Abstract
Angiotensin II (Ang II) and aldosterone contribute to hypertension, oxidative stress and cardiovascular damage, but the contributions of aldosterone during Ang II-dependent hypertension are not well defined because of the difficulty to assess each independently. To test the hypothesis that during Ang II infusion, oxidative and nitrosative damage is mediated through both the mineralocorticoid receptor (MR) and angiotensin type 1 receptor (AT1), five groups of Sprague-Dawley rats were studied: 1) control, 2) Ang II infused (80 ng/min × 28d), 3) Ang II + AT1 receptor blocker (ARB; 10 mg losartan/kg/d × 21d), 4) Ang II + mineralocorticoid receptor (MR) antagonist (Epl; 100 mg eplerenone/d × 21d) and 5) Ang II + ARB + Epl (Combo; × 21d). Both ARB and combination treatments completely alleviated the Ang II-induced hypertension, whereas eplerenone treatment only prolonged the onset of the hypertension. Eplerenone treatment exacerbated the Ang II-mediated increase in plasma and heart aldosterone 2.3- and 1.8-fold, respectively, while ARB treatment reduced both. Chronic MR blockade was sufficient to ameliorate the AT1-mediated increase in oxidative damage. All treatments normalized protein oxidation (nitrotyrosine) levels; however, only ARB and Combo treatments completely reduced lipid peroxidation (4-hydroxynonenal) to control levels. Collectively, these data suggest that receptor signaling, and not the elevated arterial blood pressure, is the principal culprit in the oxidative stress-associated cardiovascular damage in Ang II-dependent hypertension.
Keywords: aldosterone, angiotensin receptor blocker, cardiotrophin-1, hypertension, mineralocorticoid receptor, NADPH oxidase
Introduction
Angiotensin II (Ang II) is a major mediator of blood pressure and fluid homeostasis (1). When chronically elevated, Ang II can cause severe consequences such as hypertension and congestive heart failure (1, 2). Important cellular effects of Ang II include induction of oxidative stress and the generation of free radicals, which contribute to the activation of the fibrotic process and hypertrophy in the heart (1, 3, 4). Ang II exerts its pro-oxidative effects mainly through Ang II type 1 receptor (AT1)-mediated increase of reactive oxygen species (ROS; i.e., •O2− and H2O2) via activation of NADPH oxidase (Nox) (1, 5, 6). Specifically, Ang II up-regulates the most abundant Nox isoforms in the heart, Nox2 and Nox4, causing fibrosis, cardiac remodeling and hypertension, while AT1 antagonism provides cardioprotection (3, 6). Additionally, Ang II stimulates the release of aldosterone from the adrenal cortex, which in turn causes inflammation and oxidative damage (7–9). Although Ang II is considered a major mediator of hypertension and cardiovascular damage, it has been suggested that aldosterone promotes cardiac AT1 receptor density and Ang II-induced cardiac damage (10, 11). Subsequently, oxidative stress mediates lipid peroxidation and peroxynitrite production, exacerbating tissue remodeling and impaired cardiac function (12–14). Collectively, these results indicate that aldosterone may stimulate ROS production via up-regulation of Nox2/4 through AT1 activation (6, 15, 16).
Mineralocorticoid receptor (MR) antagonism offers cardioprotection against oxidative damage despite increasing intra-cardiac aldosterone during Ang II-dependent hypertension (3, 17–19). Data from the Randomized Aldactone Evaluation Study (RALES) revealed additional benefits of MR antagonism with spironolactone on overall mortality in patients with advanced heart failure treated with angiotensin-converting enzyme inhibitors (ACEi) and loop diuretics (20). Furthermore, recent reviews suggest that dual blockade of RAAS should not be used (21) or has limited effectiveness (22, 23) for treatment of hypertension, heart failure, nephropathy or other cardiovascular-related complications. However, the benefits of combination therapies including MR blockade are scarce.
Increasing evidence suggests that Ang II and aldosterone function interdependently to regulate vascular function and induce injury (24, 25). However, the combined benefits of AT1 and MR blockade on cardiac aldosterone and systemic oxidative/nitrosative stress in an Ang II-infused model of hypertension remain elusive. Therefore, using an Ang II-infused model of hypertension, we tested the hypothesis that Ang II and aldosterone induced oxidative/nitrosative damage is mediated through both the MR and AT1 receptors and independent of hypertension.
Results
Systolic Blood Pressure
To accurately ascertain the contribution of the Ang II-mediated increase of aldosterone on SBP, measures of SBP were performed by telemetry. After 28 days, Ang II infusion increased mean SBP 54% compared to control (Figure 1). ARB completely ameliorated the Ang II-induced hypertension within the first two days of treatment, demonstrating the effectiveness of both the Ang II infusion and ARB treatment (Figure 1). Eplerenone treatment prolonged the onset of hypertension between days 6 and 19 indicating that MR blockade was sufficient to partially inhibit the Ang II-induced increase in SBP, but could not prevent the ultimate manifestation of hypertension. When combined with ARB, the co-therapy completely ameliorated the Ang II-induced increase in SBP, but the effect was not additive.
Figure 1.
Mean (± SE) systolic blood pressure in control, angiotensin II (Ang II) infused, Ang II + angiotensin receptor blocker (ARB + Ang II) treated, Ang II + mineralocorticoid receptor blocker (Epl + Ang II) treated and Ang II + ARB + Epl (Combo + Ang II) treated groups. The arrow indicates when treatment was initiated (day 7) with diets containing the receptor blockers. * denotes significantly different (p<0.0001) from Control; ‡ denotes significantly different (p<0.05) between Ang II and Epl from day 6 to day 18
Body and Heart Masses
By day 28, Ang II decreased mean body mass (BM) by 15%, while both ARB and Combo increased mean BM similar to control levels (Table 1). However, Epl did not recover body mass. Ang II increased mean absolute heart mass by 26% and ARB and Epl reduced mean absolute heart mass to control levels (Table 1). Combo had no significant effect on mean absolute heart mass compared to control (Table 1). Ang II-infusion increased mean relative heart mass by 19%, while ARB and Combo ameliorated the increase suggesting that blockade of Ang II receptor alleviated the hypertrophy. Epl alone was not as effective as ARB at reducing the Ang II-associated hypertrophy (Table 1).
Table 1.
Mean (± SE) body mass, heart mass, and relative heart mass from control, angiotensin II (Ang II) infused, and Ang II + angiotensin receptor blocker (ARB) treated, Ang II + mineralocorticoid receptor (Epl) treated, and Ang II + ARB + Epl (Combo) treated Sprague-Dawley rats after 28 days.
| Control | Ang II | Ang II + ARB | Ang II + Epl | Ang II + Combo | |
|---|---|---|---|---|---|
| Body Mass (g) | 413 ± 9 | 352 ± 14* | 410 ± 7† | 356 ± 9 | 421 ± 9†§ |
| Heart Mass (g) | 1.23 ± 0.47 | 1.29 ± 0.04* | 1.14 ± 0.04† | 1.10 ± 0.03† | 1.25 ± 0.03† |
| Relative Heart Mass (g/100 g BM) | 0.31 ± 0.01 | 0.37 ± 0.01* | 0.28 ± 0.01† | 0.32 ± 0.01† | 0.28 ± 0.01† |
denotes significantly (p<0.05) different from Control;
denotes significantly (p<0.05) different from Ang II;
denotes significantly (p<0.05) different from ARB;
denotes significantly (p<0.05) different from Epl.
