monitoring stations | Asthma ED visits | Positive and statistically significant associations were observed for same-day and 9-day lag exposure (both OR 1.11 [95% CI 1.01–1.21]) and 3-day lag exposure (OR 1.09 [95% CI 1.00–1.18]) | Ambient temperature, relative humidity and daily counts of ED visits for influenza |
Parts per billion for gasses, μg/m3 for particulate matter (PM). AQHI Air Quality Health Index; BC British Columbia; CO Carbon monoxide; ED Emergency department; IQR Interquartile range; NO2 Nitrogen dioxide; NS Not stated; O3 Ozone; OASIS Ontario Asthma Surveillance Information System; RR Relative risk; SES Socioeconomic status; SO2 Sulphur dioxide; TEOM Tapered element oscillating microbalance; TRS Total reduced sulphur
TABLE 2.
Characteristics and results of included studies with respiratory symptoms, lung function measures and incidence of asthma diagnosis outcomes
| Author (reference), year; location; study period | Study design; study population and size | Pollutants (mean or median levels*) and methods assessing exposure | Respiratory outcome | Study findings | Adjustment for confounding factors |
|---|---|---|---|---|---|
| Pouliou et al (38), 2008; Hamilton (Ontario); 1978–1985 | Reanalysis of cohort study; 9–12 year olds identified by postal code (n=1164) | TSP measured at 28 monitoring stations; exposures assigned to postal code using Kriging and LUR; mean of five stations (station/Kriging/LUR): 58.64/55.69/58.57 | FEV1, FVC, MEF, PF; survey used for respiratory symptoms | OR for association between TSP and wheezy: 1.01 (95% CI 0.99–1.02), Cold usually goes to chest: 1.01 (95% CI 1.005–1.019), and having a cough: 1.56 (95% CI 1.35–1.80); coefficient for lung measures: FEV1 (0.002), FVC (0.003), MEF75% (0.002), and FEF25–75% (0.099); LUR performed better than Kriging | Height, sex, previous hospitalizations, medical history of siblings, SES, parental smoking, use of gas for cooking and heating |
| Dales et al (27), 2008; Windsor (Ontario); study period not stated | Cross-sectional; 9–12-year-old school children (n=2328) | Roadway density and mean/median annual SO2 (5.39/5.28), NO2 (13.58/13.15), PM10-2.5 (7.25/7.27), PM2.5 (15.62/15.42), and black smoke (0.75/0.75 10−5/m); LUR model assigned exposures at postal code level | FVC, FEV1, eNO | 3.9% eNO increase associated with 1 μg/m3 increase in PM2.5; each km of road within 200 m associated with 6.8% increase in eNO, and 0.70% decrease in FVC | Previous respiratory infection, asthma medication usage, cigarette exposure and house pets |
| Chen et al (22), 2008; Vancouver (British Columbia); study period not reported | Longitudinal study for symptoms and lung function measures; 9–18-year-old asthmatic children (n=73) | NO2 concentrations; LUR model assigned exposures for the entire study area at a resolution of 10 m. | Daily PEF measurements and asthma symptoms reported by parents and children (diary). Baseline inflammatory markers measured | Chronic exposure to traffic and psychosocial stress interact to predict both biological and clinical outcomes in children with asthma. The effect of psychosocial stress was more evident among children living in lower-pollution areas. | Asthma severity, asthma medication use, and demographic characteristics (age, sex, ethnicity, time of year of study visit). |
| Dales et al (26), 2009; Windsor (Ontario); September 2004 | Cross-sectional; 6–14-year-old school children (n=12,693) | Exposure to roadways; total length of local roadways within 200 m radius around postal code of each house | Respiratory symptoms and illnesses (cough, wheezing, chest illness) | OR comparing the highest to the lowest exposure (roadway density) quintiles significant for wheeze: 1.23 (95% CI 1.07–1.41) and wheeze with dyspnea: OR 1.27 (95% CI 1.05–1.52), but not cough, chest illness or asthma; general OR lowest versus others quintiles was 1.08 (95% CI 1.012–1.149) | Age, sex, parental history of asthma and allergy, parental education, household income, home smokers, number of bedrooms, siblings, pets, stove type, visible indoor moulds |
| Dales et al (24), 2009; Windsor (Ontario); October to December 2005 | Cross-sectional; 9–14-year-old asthmatic school children (n=182) | Mean PM2.5 (7.8), NO2 (19.1), O3 (14.1), O3max (27.3), and SO2 (6.0); from monitoring stations | Acute (daily) FEV1 | IQR increase (6.0 μg/mm3) in the previous 24 h mean PM2.5 associated with a 0.54% (95% CI 0.06–1.02) decrease in bedtime FEV1 | Daily mean temperature, relative humidity, day of the week, number of hours spent on outdoor activities, sex, and study period |
| Sahsuvaroglu et al (39), 2009; Hamilton (Ontario); 1994–1995 | Cross-sectional; 6–7 and 13–14-year-old school children (n=1467) | Air pollution in 4 ways: distance from roadways 50 m-100 m; mean interpolated surfaces of O3 (20.12), SO2 (5.81), PM10 (20.90), NOX (31.77) from monitoring stations; Krigged NO2 (15.36) surface based on a network of 100 monitors; and LUR for NO2 (14.84) derived from the same monitoring network | Asthma symptoms | Effects were observed for the association of asthma without hay fever and NO2 LUR in 6–7 and 13–14-year-old girls (OR 1.86 [95% CI 1.59–2.16]) and 13–14-year-old girls (OR 2.98 [95% CI 0.98–9.06]); refined exposure models produced the most robust associations | Income, dwelling value (Census), smoking data available, % houses built pre-1946, rate of repair of housing to account for mould and damp conditions (from Census 1996), Deprivation Index by using principal components analysis for income, education and employment variables |
