Abstract
Celiac disease is a multisystem immune based disorder that is triggered by the ingestion of gluten in genetically susceptible individuals. The prevalence of celiac disease has risen in recent decades and is currently about 1% in most Western populations. The reason for this rise is unknown, although environmental factors related to the hygiene hypothesis are suspected. The pathophysiology of celiac disease involves both the innate and adaptive immune response to dietary gluten. Clinical features are diverse and include gastrointestinal symptoms, metabolic bone disease, infertility, and many other manifestations. Although a gluten-free diet is effective in most patients, this diet can be burdensome and can limit quality of life; consequently, non-dietary therapies are at various stages of development. This review also covers non-celiac gluten sensitivity. The pathophysiology of this clinical phenotype is poorly understood, but it is a cause of increasing interest in gluten-free diets in the general population.
Introduction
Celiac disease occurs in about 1% of the population worldwide, although most people with the condition are undiagnosed.1 It can cause a wide variety of symptoms, both intestinal and extra-intestinal because it is a systemic autoimmune disease that is triggered by dietary gluten. Patients with celiac disease are at increased risk of cancer, including a twofold to fourfold increased risk of non-Hodgkin’s lymphoma and a more than 30-fold increased risk of small intestinal adenocarcinoma, and they have a 1.4-fold increased risk of death.2
Studies of stored serum show that the prevalence of celiac disease has increased fourfold to fivefold over the past 50 years, and the reason for this rise is unknown, although it may relate to aspects of the hygiene hypothesis (exposure to micro-organisms and antibiotics).3 Despite advances in our understanding of its pathophysiology and improved diagnostic tools, the rise in celiac disease has been a largely silent epidemic, with undiagnosed patients going untreated and at increased risk of morbidity from intestinal and extra-intestinal symptoms, as well as the risks of cancer and mortality mentioned above.
Interest in gluten as a determinant or contributing factor in a variety of conditions has also increased, with many people identifying themselves as being gluten sensitive in the absence of celiac disease. The biological basis of gluten induced symptoms in the absence of celiac disease is largely unknown but may be related to immune responses to components of wheat apart from gluten. This review covers celiac disease and non-celiac gluten sensitivity because they are considered part of a spectrum of gluten related disorders.4 5
Sources and selection criteria
We identified relevant publications by searching PubMed using the terms “c(o)eliac disease”, “c(o)eliac sprue”, and “gluten” from the year 2000 to 31 January 2015. We also identified publications by searching the bibliographies of relevant articles, as well as abstracts from Digestive Disease Week conferences for the years 2011-14 and the biennial International Coeliac Disease Symposium in 2011 and 2013. The literature review included randomized controlled trials, cohort studies, case-control studies, and cross sectional analyses. A few studies were randomized controlled trials, and those pertaining to celiac disease or non-celiac gluten sensitivity of adequate size and quality were included. Most studies were well designed non-randomized controlled trials or observational studies with controls. We included all relevant randomized trials on the subjects of celiac disease and non-celiac gluten sensitivity, and included other studies on the basis of relevance, sample size, quality, and outcomes.
Prevalence worldwide
Celiac disease currently occurs in about 1% of the general population worldwide.4 In Sweden this prevalence was first noted 15 years ago,6 and similar levels were subsequently reported elsewhere1; even higher levels have sometimes been reported in young (12 year olds in Sweden) and older people (aged 52-74 in Finland).7 8 In general, prevalence studies based on serology only (tissue transglutaminase (TTG) and endomysial (EMA) antibodies) report higher prevalence than screening that requires confirmation through small intestinal biopsy.9 10
Prevalence by country
The differences in prevalence between countries cannot be fully explained by diagnostic criteria. Two recent studies indicate a biopsy verified prevalence of 0.7-0.8% in the United States,1 11 which is consistent with earlier data from North America.12 The disease seems to be more common in white people than in African-Americans or Hispanics in the US.1 13
Data from Europe vary widely, with the United Kingdom and Germany having a low prevalence,14 15 while Sweden and Finland have perhaps the highest prevalence rates reported to date (2-3%).7 8
Reports on the prevalence of celiac disease outside of Europe and the US are less abundant. The prevalence of celiac disease in China is low (probably because of the scarcity of the necessary HLA haplotypes, DQ2 and DQ8, in the Chinese population).16
The prevalence of biopsy verified celiac disease in the Indian Punjab region, where wheat is a staple food, is 1%.17 The disease is rare in people from sub-Saharan Africa—none of 600 people in Burkina Faso who were screened were positive for EMA or TTG antibodies.18
Prevalence by age
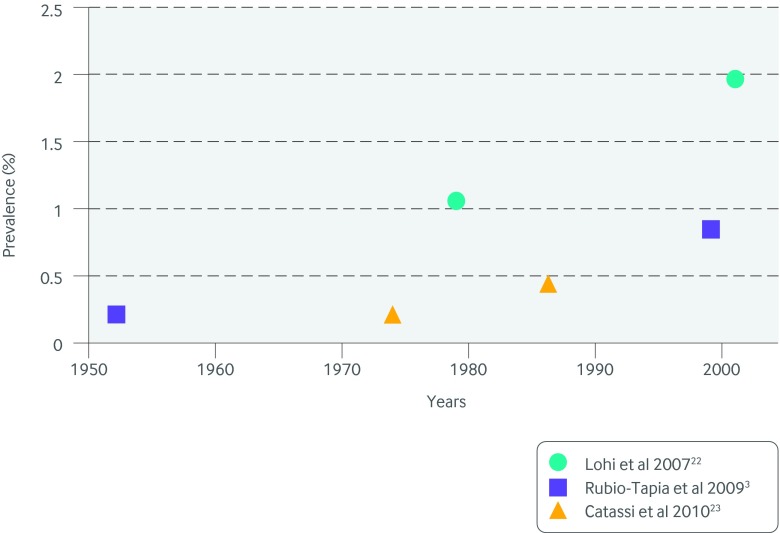
Because celiac disease can develop at any age19 and the absolute mortality rate after diagnosis is low,2 20 it might be expected that the prevalence of disease would be higher in older age groups. The similar prevalence in children and adults is therefore surprising.10 The conspicuous lack of a higher prevalence in adults may partly be the result of cohort effects. For instance, the incidence of celiac disease increased dramatically among young children during an approximately 10 year period in Sweden that began in the late 1980s, and the prevalence of celiac disease in those who were born during that period remains raised.21 Screening studies of unselected people have shown an increase in the prevalence of celiac disease over time—both undiagnosed plus diagnosed disease22 23 and undiagnosed disease only (fig 1 ).3
Fig 1 Increasing prevalence of celiac disease over time as illustrated by screening studies
First degree relatives of people with the disease form a special high risk group. The lifetime risk of celiac disease in these people has been estimated at 4-17%.12 24 First degree relatives who are homozygous for HLA DQ2 are at particularly high risk, with about a 26% chance of developing celiac disease during childhood.25 26 Second degree relatives are also at increased risk, although the risk is smaller.12
Incidence of diagnosed celiac disease
Several studies suggest that the incidence of diagnosed celiac disease is increasing. Data from a North American county have shown a continuous rise in incidence since the 1950s,27 reaching 17 per 100 000 person years in 2008-2011.28 Similar data were recently reported from the UK,14 where the incidence in an unselected population reached 19 per 100 000 person years in 2010 and 2011.
The prevalence and incidence of celiac disease are dependent on several factors:
Underlying genetics of the population (a prerequisite for diagnosis)
Gluten exposure and possibly infant feeding patterns
Other environmental risk factors
Awareness of disease (among patients and physicians)
Method and frequency of testing.
Although the rise in the prevalence of celiac disease may be partly due to changing diagnostic criteria (serology v histological examination), this is unlikely to be the only reason for the increase. Thus, other factors must be sought to explain these higher rates.
Environmental risk factors
Even in monozygotic twins, concordance is only about 85%.29 The lack of concordance suggests that non-genetic factors are crucial in the development of celiac disease. The most obvious risk factor is gluten exposure. In settings with a high gluten load (such as refugee camps of the Saharawi people in Africa30 and formula fed Swedish infants born in the early 1990s21) well over 1% of the population was affected.
Infant feeding patterns
Given that an epidemic of celiac disease in Swedish infants coincided with a change in infant feeding recommendations,21 the timing of gluten introduction, quantity of gluten at introduction, and breastfeeding patterns in relation to gluten introduction had long been assumed to affect the development of celiac disease.31 However, three recent prospective observational studies have failed to confirm an association between breastfeeding patterns and later celiac disease.32 33 34 This lack of association was corroborated by two multicenter randomized clinical trials in 2014, which found no link between age of gluten introduction, ongoing breast feeding, and the development of celiac disease.25 26 Nevertheless, data on the importance of the amount of gluten given at introduction and whether a gradual increase in gluten exposure will protect against celiac disease need to be examined further.
Perinatal exposure
A Swedish study of prospectively collected data on perinatal risk factors in more than 11 000 people with celiac disease found no association between any cesarean section and later celiac disease (odds ratio 1.06, 95% confidence interval 0.99 to 1.13) but did find a small increased risk in those undergoing elective cesarean section (1.15, 1.04 to 1.26).35 This might be because the baby does not enter the birth canal during elective cesarean section. This would have an effect on the baby’s bacterial gut flora and could potentially mediate celiac disease.35
Infection
As with other immune mediated diseases, such as type 1 diabetes,36 viral infections have sometimes been linked to celiac disease,37 but the evidence for an underlying viral trigger is inconclusive. Exposure to gastrointestinal infection during early life and adulthood seems to be linked to the development of celiac disease,33 38 39 but study shortcomings (potential recall bias,40 lack of significance,33 and data being significant only when analyzed for trend38) make the interpretation of data difficult. One cross sectional study from the US suggests that gastric colonization with Helicobacter pylori may protect against the development of celiac disease.41
Smoking
Data on smoking are inconsistent and inconclusive. In the UK and elsewhere,42 43 44 smoking seems to protect against celiac disease. By contrast, other studies have found little association with smoking.45 Population based prospectively recorded data on smoking are probably needed to determine whether smoking influences the risk of developing celiac disease.