Plasma Renin Activity and Ang II Levels
To provide a more comprehensive assessment of ARB, MR blockade and combination treatments on circulating renin-angiotensin system (RAS) components, changes in plasma renin activity (PRA) and plasma Ang II were measured. Infusion of Ang II decreased mean PRA 3.6-fold compared to control, which was not altered by ARB (Table 2). Both eplerenone treatments reduced PRA further compared to Ang II and ARB (Table 2). Plasma Ang II was not significantly elevated by the Ang II infusion (Table 2). As expected, ARB was associated with a nearly 3-fold increase in plasma Ang II. Plasma Ang II was not significantly altered by either eplerenone treatments.
Table 2.
Mean (± SE) plasma renin activity (PRA), plasma Ang II, and plasma corticosterone from control, angiotensin II (Ang II) infused, and Ang II + angiotensin receptor blocker (ARB) treated, Ang II + mineralocorticoid receptor (Epl) treated, and Ang II + ARB +Epl (Combo) treated Sprague -Dawley rats after 28 days.
| Control | Ang II | Ang II + ARB | Ang II + Epl | Ang II + Combo | |
|---|---|---|---|---|---|
| PRA (ngAng I/ml/hr) | 2.9 ± 0.4 | 0.8 ± 0.3* | 0.6 ± 0.2 | 0.3 ± 0.1† | 0.2 ± 0.1‡ |
| Plasma Ang II (fmol/ml) | 45 ± 4 | 51 ± 7 | 145 ± 29† | 46 ± 5 | 53 ± 11 |
| Plasma corticosterone (ng/ml) | 100 ± 20 | 323 ± 23* | 94 ± 19† | 259 ± 12† | 360 ± 37* |
denotes significantly (p<0.05) different from Control;
denotes significantly (p<0.05) different from Ang II;
denotes significantly (p<0.05) different from ARB;
denotes significantly (p<0.05) different from Epl.
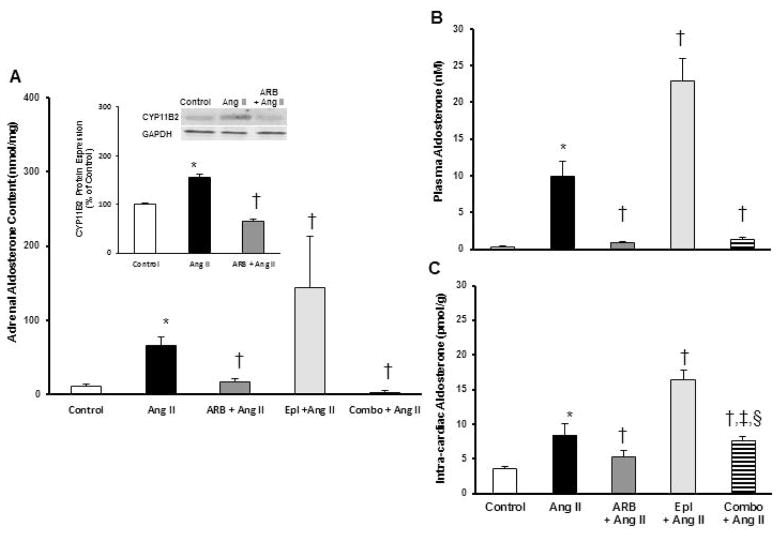
Adrenal Response and Heart Aldosterone Levels
To provide an integrated assessment of the adrenal response to ARB, Epl and combination treatments, changes in adrenal CYP11B2, adrenal aldosterone content, and plasma aldosterone and corticosterone (B) were measured. Mean adrenal CYP11B2 protein expression increased 1.5-fold in Ang II compared to control, and was significantly reduced with ARB treatment (Figure 2A). Mean adrenal aldosterone content increased 5-fold in Ang II compared to control, and adrenal aldosterone levels increased 2-fold in Epl compared to the Ang II infused group (Figure 2A). However, ARB and Combo decreased adrenal aldosterone content compared to Ang II suggesting that AT1 activation is an important regulating factor in the MR-mediated exacerbation of aldosterone during Ang II-infusion.
Figure 2.
Mean (± SE) A) adrenal aldosterone content, insert) adrenal aldosterone synthase (CYP11B2) protein content, B) plasma aldosterone concentration, and C) heart aldosterone content from control, angiotensin II (Ang II) infused, Ang II + angiotensin receptor blocker (ARB + Ang II) treated, Ang II + mineralocorticoid receptor blocker (Epl + Ang II) treated and Ang II + ARB + Epl (Combo + Ang II) treated groups. * denotes significantly different (p<0.05) from Control; † denotes significantly different (p<0.05) from Ang II; ‡ denotes significantly different (p<0.05) from ARB; § denotes significantly different (p<0.05) from Epl
Mean plasma aldosterone increased 27-fold with Ang II-infusion, while levels were significantly reduced in ARB and Combo; however, these levels remained significantly elevated compared to control (Figure 2B). In contrast to treatments including ARB, eplerenone treatment increased mean plasma aldosterone 2.5-fold above that in the Ang II-infused group (Figure 2B).
Mean plasma B increased over 3-fold with Ang II infusion, and this increase was completely ameliorated by ARB (Table 2). While eplerenone reduced the Ang II-induced levels of plasma B by 20%, these levels remained 2.5-fold greater than control. Interestingly, Combo did not reduce the Ang II-induced increase in plasma B that was observed in the individual treatments.
Ang II infusion increased mean heart aldosterone content 2.5-fold and ARB completely ameliorated this increase (Figure 2C). Similar to the effect on plasma aldosterone, eplerenone exacerbated the Ang II-induced increase in heart aldosterone content by an additional 82%, and Combo reduced heart aldosterone content to Ang II levels (Figure 2C).
Heart NADPH Oxidase Protein Expression
To assess the contributions of AT1 and MR activation on the potential for Nox-derived oxidant production during Ang II infusion, heart Nox2 and Nox4 were measured. Furthermore, to confirm the potential for increased Nox2 to generate ROS, the translocation of p47 was measured. Mean protein expression of Nox2 increased 70% in Ang II compared to control (Figure 3A). All treatments ameliorated the Ang II-induced increase below control levels (Figure 3A). The Ang II-induced increase in Nox2 was associated with a 60% increase in p47 translocation, and ARB reduced it approximately 40% (Figure 3B). Ang II infusion increased the mean protein expression of Nox4 by 1.5–fold compared to control, and all treatments reduced expression levels beyond control (Figure 3C).
Figure 3.
