Abstract
Despite very wide variations of malondialdehyde (MDA) concentrations in biological samples, it is still used as a biomarker of oxidative stress in clinical investigations. In the current perspective study, we aimed to summarize a number of critical analytical points for determination of MDA. Technical problems and controversial findings in healthy people and some psychiatric disorders reveal that the reliability of MDA as a biomarker of oxidative stress n eeds to be re-evaluated by experts.
Keywords: Thiobarbitoric acid reactive substances, Oxidative stress, Biomarker
Malondialdehyde (MDA) is the most frequently used biomarker of oxidative stress in many health problems such as cancer, psychiatry, chronic obstructive pulmonary disease, asthma, or cardiovascular diseases. This perspective study aimed to collect some evidence for low reliability of the MDA as a biomarker of oxidative stress. Our main hypothesis is that MDA assay is not able to provide valid analytical data for biological samples due to its high reactivity and possibility of various cross-reactions with co-existing biochemicals. Thiobarbitoric acid (TBA) assay is the most commonly used method for determination of the MDA in biological fluids.1 The assay is based on a condensation reaction of two molecules of TBA with one molecule of MDA, in which the reaction rate depends on temperature, pH and concentration of TBA. The reaction is carried out in acidic solution and temperature of ~ 100°C within one hour time course and most of MDA is produced during reaction process from decomposition of products of lipid peroxidation.2 The rapidity, ease of use and cost of TBA assay made it the most common method in spite of some consideration and limitations of the method. These mainly are:
Non-specificity of TBA reactivity on MDA3,4 and production of MDA from reactions other than lipid peroxidation.5 Concerning these characteristics of TBA assay and cross-reaction of other aldehydes produced from lipid peroxidation, most of researchers used total values of TBA reactive substances (TBARs) as a biomarker of oxidative stress instead of MDA values,
Effects of procedural modifications on MDA-TBA adduct development,3
Low stability of MDA in biological samples due to its high tendency for reacting with proteins, amino acids etc.6 and rapid enzymatic degradation,7
Low recovery test results.10
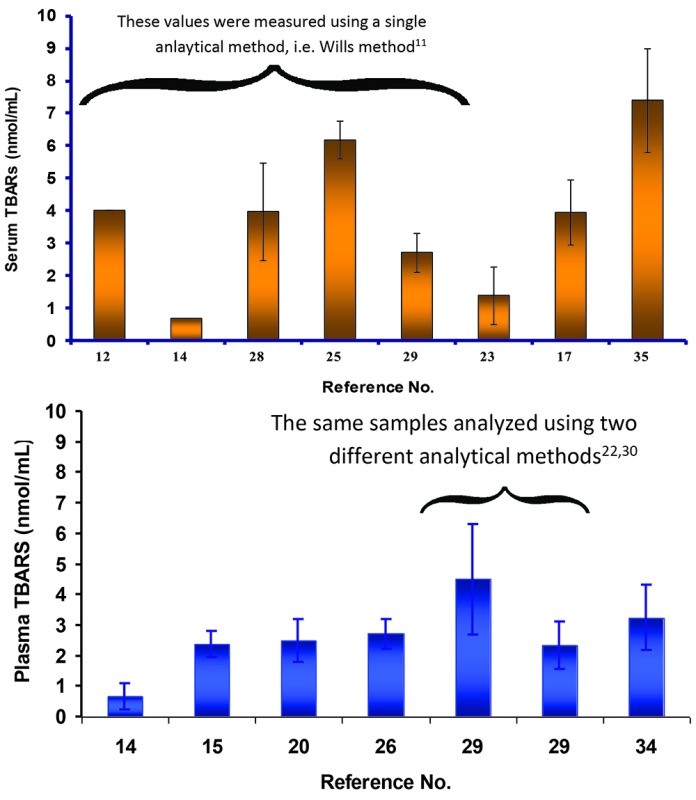
Variations of TBARs in biological samples of a number of psychiatric patients were investigated and compared with the values of healthy controls (for details see Table 1).9,11-36 In a more recent article, de Sousa et al19 compared plasma TBARs and some other markers in healthy individuals and patients with bipolar disorder (BD) before and after lithium therapy. Plasma samples were collected during two years, stored at -80ºC and TBARs were measured using a spectrophotometric analysis. The reported TBARs for healthy controls was 62.74 ± 37.58 nmol/mL, those of BD patients before and after lithium therapy were 60.77 ± 45.14 and 37.88 ± 35.85 nmol/mL, respectively, and a significant decrease was observed from baseline to endpoint TBARs (p=0.023) in patients with lithium therapy.19 Decreased TBAR levels after lithium therapy (3.6 ± 0.3 vs. 5.1 ± 1.1 nmol/mL) has been confirmed by Machedo-Vieira et al,28 whereas no significant difference (6.33 ± 1.16 vs. 6.63 ± 1.15 nmol/mL) was observed in another investigation.17 Further, no change in TBAR levels in healthy people receiving lithium was observed by the same group of de Sousa.25 There are also other controversies on TBARs of healthy people (e.g., for plasma ranging from 0.6714 to 62.7410 nmol/mL) among various reports (Figs. 1 and 2). In both Figs. 1 and 2, one datum with very high deviation was excluded, however, significant variations were observed for healthy people, which is obviously questionable finding. One might consider analytical methods as a source of these discrepancies. When we considered a given analytical technique, namely, Wills method,11 discrepancies were still present varying from 0.67 ± 0.01 nmol/mL24 to 6.18 ± 0.58 nmol/mL.25 We would like to point out some considerations on TBARs measurements and to discuss their validity from a bioanalytical point of view. A number of reasons could be considered as possible causes of these observations including variations in sample preparation, storage, pre-treatment, and analysis which are briefly reviewed in this perspective. Full details could be found in a recent review article.37
Table 1 . A summary of TBARs variations in some psychiatric disorders .