Drugs
Drugs such as proton pump inhibitors and antibiotics have been linked to the development of celiac disease,46 47 but these data should be interpreted with caution because some of these drugs may have been given in response to symptoms caused by undiagnosed celiac disease rather than triggering its development.
Pathophysiology
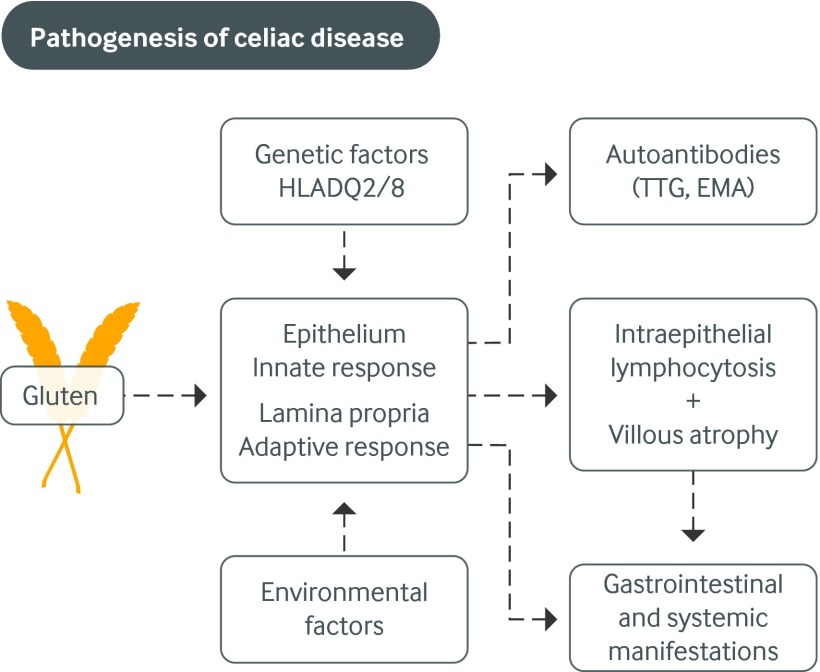
Celiac disease results from the interaction of environmental factors, mainly gluten, with immune and genetic factors (fig 2 ). For immunological reasons, the disease almost exclusively occurs in people with the DQ2 or DQ8 HLA haplotype.48
Fig 2 The pathogenesis of celiac disease involves a triad of predisposing genes (HLA-DQ2 and HLA-DQ8 haplotypes), dietary gluten, and other less well defined environmental factors. Innate and adaptive immune responses to gluten fragments at the small intestinal epithelium result in characteristic autoantibodies, histologic changes (intraepithelial lymphocytosis and villous atrophy), and clinical symptoms (such as diarrhea or iron deficiency anemia). Adapted, with permission, from Green and colleagues49
Gluten is the term for the storage proteins of the cereal grains wheat, rye, and barley. Gluten proteins are rich in glutamines and prolamines and are therefore incompletely digested by gastric, pancreatic, and brush border peptidases, leaving large peptides up to 33 amino acids long.50 These peptides pass through the epithelial barrier of the intestine and enter the lamina propria through a transcellular or paracellular route.51 52 The relative importance of each route in the pathogenesis of celiac disease is unclear.
The immune response to gluten involves both the adaptive and innate immune systems. Within the lamina propria an adaptive immune reaction occurs. TTG deamidates gliadin, and this increases its immunogenicity by altering the charge of the gliadin fragments that facilitate binding to the HLA DQ2 or DQ8 molecule on antigen presenting cells. Gliadin reactive CD4 positive T cells recognize gliadin peptides presented by these antigen presenting cells and subsequently produce proinflammatory cytokines,53 especially interferon γ.54 During the inflammatory cascade, the release of metalloproteinases and other tissue damaging mediators induces tissue injury.55 During this process TTG antibodies are formed through unclear mechanisms. The role of these TTG antibodies in disease modulation is uncertain; however, they may contribute to systemic manifestations of celiac disease such as dermatitis herpetiformis.56
The presence of increased intraepithelial lymphocytes (IELs) reflects the role of the innate immune system in celiac disease because IELs express the natural killer (NK) T cell receptors, NKG2D and CD9/NKG2A, which recognize the products of stress induced genes MICA and MICB and the protein HLA-E on epithelial cells.57 Interleukin 15 (IL-15) plays a central role in upregulating NK receptors on these cytotoxic epithelial cells.58 The mechanism of the interaction between the processes in the epithelium and lamina propria has not been elucidated. Recently non-gluten wheat proteins have been suggested to be responsible for the innate epithelial cell damage.59
Clinical presentations and the role of screening
Celiac disease can present at any age, although nowadays rarely presents as a malabsorption syndrome with diarrhea, edema, and wasting.60
Children
The major modes of presentation in children are recurrent abdominal pain, growth problems (failure to thrive and short stature), and the screening of high risk groups.61
A diarrhea predominant presentation currently occurs in only 10% of children and tends to be most prominent in those who are very young at diagnosis.61 62 Those detected at screening have family members with the disease or have an autoimmune disease such as type 1 diabetes or thyroid disease. Children may be overweight or obese at diagnosis.61
Adults
Although diarrhea remains one mode of presentation that prompts testing for celiac disease in adults, most patients with the disease do not have diarrhea. Instead, most adults have one of the many “non-classic symptoms” such as anemia (usually as a result of iron deficiency, although it may be caused by chronic disease63); osteoporosis; and various other presentations, including dermatitis herpetiformis, abdominal pain,64 neurological or psychiatric problems,65 infertility, aphthous stomatitis,66 and vitamin deficiencies.67
Screening
Patients may be diagnosed as a result of screening of high risk groups or incidental discovery at endoscopy, which is typically performed for reflux disease.68 Most newly diagnosed patients have a normal body mass index, with 15% being underweight and a similar proportion being overweight or obese.69 70 The diagnosis is made more often in women than in men and is rarely made in young men.71
In adults, as with children, screening of at risk groups involves family members of people with celiac disease, as well as people with type 1 diabetes, other autoimmune disorders, and Down’s syndrome. Although celiac disease fulfils some of the World Health Organization criteria for general population screening, such screening is currently not recommended. Screening for celiac disease is controversial, with some authorities advising this practice in high risk groups,72 and others not.73 Recent British Society of Gastroenterology (BSG) guidelines advise screening people at high risk, including those with a family member who has the disease.74
Mortality and cancer in people with celiac disease
Mortality
Most studies indicate that celiac disease is associated with an increased risk of mortality2 75 and cancer.76 77 However, as shown in a meta-analysis, excess mortality is low,78 and one British study published in 2015 even suggests that patients have no increased risk of death.20 Different risk estimates may mirror country specific factors (such as disease management), but they may also depend on how disease is defined and how patients in each study are identified. The absolute risk of death is low. In the largest study so far the excess risk (attributable risk) beyond one year after diagnosis was 0.2 per 1000 person years in children (≤20 years) and 8.2 per 1000 in adults aged over 60 years at diagnosis.2 In that study the risk of the most common causes of death (cardiovascular disease and cancer) was similar to that seen in the general population.
Cancer
Non-Hodgkin’s lymphoma has attracted most attention in celiac disease. Earlier reports of a 10-fold increased risk in patients with celiac disease have been dramatically reduced to relative risks between two and four, with one study reporting an absolute excess risk of 40 per 100 000 person years.77 78 79 The risk of both T cell and B cell non-Hodgkin’s lymphoma is increased. The future risk of non-Hodgkin’s lymphoma is dependent on mucosal healing.80 Of the gastrointestinal cancers, the largest relative increase is that for small intestinal adenocarcinoma (hazard ratio 31.0) although the absolute risk of that rare cancer is low (10 instances in 28 882 patients), and the absolute excess risk of any gastrointestinal cancer was two per 100 000 person years.81
Patients with celiac disease do not seem to be at increased risk of prostate cancer and breast cancer, which are common in the general population.82 83
Other comorbidities and complications associated with celiac disease
Many of the conditions associated with celiac disease share a common genetic basis.84 The genetic overlap does not only involve HLA genes but also non-HLA genes, such as those encoding CTLA-4 and myosin 1XB. IL2 and IL21 genes have also been linked to celiac disease.85 However, considering the overwhelming importance of the HLA system, it is not unexpected that diseases that are associated with the same HLA haplotypes as celiac disease (such as type 1 diabetes and autoimmune thyroid disease) have been linked to celiac disease.86
Autoimmune diseases
The prevalence of celiac disease approaches 5% in many autoimmune diseases. The association with celiac disease is often bi-directional—people with celiac disease are at increased risk of immune mediated diseases both before and after the diagnosis of celiac disease.87 88 One rationale for diagnosing minimally symptomatic celiac disease is that this may reduce the risk of developing other autoimmune diseases, although the results of studies on such a protective effect are conflicting.89
Gastrointestinal disease
Celiac disease has also been linked to gastrointestinal disorders such as liver disease and pancreatic disease.90 91 92 93 The spectrum of disease varies from an asymptomatic increase in serum transaminases,94 to liver failure,91 liver cancer,81 and pancreatic cancer.81 For several gastrointestinal cancers, particularly small intestinal adenocarcinoma, the relative risks are strikingly high in the first year after the diagnosis of celiac disease, suggesting that part of the increased risk may be due to ascertainment bias or confounding by indication.