| Liu et al (36), 2009; Windsor (Ontario); 4 weeks: October to December 2005 | Longitudinal repeated measures study; 9–14-year-old asthmatic children (n=182) | 1-day/2-day/3-day median SO2 (4.5/5.0/5.6), NO2 (19.8/18.3/18.3), O3 (13.0/14.1/14.0), and PM2.5 (6.5/6.6/6.9); from two fixed monitors in study area | Pulmonary function, airway oxidative stress and inflammation in asthmatic children | IQR increases in 3-day average SO2, NO2, and PM2.5 were associated with decreases in forced expiratory flow with changes between −2.8% and 3.1%. SO2, NO2 and PM2.5 were associated with increases in TBARS but not FeNO, 8-isoprostane or interleukin 6; O3 was not associated with health outcomes | Testing period, interactions of pollutant concentrations with sex and use of inhaled corticosteroids |
| Clark et al (23), 2010; British Columbia Southwest; 1999–2003 | Case-control population-based study; children born in 1999 and 2000 in the study location; (n=3482) | IDW/LUR modelled exposures for NO, NO2, CO, O3, PM10, PM2.5, black carbon, SO2, and road proximity In utero and in first year of life based on monitor data (see source data) | Asthma diagnosis (incidence) | Highest OR for asthma diagnosis was associated with increased early life exposures to CO (100 μg/m3 increase OR 1.10; 95% CI 1.06–1.13), NO (10 μg/m3 increase OR 1.08; 95% CI 1.04–1.12) and NO2 (10 μg/m3 increase OR 1.12; 95% CI 1.07–1.17); PM10, SO2, black carbon and proximity roads and pollution point sources also showed significant associations with asthma diagnosis | Age, sex, birth weight, gestational age, maternal smoking, maternal age, # siblings, intention to breast-feed, First Nation status, income quintiles and maternal education quartiles by dissemination area to approximate SES |
| Cakmak et al (21), 2012; Windsor (Ontario); February to June (year NS) | Cross-sectional; 9–11-year-old school children; (n=2328) | Annual volume of vehicles within 200 m radius of child’s neighbourhood; used sensors to measure traffic counts and turning movements | Respiratory symptoms; FCV, FEV1, and eNO | OR associated with IQ increase of turning movements: chest congestion 1.20 (95% CI 1.06–1.35), FEV1 decline 1.84% (95% CI 0.007–3.61); OR associated with IQ increase in traffic counts: FVC decrease 0.68% (95% CI 1.32–0.03); effects on asthmatic children were larger; traffic measures had association with effect on eNO | Ethnic background (Caucasian versus other), smokers at home, pets at home, acute respiratory illness in past 2 weeks, medication for wheezing/asthma in last 2 weeks, month or the year |
| Deger et al (28), 2012; Montreal (Quebec); April to July 2006 | Cross-sectional; 6 month to 12 year olds exposed to refinery emissions (n=482) | Yearly mean ambient SO2 exposures in children (with active asthma/no active asthma/poor asthma control/active asthma with acceptable control/no asthma/controlled asthma) (1.68/1.55/1.90/1.61/1.56); SO2 exposure levels estimated using AERMOD dispersion model | Symptoms of active asthma and poor asthma control | Adjusted PR for IQR increase of SO2 exposure on increased: active asthma: 1.14 (95% CI 0.94–1.39); poorly controlled asthma: 1.39 (95% CI 1.00–1.94) | Age, sex, parental history of asthma or rhinitis or eczema, household income, maternal educational level, house tobacco smoke; for SO2 models longitude, latitude, emission temperature, height and exit velocity for each vent and stack used |
| Johnson et al (31), 2013; Windsor (Ontario); 2004–2005 | Longitudinal repeated measures study; asthmatic 10–13 year olds; (n=45) | Daily outdoor house levels of NO2 and PM2.5; Comparison of home monitoring data and LUR temporally refined models based on monitoring site data | FEV1 and PEF | Daily home NO2 associated with 7%–8% decrement in FEV1/IQR; LUR temporally adjusted models better predicts spatial and temporal variability in lung function models in asthmatic children | Environmental tobacco smoke, height and weight; home: temperature and relative humidity |
| Dell et al (29), 2014; Toronto (Ontario); June to September 2006 | Cross-sectional; School children grades 1–2 (5–9 year olds); (n=1497) | Cumulative NO2 exposures; estimations using LUR and IDW models including lifetime addresses (birth, moving, daycare/school and current addresses) | Current and lifetime asthma and wheeze | In children with other allergic disease, birth, cumulative and 2006 NO2 were associated with lifetime asthma and wheeze; no or weaker effects were seen without other allergic diseases | Presence of other allergic diseases was tested for effect modification; other variables include ETS and other house-hold exposures, family history of asthma and demographics. |
