Abstract
Strategic purchasing is one of the key policy instruments to achieve the universal health coverage (UHC) goals of improved and equitable access and financial risk protection. Given favourable outcomes of Universal Coverage Scheme (UCS), this study synthesized strategic purchasing experiences in the National Health Security Office (NHSO) responsible for the UCS in contributing to achieving UHC goals. The UCS applied the purchaser–provider split concept where NHSO, as a purchaser, is in a good position to enforce accountability by public and private providers to the UCS beneficiaries, through active purchasing. A comprehensive benefit package resulted in high level of financial risk protection as reflected by low incidence of catastrophic health spending and impoverished households. The NHSO contracted the District Health System (DHS) network, to provide outpatient, health promotion and disease prevention services to the whole district population, based on an annual age-adjusted capitation payment. In most cases, the DHS was the only provider in a district without competitors. Geographical monopoly hampered the NHSO to introduce a competitive contractual agreement, but a durable, mutually dependent relationship based on trust was gradually evolved, while accreditation is an important channel for quality improvement. Strategic purchasing services from DHS achieved a pro-poor utilization due to geographical proximity, where travel time and costs were minimal. Inpatient services paid by Diagnostic Related Group within a global budget ceiling, which is estimated based on unit costs, admission rates and admission profiles, contained cost effectively. To prevent potential under-provisions of the services, some high cost interventions were unbundled from closed end payment and paid on an agreed fee schedule. Executing monopsonistic purchasing power by NHSO brought down price of services given assured quality. Cost saving resulted in more patients served within a finite annual budget.
Keywords: Universal health coverage, universal coverage scheme, Thailand, purchasing functions
Introduction
In 2001, prior to the achievement of universal health coverage (UHC), ∼30% of the Thai population were uninsured despite a gradual extension of coverage to various population groups (Tangcharoensathien et al. 2009). In 2002, >98% of population were covered by one of the three financial risk protection schemes: Civil Servant Medical Benefit Scheme (CSMBS) for public employees and dependants, Social Health Insurance (SHI) for private employees and Universal Coverage Scheme (UCS) for the remaining population who were not covered by the former two Schemes. Though benefit package was quite similar across the three schemes, the CSMBS pays outpatient (OP) services based on fee for service resulting in a high level of per capita expenditure, US$ 366 in 2011, 3.8 times higher than the UCS expenditure, Table 1.
Table 1.
Key characteristics across three public health insurance schemes, 2013
| UCS | SHI | CSMBS | |
|---|---|---|---|
| 1. Legal status | National Health Security Act | Social Security Act | Royal Decree |
| 2. Established since | 2002 | 1990 | 1980 |
| 3. Responsible agency | NHSO | MOL, Social Security Office | MOF, Comptroller General Dept. |
| 4. Population coverage, % of total | People who are not covered by SHI and CSMBS, 75% | Private sector employees, no dependents, 15% | Government employee, pensioners, dependants, 9% |
| 5. Financing sources | General tax, through annual budget bill | Tripartite, 4.5% payroll, 1.5% each | General tax, through annual budget bill |
| 6. Expenditure per capita, 2011 | 2900 Baht (US$ 97) | ∼2134 Baht (US$ 71) | ∼11 000 Baht (US$ 366) |
| 7. Benefit package | Comprehensive, small exclusion list | Comprehensive, small exclusion list | Comprehensive, no explicit exclusion list, private bed covered |
| 8. Prevention/promotion | Managed by NHSO for whole population since 2002 | ||
| 9. Providers | Mostly public network, typical DHS (DH + HCs) | Competing public, private hospitals > 100 beds (60% private) | Public provider only, selected disease (2011) |
| 10. Registration with provider | Required, limited choice to domicile district for OP | Required, annual choices if needed | Not required |
| 11. Choices of provider when ill | Limited to registered contractor network, plus referral | Limited to registered contractor hospital and its network | Free choice to any public, no referral required |
| 12. Choices of providers for accident and emergency services | Free choice | Free choice | Free choice |
| 13. Gate keeping function | Yes for OP | Yes for OP and IP | No |
| 14. Provider payment methods | OP: Capitation (age adjusted) | Capitation inclusive for OP and IP | OP: Fee-for-service |
| IP: DRG with global budget | DRG for IP DRG RW > 2 | IP: DRG multiple baserates, 2007 | |
| 15. Additional payment | Fee schedules for selected conditions or services | ||
| 16. Copayment | No, full pay when bypassing registered providers without proper referral | No, full pay outside contractor | Full pay in private |
MOF: Ministry of Finance, MOL: Ministry of Labor, DH + HCs: district hospitals and health centers, RW: Relative Weight, DRG: Diagnostic Related Group
UCS was selected for detail investigation as it covers the largest population. This article reviewed purchasing experiences for which the National Health Security Office (NHSO) who manages UCS had gradually developed and discussed how these purchasing functions contributed to the achievement of improved and equitable use of health service and financial risk protection to its members.
Document reviews were conducted; main sources were NHSO archives mostly grey documents related to UCS operations, e.g. minutes of the meetings of NHSO Governing Board and its related sub-committees such as Benefit, Finance and Budget, purchased price of goods and services after negotiation and its annual report. Published literatures related to UCS outcome were retrieved.