Mean (± SE) heart A) NADPH oxidase 2 (Nox2) content, B) p47 translocation, and C) Nox4 content from control, angiotensin II (Ang II) infused, Ang II + angiotensin receptor blocker (ARB + Ang II) treated, Ang II + mineralocorticoid receptor blocker (Epl + Ang II) treated and Ang II + ARB + Epl (Combo + Ang II) treated groups. * denotes significantly different (p<0.05) from Control; † denotes significantly different (p<0.05) from Ang II
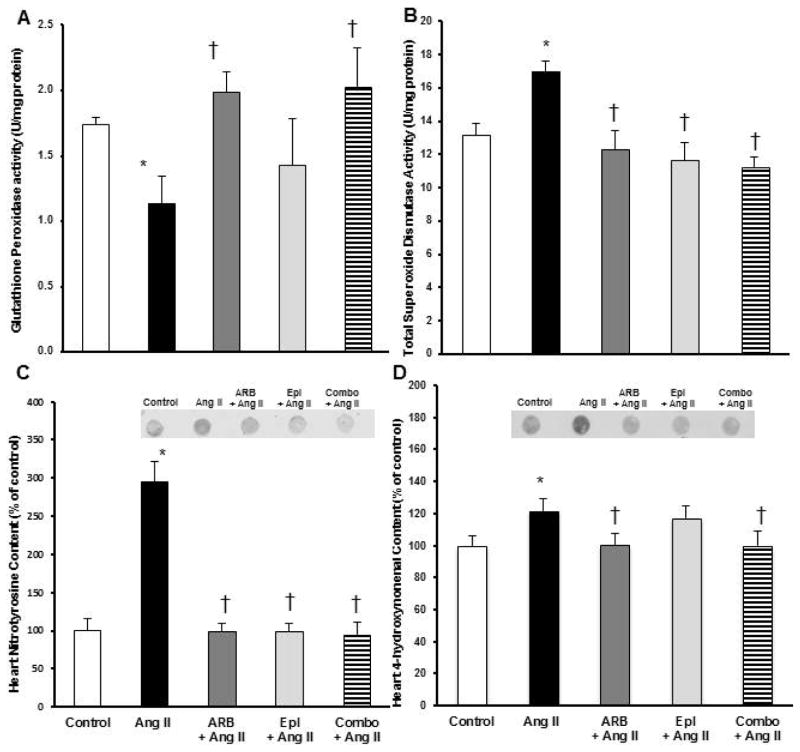
Heart Antioxidant Enzyme Activities & Oxidative Damage
To assess the contribution of MR activation on antioxidant (AO) enzyme activities in the heart of Ang II-infused animals, changes in GPx and total SOD activities were measured. Infusion of Ang II reduced mean GPx activity by 29% compared to control, while ARB and Combo recovered activity beyond control (Figure 4A). Mean SOD activity increased with Ang II infusion, and all treatments reduced the Ang II-induced increase (Figure 4B).
Figure 4.
Mean (± SE) heart A) glutathione peroxidase (GPx) activity, B) total superoxide dismutase (SOD) activity, C) nitrotyrosine (NT) content and D) 4-hydroxynonenal (4-HNE) content from control, angiotensin II (Ang II) infused, Ang II + angiotensin receptor blocker (ARB + Ang II) treated, Ang II + mineralocorticoid receptor blocker (Epl + Ang II) treated and Ang II + ARB + Epl (Combo + Ang II) treated groups. * denotes significantly different (p<0.05) from Control; † denotes significantly different (p<0.05) from Ang II
To assess the contribution of the eplerenone-induced exacerbation in plasma aldosterone to cardiac oxidative damage in response to changes in AO activities during Ang II infusion, changes in heart NT and 4-HNE content were measured. Ang II infusion increased mean heart NT levels 3-fold, and all treatments completely ameliorated this increase (Figure 4C). Ang II infusion increased heart 4-HNE 26% compared to control, and ARB and Combo alleviated this increase (Figure 4D). However, eplerenone alone was not effective at reducing the Ang II-mediated increase suggesting that AT1 activation contributes to a greater extent than MR activation to lipid peroxidation.
Urinary 8-Isoprostane & Angiotensinogen Excretion
To assess the contributions Ang II and aldosterone on systemic oxidative stress, changes in U8-isoV were measured. Ang II increased mean U8-isoV 2.5-fold compared to control, and ARB reduced U8-isoV by 57% of Ang II levels; however, eplerenone had no effect (Figure 5A). In combination, these treatments provided an additive benefit beyond both treatments individually, reducing U8-isoV by 84% of Ang II levels suggesting that the systemic lipid peroxidation is primarily mediated by the activation of AT1.
Figure 5.
Mean (± SE) A) urinary 8-isoprostane (8-iso) excretion and B) urinary angiotensinogen (Agt) excretion from control, angiotensin II (Ang II) infused, Ang II + angiotensin receptor blocker (ARB + Ang II) treated, Ang II + mineralocorticoid receptor blocker (Epl + Ang II) treated and Ang II + ARB + Epl (Combo + Ang II) treated groups. * denotes significantly different (p<0.05) from Control; † denotes significantly different (p<0.05) from Ang II; ‡ denotes significantly different (p<0.05) from ARB; § denotes significantly different (p<0.05) from Epl
Because UAgtV is a reliable marker of intrarenal RAS activation and elevated levels of kidney Ang II content (26), changes in UAgtV were determined to assess the contributions of elevated aldosterone on renal Ang II content, and the effects of aldosterone on Agt, in general. Ang II infusion increased UAgtV 79-fold, while ARB and Combo completely ameliorated this increase (Figure 5B). While eplerenone reduced UAgtV by 81% of Ang II levels, this level remained greater than control, ARB and Combo suggesting that AT1 activation contributes to Agt production to a much greater extent than that of MR.
Heart and Plasma Cardiotrophin-1 Levels
Because the effects of Ang II and aldosterone on heart and subsequent plasma levels of CT-1 are not well defined, the contributions of AT1 and MR activation on heart and plasma CT-1 levels were assessed. Intracardiac CT-1 protein expression increased 42% with Ang II infusion and was completely ameliorated by ARB and Combo (Figure 6A). Additionally, eplerenone reduced heart CT-1 25% from Ang II (Figure 6A). Mean plasma CT-1 increased 27% with Ang II infusion, and ARB, eplerenone and Combo treatments reduced levels to 81%, 88% and 84%, respectively, of control (Figure 6B).
Figure 6.
Mean (± SE) A) heart cardiotrophin-1 (CT-1) content and B) plasma CT-1 concentration from control, angiotensin II (Ang II) infused, Ang II + angiotensin receptor blocker (ARB + Ang II) treated, Ang II + mineralocorticoid receptor blocker (Epl + Ang II) treated and Ang II + ARB + Epl (Combo + Ang II) treated groups. * denotes significantly different (p<0.05) from Control; † denotes significantly different (p<0.05) from Ang II
Discussion
The classical actions of Ang II are as a vasoconstrictor and a stimulator of adrenal aldosterone, both of which can contribute to the development of hypertension when not regulated appropriately. Growing evidence indicates that excessive Ang II induces oxidative stress and inflammation, principal mediators in the manifestation of cardiovascular injury. Chronically elevated Ang II can have severe consequences on cardiovascular health such as persistent hypertension and congestive heart failure (10, 27, 28). However, the cellular mechanisms and contributing factors remain elusive. To this end, the present study contributes the following novel and important discoveries: (1) activation of AT1 contributes to a greater extent than that of MR to the Nox-mediated oxidative damage in the heart (and likely kidneys), (2) the benefits of simultaneous blockade of AT1 and MR on alleviating the oxidative damage are not additive, (3) the eplerenone-induced exacerbation of plasma and intra-cardiac aldosterone is not associated with inappropriately elevated Nox expression and markers of injury in the heart, and (4) despite the lack of amelioration of the Ang II-induced hypertension by chronic MR blockade, some benefits on alleviating pro-oxidant consequences were still observed.
Alleviation of AT1-mediated Cardiac Oxidative Damage
Our data show that Ang II-infusion increased plasma and heart aldosterone concentrations. Aldosterone increases the density of cardiac AT1 receptors in vascular smooth muscle cells, increasing the potential for AT1-mediated stimulation of ROS and therefore oxidative damage (11, 29, 30). The decrease in urinary 8-isoprostane by chronic treatment of AT1 blockade suggests that systemic oxidative stress is reduced, in agreement with earlier studies (1, 5). More importantly, despite the increased concentrations of plasma and heart aldosterone, chronic MR blockade prevents aldosterone-induced tissue damage, providing cardioprotection independent of a reduction in arterial blood pressure. This provides evidence that MR blockade was sufficient to ameliorate the aldosterone-mediated consequences suggesting that the exacerbated plasma aldosterone concentrations commonly associated with chronic MR blockade do not promote detrimental effects during the measurement period implemented in the present study. Combining ARB and MR blockade did not provide an additive effect on ameliorating the decrease in urinary 8-isoprostane suggesting that the levels reported here may represent some minimal threshold of effectiveness of the receptor blockade of both AT1 and MR. The changes in heart nitrotyrosine content were similar to those for urinary 8-isoprostane suggesting that the mechanisms inducing both oxidative and nitrosative stress in Ang II-infused hypertension are similar and primarily mediated by AT1.