| Smargiassi et al (40), 2014; Montreal (Quebec); 10 days between 2009–2010 | Longitudinal repeated measures; asthmatic 8–12 year olds living near two oil refineries; (n=72) | Daily personal monitoring of SO2, NO2, PAHs, VOCs and PM2.5 concentrations (data not shown); passive samplers for gases and real time monitor for PM2.5 (NS) | FVC, FEV1 and FEF25–75% | No consistent associations were observed with PM2.5, NO2 and benzene; suggestion of small decrease in respiratory function with PAHs (FVC: −9.9 mL per IQR PAH [95% CI −23.4 to 3.7]) | Within-subject serial correlation, medication use, parent’s or caregiver’s education, ethnicity, temperature, relative humidity, age, height, sex, and the design variable month of study |
Parts per billion for gasses, μg/m3 for particulate matter (PM) and total suspended particles (TSP). CO Carbon monoxide; ED Emergency department; eNO Exhaled nitric oxide; ETS Environmental tobacco smoke; FEF25–75% Forced expiratory flow between 25% and 75% of the forced vital capacity (FVC); FeNO Fractional exhaled nitric oxide; FEV1 Forced expiratory volume in 1 s; IDW Inverse distance weighted; IQ Interquartile; IQR IQ range; LUR Land use regression; MEF75%, maximum expiratory flow after 75% of FVC has been exhaled; NO Nitrogen monoxide; NO2 Nitrogen dioxide; NS Not stated; O3 Ozone; PAH Polycyclic aromatic hydrocarbon; PEF Peak expiratory flow; PF Pulmonary function; PR Prevalence ratio; RR Relative risk; SES Socioeconomic status; SO2 Sulphur dioxide; TBARS Thiobarbituric acid reactive substances; VOC Volatile organic compound
Fifteen of the 27 studies included data from Ontario (20,21,24,26,27,29,31,32,35–39,42,44), five used British Columbia (BC) data (22,23,30,34,46), four used Quebec data (28,33,40,41), two used Alberta data (43,45) and one study used data from 11 Canadian cities (25). At least one of the two Ontario cities – Windsor and Hamilton – were represented in 13 of the articles analyzed. The most common study designs used were longitudinal (n=7), cross-sectional (n=7) and case-crossover (n=6). All studies included children <15 years of age, except for one that included children up to 17 years of age (20). Twelve (44%) studies received funding support from provincial or federal government agencies. Eighteen studies focused on exposures to at least one of the CAP, two used proximity to roads as the exposure source, two used Air Quality Health Index (AQHI) as the tested exposure, and four examined CAP as well as proximity to roads or industrial facilities. One study measured exposure to total suspended particles (TSP) in Hamilton, and other polycyclic aromatic hydrocarbon (PAH) and volatile organic compounds in Montreal (Quebec). Of the 23 studies tracking CAP or TSP, the majority (n=13) used fixed ambient air monitoring stations to assess exposures, two modelled exposures, seven used a combination of measurements and models, and one used personal monitoring devices. Regarding respiratory outcomes, 14 studies relied on health services use for respiratory conditions as the main health outcome (Table 1), while five used lung function measures based on spirometry; four used self-report of respiratory symptoms; three used a combination of lung function measures and symptoms; and one calculated incidence of asthma diagnosis (23) (Table 2).
Quality assessment
The overall methodological quality assessment of the studies was moderate, with a mean (± SD) NOS score of 6.04±1.3 from a maximum score of 9. Figure 2 summarizes the methodological quality of the studies based on the NOS items. All studies clearly defined outcomes and most (96.3%) of the studies controlled for potential confounding variables; however, the nonexposed group definition, the follow-up criteria (especially for noncohort longitudinal studies), and the report of nonparticipation (in cross-sectional studies) were not met in >50% of the articles.
Figure 2).
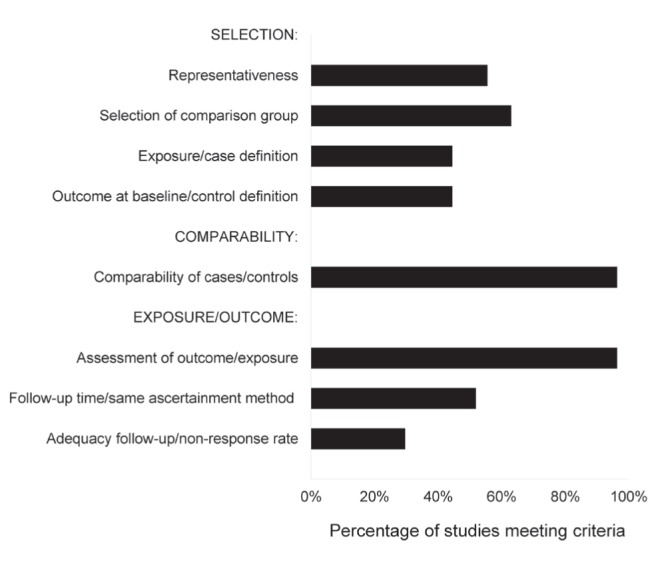
Quality assessment of the 27 included studies using the Newcastle-Ottawa Scale, which assess three main groups of criteria consisting of a total of eight items. All criteria are assessed in a binary fashion (0 or 1), except for ‘comparability of cases/controls’, which was scored as 0, 1 or 2. Percentages indicate the total score of all the articles in the indicated categories out of the total possible score
HSU as a result of air pollution exposure
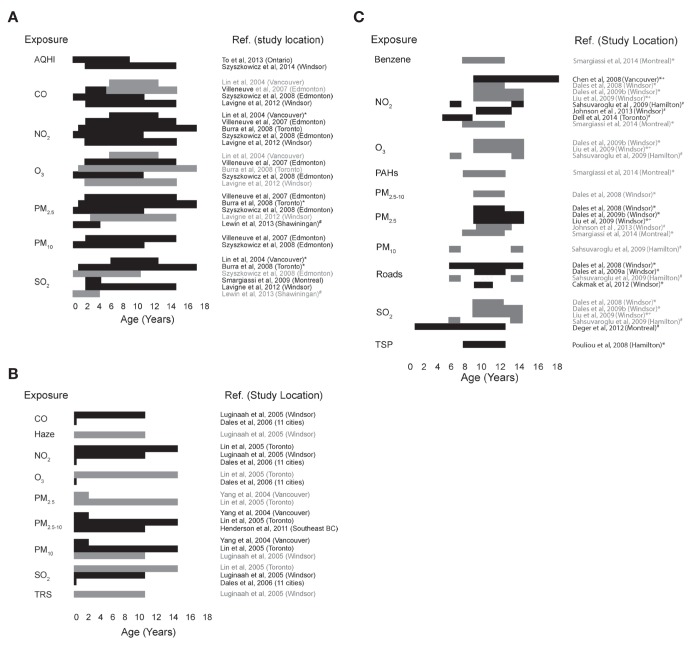
Nine studies focused on HSU for the treatment of asthma symptoms. A variety of age ranges and pollutants had positive associations with asthma-related HSU (Figure 3A). Higher adverse effects were reported consistently during the warm season in different cities. The highest percentage increase of emergency department (ED) visits for asthma (up to 36%) was reported in one-day lag exposures to CO, SO2 and NO2 in Windsor during the warm season (32), and the highest percentage increase of asthma hospitalization (up to 42%) was reported in children exposed to SO2 in refinery areas in Montreal (41). Studies examining NO2 produced the most consistent results, showing a positive association with HSU at different ages (from 0 to 17 years of age). There was also evidence that the effect of NO2 was exacerbated among female children of low socioeconomic status (20,34). Two pollutants (CO, O3) gave conflicting results among studies; however, it is important to note that the studies generally differed according to age and city studied, as well as the study period. Two studies using the AQHI as an air pollution indicator also showed positive associations with HSU.