Findings
UCS performance
Improved and equitable access
The UCS members were entitled to free services at their registered District Health System (DHS) network; an increased utilization was observed both OP and inpatient (IP) services (Tangcharoensathien et al. 2013). Not only use rate increased, but also pro-poor utilization especially at health centres, district hospitals for OP and IP was observed. The DHS network in each district, consisting of 10–15 sub-district health centres and a district hospital—so called the ‘close to client’ provider was contracted based on capitation to provide OP services to the catchment population (Prakongsai 2008).
Using a difference-in-difference method (Limwattananon et al. 2013), a causal impact of UCS resulted in a reduced probability that a reported ill person did not have formal treatment and an increased probability of the use of public OP service, mostly provided by district hospitals and of IP in a public hospital. These effects are largest for the elderly. An increase in the OP utilization was greatest among the poor and rural residents, whereas there is a significant impact on IP care only among urban population. There was no evidence of crowding out of private formal care, reflecting that UCS reform made care more accessible to individuals previously financially deterred from utilization. Removal of user fees at public care appeared not to have induced users of private facilities to switch to the public sector, which may indicate convenience gaps between public and private providers.
It is noted that primary care services in Thailand are usually delivered by paramedics in health centres or general doctors in OP departments of district or provincial hospitals for which medicines were also dispensed. There are no primary care systems where family doctors or general practitioners diagnose and prescribe and patients receive medicines from another dispensary or pharmacies. Statistics showed increased OP utilization at district heath systems which beneficiaries can effectively use with low travel cost.
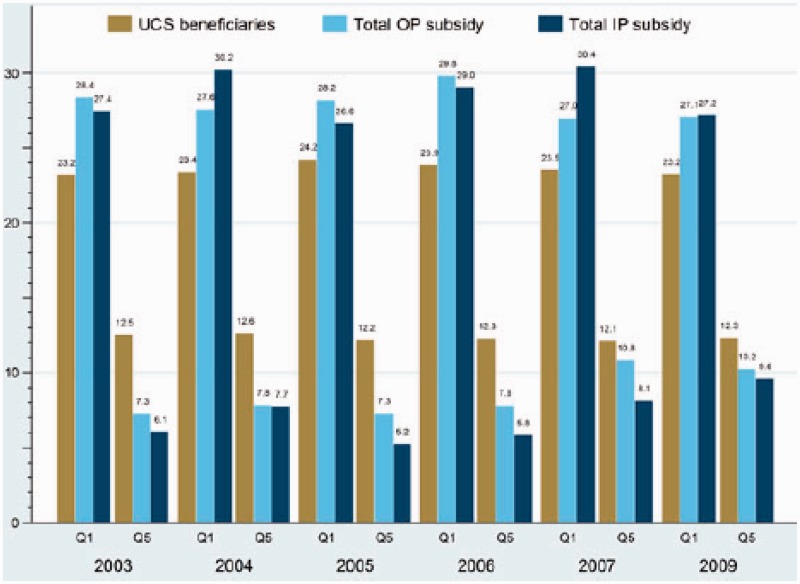
Prior to UHC in 2002, the government health spending, as measured by benefit incidence, was in favour of the poor (O’Donnell et al. 2007); a similar pro-poor trend continued in subsequent years, in particular at district and provincial hospitals. Subsidy for the OP service used by the poorest quintile of UCS members was 27–30% compared with their respective share of members, 23–24% of total UCS population, whereas the richest quintiles gained the benefit of 7–11% of the total subsidies, less than the population share, 12–13% of total UCS members (Limwattananon et al. 2012), see Figure 1.
Figure 1.
Distribution of OP and IP government subsidies by wealth quintile when compared with the UCS beneficiary distribution, 2003–2009
Financial risk protection
The predominant general tax financed UCS and CSMBS had led to an overall progressive financial incidence, where the rich contributed to health financing in a higher proportion of their income than the poor. The Concentration Indexes of financial contributions (ranges from −1 to +1, the more positive, the more progressive, where the rich pay higher proportion of their income to finance health) were consistently progressive (Prakongsai et al. 2009). See Table 2.
Table 2.
Progressivity of health financing contribution, 2003–2006
| Financing sources | 2002 |
2004 |
2006 |
|||
|---|---|---|---|---|---|---|
| CIa | Fractionb | CIa | Fractionb | CIa | Fractionb | |
| 1. Direct tax | 0.8221 | 0.20 | 0.8162 | 0.21 | 0.7687 | 0.23 |
| 2. Indirect tax | 0.5594 | 0.38 | 0.5958 | 0.37 | 0.5512 | 0.33 |
| 3. Social insurance contribution | 0.4975 | 0.06 | 0.4561 | 0.07 | 0.4492 | 0.08 |
| 4. Private insurance premium | 0.3785 | 0.09 | 0.4221 | 0.09 | 0.4188 | 0.08 |
| 5. Direct payment | 0.4883 | 0.27 | 0.4626 | 0.26 | 0.4705 | 0.28 |
| Overall | 0.5719 | 1.00 | 0.5822 | 1.00 | 0.5593 | 1.00 |
aConcentration index (CI) > 0 indicates concentration among the economically better off. This means ‘progressive’ taxation, where the rich pay relatively more than the poor.
bFraction of total health expenditure from National Health Accounts.