The highest relative risks for liver disease in celiac disease have been seen in primary biliary cirrhosis.95 Although cost effectiveness analyses have not been performed on this subject, it seems prudent to test for celiac disease in patients with raised transaminases of unclear cause and in patients with primary biliary cirrhosis.
Cardiovascular disease
Of particular interest has been the risk of ischemic heart disease because study results have been contradictory. In general, Nordic studies have reported a positive association,96 97 98 whereas most British studies have noted an inverse association. 20 98 99 100 This difference in relative risk for cardiovascular disease may reflect underlying factors, such as socioeconomic status and smoking, which seem to differ between countries.
Pregnancy
Unlike diagnosed celiac disease, undiagnosed disease has repeatedly been linked to adverse pregnancy outcomes, including spontaneous abortion.101 102 103 104 However, in large scale studies, both diagnosed and undiagnosed celiac disease do not seem to be major risk factors for congenital malformations.105 Recent data also indicate that infertility is rare in women with the disease.106
Assessment and importance of healing of the intestinal mucosa
Persistent intraepithelial lymphocytosis
After celiac disease is diagnosed and a gluten-free diet is started the intestinal mucosa usually starts to heal. This is a gradual process, and the median time to achieve a normal villous height was estimated to be 3.8 years in one study of 241 adults who underwent serial follow-up biopsy.107 In some patients villous height normalizes but intraepithelial lymphocytosis persists. The implications of this are uncertain, but one study that compared 96 patients with persistence versus 74 patients with completely normal small intestinal histology found no difference in the risk of cancer or quality of life, although the study may have been underpowered for either of these two outcome measures.108 Patients with persistent intraepithelial lymphocytosis were more likely to be regular consumers of oats, although this finding did not translate into clinical significance.108
Persistent villous atrophy
By contrast, persistent villous atrophy has been linked to clinically important outcomes. A population based study of patients in Sweden who underwent follow-up biopsy found that 44% had persistent villous atrophy.109 However, there was no difference between groups in overall mortality,110 cardiovascular outcomes,111 or obstetric complications (in women who were pregnant within five years of follow-up biopsy),112 although those with persistent villous atrophy were found to have a higher risk of lymphoproliferative disorders than those with mucosal healing (hazard ratio 2.25, 1.18 to 4.34; absolute excess risk 57 per 100 000 person years).80 Patients with persistent villous atrophy also had a higher risk of hip fracture and other fractures that were probably caused by osteoporosis than those with mucosal healing.113
Follow-up biopsy
Results of the follow-up biopsy correlate with adherence to a gluten-free diet and seem to be more sensitive as a marker of gluten exposure than normalization of TTG antibodies.114 Follow-up biopsy can therefore help discern the cause of persistent or recurrent symptoms and is crucial for the diagnosis of refractory disease. However, it is unclear whether a follow-up biopsy is needed in all patients. Management guidelines note that practitioners disagree about the need for routine follow-up biopsy in patients who become asymptomatic after starting a gluten-free diet, so it is not universally recommended in this setting.74 115 But the link between persistent villous atrophy and long term morbidity (specifically the risk of lymphoproliferative cancers and osteoporotic fractures) provides support for its role as a risk stratifying tool. Those with persistent villous atrophy, even if asymptomatic, may be appropriate targets for more intensive education with a dietitian; such an approach has been shown to improved histologic outcomes.114
Treatment
Diet
The only known treatment is adherence to a lifelong strict gluten-free diet. Such a diet results in the normalization of symptoms in most patients, with a mean resolution of four weeks.116 Symptom improvement (resolution of diarrhea or abatement of abdominal pain) typically precedes serologic normalization of TTG antibodies (which can take months to more than a year) and is then followed by normalization (or at least improvement) of histologic results. As noted above, intestinal healing is not universal. In a population based study of Swedish patients, lower educational attainment was associated with an increased risk of persistent villous atrophy, which probably reflected poorer adherence to a gluten-free diet.109
Limitations of a gluten-free diet
Although a gluten-free diet is effective when implemented correctly, many patients find it unsatisfactory. It is expensive, with bread and pasta substitutes costing substantially more than their gluten-containing counterparts.117 It can be socially isolating in settings such as communal celebrations, religious rituals, and dining out. Strict avoidance of gluten can be a challenge because of hidden sources of gluten (box). Potential hidden gluten in drugs or sauces is a legitimate source of anxiety for patients, including those who have minimal acute symptoms on exposure to gluten and so remain unsure of the safety of their daily practices. Given these everyday worries about gluten exposure, it is perhaps not surprising that patients’ self rated treatment burden from adhering to a gluten-free diet was similar to that of patients with end stage renal disease in one questionnaire study.118 The shortcomings of this diet are also underscored by the fact that about 20% of patients report persistent or recurrent symptoms after diagnosis, and the most common cause of these symptoms is gluten exposure.119 (Other causes of persistent or recurrent symptoms in celiac disease, once the initial diagnosis is verified, include concomitant irritable bowel syndrome, additional food intolerances, microscopic colitis, and small bacterial overgrowth.)
Sources of dietary gluten
Primary sources
Wheat (triticale, semolina, spelt, khorasan wheat)
Rye
Barley (malt)
Hidden sources
Oats (unless harvested separately from wheat)
Sauces (marinades, soy sauce)
Drug fillers (prescription and over the counter items, including dietary supplements)
Shared food preparation equipment (pasta pot, toaster, deep fryer)
Processed meats
Because of these problems with gluten-free diets, most patients are interested in non-dietary treatments for celiac disease.120
Non-dietary treatments
Categories for drug therapy include the detoxification of ingested gluten (glutenases); the enhancement of tight junctions in the intestinal epithelium; a vaccine to induce gluten tolerance; and blockers of immune activation, such as inhibitors of the HLA DQ2 and DQ8 proteins or TTG.121
To date, two drugs have been evaluated in phase II studies. Larazotide acetate is an oral peptide that modulates tight junctions, enhancing the epithelial barrier to prevent immune activation in the lamina propria. In two randomized studies (270 patients) involving a gluten challenge, larazotide acetate did not differ significantly from placebo regarding the outcome of intestinal permeability (as measured by the lactulose to mannitol urinary excretion ratio). However, symptoms were attenuated (P=0.013) and the rise in TTG levels was blunted (P=0.01) compared with placebo.122 123 In another phase II study, a combined oral endopeptidase and endoprotease (ALV003) was compared with placebo in 34 patients with celiac disease who were undergoing gluten challenge. Those randomized to ALV003 had no significant reduction in villous height on intestinal biopsy, whereas those taking placebo had the expected gluten induced mucosal injury.124 Subsequent trials of both of these drugs are planned.
Non-celiac gluten sensitivity
Worldwide there is a great interest in gluten-free diets, and many people have adopted such a diet in the absence of a diagnosis of celiac disease or clear health benefit.
The term non-celiac gluten sensitivity (NCGS) was coined to encompass those people who report symptoms that respond to withdrawal of gluten from the diet in the absence of celiac disease and wheat allergy.4 125 Perhaps a more accurate term for this condition is people who avoid gluten. It is not clear how common this condition is, or whether all those buying gluten-free food are on a strict gluten-free diet. However, data on this subject are available from several countries.
Prevalence of people who avoid gluten
In a population based questionnaire of 1002 people from the UK, 13% reported gluten sensitivity, with 3.7% claiming to be on a gluten-free diet.126 In a similar random sampling of Australians (n=1184), 7.3 % reported adverse effects from wheat ingestion but most had had no formal medical assessment.127 An analysis of population based data in the US (from the National Health and Nutrition Examination Survey) found that 0.55-0.63% of people were adherent to a gluten-free diet in the absence of celiac disease, a prevalence similar to that of celiac disease (diagnosed and undiagnosed combined).1 128 Women and older people predominated.128 A multicenter study from Italy (n=12 255) found that non-celiac gluten sensitivity was only slightly more common than celiac disease.129 Some population groups seem to be especially wed to the gluten-free diet, with nearly 50% of 910 athletes (including world class and Olympic medalists) adhering to a gluten-free diet, mainly because of the perceived health and energy benefits.130
Diagnosis
The concept of NCGS is not new—reports from the 1970s and 1980s describe patients who had a symptomatic response to wheat or gluten withdrawal in the absence of celiac disease.131 132 However, today NCGS is typically a self diagnosis or a diagnosis made by alternative health practitioners, with patients reporting both gastrointestinal and extra-intestinal symptoms.129 133 134 After gluten exposure those with NCGS report more symptoms than those with celiac disease.135 People who avoid gluten rarely have celiac disease excluded before adopting a gluten-free diet,134 and when evaluated alternative diagnoses such as fructose intolerance or small bowel bacterial overgrowth may be identified.133
Association with irritable bowel syndrome
Some patients with irritable bowel syndrome improve when gluten is restricted. This was demonstrated in an Australian double blind randomized trial of 34 self identified gluten sensitive patients who experienced more symptoms when exposed to gluten compared with placebo (68% v 40%, P=0.0001).136 In another randomized controlled trial in 45 patients with diarrhea predominant irritable bowel syndrome, a gluten containing diet was associated with increased bowel movements (P=0.04) and small bowel permeability (P=0.028), especially in those positive for HLA DQ2 or DQ8.137 A subsequent study of 37 patients found that the effect of gluten exposure in patients with gluten sensitive irritable bowel syndrome was nullified by the use of a diet low in FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols), indicating that other dietary products may be important in some people with NCGS.138 That study raised the possibility that a large proportion of patients with apparent NCGS are instead sensitive to FODMAPs. Most recently, a randomized crossover trial of 61 patients found a significant increase in intestinal and extra-intestinal symptoms in patients exposed to gluten compared with placebo. However, most patients showed no significant difference and the positive result was driven by a large effect of gluten in three patients.139
Pathophysiology
The pathophysiology of NCGS is unclear. Increased permeability of the small intestine was noted in two studies,137 140 but not in a third.141 Gut mucosal immune activation seems to be present, with increased CD3 positive intraepithelial lymphocytes compared with patients with celiac disease who are maintained on a gluten-free diet,135 141 evidence of an adaptive immune response,141 and increased interferon γ response to a gluten challenge.135
Interest has recently developed in the non-gluten components of wheat.142 These include the amylase trypsin inhibitors, which seem to activate the innate immune system,59 and have been suggested to have a role in both celiac disease and NCGS. By definition those with NCGS lack celiac disease specific antibody markers, but some have antibodies to native gliadin, which are thought to have low specificity for celiac disease. In some patients with NCGS and antibodies to gliadin (especially IgG ones), the antibodies disappear and symptoms improve after a gluten-free diet is started.143
Neuropsychiatric disorders
Gluten has been proposed to be involved in various neuropsychiatric disorders including schizophrenia, autism, peripheral neuropathy, and ataxia. Associations have been reported between these conditions, especially schizophrenia144 and peripheral neuropathy,145 and celiac disease. However, studies using larger databases and stored serum from patients with schizophrenia show a high incidence of anti-gliadin antibodies,146 147 148 rather than the more celiac disease specific antibodies, indicating a closer association with NCGS. The clinical significance of these anti-gliadin antibodies is not clear.