Figure 3).
Respiratory health outcomes according to air pollutant and children’s age range. The age groups of children tested by each reference were plotted for each air pollutant measure tested. Bars indicate either a statistically significant (P<0.05, black) or nonsignificant (P>0.05, grey) association between the indicated pollutant and the health effect, for each age group studied by the indicated study. A The incidence of emergency department (ED) visits and hospitalizations for asthmatic symptoms and pollution exposure. *Effect was present or stronger in populations with low socioeconomic status. #ED visits and hospitalizations for bronchiolitis were also included as relevant health outcomes in the study. B Associations between pollution exposure and health services use for conditions other than asthma. C Lung function measurements and symptoms of affected lung function (eg, wheezing and other asthma-like symptoms) were tested for associations with differing levels of pollutant exposure. *Lung function was measured; +Lung inflammation was measured;#Asthmatic symptoms were measured. AQHI Air Quality Health Index; CO Carbon monoxide; NO2 Nitrogen dioxide; O3 Ozone; PAHs Polycyclic aromatic hydrocarbons; PM2.5/PM10 Particulate matter size ≤2.5 μm/≤10 μm in aerodynamic diameter; SO2 Sulphur dioxide; TRS Total reduced sulphur; TSP Total suspended particles
Five studies examined HSU for general respiratory conditions (which could include, but were not limited to, asthma) and infections. As with HSU for asthma, several positive associations were demonstrated (Figure 3B). In this case, CO, NO2 and PM2.5–10 were positively associated with HSU for respiratory ailments. Conflicting results were demonstrated for O3, PM10 and SO2, depending on the city and age of the children studied.
Air pollution effects on lung function and asthma symptoms/diagnosis
A variety of pollutants was tested for an association with increased asthma symptoms (AS) or decreased lung function (LF) (Figure 3C). LF was typically assessed using forced vital capacity (FVC) and/or forced expiratory volume in 1 s (FEV1) measures. The most consistent null effects were reported for O3, when either LF or AS were examined in children, in Windsor and Hamilton. Associations with reduced LF were also apparent for PAH (Montreal) and TSP (Hamilton). No associations with reduced lung function were seen with benzene (Montreal) or PM2.5–10 (Windsor); and no increased AS were apparent with increased PM10 exposure (Hamilton). While proximity to roadways had no association with AS in Hamilton, it did show an effect on LF in three Windsor-based studies (21,26,27). Inconsistent results were observed for NO2, PM2.5 and SO2, even though the contradictory studies often examined similar health effects and age groups in the same cities. For NO2, most LF data failed to demonstrate an association (Montreal and Windsor), while one showed the opposite (Windsor), as did one study using AS (Hamilton). There was no clear pattern in the PM2.5 data, with three Windsor articles identifying effects on LF and/or inflammation, and two from Montreal and Windsor showing no effect on LF. For SO2, four studies using either LF, AS, or LF and inflammation failed to demonstrate an effect in Hamilton and Windsor, while a single study in Montreal detected an association with AS. Two studies showed effect modification of NO2 on asthma symptoms by chronic psychosocial stress and other allergic disease (20,27).
Only one study examined increases in asthma diagnosis, as a consequence of exposure to CAPs, wood smoke and black carbon (soot), or industrial and road proximity in children <5 years of age from southwest BC (23). Positive associations were seen with CO, NO, NO2, PM10, SO2, black carbon and industrial proximity (Table 2).
DISCUSSION
The present systematic review summarizes the evidence available from epidemiological studies exploring the association of outdoor air pollution on Canadian children’s respiratory in the past 10 years. From 2004 to 2014, 27 new studies were identified; all but one (40) reconfirm the adverse effects of outdoor air pollution on respiratory symptoms, lung function and HSU at different CAP concentrations, almost all of which were below United States and Canadian (available only for PM2.5 and O3) standards (47). The present review also identified that the increase in respiratory-related ED visits and hospitalizations were demonstrated in higher proportions than the outpatient visits, and that those effects are even higher in places near industrial facilities or refinery areas in Windsor and Montreal, respectively. The findings showed more consistent associations of adverse respiratory outcomes for traffic-related exposures of PM and NO2, especially related to health services use. Some studies also report differential effects of gases and particles on female and socially disadvantaged children.