Source: Prakongsai et al. (2009).
A study by Limwattananon et al. (2013) demonstrated that mean household medical expenditures was reduced by one-third, whereas spending at the very top of the distribution of medical expenditures (i.e. the 95th conditional quantile) was reduced by one-half.
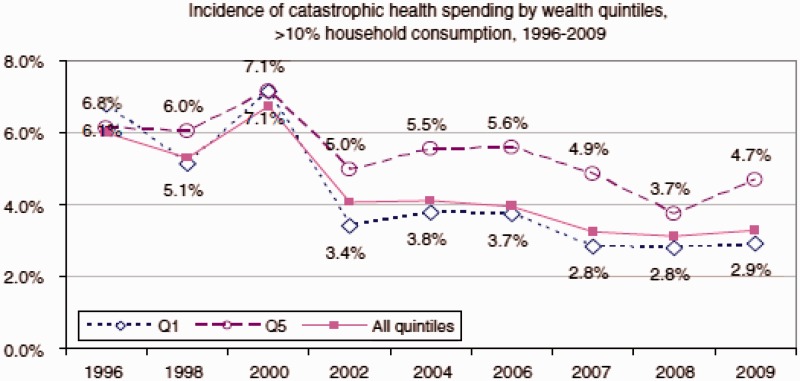
Financial risk protection had greatly improved; there was a minimal incidence of catastrophic health expenditure, as measured by household out-of-pocket payment for health exceeding 10% of total household consumption expenditure (Evans et al. 2012); see Figure 2. The incidence of medical impoverishment, as measured by an additional number of non-poor households falling under the national poverty lines as a result of health payments was low and decreasing (Limwattananon et al. 2007).
Figure 2.
Incidence of catastrophic health expenditure prior to universal coverage (1996–2000) and after universal coverage (2002–2009) national averages. Note: catastrophic health expenditure refers to household spending on health that exceeds 10% of total household consumption expenditure. Source: Computed by Limwattananon S using the national dataset of household socio-economic surveys conducted by the National Statistical Office. Source: Evans et al. (2012).
UCS strategic purchasing functions
Content analysis of the document reviews resulted in key strategies in six issues of the purchasing functions.
Design of benefit packages
For services to be included in benefit packages, UCS applies negative list concept—all diseases and services were covered except a few such as aesthetic surgeries and proven ineffective interventions. Maximum ceiling of financial coverage for each treatment was not applicable. Later in 2008 when Thailand had developed more capacity on health technology assessment (HTA) (Tangcharoensathien and Kamolratanakul 2008; Jongudomsuk et al. 2012), inclusion of new interventions into the UCS benefit package was guided by evidence through stringent economic evaluation, budget impact assessment and ethical concerns especially when there was limited supply-side capacities to offer such new services equitably.
Health Intervention and Technology Assessment Programme (HITAP) established in 2007 (HITAP 2013) as a research organization, contributed studies with major policy impacts, such as the economic evaluation of cervical cancer screening and human papilloma virus vaccines (Yothasamut et al. 2010). One Gross National Income per capita for a quality-adjusted life year was applied as a benchmark for public investment in health (Tantivess et al. 2009).
Renal replacement therapy (RRT) was initially excluded from the UCS benefit package due to its high cost (Kasemsup et al. 2006). UCS members faced catastrophic spending, whereas CSMBS and SHI fully covered (Prakongsai et al. 2007). RRT was heavily analysed over several years, including demand estimates (Kasemsup et al. 2006), cost-effectiveness analysis (Teerawattananon et al. 2007), policy analysis (Prakongsai et al. 2006) and public opinion surveys (Tangcharoensathien et al. 2006). Clearly, RRT was not cost-effective and contributed to long-term fiscal burden (Tangcharoensathien et al. 2005), especially given an increasing prevalence of diabetes and hypertension. Despite cost ineffective, the government in 2006 decided to include RRT into the UCS benefit package, to prevent catastrophic spending and ensure equity across all Schemes financed by public resources (Tangcharoensathien et al. 2013). Peritoneal dialysis first policy was adopted in view of equitable access by all, dialysis solution was delivered to health centres, for patient home dialysis result in minimum travelling cost. A full account of discussion on the outcomes of the peritoneal dialysis-first policy was reported (Tantivess et al. 2013). Table 3 lists disease conditions that were singled out from closed end payment and paid on an agreed fee schedule. Number of cases and unit costs were used to estimate total budget requirement and approval in a transparent way.
Table 3.