Similarly about 20% of people with autism spectrum disorder had antibodies to gliadin, specifically IgG anti-gliadin antibodies rather than the celiac disease specific antibodies to TTG or deamidated gliadin.149 The largest study so far in this field, a population based cohort study of 26 995 patients with celiac disease, found no association between autism and biopsy verified celiac disease but did find a positive association between autism and positive serology, primarily the less specific gliadin antibodies (IgA and IgG).150 Although the importance of these observations needs to be determined, future randomized studies of a gluten-free diet in people with various psychiatric disorders should be targeted at those with a measurable immune response to gluten.
Management
Because NCGS currently has no firm biologic basis, the approach to patients on a self prescribed gluten-free diet is uncertain. Measures should be taken to determine whether the patient has celiac disease, because this has implications for long term dietary guidance and monitoring of complications. It is sometimes necessary to determine the patient’s HLA haplotype in this setting because those negative for DQ2 and DQ8 will not have celiac disease. A focused evaluation for alternative causes of symptoms (such as irritable bowel syndrome or other food intolerances, including intolerance to FODMAPs) is also warranted. Finally, it is advisable to have a frank discussion with patients about the limited current understanding of non-celiac gluten sensitivity, offering guidance on medical and dietary follow-up to guide symptom control.
Future areas of research
Gluten exposure
The prevention of celiac disease in at risk people requires further investigation. The negative results of two recent randomized trials evaluating early low dose gluten exposure at four months after birth25 or delayed gluten exposure until 12 months26 have led to speculation about why these interventions failed and whether celiac disease can be prevented at all.151 Nonetheless, these trials did provide evidence that the number of copies of the HLA DQ2 gene effectively stratifies patients with regard to subsequent risk of celiac disease. In both trials, more than 25% of infants who were homozygous for HLA DQ2 developed the disease,25 26 indicating that this high risk group may be of particular interest when studying future interventions. However, most of those who develop celiac disease do not have a family history and are therefore not in this high risk group.
Although studies into the dose or duration of gluten exposure in infancy may prove useful, further study is needed into exposure in adults. Because celiac disease can develop at any age, studies of dietary habits or drug use in adults may produce insights into the triggers of celiac disease.152
Microbiome
The duodenal and colonic microbiome may prove to be an important mediator in the loss of gluten tolerance in at risk people. Patients with celiac disease have distinct duodenal microbial populations at diagnosis compared with non-celiac controls, with more abundant Bacteroides spp and Escherichia coli, and this normalizes after starting a gluten-free diet.153 One study showed that the microbiome may contribute to, and not be a mere consequence of, the loss of gluten tolerance.154 The study stratified infants of age 1 month who had a first degree relative with celiac disease by risk of celiac disease according to HLA haplotype. Those with an at risk (DQ2) gene had higher proportions of firmicutes and proteobacteria and lower proportions of actinobacteria in their feces than those who were negative for HLA DQ2 and DQ8. Because all of these infants had been vaginally delivered and exclusively breast fed (not yet exposed to gluten), the results indicate that these gut microbial characteristics are a consequence of HLA genotype and may contribute to the pathogenesis of celiac disease.
Reintroduction of gluten
Although there is a need to study prevention strategies for celiac disease, future research should focus on the re-induction of tolerance to gluten after diagnosis. Transient celiac autoimmunity, in which a person develops TTG antibodies that normalize with ongoing gluten ingestion, has been noted in children,155 and it has been documented in one adult.156 This provides proof of concept evidence that the development of celiac disease can be halted, although it is not known whether there is any step beyond which the path is irreversible.
A vaccine is being developed that consists of select immunogenic gluten peptides, and parenteral administration has been shown to mobilize gluten specific peripheral T cells in people with celiac disease who are adhering to a gluten-free diet.121 It remains to be seen whether the immune activation induced by this method can be manipulated into a way to re-induce tolerance.
Diagnosis and follow-up
In addition to efforts to prevent or reverse celiac disease, research is under way to improve diagnosis and follow-up. Point of care kits for diagnosis have been developed with the rationale that ease of testing will improve the problem of underdiagnosis.157 One potential setting for such testing is in patients undergoing upper gastrointestinal endoscopy for any reason, because many of these patients do not undergo duodenal biopsy, so celiac disease may be missed.158 Another potentially useful technology for patients adhering to a gluten-free diet is a consumer friendly detector of gluten in food. When developing such technology, ease of use, portability, speed, and accuracy would need to be optimized.
Biomarkers are also needed for the follow-up of patients with celiac disease. Assessment of symptoms, evaluation by a dietitian, serological test results, and follow-up histologic examination are currently used to assess adherence and response to a gluten-free diet. Efforts are under way to identify biomarkers that correlate more closely than TTG antibody titer with follow-up intestinal histology.
Intestinal fatty acid binding protein is one such candidate. In one study of patients with newly diagnosed celiac disease and patients adhering to a gluten-free diet for various durations, concentrations of this protein correlated with the degree of villous atrophy at diagnosis and on follow-up, and it was raised in those with normalized TTG antibody titer but persistent villous atrophy.159 After further validation, this biomarker may be useful for the regular assessment of the patients with celiac disease. A marker of incompletely digested gluten, that is measurable in the stool as partial epitopes of a 33-amino acid chain, may also prove to be clinically useful when assessing adherence to a gluten-free diet.160
A marker of celiac disease that remains present regardless of the duration of adherence to a gluten-free diet would be particularly useful when evaluating those people who avoid gluten who have not yet been tested for celiac disease, but such a marker has not yet been identified. A marker that can predict the degree of sensitivity to gluten is also needed. The minimum amount of ingested gluten that induces symptoms or villous atrophy varies substantially,161 and future biomarkers, such as those that could identify patients at high risk of complications or refractory disease, might enable a personalized approach, rather than the current blanket mandate of total gluten avoidance.
Education
Improvements in the diagnosis and treatment of patients with celiac disease are crucially dependent on the education of healthcare providers regarding the condition. Even in countries with a high rate of diagnosis patients may have symptoms for a long times before a diagnosis is made.162 There is a paucity of publications on celiac disease relative to its prevalence and compared with other gastrointestinal diseases, although the general quality is high,163 164 indicating that exposure to the disease among non-experts may not be great. Knowledge that celiac disease can be a cause of iron deficiency was poor in a recent survey of hematologists in the US,165 and erratic screening practices in patients with diabetes reflect a lack of and inconsistent guidelines.166 The development of national guidelines in Finland resulted in an increase in the diagnosis of celiac disease.162 167 Importantly, these guidelines had input from and targeted primary care physicians, a group that has first contact with patients and the potential to increase the rate of diagnosis.168 Guidelines need to be developed that are consistent and applicable to the physician population who come into contact with patients with possible celiac disease.
Guidelines
Numerous societies have published guidelines on the diagnosis and management of celiac disease, including the British Society of Gastroenterology74; the American College of Gastroenterology115; the World Gastroenterology Organisation169; the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition72; and the European Society for Paediatric Gastroenterology Hepatology and Nutrition (ESPGHAN).170 Broad areas of agreement include the need for active case finding to identify patients with celiac disease and for a strict gluten-free diet and assessment by a dietitian. All guidelines mandate a duodenal biopsy for diagnosis, except for ESPGHAN, which allows for the diagnosis to be made in certain scenarios on the basis of symptoms, the presence of high titers of celiac disease specific antibodies, and a compatible HLA haplotype.
Conclusion
Celiac disease is an increasingly common autoimmune condition that affects the intestine and has multiple systemic manifestations. Despite the increase in rates of diagnosis, most people with celiac disease remain undiagnosed. This must be remedied by appropriate testing and correct interpretation of serologic and histologic results. The availability of expert dietitians must be increased to improve the care of patients who strive to avoid hidden sources of gluten while maintaining a healthy diet. With knowledgeable patients and healthcare providers, advances in celiac disease will translate into symptom control, reduced morbidity, and improved quality of life.
Despite interest in the health effects of gluten in people without celiac disease, the biology underlying NCGS is unclear. As such, future research should focus on the identification of biomarkers to better characterize what is probably a heterogeneous group of disorders. Evaluation of the innate immune response to gluten in people with NCGS, as well as long term natural history studies, will inform the management of these patients. Despite our lack of knowledge about the epidemiology, pathophysiology, and natural course of NCGS, the approach to people who avoid gluten should involve ruling out celiac disease, assessing for other disorders, and providing symptom based medical and dietary treatment.