Our review updates a similar study covering 1989 to 2004 (16), enabling us to compare publications and describe trends in the research related to the effect of air pollution on Canadian children over the past 25 years. There are differences, mainly in terms of the number of publications, type of study designs, exposure measurement and study locations. Compared with publications from 1989 to 2004, the publications in the past decade were: more than twofold more frequent, over a shorter period of time studied; conducted mainly in Windsor and Hamilton rather than in Toronto and Vancouver; most commonly used cross-sectional, longitudinal and case-crossover study designs rather than time-series analysis; and increasingly introduced air pollutant exposure assessment using model-based small area estimations (eg, land-use regression models), in addition to data from fixed ambient air monitoring stations. These changes could be explained by several factors, such as the increase in funding for the study of environmental-related health conditions in Canadian children (48), the increased access to high quality administrative data, growing societal concern for the potential health effects of industrial development around cities (12 of 27 studies between 2004 and 2014 were supported by provincial or federal government agencies), and the development of epidemiology, spatial and statistical methods applicable to air pollution research (49).
Conversely, similarities across time included the preference for reporting asthma-related outcomes and the use of CAP concentrations as the metric to assess outdoor air pollution exposure. These similarities can be explained by the persistent high prevalence of asthma in Canadian children (50), the availability of high-quality administrative health data, especially for acute asthma-related conditions (51) and detailed CAP data from the air quality monitoring surveillance systems in many densely populated Canadian cities (52).
National air pollution surveillance data have shown that the concentration of CAP gases decreased slightly over time in Canada (53), and mean Canadian CAP levels are lower than those in most of the major cities of the world (54–58). Even at current Canadian levels, however, they are associated with adverse health effects in children, as well as cardiovascular, respiratory and gastrointestinal effects in adults (mainly linked to SO2 and PM) (59,60). Moreover, several of the studies referenced herein suggest heterogeneous effects of the current levels of gases and particles on children according to sex, socioeconomic status and seasonality; however, none of them included an analysis of potential mechanisms explaining those differences, which may vary across populations (61).
Limitations
The methodological quality of the studies included in the present review was relatively homogeneous, with a mean ‘moderate quality’ score according to the NOS tool. This ‘moderate’ score is lower than expected for most included articles because the NOS tool is designed only for classic cohort or case-control studies. Thus, we believe that properly assessing the quality of observational studies related to environmental health remains challenging.
To avoid selection bias in the present review, two independent reviewers conducted the screening and selection processes. Although efforts to undertake meta-analyses failed due to the high qualitative heterogeneity in the included studies, qualitative summary tables and graphs were developed to examine trends. Having more homogeneous studies in terms of children’s age in studies would allow quantitative analysis in future reviews. Another limitation of the review was that unpublished studies in the formal scientific literature were not identified; therefore, there may be a chance of publication bias. However, the included studies showed both positive and null effects of different CAP for different cities. In fact, the common mixture of positive and null effects in many studies may be explained by the fact that air pollutants effects differ not only according to type of pollutant (alone or in combination), but also by the different physical and sociodemographic conditions of the places and populations under study. Finally, the scope of the present review was limited to the childhood population and the results and conclusions may be not generalizable to adults, even in Canada.
CONCLUSIONS
The present review provides researchers, clinicians and environmental health authorities with a current summary of the evidence linking the adverse effects of outdoor air pollution to children’s respiratory health in Canada. Further studies should fill knowledge and methodological gaps that are related but not restricted to: deepening the understanding of the ‘why’ of the differences in the observed adverse effects for some pollutants and socioeconomic conditions across cities; exploring the combined effect of various air pollutants; expanding the study of the health effects of non-CAP air toxicants that are emitted in Canada, such as PAH or volatile organic compounds; strengthening the advances in epidemiological, spatial, statistical and social analysis as applied to air pollution studies, aiming for a more integrated approach between the physical and social environment; and developing and validating a tool for assessing the methodological quality of observational studies commonly used in environmental health studies, other than cohort and case control studies.
Acknowledgments
The authors thank Mrs Maria Tan, library consultant at the John W Scott Health Sciences Library at University of Alberta for her support in defining the specific search strings. Author contributions: LR-V designed the study, undertook the literature searches, study assessment, data extraction and analysis. AM conducted study assessment, data extraction and analysis. AO-V contributed as third reviewer in the selection process and contributed to the data interpretation. BR contributed to the study design and data interpretation. All authors contributeed to writing and editing the manuscript, and approved the final version for publication.