Specific diseases management and earmarked budget for UCS, Fiscal year (FY) 2014
| Disease management items | Percentage of budget | Target (cases) |
|---|---|---|
| 1. Asthma | 0.14 | 106 950 |
| 2. Tuberculosis | 0.19 | 51 180 |
| 3. Leukaemia and lymphoma, new cases | 0.12 | 1231 |
| 4. Cataract, including cost of soft lens | 0.75 | 119 425 |
| 5. Laser treatment for diabetic retinopathy | 0.03 | 15 026 |
| 6. Kidney stone using extracorporeal shock wave therapy | 0.32 | 38 900 |
| 7. Palliative care for end stage patients | 0.03 | 5961 |
| 8. Transplant (liver, heart, corneal, bone marrow and stem cell) | 0.06 | 150 |
| 9. ARV | 1.51 | 188 000 |
| 10. RRT | 3.48 | 35 429 |
| 11. Secondary prevention for diabetes and hypertension | 0.54 | 2 726 800 |
| Total budget, US$ million | 4960 |
ARV: Antiretrovirals.
Source: NHSO budget approved for fiscal year 2014.
Managing contracts: provider network as a gate keeper
When OP services were paid on a capitation basis, beneficiaries were required to register with a preferred provider network; typically, a DHS in their domicile district. When the beneficiary database was fully computerized a few years later, beneficiaries were allowed, four times a year, to register with another provider network they preferred especially among seasonal migrant workers such as taxi drivers and factory workers. Regular updates of electronic registries (birth, deaths, transfer across schemes and re-registrations) to all provider networks nationwide facilitate effective payment of capitation by NHSO.
Patients were entitled to services provided by their registered provider networks, while the network received an annual budget based on the capitation rate for OP service multiplied by total number of registries. The registered network, as a gate keeper, was liable to pay for the OP they referred to outside network out of its OP capitation budget. Patients bypassing without a proper referral were liable to pay OP services in full. Primary healthcare gate keeping function resulted in systems efficiency as most OP services can be and actually were provided by health centres and district hospitals with lower medical cost, time and transport costs shouldered by patients. Better outcome was noted, especially for chronic non-communicable diseases needing continual care, medication and home visits offered to those who cannot travel, such as stroke and elderly.
As the provider network under the Ministry of Public Health (MOPH) jurisdiction did not gain a corporate status, the MOPH, having the corporate status by law, signed an annual contract with the NHSO, but capitation payment and disbursement of admission services based on Diagnostic Related Group (DRG) were directly paid to the providers, not via MOPH. This ensures mutual financial accountability between provider networks and NHSO.
Access to the IP services does not require registration. Clinically indicated cases were admitted by a district hospital or referred to provincial hospital when beyond its clinical capacities. Upon discharge, summaries of clinical data were electronically submitted to NHSO where a specific DRG group was assigned with an attached relative weight. The total annual IP global budget when divided by the total relative weights of the whole country admissions resulted in reimbursement rate per weight. This is the amount disbursed to respective hospitals. The relative weight was regularly calibrated every 4–5 years. Upon series of stakeholder consultations, new relative weight was agreed and adopted. The annual global IP budget was estimated based on expected admission utilization rate and unit cost per admission at different level of hospitals.
Managing geographical monopoly and quality issues
It is not uncommon to find a DHS the sole provider in a district; a geographical monopoly of health services in the locality. It was not possible not to contract such a DHS even though it was not accredited by the Healthcare Accreditation Institute (HAI) as people had no choice; travelling to neighbouring DHS was expensive and inconvenient. In such case, a strict application of quality condition such as accreditation or re-accreditation status for entering to contractual agreement was not viable.
A financial incentive was offered by NHSO in 2007 by recognizing a stepwise quality improvement initiated by HAI in 2003. Step 1 means risk identification system was installed; step 2 means quality assurance and quality improvement were in place and step 3 means a full accreditation or re-accreditation status every 2 and 3 years for the first and second re-accreditation, respectively (HAI 2013). Accreditation status certifies a sustained system of risk management and quality improvement. It should be noted that HAI focuses on strengthening hospitals as learning organizations where the national hospital standards is established and hospitals are empowered, step by step, to identify risk and build in risk management and quality improvement in all dimensions such as administration, ancillary and clinical service managements in line with the national standards. Since the inception, the HAI deliberately decided not to accredit hospital outcome per se but concentrated on quality improvement processes. Hence, accreditation is certifying a well established and sustained quality improvement system. However, HAI will assess the trend of clinical outcome in the forthcoming years. The NHSO earmarked a budget of 0.76 Baht per capita (35.7 million Baht per annum in total) to boost the quality improvement, with an application of the maximum score of 5 for the accredited hospitals (step 3), score 2 for step 2 and score 1 for step 1 status. It is noted that the scores 1, 2 and 5 were developed by NHSO for its incentive scheme and are not an outcome of the HAI accreditation process. Accredited primary health care facilities received a grant of 30 Baht per capita multiplied by catchment population it served. Figure 3 showed rapid improvement from steps 1 to 2 after quality incentives were offered in 2007. Note that an increase in the proportion of hospitals in step 0 from 1% in 2011 to 14% in 2012 was the effect of hospitals with accreditation status expired after 3 years and had not yet re-accredited.
Figure 3.