Questions for future research
Why is celiac disease increasing in incidence, and what environmental triggers can be modified so as to prevent its development?
What causes intestinal symptoms (abdominal pain and altered bowel habits) in patients with celiac disease and why do some patients have no symptoms?
Is the loss of tolerance to gluten irreversible or can tolerance be regained through immunotherapy?
Is there a biomarker that can distinguish patients with non-celiac gluten sensitivity from those with celiac disease and those with functional gastrointestinal disorders?
Contributors: All three authors participated in all four components of authorship: the conception or design of the work; the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; and final approval of the version to be published. Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. PHRG is guarantor.
Funding: BL: National Center for Advancing Translational Sciences, National Institutes of Health (UL1 TR000040). JFL: Örebro University Hospital, Karolinska Institutet, the Swedish Society of Medicine, the Swedish Research Council—Medicine (522-2A09-195), and the Swedish Coeliac Society.
Competing interests: We have read and understood BMJ policy on declaration of interests and declare the following interests: PHRG serves on the scientific advisory boards of Alvine Pharmaceuticals and ImmusanT. The other authors have no competing interests.
Provenance and peer review: Commissioned; externally peer reviewed.
Cite this as: BMJ 2015;351:h4347
References
- 1.Rubio-Tapia A, Ludvigsson JF, Brantner TL, et al. The prevalence of celiac disease in the United States. Am J Gastroenterol 2012;107:1538-44. [DOI] [PubMed] [Google Scholar]
- 2.Ludvigsson JF, Montgomery SM, Ekbom A, et al. Small-intestinal histopathology and mortality risk in celiac disease. JAMA 2009;302:1171-8. [DOI] [PubMed] [Google Scholar]
- 3.Rubio-Tapia A, Kyle RA, Kaplan EL, et al. Increased prevalence and mortality in undiagnosed celiac disease. Gastroenterology 2009;137:88-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ludvigsson JF, Leffler DA, Bai JC, et al. The Oslo definitions for coeliac disease and related terms. Gut 2013;62:43-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sapone A, Bai JC, Ciacci C, et al. Spectrum of gluten-related disorders: consensus on new nomenclature and classification. BMC Med 2012;10:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carlsson AK, Axelsson IE, Borulf SK, et al. Serological screening for celiac disease in healthy 2.5-year-old children in Sweden. Pediatrics 2001;107:42-5. [DOI] [PubMed] [Google Scholar]
- 7.Myleus A, Ivarsson A, Webb C, et al. Celiac disease revealed in 3% of Swedish 12-year-olds born during an epidemic. J Pediatr Gastroenterol Nutr 2009;49:170-6. [DOI] [PubMed] [Google Scholar]
- 8.Vilppula A, Collin P, Maki M, et al. Undetected coeliac disease in the elderly: a biopsy-proven population-based study. Dig Liver Dis 2008;40:809-13. [DOI] [PubMed] [Google Scholar]
- 9.Dube C, Rostom A, Sy R, et al. The prevalence of celiac disease in average-risk and at-risk Western European populations: a systematic review. Gastroenterology 2005;128:S57-67. [DOI] [PubMed] [Google Scholar]
- 10.Kang JY, Kang AH, Green A, et al. Systematic review: worldwide variation in the frequency of coeliac disease and changes over time. Aliment Pharmacol Ther 2013;38:226-45. [DOI] [PubMed] [Google Scholar]
- 11.Katz KD, Rashtak S, Lahr BD, et al. Screening for celiac disease in a north american population: sequential serology and gastrointestinal symptoms. Am J Gastroenterol 2011;106:1333-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fasano A, Berti I, Gerarduzzi T, et al. Prevalence of celiac disease in at-risk and not-at-risk groups in the United States: a large multicenter study. Arch Intern Med 2003;163:286-92. [DOI] [PubMed] [Google Scholar]
- 13.Mardini HE, Westgate P, Grigorian AY. Racial differences in the prevalence of celiac disease in the US population: National Health and Nutrition Examination Survey (NHANES) 2009-2012. Dig Dis Sci 2015;60:1738-42. [DOI] [PubMed] [Google Scholar]
- 14.West J, Fleming KM, Tata LJ, et al. Incidence and prevalence of celiac disease and dermatitis herpetiformis in the UK over two decades: population-based study. Am J Gastroenterol 2014;109:757-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mustalahti K, Catassi C, Reunanen A, et al. The prevalence of celiac disease in Europe: results of a centralized, international mass screening project. Ann Med 2010;42:587-95. [DOI] [PubMed] [Google Scholar]
- 16.Yuan J, Gao J, Li X, et al. The tip of the “celiac iceberg” in China: a systematic review and meta-analysis. PLoS One 2013;8:e81151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Makharia GK, Verma AK, Amarchand R, et al. Prevalence of celiac disease in the northern part of India: a community based study. J Gastroenterol Hepatol 2011;26:894-900. [DOI] [PubMed] [Google Scholar]
- 18.Cataldo F, Lio D, Simpore J, et al. Consumption of wheat foodstuffs not a risk for celiac disease occurrence in burkina faso. J Pediatr Gastroenterol Nutr 2002;35:233-4. [DOI] [PubMed] [Google Scholar]
- 19.Ludvigsson JF, Brandt L, Montgomery SM, et al. Validation study of villous atrophy and small intestinal inflammation in Swedish biopsy registers. BMC Gastroenterol 2009;9:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abdul Sultan A, Crooks CJ, Card T, et al. Causes of death in people with coeliac disease in England compared with the general population: a competing risk analysis. Gut 2015;64:1220-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ivarsson A, Persson LA, Nystrom L, et al. Epidemic of coeliac disease in Swedish children [see comments]. Acta Paediatr 2000;89:165-71. [DOI] [PubMed] [Google Scholar]
- 22.Lohi S, Mustalahti K, Kaukinen K, et al. Increasing prevalence of coeliac disease over time. Aliment Pharmacol Ther 2007;26:1217-25. [DOI] [PubMed] [Google Scholar]
- 23.Catassi C, Kryszak D, Bhatti B, et al. Natural history of celiac disease autoimmunity in a USA cohort followed since 1974. Ann Med 2010;42:530-8. [DOI] [PubMed] [Google Scholar]
- 24.Biagi F, Campanella J, Bianchi PI, et al. The incidence of coeliac disease in adult first degree relatives. Dig Liver Dis 2008;40:97-100. [DOI] [PubMed] [Google Scholar]
- 25.Vriezinga SL, Auricchio R, Bravi E, et al. Randomized feeding intervention in infants at high risk for celiac disease. N Engl J Med 2014;371:1304-15. [DOI] [PubMed] [Google Scholar]
- 26.Lionetti E, Castellaneta S, Francavilla R, et al. Introduction of gluten, HLA status, and the risk of celiac disease in children. N Engl J Med 2014;371:1295-303. [DOI] [PubMed] [Google Scholar]
- 27.Murray JA, Van Dyke C, Plevak MF, et al. Trends in the identification and clinical features of celiac disease in a North American community, 1950-2001. Clin Gastroenterol Hepatol 2003;1:19-27. [DOI] [PubMed] [Google Scholar]
- 28.Ludvigsson JF, Rubio-Tapia A, van Dyke CT, et al. Increasing incidence of celiac disease in a north American population. Am J Gastroenterol 2013;108:818-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nistico L, Fagnani C, Coto I, et al. Concordance, disease progression, and heritability of coeliac disease in Italian twins. Gut 2006;55:803-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Catassi C, Ratsch IM, Gandolfi L, et al. Why is coeliac disease endemic in the people of the Sahara? Lancet 1999;354:647-8. [DOI] [PubMed] [Google Scholar]
- 31.Ivarsson A, Hernell O, Stenlund H, et al. Breast-feeding protects against celiac disease. Am J Clin Nutr 2002;75:914-21. [DOI] [PubMed] [Google Scholar]
- 32.Roberts SE, Williams JG, Meddings D, et al. Perinatal risk factors and coeliac disease in children and young adults: a record linkage study. Aliment Pharmacol Ther 2009;29:222-31. [DOI] [PubMed] [Google Scholar]
- 33.Welander A, Tjernberg AR, Montgomery SM, et al. Infectious disease and risk of later celiac disease in childhood. Pediatrics 2010;125:e530-6. [DOI] [PubMed] [Google Scholar]
- 34.Aronsson CA, Lee HS, Liu E, et al. Age at gluten introduction and risk of celiac disease. Pediatrics 2015;135:239-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Marild K, Stephansson O, Montgomery S, et al. Pregnancy outcome and risk of celiac disease in offspring: a nationwide case-control study. Gastroenterology 2012;142:39-45.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hyoty H, Hiltunen M, Knip M, et al. A prospective study of the role of coxsackie B and other enterovirus infections in the pathogenesis of IDDM. Childhood Diabetes in Finland (DiMe) Study Group. Diabetes 1995;44:652-7. [DOI] [PubMed] [Google Scholar]
- 37.Kagnoff MF, Paterson YJ, Kumar PJ, et al. Evidence for the role of a human intestinal adenovirus in the pathogenesis of coeliac disease. Gut 1987;28:995-1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stene LC, Honeyman MC, Hoffenberg EJ, et al. Rotavirus infection frequency and risk of celiac disease autoimmunity in early childhood: a longitudinal study. Am J Gastroenterol 2006;101:2333-40. [DOI] [PubMed] [Google Scholar]