APPENDIX 1. OVID MEDLINE, CINAHL Plus, Scopus and CAB search strategies
|
Ovid MEDLINE sequence and terms
| |
| 1. | Air Pollution/ |
| 2. | air pollutants/ or gasoline/ or hydrogen sulfide/ or particulate matter/ or sulfur dioxide/ or vehicle emissions/ |
| 3. | (“Air pollution” or “air pollutant”).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 4. | (“ambient air pollution” or “outdoor air pollution”).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 5. | 1 or 2 or 3 or 4 |
| 6. | asthma/ or bronchitis/ or respiration disorders/ |
| 7. | (“respiratory health” or “asthma” or “respiratory condition*”).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 8. | (“respiratory symptoms” or “wheeze*” or “respiratory function” or “pulmonary function”).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 9. | 6 or 7 or 8 |
| 10. | Child/ |
| 11. | (“child*” or “adolesc*” or “teen*” or “youth” or “pediat*”).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 12. | 10 or 11 |
| 13. | canada/ or alberta/ or british columbia/ or manitoba/ or new brunswick/ or “newfoundland and labrador”/ or northwest territories/ or nova scotia/ or nunavut/ or ontario/ or prince edward island/ or quebec/ or saskatchewan/ or yukon territory/ |
| 14. | (“Canada” or “Vancouver” or “Edmonton” or “Calgary” or “Victoria” or “Regina” or “Saskatchewan” or “Winnipeg” or “Toronto” or “Hamilton” or “Windsor” or “Mississauga” or “Montreal” or “Halifax” or “Ottawa” or “Kingston” or “London”).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 15. | 13 or 14 |
| 16. | 5 and 9 and 12 and 15 |
| 17. | limit 16 to yr=”2004 -Current” |
|
CINAHL Plus sequence and string terms*
| |
| 1. | Air pollut* |
| 2. | (Respirat* OR Asthm* OR Pulmon*) |
| 3. | 1 and 2 |
| 4. | (Child* OR adolescen*) |
| 5. | 3 and 4 |
|
Scopus exact string terms
| |
| TITLE-ABSKEY | |
| (AIR POLLUT* AND (RESPIRAT* OR ASTHM* OR PULMON*) AND (CHILD* OR ADOLESCEN*) AND CANAD*) | |
| AND SUBJAREA | |
| (MULT OR AGRI OR BIOC OR IMMU OR NEUR OR PHAR OR MULT ORMEDI OR NURS OR VETE OR DENT OR HEAL) | |
| AND PUBYEAR > 2003 | |
| CAB abstracts | |
| (“air pollut*” AND “respirat*” AND “child*” AND “Canada”). | |
| Indexes=CAB Abstracts Timespan=2004–2014 | |
Limiters - Published Date: 20040101–20140231; Geographic Subset: Canada; Age Groups: All Child
Footnotes
FUNDING: The study was supported by the Emergency Medicine Research Group (EMeRG) affiliated with the Department of Emergency Medicine, and by the Department of Pediatrics, University of Alberta. Dr Rodriguez-Villamizar is supported by COLCIENCIAS Colombia. Adam Magico’s postdoctoral research is supported by a Hair Massacure grant to Dr Osornio-Vargas. Dr Rowe’s research is supported by a Canadian Institutes of Health Research through a Tier I Canada Research Chair in Evidence-based Emergency Medicine from the Government of Canada (Ottawa, Ontario)
REFERENCES
- 1.Brunekreef B, Holgate ST. Air pollution and health. Lancet. 2002;360:1233–42. doi: 10.1016/S0140-6736(02)11274-8. [DOI] [PubMed] [Google Scholar]
- 2.(WHO) WHO Air pollution 2013 < www.who.int/topics/air_pollution/en/> (Accessed April 5, 2013).
- 3.Van Donkelaar A, Martin RV, Brauer M, et al. Global estimates of ambient fine particulate matter concentrations from satellite-based aerosol optical depth: Development and application. Environ Health Perspect. 2010;118:847–55. doi: 10.1289/ehp.0901623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nemmar A, Holme Ja, Rosas I, Schwarze PE, Alfaro-Moreno E. Recent advances in particulate matter and nanoparticle toxicology: A review of the in vivo and in vitro studies. Biomed Res Int. 2013;2013:279371. doi: 10.1155/2013/279371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.International Agency for Research on Cancer . Outdoor air pollution a leading environmental cause of cancer deaths. 2013. Press Release No. 221. < www.iarc.fr/en/media-centre/iarcnews/pdf/pr221_E.pdf> (Accessed January 17, 2014). [Google Scholar]
- 6.Schwartz J. Air pollution and children’s health. Pediatrics. 2004;113:1037–43. [PubMed] [Google Scholar]
- 7.Kappos AD, Bruckmann P, Eikmann T, et al. Health effects of particles in ambient air. Int J Hyg Env Heal. 2004;207:399–407. doi: 10.1078/1438-4639-00306. [DOI] [PubMed] [Google Scholar]
- 8.Gilliland F, McConnell R, Peters J, Gong H. A theoretical basis for investigating air pollution and children’s respiratory health. Environ Health Perspect. 1999;107(Suppl 3):403–7. doi: 10.1289/ehp.99107s3403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dixon JK. Kids need clean air: Air pollution and children’s health. Fam Community Heal. 2002;24:9–26. doi: 10.1097/00003727-200201000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Holguin F. Traffic, outdoor air pollution, and asthma. Immunol Allergy Clin North Am. 2008;28:577–88. viii–ix. doi: 10.1016/j.iac.2008.03.008. [DOI] [PubMed] [Google Scholar]
- 11.Organization for Economic Co-operation and Development . The cost of air pollution: Health impacts of road transport. Paris: OECD Publishing; 2014. [Google Scholar]
- 12.World Health Organization . In: The global burden of disease: 2004 update. World Health Organization, editor. Geneva: 2008. [Google Scholar]
- 13.Stieb D, Liu L. Air quality impacts on health. In: Taylor E,, McMIllan A, editors. Air Quality Management: Canadian Perspectives on a Global Issue. Dordrecht: Springer; 2014. p. 388. [Google Scholar]
- 14.Evans L. Diversity in Canada: an overview. Canadian Immigrant. 2013 < http://canadianimmigrant.ca/guides/moving-to-canada/diversity-in-canada-an-overview> (Accessed February 13, 2015). [Google Scholar]