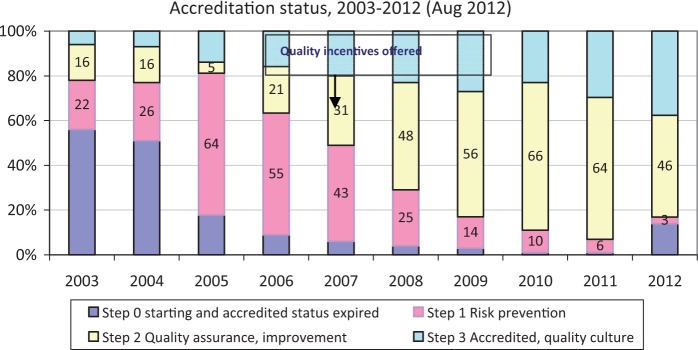
Hospital accreditation status 2003–2012 and quality incentives offered by NHSO in 2007
Managing provider payment and annual budget
Unlike SHI which paid for both OP and IP services to public and private contracting hospitals on a per capita basis, UCS decided to apply two distinct payment methods; OP was paid by capitation and later on age- and gender-adjusted and IP was paid by a national global budget (later global budget at regional level) and within this budget envelope, using DRG relative weights for total national discharges to calculate reimbursement rate per weight to respective hospitals.
The capitation fee for OP was estimated by multiplying utilization rate (visits per capita per year projected from historical data to that fiscal year) with the unit cost of providing OP services by different levels of care. Capitation fee for prevention and health promotion was estimated based on cost and quantity of age and gender-specific services to be provided such as ante natal care (ANC), family planning and cervical screening.
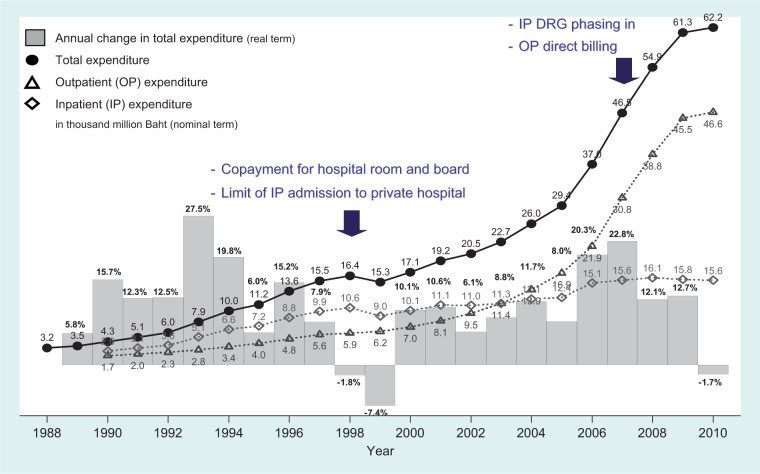
CSMBS applied fee for service for OP, but Comptroller General Department had limited capacity to regulate price and quantity of service provided. It directly disbursed healthcare providers (not patients), while no copayment was enforced. The excessive use of medicines outside the National List of Essential Medicines and diagnostics resulted in rapid cost escalation. In 2007, CSMBS replaced fee for services by DRG but no global budget for IP payment. DRG-based payment despite no global budget can contain costs well in 2008–2010, see Figure 4.
Figure 4.
CSMBS expenditure in total and on OP and IPs and annual growth, 1988–2010
The UCS capitation payment sent a strong cost-containment signal, as financial risk was transferred from NHSO to providers. Capitation resulted in the use of generic essential medicines where cost was lower than branded and non-essential items. Providers need to keep a positive balance out of their capitation revenue; there was less incentives to prescribe more than necessary. Global budget and DRG for IP also contained cost effectively, preventing financial implications from possible DRG creep.
NHSO negotiated with Bureau of Budget, based on per capita budget multiplied by total number of the UCS beneficiaries. Different components of the per capita budget were estimated, based on utilization rate and unit cost of service. Administrative cost of NHSO was based on personnel, operating and capital cost. Budgets for OP and for prevention and health promotion were fully allocated to the contracting provider networks based on the number of registered population. The provider networks were allowed to keep the positive balance and shouldered the negative balance if any. Other high-cost services, such as RRT and Antiretroviral treatment, were managed separately.
Preventing the downside of close end payment
One major risk associated with closed end payment was under-service provision (Preker et al. 2013). Effective counter measures introduced by NHSO included complaint management through 24-h call centre. The UCS members dialled 1330 to seek advice or make complaint where simple conflict resolution was settled between patients and providers by call centre staff. In 2012, there were 617 694 calls of which 4370 (1%) were complaints, the remaining majority (93%) were counselling and advice to beneficiaries, 6% were queries by healthcare providers. Of the total 4370 complaints, 17% were poor quality and standard, 23% were poor service attention, 27% were being charged and 33% were not receiving services covered in the benefit package. In 2011, the complaint rate was low, 2.9 per 100 000 patients (4386 out of the total 153 million combined OP visits and admissions). Of these total complaints, 97% were investigated and settled within 30 days as required by Law. Of the total settled cases, 54% found provider guilty where appropriate actions were taken, whereas 46% were misunderstood by beneficiaries.