- 39.Riddle MS, Murray JA, Porter CK. The incidence and risk of celiac disease in a healthy US adult population. Am J Gastroenterol 2012;107:1248-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Decker E, Engelmann G, Findeisen A, et al. Cesarean delivery is associated with celiac disease but not inflammatory bowel disease in children. Pediatrics 2010;125:e1433-40. [DOI] [PubMed] [Google Scholar]
- 41.Lebwohl B, Blaser MJ, Ludvigsson JF, et al. Decreased risk of celiac disease in patients with Helicobacter pylori colonization. Am J Epidemiol 2013;178:1721-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Austin AS, Logan RF, Thomason K, et al. Cigarette smoking and adult coeliac disease. Scand J Gastroenterol 2002;37:978-82. [DOI] [PubMed] [Google Scholar]
- 43.Snook JA, Dwyer L, Lee-Elliott C, et al. Adult coeliac disease and cigarette smoking [see comments]. Gut 1996;39:60-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vazquez H, Smecuol E, Flores D, et al. Relation between cigarette smoking and celiac disease: evidence from a case-control study. Am J Gastroenterol 2001;96:798-802. [DOI] [PubMed] [Google Scholar]
- 45.Ludvigsson JF, Montgomery SM, Ekbom A. Smoking and celiac disease: a population-based cohort study. Clin Gastroenterol Hepatol 2005;3:869-74. [DOI] [PubMed] [Google Scholar]
- 46.Lebwohl B, Spechler SJ, Wang TC, et al. Use of proton pump inhibitors and subsequent risk of celiac disease. Dig Liver Dis 2014;46:36-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Marild K, Ye W, Lebwohl B, et al. Antibiotic exposure and the development of coeliac disease: a nationwide case-control study. BMC Gastroenterol 2013;13:109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lundin KE, Scott H, Hansen T, et al. Gliadin-specific, HLA-DQ(alpha 1*0501,beta 1*0201) restricted T cells isolated from the small intestinal mucosa of celiac disease patients. J Exp Med 1993;178:187-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Green PH, Lebwohl B, Greywoode R. Celiac disease. J Allergy Clin Immunol 2015;135:1099-106; quiz 1107. [DOI] [PubMed] [Google Scholar]
- 50.Shan L, Molberg O, Parrot I, et al. Structural basis for gluten intolerance in celiac sprue. Science 2002;297:2275-9. [DOI] [PubMed] [Google Scholar]
- 51.Matysiak-Budnik T, Moura IC, Arcos-Fajardo M, et al. Secretory IgA mediates retrotranscytosis of intact gliadin peptides via the transferrin receptor in celiac disease. T J Exp Med 2008;205:143-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Visser J, Rozing J, Sapone A, et al. Tight junctions, intestinal permeability, and autoimmunity: celiac disease and type 1 diabetes paradigms. Ann N Y Acad Sci 2009;1165:195-205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sollid LM. Coeliac disease: dissecting a complex inflammatory disorder. Nat Rev Immunol 2002;2:647-55. [DOI] [PubMed] [Google Scholar]
- 54.Nilsen EM, Jahnsen FL, Lundin KE, et al. Gluten induces an intestinal cytokine response strongly dominated by interferon gamma in patients with celiac disease. Gastroenterology 1998;115:551-63. [DOI] [PubMed] [Google Scholar]
- 55.Mohamed BM, Feighery C, Kelly J, et al. Increased protein expression of matrix metalloproteinases -1, -3, and -9 and TIMP-1 in patients with gluten-sensitive enteropathy. Dig Dis Sci 2006;51:1862-8. [DOI] [PubMed] [Google Scholar]
- 56.Taylor TB, Schmidt LA, Meyer LJ, et al. Transglutaminase 3 present in the IgA aggregates in dermatitis herpetiformis skin is enzymatically active and binds soluble fibrinogen. J Invest Dermatol 2015;135:623-5. [DOI] [PubMed] [Google Scholar]
- 57.Mention JJ, Ben Ahmed M, Begue B, et al. Interleukin 15: a key to disrupted intraepithelial lymphocyte homeostasis and lymphomagenesis in celiac disease. Gastroenterology 2003;125:730-45. [DOI] [PubMed] [Google Scholar]
- 58.Tang F, Chen Z, Ciszewski C, et al. Cytosolic PLA2 is required for CTL-mediated immunopathology of celiac disease via NKG2D and IL-15. J Exp Med 2009;206:707-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Junker Y, Zeissig S, Kim SJ, et al. Wheat amylase trypsin inhibitors drive intestinal inflammation via activation of toll-like receptor 4. J Exp Med 2012;209:2395-408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rampertab SD, Pooran N, Brar P, et al. Trends in the presentation of celiac disease. Am J Med 2006;119:355 e9-14. [DOI] [PubMed] [Google Scholar]
- 61.Reilly NR, Aguilar K, Hassid BG, et al. Celiac disease in normal-weight and overweight children: clinical features and growth outcomes following a gluten-free diet. J Pediatr Gastroenterol Nutr 2011;53:528-31. [DOI] [PubMed] [Google Scholar]
- 62.Rizkalla Reilly N, Dixit R, Simpson S, et al. Celiac disease in children: an old disease with new features. Minerva Pediatr 2012;64:71-81. [PubMed] [Google Scholar]
- 63.Harper JW, Holleran SF, Ramakrishnan R, et al. Anemia in celiac disease is multifactorial in etiology. Am J Hematol 2007;82:996-1000. [DOI] [PubMed] [Google Scholar]
- 64.Sanders DS, Hopper AD, Azmy IA, et al. Association of adult celiac disease with surgical abdominal pain: a case-control study in patients referred to secondary care. Ann Surg 2005;242:201-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hadjivassiliou M, Duker AP, Sanders DS. Gluten-related neurologic dysfunction. Handb Clin Neurol 2014;120:607-19. [DOI] [PubMed] [Google Scholar]
- 66.Volta U, Caio G, Stanghellini V, et al. The changing clinical profile of celiac disease: a 15-year experience (1998-2012) in an Italian referral center. BMC Gastroenterol 2014;14:194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Green PH, Cellier C. Celiac disease. N Engl J Med 2007;357:1731-43. [DOI] [PubMed] [Google Scholar]
- 68.Nachman F, Vazquez H, Gonzalez A, et al. Gastroesophageal reflux symptoms in patients with celiac disease and the effects of a gluten-free diet. Clin Gastroenterol Hepatol 2011;9:214-9. [DOI] [PubMed] [Google Scholar]
- 69.Cheng J, Brar PS, Lee AR, et al. Body mass index in celiac disease: beneficial effect of a gluten-free diet. J Clin Gastroenterol 2010;44:267-71. [DOI] [PubMed] [Google Scholar]
- 70.Kabbani TA, Goldberg A, Kelly CP, et al. Body mass index and the risk of obesity in coeliac disease treated with the gluten-free diet. Aliment Pharmacol Ther 2012;35:723-9. [DOI] [PubMed] [Google Scholar]
- 71.Dixit R, Lebwohl B, Ludvigsson JF, et al. Celiac disease is diagnosed less frequently in young adult males. Dig Dis Sci 2014;59:1509-12. [DOI] [PubMed] [Google Scholar]
- 72.Hill ID, Dirks MH, Liptak GS, et al. Guideline for the diagnosis and treatment of celiac disease in children: recommendations of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr 2005;40:1-19. [DOI] [PubMed] [Google Scholar]
- 73.NIH Consensus Development Conference on Celiac Disease. http://consensus.nih.gov/2004/2004CeliacDisease118html.htm. [PubMed]
- 74.Ludvigsson JF, Bai JC, Biagi F, et al. Diagnosis and management of adult coeliac disease: guidelines from the British Society of Gastroenterology. Gut 2014;63:1210-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Peters U, Askling J, Gridley G, et al. Causes of death in patients with celiac disease in a population-based Swedish cohort. Arch Intern Med 2003;163:1566-72. [DOI] [PubMed] [Google Scholar]
- 76.West J, Logan RF, Smith CJ, et al. Malignancy and mortality in people with coeliac disease: population based cohort study. BMJ 2004;329:716-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Elfstrom P, Granath F, Ekstrom Smedby K, et al. Risk of lymphoproliferative malignancy in relation to small intestinal histopathology among patients with celiac disease. J Natl Cancer Inst 2011;103:436-44. [DOI] [PubMed] [Google Scholar]
- 78.Tio M, Cox MR, Eslick GD. Meta-analysis: coeliac disease and the risk of all-cause mortality, any malignancy and lymphoid malignancy. Aliment Pharmacol Ther 2012;35:540-51. [DOI] [PubMed] [Google Scholar]
- 79.Ilus T, Kaukinen K, Virta LJ, et al. Incidence of malignancies in diagnosed celiac patients: a population-based estimate. Am J Gastroenterol 2014;109:1471-7. [DOI] [PubMed] [Google Scholar]
- 80.Lebwohl B, Granath F, Ekbom A, et al. Mucosal healing and risk for lymphoproliferative malignancy in celiac disease: a population-based cohort study. Ann Intern Med 2013;159:169-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Elfstrom P, Granath F, Ye W, et al. Low risk of gastrointestinal cancer among patients with celiac disease, inflammation, or latent celiac disease. Clin Gastroenterol Hepatol 2012;10:30-6. [DOI] [PubMed] [Google Scholar]
- 82.Ludvigsson JF, Fall K, Montgomery S. Risk of prostate cancer in a population-based cohort of men with coeliac disease. Br J Cancer 2012;106:217-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ludvigsson JF, West J, Ekbom A, et al. Reduced risk of breast, endometrial and ovarian cancer in women with celiac disease. Int J Cancer 2012;131:E244-50. [DOI] [PubMed] [Google Scholar]
- 84.Gutierrez-Achury J, Coutinho de Almeida R, Wijmenga C. Shared genetics in coeliac disease and other immune-mediated diseases. J Intern Med 2011;269:591-603. [DOI] [PubMed] [Google Scholar]