Ang II activates NADPH oxidase (Nox) through AT1 and MR stimulating oxidative/nitrosative damage (1, 5, 15, 16). Nox2 generates superoxide (•O2−), a free radical that is scavenged by SOD and Nox4 produces hydrogen peroxide (H2O2), which is reduced by GPx. Additionally, aldosterone generates •O2− by increasing NADPH oxidase expression through MR activation (31). Our data suggest that Nox2 and Nox4 may be similarly stimulated by both Ang II and aldosterone or may reach maximal stimulation when both hormones are elevated and thus, blocking both receptors does not provide an additive effect. The present data support prior studies suggesting that the contributions of Ang II and aldosterone to oxidative damage are mediated through their respective receptors (29, 32). Independent blockade of these receptors can reduce oxidative/nitrosative damage regardless of blood pressure, and combining ARB and eplerenone did not additively reduce the oxidative damage. However, co-therapy is associated with reduced blood pressure, which in of itself may have additional benefits. This finding is intriguing because it has been shown that hypertension occurs independently of oxidative damage suggesting that Nox-induced cardiac damage is a result of the hypertension (33). Furthermore, in the aldosterone-infused, uninephrectomized rat, treatment with a MR antagonist (eplerenone), an ARB (candesartan) or a SOD mimetic (tempol) similarly reduced (approximately 14%) the SBP and aortic 4-HNE (lipid peroxidation) content, despite only the eplerenone treatment reducing the aortic mRNA levels of gp91phox (Nox2), p47phox (Nox2 subunit), and p22phox (Nox2 and Nox4 subunit) to control levels (32). The mRNA levels of gp91phox and p22phox were not different from the aldo-infused group after treatment with either ARB and SOD mimetic suggesting that the regulation of Nox2 (and possibly Nox4) mRNA expression is sensitive to MR mediation. This may be especially true because the changes in the mRNA expressions of these Nox subunits parallel the changes in Nox2 and Nox4 protein levels after eplerenone in the present study. The sensitivity may also be linked to levels of Ang II as aldosterone infusion was associated with reduced plasma Ang II (32), whereas in the present, ARB treatment was equally effective in reducing both Nox2 and Nox4 in the presence of elevated Ang II (infused). The parallel changes in p47 translocation with those of Nox2 protein suggest that elevated Nox2 was activated and had an increased potential for generating ROS.
The observed changes in Nox2 and Nox4 in the aorta (32) and the heart (present study) are consistent with those in the kidney as well. Chronic (4 wks) eplerenone treatment in aldosterone-infused, Dahl salt-sensitive rats on either a low- (0.3%; LS) or high-salt (8%; HS) diet effectively reduced renal Nox4 expression (regardless of diet) and urinary 8-isoprostane excretion (34) suggesting that MR contributes to the activation of both renal and cardiac Nox4. These reductions in renal Nox4 and U8-isoV in the eplerenone-treated groups were associated with a 25% decrease in SBP in LS and 15% decrease in HS (34), unlike the present study where eplerenone had virtually no effect on SBP suggesting that the AT1- and MR-mediated regulation of Nox proteins are independent of changes elevated arterial pressure. Nonetheless, the causal relationship between the regulation of Nox proteins and hypertension remains elusive (35).
Another important finding of the present study is the contribution of AT1 activation, and not MR activation, to impaired antioxidant defense mechanisms as indicated by the ability of ARB to recover antioxidant activity and reduce markers of oxidative damage. Nonetheless, another significant and novel contribution of the present study is that, despite the sustained increase in SBP, chronic MR blockade provided cardio-protective benefits consistent with that provided by ARB suggesting that the protective benefits of MR blockade are independent of elevated SBP.
Hypertrophic Effects and CT-1
Left ventricular hypertrophy (LVH) is commonly considered a consequence of hypertension and heart disease (36). Cardiotrophin-1, a member of the interleukin-6 family of cytokines, induces cardiomyocyte proliferation, and is elevated in the serum of patients with heart failure, myocardial infarction, and LVH during hypertension (37–39). In spontaneously hypertensive rats, AT1 antagonism inhibits the hypertrophic effects of CT-1 (30). Additionally, CT-1 may contribute to aldosterone-induced cardiac remodeling suggesting that MR blockade is a potential target for reduction of LVH (40). Inflammation and the generation of free radicals also contribute to the activation of the fibrotic process and hypertrophy (3, 4). In the present study, Ang II infusion increased relative heart mass while blockade of AT1 was able to prevent the Ang II-induced increase suggesting that Ang II induces hypertrophy via an AT1-mediated process. Blocking AT1 not only ameliorated the increase in relative heart mass, but also significantly improved it beyond control levels. While the cardiac hypertrophy was less in Epl than in Ang II and similar to control, the degree of hypertrophy was still greater than ARB suggesting that elevated aldosterone (plasma and/or heart) contributes minimally, at most, to cardiac hypertrophy. This is further supported by the finding that mean relative heart mass was similar between ARB and Combo suggesting that Ang II, largely independent of aldosterone, is primarily responsible for cardiac hypertrophy in this model. Additionally, Ang II infusion increased cardiac CT-1 protein expression associated with a parallel increase in circulating CT-1 levels. Although the three treatments reduced both plasma and cardiac CT-1 to control levels, the lack of an additive benefit of co-therapy suggests that levels were reduced to some minimum threshold as defined by control levels. The parallel decreases in CT-1 and cardiac hypertrophy suggest that CT-1 contributes to cardiac hypertrophy via activation of AT1 and/or MR, independent of arterial blood pressure.
Selective deletion of MR from macrophage cells in mice protects against fibrosis, and MR activation causes an inflammatory and oxidative stress (41, 42). In recent studies, MR blockade (eplerenone) reduced cardiac hypertrophy in salt sensitive models of hypertension, but was not effective in a low-salt Ren2 model (43, 44) suggesting that the effects of MR activation on cardiac hypertrophy are dependent on the conditions. Additionally, there is a strong association between aldosterone dysregulation and cardiometabolic disease, and MR antagonism improves vascular and endothelial function in obese human subjects with cardiac complications (45). Collectively, these data suggest that MR activation may play a measurable role in hypertrophy in the absence of elevated Ang II, but in the presence of inappropriately elevated Ang II, AT1 activation is primarily responsible for cardiac remodeling.
Blood Pressure Effects
The infusion of Ang II increased SBP and AT1 receptor antagonism reduced the elevated blood pressure to control levels soon after initiating the treatment, demonstrating the effectiveness of both the Ang II infusion and ARB treatment. Similar to previous studies, the anti-hypertensive effect of eplerenone was marginally significant (46). Subsequently, combination treatment did not provide additive benefit to AT1 blockade alone. These data demonstrate that during Ang II-mediated hypertension, AT1 activation is the principal contributing factor to elevated arterial blood pressure and the Ang II-induced increase in plasma aldosterone has little effect on SBP. Furthermore, the cellular oxidative pathways appear more sensitive to AT1 and MR mediation than to elevated arterial pressure.