- 15.Esposito S, Tenconi R, Lelii M, et al. Possible molecular mechanisms linking air pollution and asthma in children. BMC Pulm Med BMC Pulmon Med. 2014;14:31. doi: 10.1186/1471-2466-14-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Koranteng S, Osornio-Vargas A, Buka I. Ambient air pollution and children’ s health: A systematic review of Canadian epidemiological studies. Paediatr Child Health. 2007;12:225–33. [PMC free article] [PubMed] [Google Scholar]
- 17.Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scales (NOS) for assessing the quality of nonrandomized studies in meta-analyses. Ottawa: University of Ottawa; < wwwohrica/programs/clinical_epidemiology/oxford.asp> (Accessed March 12, 2014). [Google Scholar]
- 18.Higgins JP, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.2. [updated September 2009] The Cochrane Collaboration; 2009. < www.cochrane-handbook.org> (Accessed January 5, 2013). [Google Scholar]
- 19.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Burra TA, Moineddin R, Agha MM, Glazier RH. Social disadvantage, air pollution, and asthma physician visits in Toronto, Canada. Environ Res. 2009;109:567–74. doi: 10.1016/j.envres.2009.03.004. [DOI] [PubMed] [Google Scholar]
- 21.Cakmak S, Mahmud M, Grgicak-Mannion A, Dales RE. The influence of neighborhood traffic density on the respiratory health of elementary schoolchildren. Environ Int. 2012;39:128–32. doi: 10.1016/j.envint.2011.10.006. [DOI] [PubMed] [Google Scholar]
- 22.Chen E, Schreier HM, Strunk RC, Brauer M. Chronic traffic-related air pollution and stress interact to predict biologic and clinical outcomes in asthma. Environ Health Perspect. 2008;116:970–5. doi: 10.1289/ehp.11076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Clark NA, Demers PA, Karr CJ, et al. Effect of early life exposure to air pollution on development of childhood asthma. Environ Health Perspect. 2010;118:284–90. doi: 10.1289/ehp.0900916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dales R, Chen L, Frescura AM, Liu L, Villeneuve PJ. Acute effects of outdoor air pollution on forced expiratory volume in 1 s: A panel study of schoolchildren with asthma. Eur Respir J. 2009;34:316–23. doi: 10.1183/09031936.00138908. [DOI] [PubMed] [Google Scholar]
- 25.Dales RE, Cakmak S, Doiron MS. Gaseous air pollutants and hospitalization for respiratory disease in the neonatal period. Environ Health Perspect. 2006;114:1751–4. doi: 10.1289/ehp.9044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dales R, Wheeler AJ, Mahmud M, Frescura A-M, Liu L. The influence of neighborhood roadways on respiratory symptoms among elementary schoolchildren. J Occup Environ Med. 2009;51:654–60. doi: 10.1097/JOM.0b013e3181a0363c. [DOI] [PubMed] [Google Scholar]
- 27.Dales R, Wheeler A, Mahmud M, et al. The influence of living near roadways on spirometry and exhaled nitric oxide in elementary schoolchildren. Environ Health Perspect. 2008;116:1423–7. doi: 10.1289/ehp.10943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Deger L, Plante C, Jacques L, et al. Exposed to air stack emissions of sulphur dioxide from petroleum refineries in Montreal, Quebec: A cross-sectional study. Can Respir J. 2012;19:97–102. doi: 10.1155/2012/218957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dell SD, Jerrett M, Beckerman B, et al. Presence of other allergic disease modifies the effect of early childhood traffic-related air pollution exposure on asthma prevalence. Environ Int. 2014;65:83–92. doi: 10.1016/j.envint.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 30.Henderson SB, Brauer M, Macnab YC, Kennedy SM. Three measures of forest fire smoke exposure and their associations with respiratory and cardiovascular health outcomes in a population-based cohort. Environ Health Perspect. 2011;119:1266–71. doi: 10.1289/ehp.1002288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Johnson M, Macneill M, Grgicak-Mannion A, et al. Development of temporally refined land-use regression models predicting daily household-level air pollution in a panel study of lung function among asthmatic children. J Expo Sci Environ Epidemiol. 2013;23:259–67. doi: 10.1038/jes.2013.1. [DOI] [PubMed] [Google Scholar]
- 32.Lavigne E, Villeneuve PJ, Cakmak S. Air pollution and emergency department visits for asthma in Windsor, Canada. Can J Public Health. 2012;103:4–8. doi: 10.1007/BF03404060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lewin A, Buteau S, Brand A, Kosatsky T, Smargiassi A. Short-term risk of hospitalization for asthma or bronchiolitis in children living near an aluminum smelter. J Expo Sci Environ Epidemiol. 2013;23:474–80. doi: 10.1038/jes.2013.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lin M. Gaseous air pollutants and asthma hospitalization of children with low household income in Vancouver, British Columbia, Canada. Am J Epidemiol. 2004;159:294–303. doi: 10.1093/aje/kwh043. [DOI] [PubMed] [Google Scholar]
- 35.Lin M, Stieb DM, Chen Y. Coarse particulate matter and hospitalization for respiratory infections in children younger than 15 years in Toronto: A case-crossover analysis. Pediatrics. 2005;116:e235–40. doi: 10.1542/peds.2004-2012. [DOI] [PubMed] [Google Scholar]
- 36.Liu L, Poon R, Chen L, et al. Acute effects of air pollution on pulmonary function, airway inflammation, and oxidative stress in asthmatic children. Environ Health Perspect. 2009;117:668–74. doi: 10.1289/ehp11813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Luginaah IN, Fung KY, Gorey KM, Webster G, Wills C. Association of ambient air pollution with respiratory hospitalization in a government-designated “area of concern”: The case of Windsor, Ontario. Environ Health Perspect. 2004;113:290–6. doi: 10.1289/ehp.7300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pouliou T, Kanaroglou PS, Elliott SJ, Pengelly LD. Assessing the health impacts of air pollution: A re-analysis of the Hamilton children’s cohort data using a spatial analytic approach. Int J Environ Health Res. 2008;18:17–35. doi: 10.1080/09603120701844290. [DOI] [PubMed] [Google Scholar]