| Matrix | Conditions | TBARs (nmol/mL) | Reference of analytical method | Reference of TBARs data |
| Serum | Euthymic | ~ 6.2 | 11 | 12 |
| Serum | Depressed | ~ 5.0 | 11 | 12 |
| Serum | Manic | ~ 7.8 | 11 | 12 |
| Plasma | Schizophrenia | 1.15± 0.35 | 13 | 14 |
| Plasma | Schizophrenia - medicated | 0.93 ± 0.65 | 13 | 14 |
| Plasma*** | Social phobia* | 2.32 ± 0.38 | 9 | 15 |
| Plasma*** | Social phobia** | 4.52 ± 0.42 | 9 | 15 |
| Serum | Bipolar disorder before lithium therapy | 6.63 ± 1.51 | 16 | 17 |
| Serum | Bipolar disorder after lithium therapy | 6.33 ± 1.16 | 16 | 17 |
| Plasma | Bipolar disorder before lithium therapy | 60.77 ± 45.14 | 18 | 19 |
| Plasma | Bipolar disorder after lithium therapy | 37.88 ± 35.85 | 18 | 19 |
| Plasma | Schizophrenia* | 3.8 ± 0.8 | 11 | 20 |
| Plasma | Schizophrenia* after haloperidol therapy | 3.4 ± 0.7 | 11 | 20 |
| Plasma | Schizophrenia* after clozapine therapy | 4.4 ± 0.7 | 11 | 20 |
| Serum | Schizophrenia - paranoid | 5.1 ± 1.7 | 11 | 21 |
| Serum | Schizophrenia - disorganized | 5.0 ± 1.3 | 11 | 21 |
| Serum | Schizophrenia - undifferentiated | 5.4 ± 1.4 | 11 | 21 |
| Serum | Schizophrenia – partial remission | 4.9 ± 1.6 | 11 | 21 |
| Serum | Schizophrenia – marked symptoms | 5.9 ± 2.0 | 11 | 21 |
| Serum | Schizophrenia - deteriorated | 4.7 ± 1.3 | 11 | 21 |
| Serum | Schizophrenia | 1.34 ± 0.97 | 22 | 23 |
| Serum | Euthymic | 0.62 ± 0.02 | 11 | 24 |
| Serum | Depression | 0.89 ± 0.02 | 11 | 24 |
| Serum | Manic | 1.73 ± 0.16 | 11 | 24 |
| Plasma | Schizophrenia | 4.76 ± 0.79 | 9 | 26 |
| Plasma | Bipolar disorder | 4.26 ± 0.46 | 9 | 26 |
| Serum | Schizophrenia | 4.95 ± 1.56 | 11 | 27 |
| Serum | Bipolar disorder - euthymic | 6.36 ± 1.46 | 11 | 27 |
| Serum | Bipolar disorder - manic | 7.54 1.74 | 11 | 27 |
| Serum | Bipolar disorder - depressed | 5.28 ± 1.54 | 11 | 27 |
| Serum | Mania before lithium therapy | 5.1 ± 1.1 | 11 | 28 |
| Serum | Mania after lithium therapy | 3.6 ± 0.3 | 11 | 28 |
| Plasma | Schizophrenia - chronic | 8.01 ± 5.5 | 22 | 29 |
| Plasma | Schizophrenia - chronic | 5.16 ± 1.85 | 30 | 29 |
| Plasma | Adult attention-deficit hyperactivity disorder | 2.44 ± 0.84 | 31 | 32 |
| Serum | Schizophrenia** after haloperidol therapy | ~ 78 | 33 | |
| Serum | Schizophrenia** after quetiapine therapy | ~ 75 | 33 | |
| Serum | Schizophrenia** after olanzepine therapy | ~ 73 | 33 | |
| Serum | Schizophrenia** after risperidone therapy | ~ 80 | 33 | |
| Plasma*** | Schizophrenia | 4.06 ± 1.79 | 22 | 34 |
| Serum | Mania | 9.8 ± 5.0 | 18 | 35 |
| Serum | Schizophrenia – acute phase | 3.5 ± 1.2 | 18 | 36 |
| Serum | Schizophrenia – after antipsychotic treatment | 3.6 ± 1.5 | 18 | 36 |
* Non-smoker.