- 85.Van Heel DA, Franke L, Hunt KA, et al. A genome-wide association study for celiac disease identifies risk variants in the region harboring IL2 and IL21. Nat Genet 2007;39:827-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Smyth DJ, Plagnol V, Walker NM, et al. Shared and distinct genetic variants in type 1 diabetes and celiac disease. N Engl J Med 2008;359:2767-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Hadithi M, de Boer H, Meijer JW, et al. Coeliac disease in Dutch patients with Hashimoto’s thyroiditis and vice versa. World J Gastroenterol 2007;13:1715-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Elfstrom P, Montgomery SM, Kampe O, et al. Risk of thyroid disease in individuals with celiac disease. J Clin Endocrinol Metab 2008;93:3915-21. [DOI] [PubMed] [Google Scholar]
- 89.Aggarwal S, Lebwohl B, Green PH. Screening for celiac disease in average-risk and high-risk populations. Ther Adv Gastroenterol 2012;5:37-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Mirzaagha F, Azali SH, Islami F, et al. Coeliac disease in autoimmune liver disease: a cross-sectional study and a systematic review. Dig Liver Dis 2010;42:620-3. [DOI] [PubMed] [Google Scholar]
- 91.Kaukinen K, Halme L, Collin P, et al. Celiac disease in patients with severe liver disease: gluten-free diet may reverse hepatic failure. Gastroenterology 2002;122:881-8. . [DOI] [PubMed] [Google Scholar]
- 92.Sadr-Azodi O, Sanders DS, Murray JA, et al. Patients with celiac disease have an increased risk for pancreatitis. Clin Gastroenterol Hepatol 2012;10:1136-42 e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Evans KE, Leeds JS, Morley S, et al. Pancreatic insufficiency in adult celiac disease: do patients require long-term enzyme supplementation? Dig Dis Sci 2010;55:2999-3004. [DOI] [PubMed] [Google Scholar]
- 94.Volta U, De Franceschi L, Lari F, et al. Coeliac disease hidden by cryptogenic hypertransaminasaemia. Lancet 1998;352:26-9. [DOI] [PubMed] [Google Scholar]
- 95.Sorensen HT, Thulstrup AM, Blomqvist P, et al. Risk of primary biliary liver cirrhosis in patients with coeliac disease: Danish and Swedish cohort data. Gut 1999;44:736-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ludvigsson JF, James S, Askling J, et al. Nationwide cohort study of risk of ischemic heart disease in patients with celiac disease. Circulation 2011;123:483-90. [DOI] [PubMed] [Google Scholar]
- 97.Emilsson L, Carlsson R, Holmqvist M, et al. The characterisation and risk factors of ischaemic heart disease in patients with coeliac disease. Aliment Pharmacol Ther 2013;37:905-14. [DOI] [PubMed] [Google Scholar]
- 98.West J, Logan RF, Card TR, et al. Risk of vascular disease in adults with diagnosed coeliac disease: a population-based study. Aliment Pharmacol Ther 2004;20:73-9. [DOI] [PubMed] [Google Scholar]
- 99.West J, Logan RF, Hill PG, et al. Seroprevalence, correlates, and characteristics of undetected coeliac disease in England. Gut 2003;52:960-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Grainge MJ, West J, Card TR, et al. Causes of death in people with celiac disease spanning the pre- and post-serology era: a population-based cohort study from Derby, UK. Am J Gastroenterol 2011;106:933-9. [DOI] [PubMed] [Google Scholar]
- 101.Khashan AS, Henriksen TB, Mortensen PB, et al. The impact of maternal celiac disease on birthweight and preterm birth: a Danish population-based cohort study. Hum Reprod 2010;25:528-34. [DOI] [PubMed] [Google Scholar]
- 102.Ludvigsson JF, Montgomery SM, Ekbom A. Celiac disease and risk of adverse fetal outcome: a population-based cohort study. Gastroenterology 2005;129:454-63. [DOI] [PubMed] [Google Scholar]
- 103.Kiefte-de Jong JC, Jaddoe VW, Uitterlinden AG, et al. Levels of antibodies against tissue transglutaminase during pregnancy are associated with reduced fetal weight and birth weight. Gastroenterology 2013;144:726-35 e2. [DOI] [PubMed] [Google Scholar]
- 104.Martinelli P, Troncone R, Paparo F, et al. Coeliac disease and unfavourable outcome of pregnancy. Gut 2000;46:332-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Zugna D, Richiardi L, Stephansson O, et al. Risk of congenital malformations among offspring of mothers and fathers with celiac disease: a nationwide cohort study. Clin Gastroenterol Hepatol 2014;12:1108-16.e6. [DOI] [PubMed] [Google Scholar]
- 106.Zugna D, Richiardi L, Akre O, et al. A nationwide population-based study to determine whether coeliac disease is associated with infertility. Gut 2010;59:1471-5. [DOI] [PubMed] [Google Scholar]
- 107.Rubio-Tapia A, Rahim MW, See JA, et al. Mucosal recovery and mortality in adults with celiac disease after treatment with a gluten-free diet. Am J Gastroenterol 2010;105:1412-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Tuire I, Marja-Leena L, Teea S, et al. Persistent duodenal intraepithelial lymphocytosis despite a long-term strict gluten-free diet in celiac disease. Am J Gastroenterol 2012;107:1563-9. [DOI] [PubMed] [Google Scholar]
- 109.Lebwohl B, Murray JA, Rubio-Tapia A, et al. Predictors of persistent villous atrophy in coeliac disease: a population-based study. Aliment Pharmacol Ther 2014;39:488-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Lebwohl B, Granath F, Ekbom A, et al. Mucosal healing and mortality in coeliac disease. Aliment Pharmacol Ther 2013;37:332-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Lebwohl B, Emilsson L, Frobert O, et al. Mucosal healing and the risk of ischemic heart disease or atrial fibrillation in patients with celiac disease; a population-based study. PLoS One 2015;10:e0117529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Lebwohl B, Stephansson O, Green PH, et al. Mucosal healing in patients with celiac disease and outcomes of pregnancy: a nationwide population-based study. Clin Gastroenterol Hepatol 2015;13:1111-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Lebwohl B, Michaelsson K, Green PH, et al. Persistent mucosal damage and risk of fracture in celiac disease. J Clin Endocrinol Metab 2014;99:609-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Sharkey LM, Corbett G, Currie E, et al. Optimising delivery of care in coeliac disease—comparison of the benefits of repeat biopsy and serological follow-up. Aliment Pharmacol Ther 2013;38:1278-91. [DOI] [PubMed] [Google Scholar]
- 115.Rubio-Tapia A, Hill ID, Kelly CP, et al; American College of Gastroenterology. ACG clinical guidelines: diagnosis and management of celiac disease. Am J Gastroenterol 2013;108:656-76; quiz 77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Murray JA, Watson T, Clearman B, et alF. Effect of a gluten-free diet on gastrointestinal symptoms in celiac disease. Am J Clin Nutr 2004;79:669-73. [DOI] [PubMed] [Google Scholar]
- 117.Lee AR, Ng DL, Zivin J, Green PH. Economic burden of a gluten-free diet. J Hum Nutr Diet 2007;20:423-30. [DOI] [PubMed] [Google Scholar]
- 118.Shah S, Akbari M, Vanga R, et al. Patient perception of treatment burden is high in celiac disease compared with other common conditions. Am J Gastroenterol 2014;109:1304-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Leffler DA, Dennis M, Hyett B, et al. Etiologies and predictors of diagnosis in nonresponsive celiac disease. Clin Gastroenterol Hepatol 2007;5:445-50. [DOI] [PubMed] [Google Scholar]
- 120.Tennyson CA, Simpson S, Lebwohl B, et al. Interest in medical therapy for celiac disease. Ther Adv Gastroenterol 2013;6:358-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Mukherjee R, Kelly CP, Schuppan D. Nondietary therapies for celiac disease. Gastointest Endosc Clin N Am 2012;22:811-31. [DOI] [PubMed] [Google Scholar]
- 122.Leffler DA, Kelly CP, Abdallah HZ, et al. A randomized, double-blind study of larazotide acetate to prevent the activation of celiac disease during gluten challenge. Am J Gastroenterol 2012;107:1554-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Kelly CP, Green PH, Murray JA, et al. Larazotide acetate in patients with coeliac disease undergoing a gluten challenge: a randomised placebo-controlled study. Aliment Pharmacol Ther 2013;37:252-62. [DOI] [PubMed] [Google Scholar]
- 124.Lahdeaho ML, Kaukinen K, Laurila K, et al. Glutenase ALV003 attenuates gluten-induced mucosal injury in patients with celiac disease. Gastroenterology 2014;146:1649-58. [DOI] [PubMed] [Google Scholar]
- 125.Catassi C, Bai JC, Bonaz B, et al. Non-celiac gluten sensitivity: the new frontier of gluten related disorders. Nutrients 2013;5:3839-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Aziz I, Lewis NR, Hadjivassiliou M, et al. A UK study assessing the population prevalence of self-reported gluten sensitivity and referral characteristics to secondary care. Eur J Gastroenterol Hepatol 2014;26:33-9. [DOI] [PubMed] [Google Scholar]
- 127.Golley S, Corsini N, Topping D, et al. Motivations for avoiding wheat consumption in Australia: results from a population survey. Public Health Nutr 2015;18:490-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Digiacomo DV, Tennyson CA, Green PH, et al. Prevalence of gluten-free diet adherence among individuals without celiac disease in the USA: results from the continuous national health and nutrition examination survey 2009-2010. Scand J Gastroenterol 2013;48:921-5. [DOI] [PubMed] [Google Scholar]