Renal Injury
Angiotensinogen (Agt) is the precursor to Ang II, and its production is stimulated by Ang II (47). It is well established that ARB reduces intrarenal Ang II levels via a receptor-mediated processes (19, 48–51). Previous studies suggest that increased intrarenal Agt is a contributing factor to hypertension and excretion of Agt is an index of intrarenal production rate, renal injury, and subsequently, Ang II-dependent hypertension (52). Our data demonstrate that ARB is effective at reducing the Ang II-induced augmentation of urinary Agt. While ARB and co-therapy completely ameliorated the Ang II-mediated increase in UAgtV, eplerenone only partially (but significantly) suppressed this increase suggesting that the excretion, and likely generation, of Agt is primarily mediated by AT1 activation and that the aldosterone contribution is minimal at best. Thus, it is reasonable to suggest that heart Ang II levels would mimic the Agt levels, which are elevated by Ang II-infusion. While MR blockade prevented the increase in cardiac oxidative damage, it did not completely normalize UAgtV (marker of intrarenal injury) or U8-isoV (marker of systemic oxidative damage) suggesting that blockade of MR may be more effective in reducing cardiac injury than renal injury in an Ang II-infused model of hypertension.
Methods
All experimental procedures were reviewed and approved by the Institutional Animal Care and Use Committees of the University of California, Merced and Kagawa Medical University in accordance with the National Institutes of Health Guide for the Care and Use of Laboratory
Animals
Male Sprague-Dawley rats (200–225g; Clea Japan Inc., Tokyo, Japan and Charles River, Wilmington, MA) were randomly assigned to five experimental groups (n= 11–14/group): 1) control, 2) angiotensin II (Ang II; 80 ng/min; Sigma-Aldrich, Saint Louis), 3) Ang II + angiotensin receptor blocker (ARB; 10 mg losartan/kg/d; Merck & Co, Inc), 4) Ang II + mineralocorticoid receptor antagonist (Epl; 100 mg eplerenone/kg/d; Myoderm, Norristown, PA) and 5) Ang II + ARB + Epl (Combo). Control and Ang II groups were maintained on a normal rat chow diet (Research Diets, Inc., New Brunswick, NJ). The dosage of ARB is consistent with that used previously to successfully block Ang II (19, 53, 54). This dosage of eplerenone has been shown to result in optimal effective inhibition of MR in the rat (55), and the most widely used dosage in cardiovascular and renal studies in rats (16, 32, 34, 43, 56–62). ARB, eplerenone, or combo treatments were mixed in the food and food consumption rates were measured weekly to verify that treatment goals were met.
Telemetry, Ang II Infusion & Drug Treatments
Systolic blood pressure (SBP) was monitored daily (24-hour averages) by radio-telemetry to accurately and chronically evaluate the effectiveness of the Ang II infusion and the pharmacological treatments on blood pressure (19, 43, 46). Animals were provided 7 days of recovery following implantation of the bio-telemeters prior to initiating the study. After recovery, animals were anesthetized and subcutaneously implanted with an osmotic mini-pump (Durect Corp, Cupertino, CA; Model 2004) to infuse Ang II (Sigma-Aldrich, St. Louis, MO) for 28 days. SBP recording began the day after mini-pump implantation and discontinued the evening before dissections. Animals were maintained individually in metabolic cages in a temperature and light controlled room. Animals had unrestricted access to water and chow throughout the experiment. Infusion of Ang II began on day 1 of the study and animals were allowed 6 days to become hypertensive prior to drug treatments to mimic the conditions in which ARB and/or eplerenone would be prescribed. The diets containing ARB, eplerenone, or combo began on day 6 for a period of 21 days.
Dissections
On day 28, animals were weighed, decapitated and trunk blood collected into chilled vials containing 5 mM EDTA and protease inhibitor cocktail (PIC; Sigma, St. Louis, MO) for subsequent plasma measurements. The heart was removed, patted dry and weighed. The heart was sectioned and a uniform piece was weighed and immediately homogenized for aldosterone extraction. Additional pieces were flash-frozen in liquid nitrogen and stored at −80°C for later analyses. Whole adrenals were removed, weighed and homogenized in cold PBS for aldosterone extraction. A supplementary study was performed in control, Ang II and ARB animals (n = 5–6/group) to complement the adrenal aldosterone measures with analyses of aldosterone synthase (CYP11B2). In this additional study, adrenals were removed, cleaned, weighed and homogenized for quantification of CYP11B2 content by Western blot. Sufficient sample to measure and statistically assess the p47 translocation was only available for the control, Ang II and Ang II + ARB groups.
Western Blot Analyses
Relative changes in the protein content of adrenal aldosterone synthase (CYP11B2), NADPH oxidase (Nox) 2 and 4, translocation of p47 (Nox2 subunit), and heart cardiotrophin-1 (CT-1) were assessed by standard Western blot. Heart or adrenal segments were harvested as described above and were homogenized in RIPA buffer containing protease and phosphatase inhibitor cocktail (Pierce, Rockford, IL). Tissue homogenates were sonicated, centrifuged and the supernatant was stored at −80°C for later analyses. Total protein content was determined by Bradford assay (Bio-Rad Laboratories, Hercules, CA). Fifty micrograms of total protein were denatured in SDS-PAGE sample buffer. Proteins were transferred electrophoretically onto 0.45-μm nitrocellulose or PVDF membranes. Membranes were blocked with nonfat milk or LI-COR blocking solution (LI-COR Biosciences, Lincoln, Nebraska). Blots were incubated in primary antibodies against aldosterone synthase (Millipore, Billerica, MA), CT-1 (Abcam, Cambridge, MA), Nox2 (Santa Cruz Biotechnology, Santa Cruz, CA), Nox4 (Epitomics, Inc., Burlington, CA), and p47 (Millipore). Densities of blots were normalized against actin or GAPDH (Santa Cruz Biotechnology). The p47 blots were normalized to total protein staining by Ponceau-S red (63) because other proteins used for normalization changed with the treatments. Membranes were washed in TBS-T and incubated with secondary antibodies against the primary host. Nitrocellulose membranes were developed and visualized using a Kodak Image station (Model #440 CF, Boston, MA) and PVDF membranes were directly visualized using a Li-COR Odyssey CLx (Li-COR, Inc, Lincoln, Nebraska, USA). Blots were quantified using NIH ImageJ or Carestream Molecular Image software (Rochester, NY). The use of two visualization platforms was needed to optimize detection of specific proteins, but the quantification of a particular protein was performed on only one platform to maintain the integrity of the measurements.
Heart Antioxidant Enzyme Activities & Oxidative Stress Measurements
Glutathione peroxidase (GPx) and total superoxide dismutase (SOD) activities were measured from heart extracts using commercially available kits (Cayman Chemical) to quantify the Ang II- and aldosterone-mediated effects on antioxidant enzyme activities as previously described (64). The relative concentrations of heart 4-hydroxynonenal (4-HNE; Calbiochem, San Diego, CA, USA) and total nitrotyrosine (NT; Cayman Chemical) were measured by dot blot to assess the contribution of Ang II and aldosterone to oxidative damage in cardiovascular tissue as previously described (64).
Plasma analyses
Plasma renin activity (DiaSorin, Stillwater, MN, USA), Ang II (Phoenix Pharmaceuticals, Burlingame, CA), corticosterone (Millipore, Bellirica, MA) and plasma, adrenal and heart aldosterone (Siemens Healthcare Diagnostics, Los Angeles, CA) were measured using commercially available RIA kits. Cardiotrophin-1 (CT-1) was measured using a commercially available ELISA kit (US Biological, Swampscott, MA).
Urinalyses
Urine samples were diluted 1:8 or 1:10 prior to the measurement of total angiotensinogen (Agt; IBL America, Minneapolis, MN) or 8-isoprostanes (Cayman Chemical, Ann Arbor, MI) as previously validated (52). Urinary excretion (UAgtV or U8-isoV) of each variable was calculated as the product of daily urine volume (UV) and urinary concentration.