** Smoker.
*** EDTA treated.
Fig. 1 .
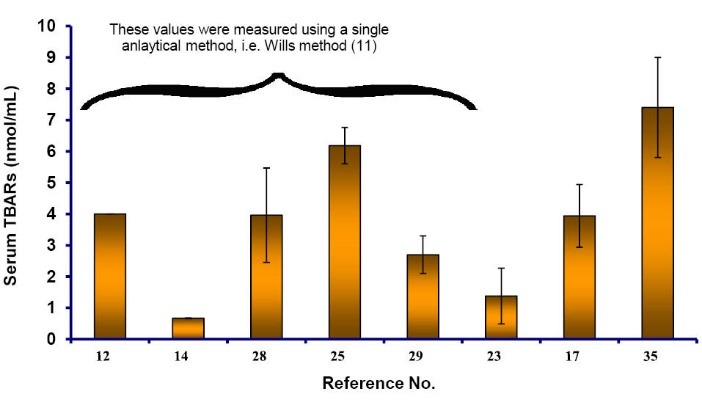
Serum TBARs (±SD) of healthy controls reported by various research groups (one datum [~ 60 nmol/mL33] was excluded from figure).
Fig. 2 .
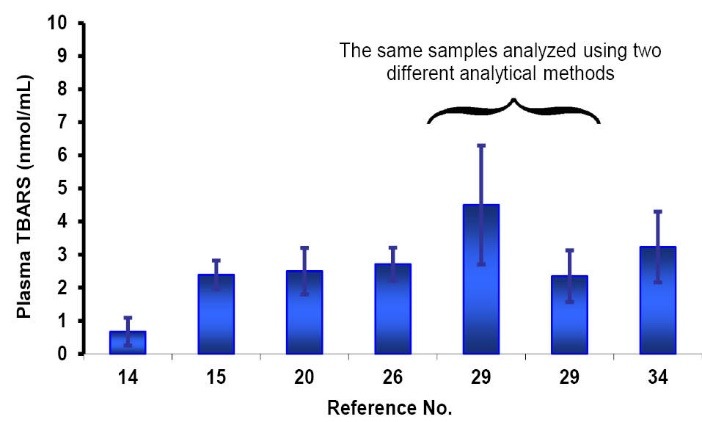
Plasma TBARs (±SD) of healthy controls reported by various research groups (one datum [~ 62.7 nmol/mL19] was excluded from figure).
There are some concerns in serum preparation, since TBARs are increased during coagulation process.38 In plasma preparation, one should consider the effects of EDTA on TBAR values. A significant increase in TBARs for plasma samples (1.39 ± 0.26 nmol/mL) treated with EDTA was reported when compared with the corresponding serum (1.07 ± 0.27 nmol/mL) and heparinized plasma (1.11 ± 0.18 nmol/mL) samples.31
Storage of serum/plasma samples at -20ºC without addition of antioxidants increased TBAR levels by a factor of two after 3-7 days and the addition of EDTA + glutathione increased the stability of TBARs up to 35 days.31
Most of TBARs are produced during the heating of acidic solutions.2,39 Some authors claimed preventive effects of addition of butylated hydroxyl toluene40 and some others denied such effect.41 It has been shown that different acids and their concentrations could affect the results of TBAR assay.41
Measurement of TBARs using spectroscopic methods is simple, low cost, convenient, and widely used in clinical studies. Modifications were made on analytical conditions, therefore various values could be produced which make the comparison of reported values very difficult and even impossible. As mentioned above, poor selectivity of spectroscopic method is another disadvantage and the methods based on separation of analytes may overcome this limitation. However, some of these methods resulted in poor recovery, reproducibility, and repeatability values.42 As clearly noted by Wade and van Rij,43 most of problems associated with TBA assay were ignored by many researchers. Despite of these points, MDA is still used as an oxidative stress biomarker.44,45
Concerning above mentioned points on TBAR levels in healthy individuals and patients, controversial findings on TBARs in psychological disorders, official definitions of a biomarker,46 poor reproducibility, low repeatability, non-specificity, low stability of the standard solutions of TBA assay, and lack of full validation data of TBARs measurements in biological fluids, the reliability of TBARs as a biomarker of oxidative stress in the psychological disorders is questionable. As a conclusion, a number of bioanalytical points are summarized and the discussions on other viewpoints are open. We believe that MDA as an oxidative stress biomarker needs to be re-evaluated by an expert panel.