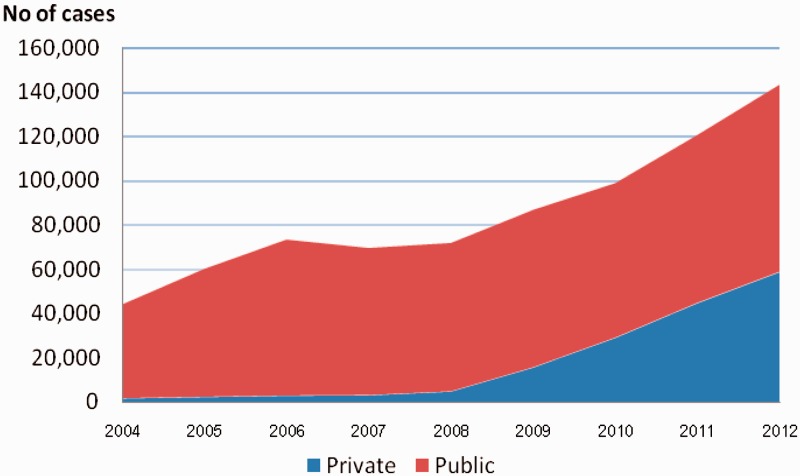
Some interventions were not adequately accessed, e.g. cataract lens replacement due to supply side constraints. Backlogs of cataract blindness in the long waiting list was removed by taking the surgical procedure out of the IP DRG system and paying by a fixed fee schedule per case to hospitals and offering surgical fees to surgeons. Central bargaining by NHSO had brought down prices of soft lens significantly; hospitals can choose to reimburse on an agreed rate or to use lens supplied by the NHSO-negotiated vendors. Private hospitals with spare capacity were contracted with the same conditions applied to public hospitals. After the 2008 launch, numbers of cataract operation doubled in 4 years, from 71 823 lens replaced in 2008 to 143 553 in 2012, see Figure 5.
Figure 5.
Number of cataract surgery before and after unbundling from DRG and replace by special payment. Source: NHSO (2012).
Executing monopsonistic purchasing power
NHSO exercised the monopsonistic power, as a single purchaser, to negotiate with suppliers of medicines and supplies over price given an assured quality. A committee consisting of NHSO officers and technical experts processed the open bidding and direct negotiation with oligopoly and monopoly suppliers. The priority items were those with high costs and/or high volumes. Table 4 summarizes total saving from exercising monopsonistic power, up to US$ 188 million in recent few years.
Table 4.
Cost saving from central negotiation for medical supplies and medicines, various years, US $
| Market unit price | Negotiated price | Units purchased | Cost difference | Cost savings | |
|---|---|---|---|---|---|
| Medical supplies | |||||
| Folding lens (2011–2012) | 133 | 93 | 64 100 | 40 | 2 564 000 |
| Unfolding lens (2011–2012) | 133 | 23 | 7197 | 110 | 791 670 |
| Balloon stent (2009–2012) | 667 | 333 | 26 655 | 334 | 8 902 770 |
| Coronary stent (2009–2012) | 1000 | 167 | 10 575 | 833 | 8 808 975 |
| Drug-coated stent (2009–2012) | 2833 | 567 | 33 794 | 2266 | 76 577 204 |
| DES alloy stent (2012) | 1833 | 833 | 343 | 1000 | 343 000 |
| Medicines | |||||
| ARV (2010–2012) | 747 | 658 | 29 973 | 89 | 2 667 597 |
| High cost drug (2010–2012) | 4508 | 3197 | 4674 | 1311 | 6 127 614 |
| Influenza vaccine (2010–2012) | 7 | 5 | 643 319 | 2 | 1 286 638 |
| Erythropoietin (2009–2012) | 22 | 8 | 1 634 239 | 14 | 22 879 346 |
| CAPD solution (2010–2012) | 7 | 4 | 19 095 657 | 3 | 57 286 971 |
| Total cost saving to UCS | 188 235 785 | ||||
DES: Drug eluting stent, CAPD: Continuous ambulatory peritoneal dialysis.
Source: NHSO 2012.
Discussion
Not only the purchasing functions contribute to achievement of UHC goals, but also enabling factors worth mentioning. First, the extensive geographical coverage of health delivery systems, DHS plays a strategic hub for provisions of primary and secondary health services and translates policy intentions into equity outcomes (Prakongsai et al. 2009). Second, the effective referral backup to tertiary care and excellent centres in the Region, ensured access to specialist care. It is noted that referral is required for OP as the DHS contractor network receiving capitation budget is the funding holder and is responsible to pay for the referred OPs. IPs paid by DRG in a global budget ceiling does not required referral. Referral statistics were kept at local level for financial management purposes and was not transmitted to NHSO. Third, an extensive road and availability of public transport nationwide facilitated physical access. Others are, for example, level of female literacy and trust in MOPH health services where health professional were qualified and observed work etiquette.
Unavoidably, developing country will face geographical monopoly, which hampers competitive contract model. Other mechanisms such as hospital accreditation, quality improvement and quality incentives are comprehensive intervention to gradually overcome unsatisfactory quality of care.
Provider payment is the most critical factor contributing tofinancial risk protection and technical efficiency. A few low- and middle-income countries where closed-end paymentwas not widely applied, fee for services result in cost escalation such as in China (Hu et al. 2008; Yip et al. 2010) andhigh level of out-of-pocket payment from balance billingby members of PhilHealth in the Philippines. Most countries in the region are moving towards capitation and DRG, such as Vietnam, Philippines and China.