- 39.Sahsuvaroglu T, Jerrett M, Sears MR, et al. Spatial analysis of air pollution and childhood asthma in Hamilton, Canada: Comparing exposure methods in sensitive subgroups. Environ Health. 2009;8:14. doi: 10.1186/1476-069X-8-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Smargiassi A, Goldberg MS, Wheeler AJ, et al. Associations between personal exposure to air pollutants and lung function tests and cardiovascular indices among children with asthma living near an industrial complex and petroleum refineries. Environ Res. 2014;132:38–45. doi: 10.1016/j.envres.2014.03.030. [DOI] [PubMed] [Google Scholar]
- 41.Smargiassi A, Kosatsky T, Hicks J, et al. Risk of asthmatic episodes in children exposed to sulfur dioxide stack emissions from a refinery point source in Montreal, Canada. Environ Health Perspect. 2009;117:653–9. doi: 10.1289/ehp.0800010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Szyszkowics M, Kousha T. Emergency department visits for asthma in relation to the Air Quality Health Index: A case-crossover study in Windsor, Canada. Can J Public Health. 2014;105:e336–e341. doi: 10.17269/cjph.105.4539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Szyszkowicz M. Ambient air pollution and daily emergency department visits for asthma in Edmonton, Canada. Int J Occup Med Environ Health. 2008;21:25–30. doi: 10.2478/v10001-008-0002-3. [DOI] [PubMed] [Google Scholar]
- 44.To T, Shen S, Atenafu EG, et al. The air quality health index and asthma morbidity: a population-based study. Environ Health Perspect. 2013;121:46–52. doi: 10.1289/ehp.1104816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Villeneuve PJ, Chen L, Rowe BH, Coates F. Outdoor air pollution and emergency department visits for asthma among children and adults: a case-crossover study in northern Alberta, Canada. Environ Health. 2007;6:40. doi: 10.1186/1476-069X-6-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yang Q, Chen Y, Krewski D, Shi Y, Burnett RT, McGrail KM. Association between particulate air pollution and first hospital admission for childhood respiratory illness in Vancouver, Canada. Arch Environ Health. 2004;59:14–21. doi: 10.3200/AEOH.59.1.14-21. [DOI] [PubMed] [Google Scholar]
- 47.Environment Canada G Canadian ambient air quality standards. Canadian Environmental Protection Act. 2013 p. Sections 54–5. < www.ecgc.ca/defaultasp?lang=En&n=56D4043B-1&news=A4B2C28A-2DFB-4BF4-8777-ADF29B4360BD> (Accessed January 21, 2013). [Google Scholar]
- 48.Canadian Institutes of Health Research Human Development, Child and Youth Health strategic research priorities. IHDCYH Strategic Plan 2013-2017: Healthy Foundations of Life. 2011. p. 27. < www.cihr-irsc.gc.ca/e/documents/ihdcyh_strategic_plan__2013-2018-en.pdf> (Accessed January 20, 2014).
- 49.Duncan T. Statistical Methods in Environmental Epidemiology. New York: Oxford University Press Inc; 2009. [Google Scholar]
- 50.Garner R, Kohen D. Changes in the prevalence of asthma among Canadian children. Health Rep. 2008;19:45–50. [PubMed] [Google Scholar]
- 51.To T, Dell S, Dick PT, Cicutto L, et al. Case verification of children with asthma in Ontario. Pediatr Allergy Immunol. 2006;17:69–76. doi: 10.1111/j.1399-3038.2005.00346.x. [DOI] [PubMed] [Google Scholar]
- 52.Environment Canada Air Quality Monitoring Networks and Data < www.ecgc.ca/air-sc-r/defaultasp?lang=En&n=C87142DF-1> (Accessed January 21, 2014).
- 53.Environment Canada . 10 years of data from the National Air Pollution Surveillance (NAPS) Network, data summary from 1999 to 2008. Ottawa: 2013. p. 213. [Google Scholar]
- 54.Braga AL, Saldiva PH, Pereira LA, et al. Health effects of air pollution exposure on children and adolescents in Sao Paulo, Brazil. Pediatr Pulmonol. 2001;113:106–13. doi: 10.1002/1099-0496(200102)31:2<106::aid-ppul1017>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 55.Romieu I, Meneses F, Ruiz S, et al. Effects of air pollution on the respirtory health of asthmatic children living in Mexico city. J Respir Crit Care Med. 1996;154:300–7. doi: 10.1164/ajrccm.154.2.8756798. [DOI] [PubMed] [Google Scholar]
- 56.Millman A, Tang D, Perera FP. Air pollution threatens the health of children in China. Pediatrics. 2008;122:620–8. doi: 10.1542/peds.2007-3143. [DOI] [PubMed] [Google Scholar]
- 57.Baldasano JM, Valera E, Jiménez P. Air quality data from large cities. Sci Total Environ. 2003;307:141–65. doi: 10.1016/S0048-9697(02)00537-5. [DOI] [PubMed] [Google Scholar]
- 58.Gurjar BR, Butler TM, Lawrence MG, Lelieveld J. Evaluation of emissions and air quality in megacities. Atmos Environ. 2008;42:1593–606. [Google Scholar]
- 59.Jerrett M, Burnett RT, Brook J, et al. Do socioeconomic characteristics modify the short term association between air pollution and mortality? Evidence from a zonal time series in Hamilton, Canada. J Epidemiol Community Health. 2004;58:31–40. doi: 10.1136/jech.58.1.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Villeneuve PJ, Johnson JY, Pasichnyk D, Lowes J, Kirkland S, Rowe BH. Short-term effects of ambient air pollution on stroke: Who is most vulnerable? Sci Total Environ. 2012;430:193–201. doi: 10.1016/j.scitotenv.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 61.O’Neill MS, Jerrett M, Kawachi I, et al. Health, wealth, and air pollution: Advancing theory and methods. Environ Health Perspect. 2003;111:1861–70. doi: 10.1289/ehp.6334. [DOI] [PMC free article] [PubMed] [Google Scholar]