Statistics
Twenty-four hour averages of SBP were calculated and compared by repeated-measures by ANOVA to identify the changes in response to treatment. Mean (±SE) plasma, urine and heart measurements were compared by one-way analysis of variance. For all cases, a Fisher’s PLSD test was applied post hoc. The changes were considered significantly different at P < 0.05. Statistics were performed using Statistica (Statsoft, Inc, Tulsa, OK), Statview (SAS, Cary, NC, USA) and SYSTAT 13 (Systat Software, Inc, San Jose, CA, USA) software. All samples were analyzed in duplicate and run in a single assay with intra-assay percent coefficients of variability of <10% for all assays.
Acknowledgments
We thank Dr. N. Pelisch, Dr. J.A. Viscarra, Mr. A. Lee, Mr. R. Rodriguez and Mr. R. Martinez for their assistance with lab protocols and animal procedures. We also thank Dr. D. Pollock for reviewing an early draft of the manuscript. J.N.M. was supported by the USDA Minority Scholar Fellowship. J.P.V.-M. was supported by The University of California Institute for Mexico and The United States (UC MEXUS) and Mexico’s National Council for Science and Technology (CONACYT). R.M.O. was partially supported by NHLBI K02HL103787. Research was funded in parts by grants from NIH NIMHD T37MD001480 and NIH National Heart, Lung and Blood Institute R01HL091767 (R.M.O.).
Footnotes
Conflicts of Interest: None
References
- 1.Touyz RM. Intracellular mechanisms involved in vascular remodelling of resistance arteries in hypertension: role of angiotensin II. Experimental Physiology. 2005;90(4):449–55. doi: 10.1113/expphysiol.2005.030080. [DOI] [PubMed] [Google Scholar]
- 2.Virdis A, Neves MF, Amiri F, Viel EC, Touyz RM, Schiffrin EL. Spironolactone improves angiotensin-induced vascular changes and oxidative stress. Hypertension. 2002;40:504–10. doi: 10.1161/01.hyp.0000034738.79310.06. [DOI] [PubMed] [Google Scholar]
- 3.Bendall JK, Cave AC, Heymes C, Gall N, Shah AM. Pivotal Role of a gp91phox-Containing NADPH Oxidase in Angiotensin II-Induced Cardiac Hypertrophy in Mice. Circulation. 2002;105(3):293–6. doi: 10.1161/hc0302.103712. [DOI] [PubMed] [Google Scholar]
- 4.Wang HD, Johns DG, Xu S, Cohen RA. Role of superoxide anion in regulating pressor and vascular hypertrophic response to angiotensin II. Am J Physiol. 2002;282:H1697–H702. doi: 10.1152/ajpheart.00914.2001. [DOI] [PubMed] [Google Scholar]
- 5.Rajagopalan S, Kurz S, Munzel T, Tarpey M, Freeman GA, Griendling K, et al. Angiotensin II-mediated hypertension in the rat increases vascular superoxide production via membrane NADH/NADPH oxidase activation. Contribution to alterations of vasomotor tone. Journal of Clinical Investigation. 1996;97:1916–23. doi: 10.1172/JCI118623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Johar S, Cave A, Narayanapanicker A, Grieve D, Shah A. Aldosterone mediates angiotensin II-induced interstitial cardiac fibrosis via a Nox2-containing NADPH oxidase. FASEB journal : official publication of the Federation of American Societies for Experimental Biology. 2006;20(9):1546–8. doi: 10.1096/fj.05-4642fje. [DOI] [PubMed] [Google Scholar]
- 7.Iglarz M, Touyz RM, Viel EC, Amiri F, Schiffrin EL. Involvement of oxidative stress in the profibrotic action of aldosterone. Am J Hypertens. 2004;17(7):597–603. [PubMed] [Google Scholar]
- 8.Endemann DH, Touyz RM, Iglarz M, Savoia C, Schiffrin EL. Eplerenone prevents salt-induced vascular remodeling and cardiac fibrosis in stroke-prone spontaneously hypertensive rats. Hypertension. 2004;43(6):1252–7. doi: 10.1161/01.HYP.0000128031.31572.a3. [DOI] [PubMed] [Google Scholar]
- 9.Sophocles C, Grant RD, Frank MF, Christopher GS. Chronic aldosterone administration causes Nox2-mediated increases in reactive oxygen species production and endothelial dysfunction in the cerebral circulation. Journal of Hypertension. 2014;32(9):1815. doi: 10.1097/HJH.0000000000000259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Atlas SA. The Renin-Angiotensin Aldosterone System: Pathophysiological Role and Pharmacologic Inhibition. Journal of Managed Care Pharmacy. 2007;13(8 suppl S-b):S9–S20. doi: 10.18553/jmcp.2007.13.s8-b.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Robert V, Heymes C, Silvestre JS, Sabri A, Swynghedauw B, Delcayre C. Angiotensin AT(1) receptor subtype as a cardiac target of aldosterone - Role in aldosterone-salt-induced fibrosis. Hypertension. 1999;33:981–6. doi: 10.1161/01.hyp.33.4.981. [DOI] [PubMed] [Google Scholar]
- 12.Liu Y-H, Carretero O, Cingolani O, Liao T-D, Sun Y, Xu J, et al. Role of inducible nitric oxide synthase in cardiac function and remodeling in mice with heart failure due to myocardial infarction. American journal of physiology Heart and circulatory physiology. 2005;289(6):23. doi: 10.1152/ajpheart.00546.2005. [DOI] [PubMed] [Google Scholar]
- 13.Mehlhorn U, Krahwinkel A, Geissler HJ, LaRosee K, Fischer UM, Klass O, et al. Nitrotyrosine and 8-isoprostane formation indicate free radical-mediated injury in hearts of patients subjected to cardioplegia. J Thorac Cardiovasc Surg. 2003;125(1):178–83. doi: 10.1067/mtc.2003.97. [DOI] [PubMed] [Google Scholar]
- 14.Waugh RJ, Murphy RC. Mass spectrometric analysis of four regioisomers of F2-isoprostanes formed by free radical oxidation of arachidonic acid. Journal of the American Society for Mass Spectrometry. 1996;7(5):490–9. doi: 10.1016/1044-0305(95)00709-1. [DOI] [PubMed] [Google Scholar]
- 15.Sun Y, Zhang J, Lu L, Chen SS, Quinn MT, Weber KT. Aldosterone-induced inflammation in the rat heart: role of oxidative stress. American Journal of Pathology. 2002;161:1773–81. doi: 10.1016/S0002-9440(10)64454-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nishiyama A, Yao L, Nagai Y, Miyata K, Yoshizumi M, Kagami S, et al. Possible Contributions of Reactive Oxygen Species and Mitogen-Activated Protein Kinase to Renal Injury in Aldosterone/Salt-Induced Hypertensive Rats. Hypertension. 2004;43:841–8. doi: 10.1161/01.HYP.0000118519.66430.22. [DOI] [PubMed] [Google Scholar]
- 17.Gomez-Sanchez CE, Gomez-Sanchez EP. The protective side of the mineralocorticoid receptor. Endocrinology. 2012;153(4):1565–7. doi: 10.1210/en.2011-2184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chai W, Garrelds IM, de Vries R, Jan Danser AH. Cardioprotective Effects of Eplerenone in the Rat Heart. Hypertension. 2006;47(4):665–70. doi: 10.1161/01.HYP.0000205831.39339.a5. [DOI] [PubMed] [Google Scholar]