NHSO has a very small administrative budget: first it has no mandate to collect premium from members, as UCS is financed by general taxation. Second, it did not have a large staff body to review itemized fee for service claims, as DRG and Global Budget was applied for IP and capitation for OP payments. NHSO administrative cost was 1.06% of total annual UCS budget over the last 11 years between 2002 and 2012.
Conclusion and policy lessons
Strategic purchasing supports achievement of UHC goals. Contracting OP services to DHS results in equitable access to care, where referral backup is essential. Geographical monopoly limits competitive contracting, for which issues on quality of care are addressed by hospital accreditation and other quality incentive mechanisms. DHS as gate keeping contributes to rational use of services and systems efficiency.
Comprehensive benefit package offered free at point of service contributes to financial risk protection. Comprehensive package is financially feasible as the self-cost-contained closed end payment was applied. In contrast, CSMBS fee for service OP services results in excessive use of health resources and cost escalations. Potential drawbacks of closed end payment especially under-provision and poor quality are addressed by complaint handling via 24-h call centre, unbundling services from capitation such as chemotherapy, radiation therapy and antiretroviral therapy (ART), and from DRG such as cataract and pay on an agreed few schedules. DRG creep is countered by medical audits and NHSO reclaims of the over-disbursed amounts, see Box 1. Global budget prevents financial impacts from DRG creep. NHSO institutional capacities, especially executing monopsonistic purchasing was gradually initiated, whereas external partners contribute to HTA evidence guiding policy decision on inclusion of new medicines and interventions into benefit package.
Box 1.
Medical Audit in action, 8 years NHSO experiences. It was not until 2006 that NHSO settled medical audit of IP claims when the number of trained independent physicians and coding auditors became adequate. Initially, random audit of 1% of medical records in all hospitals was applied between 2006 and 2008; later selective audits of potential errors using screening criteria were applied since 2009. Three errors were identified using auditors as gold standard; (1) between attending physician and medical auditor discharge summary, called ‘summary error’; (2) between hospital and auditor coders using hospital discharge summary, called ‘coding error’ and (3) relative weight computed from hospital claim and auditor, called ‘changes in relative weight’, which can be over- or under-claimed by hospitals, for which reclaiming from and additional pay to hospitals by NHSO. Appeal provision was made available if hospitals do not agree with verification by auditors. Medical audit facilitates NHSO mutual accountability; in 2012, NHSO audited 1.2% of total IP claims and reclaimed the over-reimbursement by hospitals the total amount of US$ 6.07 million.
KEY MESSAGES.
Strategic purchasing function, if managed well by insurance agencies, contributes to achieving universal health coverage (UHC) goals of equitable access and financial risk protection. Availabilities of functioning primary healthcare services and proper referral backup to secondary and tertiary care are vital.
Fee for service, when payment related to number of items of services provided, stimulated excessive provision of services, inefficient use of resources and cost escalation. In contrast, closed-end payment such as capitation and diagnostic related group send strong signal to providers to use generic medicines, appropriate use of technologies and self-cost containment resulting in efficiency. National Drug Regulatory Authority is responsible to ensure quality of generic medicines in the market.
To prevent under-provisions of services, some high cost interventions can be singled out from closed end payment, and pay on an agreed fee schedule. Institutional capacity needs to be strengthened and sustained in managing strategic purchasing.
There are great opportunities for insurance agencies to execute monopsonistic purchasing power, namely a single buyer from multiple sellers of healthcare services to gain the best possible price given assured quality of goods and services.
Acknowledgements
We appreciate contributions by senior management and staffs in the NHSO.
Funding
This study was financially supported by WHO-South East Asia Regional Office. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of interest statement: None declared.