- 129.Volta U, Bardella MT, Calabro A, et al. An Italian prospective multicenter survey on patients suspected of having non-celiac gluten sensitivity. BMC Med 2014;12:85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Lis D, Stellingwerff T, Shing CM, et al. Exploring the popularity, experiences and beliefs surrounding gluten-free diets in non-coeliac athletes. Int J Sport Nutr Exerc Metab 2015;25:37-45. [DOI] [PubMed] [Google Scholar]
- 131.Ellis A, Linaker BD. Non-coeliac gluten sensitivity? Lancet 1978;1:1358-9. [DOI] [PubMed] [Google Scholar]
- 132.Cooper BT, Holmes GK, Ferguson R, et al. Gluten-sensitive diarrhea without evidence of celiac disease. Gastroenterology 1980;79:801-6. [PubMed] [Google Scholar]
- 133.Tavakkoli A, Lewis SK, Tennyson CA, et al. Characteristics of patients who avoid wheat and/or gluten in the absence of celiac disease. Dig Dis Sci 2014;59:1255-61. [DOI] [PubMed] [Google Scholar]
- 134.Biesiekierski JR, Newnham ED, Shepherd SJ, et al. Characterization of adults with a self-diagnosis of nonceliac gluten sensitivity. Nutr Clin Pract 2014;29:504-9. [DOI] [PubMed] [Google Scholar]
- 135.Brottveit M, Beitnes AC, Tollefsen S, et al. Mucosal cytokine response after short-term gluten challenge in celiac disease and non-celiac gluten sensitivity. Am J Gastroenterol 2013;108:842-50. [DOI] [PubMed] [Google Scholar]
- 136.Biesiekierski JR, Newnham ED, Irving PM, et al. Gluten causes gastrointestinal symptoms in subjects without celiac disease: a double-blind randomized placebo-controlled trial. Am J Gastroenterol 2011;106:508-14. [DOI] [PubMed] [Google Scholar]
- 137.Vazquez-Roque MI, Camilleri M, Smyrk T, et al. A controlled trial of gluten-free diet in patients with irritable bowel syndrome-diarrhea: effects on bowel frequency and intestinal function. Gastroenterology 2013;144:903-11.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Biesiekierski JR, Peters SL, Newnham ED, et al. No effects of gluten in patients with self-reported non-celiac gluten sensitivity after dietary reduction of fermentable, poorly absorbed, short-chain carbohydrates. Gastroenterology 2013;145:320-8.e1-3. [DOI] [PubMed] [Google Scholar]
- 139.Di Sabatino A, Volta U, Salvatore C, et al. Small amounts of gluten in subjects with suspected nonceliac gluten sensitivity: a randomized, double-blind, placebo-controlled, cross-over trial. Clin Gastroenterol Hepatol 2015; published online 19 Feb. [DOI] [PubMed]
- 140.Hollon J, Puppa EL, Greenwald B, et al. Effect of gliadin on permeability of intestinal biopsy explants from celiac disease patients and patients with non-celiac gluten sensitivity. Nutrients 2015;7:1565-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Sapone A, Lammers KM, Casolaro V, et al. Divergence of gut permeability and mucosal immune gene expression in two gluten-associated conditions: celiac disease and gluten sensitivity. BMC Med 2011;9:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Huebener S, Tanaka CK, Uhde M, et al. Specific nongluten proteins of wheat are novel target antigens in celiac disease humoral response. J Proteome Res 2015;14:503-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Caio G, Volta U, Tovoli F, et al. Effect of gluten free diet on immune response to gliadin in patients with non-celiac gluten sensitivity. BMC Gastroenterol 2014;14:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Eaton WW, Byrne M, Ewald H, et al. Association of schizophrenia and autoimmune diseases: linkage of danish national registers. Am J Psychiatry 2006;163:521-8. [DOI] [PubMed] [Google Scholar]
- 145.Chin RL, Sander HW, Brannagan TH, et al. Celiac neuropathy. Neurology 2003;60:1581-5. [DOI] [PubMed] [Google Scholar]
- 146.Cascella NG, Kryszak D, Bhatti B, et al. Prevalence of celiac disease and gluten sensitivity in the United States clinical antipsychotic trials of intervention effectiveness study population. Schizophr Bull 2011;37:94-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Samaroo D, Dickerson F, Kasarda DD, et al. Novel immune response to gluten in individuals with schizophrenia. Schizophr Res 2010;118:248-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Dickerson F, Stallings C, Origoni A, et al. Markers of gluten sensitivity and celiac disease in recent-onset psychosis and multi-episode schizophrenia. Biol Psychiatry 2010;68:100-4. [DOI] [PubMed] [Google Scholar]
- 149.Lau NM, Green PH, Taylor AK, et al. Markers of celiac disease and gluten sensitivity in children with autism. PLoS One 2013;8:e66155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Ludvigsson JF, Reichenberg A, Hultman CM, et al. A nationwide study of the association between celiac disease and the risk of autistic spectrum disorders. JAMA Psychiatry 2013;70:1224-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Ludvigsson JF, Green PH. The missing environmental factor in celiac disease. N Engl J Med 2014;371:1341-3. [DOI] [PubMed] [Google Scholar]
- 152.Lebwohl B, Ludvigsson JF, Green PH. The unfolding story of celiac disease risk factors. Clin Gastroenterol Hepatol 2014;12:632-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Nadal I, Donat E, Ribes-Koninckx C, et al. Imbalance in the composition of the duodenal microbiota of children with coeliac disease. J Med Microbiol 2007;56:1669-74. [DOI] [PubMed] [Google Scholar]
- 154.Olivares M, Neef A, Castillejo G, et al. The HLA-DQ2 genotype selects for early intestinal microbiota composition in infants at high risk of developing coeliac disease. Gut 2015;64:406-17. [DOI] [PubMed] [Google Scholar]
- 155.Simell S, Hoppu S, Hekkala A, et al. Fate of five celiac disease-associated antibodies during normal diet in genetically at-risk children observed from birth in a natural history study. Am J Gastroenterol 2007;102:2026-35. [DOI] [PubMed] [Google Scholar]
- 156.Mahadev S, Bhagat G, Green PH. Transient celiac autoimmunity in an adult. J Clin Gastroenterol 2011;45:912-3. [DOI] [PubMed] [Google Scholar]
- 157.Mooney PD, Wong SH, Johnston AJ, et al. Increased detection of celiac disease with measurement of deamidated gliadin peptide antibody before endoscopy. Clin Gastroenterol Hepatol 2015;13:1278-84.e1. [DOI] [PubMed] [Google Scholar]
- 158.Lebwohl B, Bhagat G, Markoff S, et al. Prior endoscopy in patients with newly diagnosed celiac disease: a missed opportunity? Dig Dis Sci 2013;58:1293-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Adriaanse MP, Tack GJ, Passos VL, et al. Serum I-FABP as marker for enterocyte damage in coeliac disease and its relation to villous atrophy and circulating autoantibodies. Aliment Pharmacol Ther 2013;37:482-90. [DOI] [PubMed] [Google Scholar]
- 160.Comino I, Real A, Vivas S, et al. Monitoring of gluten-free diet compliance in celiac patients by assessment of gliadin 33-mer equivalent epitopes in feces. Am J Clin Nutr 2012;95:670-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Catassi C, Fabiani E, Iacono G, et al. A prospective, double-blind, placebo-controlled trial to establish a safe gluten threshold for patients with celiac disease. Am J Clin Nutr 2007;85:160-6. [DOI] [PubMed] [Google Scholar]
- 162.Fuchs V, Kurppa K, Huhtala H, et al. Factors associated with long diagnostic delay in celiac disease. Scand J Gastroenterol 2014:1-7. [DOI] [PubMed]
- 163.Master S, Lebwohl B, Ludvigsson JF, et al. Bibliometric study of the quality of celiac disease research publications. J Pediatr Gastroenterol Nutr 2013;57:527-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Narotsky D, Green PH, Lebwohl B. Temporal and geographic trends in celiac disease publications: a bibliometric analysis. Eur J Gastroenterol Hepatol 2012;24:1071-7. [DOI] [PubMed] [Google Scholar]
- 165.Smukalla S, Lebwohl B, Mears JG, et al. How often do hematologists consider celiac disease in iron-deficiency anemia? Results of a national survey. Clin Adv Hematol Oncol 2014;12:100-5. [PubMed] [Google Scholar]
- 166.Simpson SM, Ciaccio EJ, Case S, et al. Celiac disease in patients with type 1 diabetes: screening and diagnostic practices. Diabetes Educ 2013;39:532-40. [DOI] [PubMed] [Google Scholar]
- 167.Collin P, Huhtala H, Virta L, et al. Diagnosis of celiac disease in clinical practice: physician’s alertness to the condition essential. J Clin Gastroenterol 2007;41:152-6. [DOI] [PubMed] [Google Scholar]
- 168.Catassi C, Kryszak D, Louis-Jacques O, et al. Detection of celiac disease in primary care: a multicenter case-finding study in North America. Am J Gastroenterol 2007;102:1454-60. [DOI] [PubMed] [Google Scholar]
- 169.Bai JC, Fried M, Corazza GR, et al. World Gastroenterology Organisation global guidelines on celiac disease. J Clin Gastroenterol 2013;47:121-6. [DOI] [PubMed] [Google Scholar]
- 170.Husby S, Koletzko S, Korponay-Szabo IR, et al. European Society for Pediatric Gastroenterology, Hepatology, and Nutrition guidelines for the diagnosis of coeliac disease. J Pediatr Gastroenterol Nutr 2012;54:136-60. [DOI] [PubMed] [Google Scholar]