- 19.Conte D, Viscarra J, Nishiyama A, Ortiz RM. Chronic angiotensin receptor blockade suppresses intracardiac angiotensin II in angiotensin II-infused rats. Experimental Biology and Medicine. 2011 doi: 10.1258/ebm.2011.011159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. New England Journal of Medicine. 1999;341(10):709–17. doi: 10.1056/NEJM199909023411001. [DOI] [PubMed] [Google Scholar]
- 21.Steven GC. Current Status of Dual Renin Angiotensin Aldosterone System Blockade for the Treatment of Cardiovascular Diseases. The American Journal of Cardiology. 2010;105(6):849852. doi: 10.1016/j.amjcard.2009.11.044. [DOI] [PubMed] [Google Scholar]
- 22.Amber H, Ken M, Deborah M, Richard DdS. Renin Angiotensin Aldosterone System Blockade: Little to No Rationale for ACE Inhibitor and ARB Combinations. The American Journal of Medicine. 2011;124(1):1519. doi: 10.1016/j.amjmed.2010.07.021. [DOI] [PubMed] [Google Scholar]
- 23.Carlos MF. Addressing the theoretical and clinical advantages of combination therapy with inhibitors of the renin–angiotensin–aldosterone system: Antihypertensive effects and benefits beyond BP control. Life Sciences. 2010;86(9–10):289299. doi: 10.1016/j.lfs.2009.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Montezano AC, Callera GE, Yogi A, He Y, Tostes RC, He G, et al. Aldosterone and Angiotensin II Synergistically Stimulate Migration in Vascular Smooth Muscle Cells Through c-Src-Regulated Redox-Sensitive RhoA Pathways. Arteriosclerosis, thrombosis, and vascular biology. 2008;28(8):1511–8. doi: 10.1161/ATVBAHA.108.168021. [DOI] [PubMed] [Google Scholar]
- 25.Robert V, Heymes C, Silvestre J, Sabri A, Swynghedauw B, Delcayre C. Angiotensin AT1 receptor subtype as a cardiac target of aldosterone: role in aldosterone-salt-induced fibrosis. Hypertension. 1999;33(4):981–6. doi: 10.1161/01.hyp.33.4.981. [DOI] [PubMed] [Google Scholar]
- 26.Kobori H, Nishiyama A, Harrison-Bernard LM, Navar LG. Urinary angiotensinogen as an indicator of intrarenal Angiotensin status in hypertension. Hypertension. 2002;41(1):42–9. doi: 10.1161/01.hyp.0000050102.90932.cf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huggins CE, Domenighetti AA, Pedrazzini T, Pepe S, Delbridge LM. Elevated intracardiac angiotensin II leads to cardiac hypertrophy and mechanical dysfunction in normotensive mice. Journal of Renin-Angiotensin-Aldosterone System. 2003;4(3):186–90. doi: 10.3317/jraas.2003.030. [DOI] [PubMed] [Google Scholar]
- 28.Baker KM, Booz GW, Dostal DE. Cardiac Actions of Angiotensin II: Role of an Intracardiac Renin-Angiotensin System. Annual Review of Physiology. 1992;54:227–41. doi: 10.1146/annurev.ph.54.030192.001303. [DOI] [PubMed] [Google Scholar]
- 29.Rey F, Cifuentes M, Kiarash A, Quinn M, Pagano P. Novel competitive inhibitor of NAD(P)H oxidase assembly attenuates vascular O(2)( −) and systolic blood pressure in mice. Circulation research. 2001;89(5):408–14. doi: 10.1161/hh1701.096037. [DOI] [PubMed] [Google Scholar]
- 30.López N, Díez J, Fortuño M. Differential hypertrophic effects of cardiotrophin-1 on adult cardiomyocytes from normotensive and spontaneously hypertensive rats. Journal of molecular and cellular cardiology. 2006;41(5):902–13. doi: 10.1016/j.yjmcc.2006.03.433. [DOI] [PubMed] [Google Scholar]
- 31.Zhu X, Manning R, Lu D, Gomez-Sanchez C, Fu Y, Juncos L, et al. Aldosterone stimulates superoxide production in macula densa cells. American journal of physiology Renal physiology. 2011;301(3):35. doi: 10.1152/ajprenal.00596.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hirono Y, Yoshimoto T, Suzuki N, Sugiyama T, Sakurada M, Takai S, et al. Angiotensin II Receptor Type 1-Mediated Vascular Oxidative Stress and Proinflammatory Gene Expression in Aldosterone-Induced Hypertension: The Possible Role of Local Renin-Angiotensin System. Endocrinology. 2006;148(4):1688–96. doi: 10.1210/en.2006-1157. [DOI] [PubMed] [Google Scholar]
- 33.Touyz R, Mercure C, He Y, Javeshghani D, Yao G, Callera G, et al. Angiotensin II-dependent chronic hypertension and cardiac hypertrophy are unaffected by gp91phox-containing NADPH oxidase. Hypertension. 2005;45(4):530–7. doi: 10.1161/01.HYP.0000158845.49943.5e. [DOI] [PubMed] [Google Scholar]
- 34.Bayorh MA, Rollins-Hairston A, Adiyiah J, Lyn D, Eatman D. Eplerenone suppresses aldosterone/salt-induced expression of NOX-4. Journal of Renin-Angiotensin-Aldosterone System. 2011;12(3):195–201. doi: 10.1177/1470320310391330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Montezano A, Touyz R. Reactive oxygen species, vascular Noxs, and hypertension: focus on translational and clinical research. Antioxidants & redox signaling. 2014;20(1):164–82. doi: 10.1089/ars.2013.5302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Meijs MFL, Bots ML, Vonken E-JA, Cramer M-JM, Melman PG, Velhuis BK, et al. Rationale and design of the SMART Heart study, A prediction model for left ventricular hypertrophy in hypertension. Netherland’s Heart Journal. 2007;15:295–8. doi: 10.1007/BF03086003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Moreno M, San José G, Pejenaute Á, Landecho M, Díez J, Beloqui Ó, et al. Association of phagocytic NADPH oxidase activity with hypertensive heart disease: a role for cardiotrophin-1? Hypertension. 2014;63(3):468–74. doi: 10.1161/HYPERTENSIONAHA.113.01470. [DOI] [PubMed] [Google Scholar]
- 38.González A, López B, Martín-Raymondi D, Lozano E, Varo N, Barba J, et al. Usefulness of plasma cardiotrophin-1 in assessment of left ventricular hypertrophy regression in hypertensive patients. Journal of hypertension. 2005;23(12):2297–304. doi: 10.1097/01.hjh.0000184406.12634.f9. [DOI] [PubMed] [Google Scholar]
- 39.López B, Castellano J, González A, Barba J, Díez J. Association of increased plasma cardiotrophin-1 with inappropriate left ventricular mass in essential hypertension. Hypertension. 2007;50(5):977–83. doi: 10.1161/HYPERTENSIONAHA.107.098111. [DOI] [PubMed] [Google Scholar]
- 40.López-Andrés N, Martin-Fernandez B, Rossignol P, Zannad F, Lahera V, Fortuno M, et al. A role for cardiotrophin-1 in myocardial remodeling induced by aldosterone. American journal of physiology Heart and circulatory physiology. 2011;301(6):82. doi: 10.1152/ajpheart.00283.2011. [DOI] [PubMed] [Google Scholar]