References
- Evans TG, Chowdhury MR, Evans DB, et al. Thailand’s Universal Coverage Scheme: Achievements and Challenges. An Independent Assessment of the First 10 Years (2001–2010) Nonthaburi: Health Insurance System Research Office; 2012. [Google Scholar]
- HAI . Healthcare Accreditation Institute, Thailand. http://www.ha.or.th/haweb/index.php/home-2, accessed 3 September 2013. [Google Scholar]
- HITAP. Health Intervention and Technology Assessment Program Profiles. . http://www.hitap.net/en/about/background, accessed 3 September 2013. [Google Scholar]
- Hu S, Tang S, Liu Y, et al. Reform of how health care is paid for in China: challenges and opportunities. Lancet. 2008;372:1846–53. doi: 10.1016/S0140-6736(08)61368-9. [DOI] [PubMed] [Google Scholar]
- Jongudomsuk P, Limwattananon S, Prakongsai P, et al. Evidence-based health financing reform in Thailand (chapter 16) In: Clements B, Coady D, Gupta S, editors. The Economics of Public Health Care Reform in Advanced and Emerging Economies. Washington: International Monetary Fund; 2012. pp. 307–26. [Google Scholar]
- Kasemsup V, Prakongsai P, Tangcharoensathien V. Budget impact analysis of a policy on universal access to RRT under universal coverage in Thailand. Journal of the Nephrology Society of Thailand. 2006;12(suppl 2):136–48. [Google Scholar]
- Limwattananon S, Neelsen S, O'Donnell O, et al. 2013 Universal coverage on a budget: impacts on health care utilization and out-of-pocket expenditures in Thailand. Tinbergen Institute Discussion Paper, TI 2013-067/V. Tinbergen Institute. [Google Scholar]
- Limwattananon S, Tangcharoensathien V, Prakongsai P. Catastrophic and poverty impacts of health payments: results from national household surveys in Thailand. Bulletin of the World Health Organization. 2007;85:600–6. doi: 10.2471/BLT.06.033720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Limwattananon S, Tangcharoensathien V, Tisayathicom K, Boonyapaisarncharoen T, Prakongsai P. Why has the universal coverage scheme in Thailand achieved a pro-poor public subsidy for health care? BMC Public Health. 2012;12(suppl 1):S6. doi: 10.1186/1471-2458-12-S1-S6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Donnell O, van Doorslaer E, Rannan-Eliya RP, et al. The incidence of public spending on healthcare: comparative evidence from Asia. The World Bank Economic Review. 2007;21:93–123. [Google Scholar]
- Preker A, Lindner M, Chernichovsky D, Schellekens O, editors. Scaling Up Affordable Health Insurance: Staying the Course. Washington: the World Bank; 2013. [Google Scholar]
- Prakongsai P. 2008 The impact of the universal coverage policy on equity of the Thai Health Care System. Ph.D. Thesis. London School of Hygiene and Tropical Medicine, University of London. [Google Scholar]
- Prakongsai P, Limwattananon S, Tangcharoensathien V. The equity impact of the universal coverage policy: lessons from Thailand. Advances in Health Economics and Health Services Research. 2009;21:57–81. [PubMed] [Google Scholar]
- Prakongsai P, Palmer N, Uay-Trakul P, Tangcharoensathien V, Mills A. What Happened to Poorer Thai Households When Renal Replacement Therapy Was Excluded from the National Benefit Package? Nonthaburi: International Health Policy Program; 2007. [Google Scholar]
- Prakongsai P, Tangcharoensathien V, Kasemsup V, et al. Policy recommendation on universal access to renal replacement therapy under universal coverage in Thailand. Journal of the Nephrology Society of Thailand. 2006;12(suppl 2):37–49. [Google Scholar]
- Tangcharoensathien V, Kamolratanakul P. Making sensible rationing: the use of economic evidence and the need for methodological standards. Journal of the Medical Association of Thailand. 2008;91:S4–7. [PubMed] [Google Scholar]
- Tangcharoensathien V, Kasemsup V, Teerawattananon Y, et al. Universal Access to Renal Replacement Therapy in Thailand: A Policy Analysis. Nonthaburi: International Health Policy Program & Nephrology Society of Thailand; 2005. [Google Scholar]
- Tangcharoensathien V, Pitayarangsarit S, Patcharanarumol W, et al. Promoting universal financial protection: how the Thai universal coverage scheme was designed to ensure equity. Health Research Policy and Systems. 2013;11:25. doi: 10.1186/1478-4505-11-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tangcharoensathien V, Prakongsai P, Limwattananon S, Patcharanarumol W, Jongudomsuk P. From targeting to universality: lessons from the health system in Thailand. In: Townsend P, editor. Building Decent Societies: Rethinking the Role of Social Security in Development. Hampshire: Palgrave Macmillan; 2009. pp. 310–22. [Google Scholar]
- Tangcharoensathien V, Vasavid C, Kasemsup V. An opinion poll on universal access to RRT under UC in Thailand. Journal of the Nephrology Society of Thailand. 2006;12(suppl 2):21–36. [Google Scholar]
- Tantivess S, Teerawattananon Y, Mills A. Strengthening cost-effectiveness analysis in Thailand through the establishment of the health intervention and technology assessment program. Pharmacoeconomics. 2009;27:931–45. doi: 10.2165/11314710-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Tantivess S, Werayingyong P, Chuengsaman P, Teerawattananon Y. Universal coverage of renal dialysis in Thailand: promise, progress, and prospects. BMJ. 2013;346:f462. doi: 10.1136/bmj.f462. [DOI] [PubMed] [Google Scholar]
- Teerawattananon Y, Mugford M, Tangcharoensathien V. Economic evaluation of palliative management versus peritoneal dialysis and hemodialysis for end-stage renal disease: evidence for coverage decisions in Thailand. Value Health. 2007;10:61–72. doi: 10.1111/j.1524-4733.2006.00145.x. [DOI] [PubMed] [Google Scholar]
- Yip W, Hsiao W, Meng Q, Chen W, Sun X. Realignment ofincentives for health-care providers in China. Lancet. 2010;375:1120–30. doi: 10.1016/S0140-6736(10)60063-3. [DOI] [PubMed] [Google Scholar]
- Yothasamut J, Putchong C, Sirisamutr T, Teerawattananon Y, Tantivess S. Scaling up cervical cancer screening in the midst of human papillomavirus vaccination advocacy in Thailand. BMC Health Services Research. 2010;10(suppl 1):S5. doi: 10.1186/1472-6963-10-S1-S5. [DOI] [PMC free article] [PubMed] [Google Scholar]