- 41.Rickard A, Morgan J, Tesch G, Funder J, Fuller P, Young M. Deletion of mineralocorticoid receptors from macrophages protects against deoxycorticosterone/salt-induced cardiac fibrosis and increased blood pressure. Hypertension. 2009;54(3):537–43. doi: 10.1161/HYPERTENSIONAHA.109.131110. [DOI] [PubMed] [Google Scholar]
- 42.Wilson P, Morgan J, Funder J, Fuller P, Young M. Mediators of mineralocorticoid receptor-induced profibrotic inflammatory responses in the heart. Clinical science (London, England : 1979) 2009;116(9):731–9. doi: 10.1042/CS20080247. [DOI] [PubMed] [Google Scholar]
- 43.Ortiz RM, Graciano ML, Mullins JJ, Mitchell KD. Aldosterone receptor antagonism alleviates proteinuria, but not malignant hypertension, in Cyp1a1-Ren2 transgenic rats. Am J Physiol Renal Physiol. 2007;293:F1584–91. doi: 10.1152/ajprenal.00124.2007. [DOI] [PubMed] [Google Scholar]
- 44.Martinez DV, Rocha R, Matsumura M, Oestreicher E, Ochoa-Maya M, Roubsanthisuk W, et al. Cardiac Damage Prevention by Eplerenone: Comparison With Low Sodium Diet or Potassium Loading. Hypertension. 2002;39(2):614–8. [PubMed] [Google Scholar]
- 45.Pojoga L, Baudrand R, Adler G. Mineralocorticoid receptor throughout the vessel: a key to vascular dysfunction in obesity. European heart journal. 2013;34(45):3475–7. doi: 10.1093/eurheartj/eht158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ortiz RM, Graciano ML, Seth D, Awayda MS, Navar LG. Aldosterone receptor antagonism exacerbates intrarenal angiotensin II augmentation in ANG II-dependent hypertension. Am J Physiol Renal Physiol. 2007;293(1):F139–47. doi: 10.1152/ajprenal.00504.2006. Epub 2007/03/23. [DOI] [PubMed] [Google Scholar]
- 47.Klett C, Nobiling R, Gierschik P, Hackenthal E. Angiotensin II stimulates the synthesis of angiotensinogen in hepatocytes by inhibiting adenylylcyclase activity and stabilizing angiotensinogen mRNA. Journal of Biological Chemistry. 1993;268(33):25095–107. [PubMed] [Google Scholar]
- 48.Navar LG. Intrarenal renin–angiotensin system in regulation of glomerular function. Current opinion in nephrology and hypertension. 2014;23(1):38–45. doi: 10.1097/01.mnh.0000436544.86508.f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kobori H, Kamiyama M, Harrison-Bernard LM, Navar LG. Cardinal role of the intrarenal Renin-Angiotensin system in the pathogenesis of diabetic nephropathy. Journal of Investigative Medicine. 2013;61(2):256–64. doi: 10.231/JIM.0b013e31827c28bb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kobori H, Mori H, Masaki T, Nishiyama A. Angiotensin II blockade and renal protection. Current pharmaceutical design. 2013;19(17):3033–42. doi: 10.2174/1381612811319170009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Harrison-Bernard L, Zhuo J, Kobori H, Ohishi M, Navar L. Intrarenal AT(1) receptor and ACE binding in ANG II-induced hypertensive rats. American journal of physiology Renal physiology. 2002;282(1):25. doi: 10.1152/ajprenal.00335.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kobori H, Harrison-Bernard L, Navar L. Urinary excretion of angiotensinogen reflects intrarenal angiotensinogen production. Kidney international. 2002;61(2):579–85. doi: 10.1046/j.1523-1755.2002.00155.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Nagai Y, Yao L, Kobori H, Miyata K, Ozawa Y, Miyatake A, et al. Temporary Angiotensin II Blockade at the Prediabetic Stage Attenuates the Development of Renal Injury in Type 2 Diabetic Rats. J Am Soc Nephrol. 2005 doi: 10.1681/ASN.2004080649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mizuno M, Sada T, Kato M, Koike H. Renoprotective Effects of Blockade of Angiotensin II AT1 Receptors in an Animal Model of Type 2 Diabetes. Hypertens Res. 2002;25:271–9. doi: 10.1291/hypres.25.271. [DOI] [PubMed] [Google Scholar]
- 55.Blasi ER, Rocha R, Rudolph AE, Blomme EAG, Polly ML, McMahon EG. Aldosterone/salt induces renal inflammation and fibrosis in hypertensive rats. Kidney Int. 2003;63(5):1791–800. doi: 10.1046/j.1523-1755.2003.00929.x. [DOI] [PubMed] [Google Scholar]
- 56.Rocha R, Stier CT, Kifor I, Ochoa-Maya MR, Rennke HG, Williams GH, et al. Aldosterone: a mediator of myocardial necrosis and renal arteriopathy. Endocrinology. 2000;141(10):3871–8. doi: 10.1210/endo.141.10.7711. [DOI] [PubMed] [Google Scholar]
- 57.Rocha R, Martin-Berger CL, Yang P, Scherrer R, Delyani J, McMahon E. Selective Aldosterone Blockade Prevents Angiotensin II/Salt-Induced Vascular Inflammation in the Rat Heart. Endocrinology. 2002;143(12):4828–36. doi: 10.1210/en.2002-220120. [DOI] [PubMed] [Google Scholar]
- 58.Rocha R, Chander PN, Khanna K, Zuckerman A, Stier CT., Jr Mineralocorticoid blockade reduces vascular injury in stroke-prone hypertensive rats. Hypertension. 1998;31(1 Pt 2):451–8. doi: 10.1161/01.hyp.31.1.451. Epub 1998/02/07. [DOI] [PubMed] [Google Scholar]
- 59.Quaschning T, Ruschitzka F, Shaw S, Luscher TF. Aldosterone receptor antagonism normalizes vascular function in liquorice-induced hypertension. Hypertension. 2001;37(2 Pt 2):801–5. doi: 10.1161/01.hyp.37.2.801. Epub 2001/03/07. [DOI] [PubMed] [Google Scholar]
- 60.Hao L, Kanno Y, Fukushima R, Watanabe Y, Ishida Y, Suzuki H. Effects of eplerenone on heart and kidney in two-kidney, one-clip rats. Am J Nephrol. 2004;24(1):54–60. doi: 10.1159/000075945. Epub 2004/01/07. [DOI] [PubMed] [Google Scholar]
- 61.Kobayashi N, DeLano FA, Schmid-Schonbein GW. Oxidative stress promotes endothelial cell apoptosis and loss of microvessels in the spontaneously hypertensive rats. Arteriosclerosis, thrombosis, and vascular biology. 2005;25(10):2114–21. doi: 10.1161/01.ATV.0000178993.13222.f2. Epub 2005/07/23. [DOI] [PubMed] [Google Scholar]
- 62.Sanz-Rosa D, Oubina MP, Cediel E, De las Heras N, Aragoncillo P, Balfagon G, et al. Eplerenone reduces oxidative stress and enhances eNOS in SHR: vascular functional and structural consequences. Antioxid Redox Signal. 2005;7(9–10):1294–301. doi: 10.1089/ars.2005.7.1294. Epub 2005/08/24. [DOI] [PubMed] [Google Scholar]
- 63.Romero-Calvo I, Ocon B, Martinez-Moya P, Suarez MD, Zarzuelo A, Martinez-Augustin O, et al. Reversible Ponceau staining as a loading control alternative to actin in Western blots. Anal Biochem. 2010;401(2):318–20. doi: 10.1016/j.ab.2010.02.036. Epub 2010/03/09. [DOI] [PubMed] [Google Scholar]
- 64.Vázquez-Medina J, Crocker D, Forman H, Ortiz R. Prolonged fasting does not increase oxidative damage or inflammation in postweaned northern elephant seal pups. The Journal of experimental biology. 2010;213(Pt 14):2524–30. doi: 10.1242/jeb.041335. [DOI] [PMC free article] [PubMed] [Google Scholar]