Acknowledgements
This communication is a part of PhD by research project of M. Khoubnasabjafari. Authors would like to thank the reviewers’ comments on this submission and Tabriz University of Medical Sciences for partial financial support.
Ethical issues
There is none to be declared.
Competing interests
We have no conflicting interests with regard to the present submission.
Perspective Highlights
What is current knowledge?
√ MDA is used as a biomarker of oxidative stress in various diseases despite its wide variations even in healthy people.
What is new here?
√ According to the collected evidence, most of the technical problems on MDA measurement are unresolved and need further investigation, and the biomarker role of MDA should be re-evaluated by experts.
References
- 1.Janero DR, Burghardt B. Analysis of cardiac membrane phospholipids peroxidation kinetics as malondialdehyde: unspecificity of thiobarbituric acid-reactivity. Lipids. 1988;23:452–58. doi: 10.1007/BF02535519. [DOI] [PubMed] [Google Scholar]
- 2.Gutteridge JM, Toeg D. Iron-dependent free radical damage to DNA and deoxyribose Separation of TBA-reactive intermediates. Int J Biochem. 1982;14:891–3. doi: 10.1016/0020-711X(82)90071-4. [DOI] [PubMed] [Google Scholar]
- 3.Halliwell B, Gutteridge JM. Formation of a thiobarbituric-acid-reactive substance from deoxyribose in the presence of iron salts the role of superoxide and hydroxyl radicals. FEBS Lett. 1981;128:343–6. doi: 10.1016/0014-5793(81)80114-7. [DOI] [PubMed] [Google Scholar]
- 4.Kikugawa K, Kojima T, Yamaki S, Kosugi H. Interpretation of the thiobarbitoric acid reactivity of rat liver and brain homogenates in the presence of ferric ion and ethylenediaminetetraacetic acid. Anal Biochem. 1992;202:249–55. doi: 10.1016/0003-2697(92)90102-D. [DOI] [PubMed] [Google Scholar]
- 5.Liu J, Yeo HC, Doniger SJ, Ames BN. Assay of aldehydes from lipid peroxidation: Gas chromatography-mass spectrometry compared to thiobarbituric acid. Anal Biochem. 1997;245:161–5. doi: 10.1006/abio.1996.9990. [DOI] [PubMed] [Google Scholar]
- 6.Shin BC, Huggins JH, Carrawa KL. Effects of pH, concentration and aging on the malondialdehyde reaction with proteins. Lipids. 1972;7:229–33. doi: 10.1007/BF02533218. [DOI] [PubMed] [Google Scholar]
- 7.Siu GM, Draper H H. Metabolism of malondialdehyde in vivo and in vitro. Lipids. 1982;17:349–55. doi: 10.1007/BF02535193. [DOI] [PubMed] [Google Scholar]
- 8.Schoenmakers AW, Tarladgis BG. Reliability of the thiobarbitoric acid test in the presence of inorganic ions. Nature. 1966:1153. doi: 10.1038/2101153a0. [DOI] [Google Scholar]
- 9.Satoh K. Serum lipid peroxide in cerebrovascular disorders determined by a new colorimetric method. Clin Chim Acta. 1978;90:37–43. doi: 10.1016/0009-8981(78)90081-5. [DOI] [PubMed] [Google Scholar]
- 10.Mendes R, Cardoso C, Pestana C. Measurement of malondialdehyde in fish: A comparison study between HPLC methods and the traditional spectrophotometric test. Food Chem. 2009;112:1038–45. doi: 10.1016/j.foodchem.2008.06.052. [DOI] [Google Scholar]
- 11.Wills ED. Mechanisms of lipid peroxide formation in animal tissues. Biochem J. 1966;99:667–79. doi: 10.1042/bj0990667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Andreazza AC, Cassini C, Rosa AR, Leite MC, de Almeida LMV. et al. Seum S100B and antioxidant enzymes in bipolar patients. J Psychiat Res. 2007;41:523–9. doi: 10.1016/j.jpsychires.2006.07.013. [DOI] [PubMed] [Google Scholar]
- 13.Konings WT, Drijver EB. Radiation effects on membranes I: Vitamin E deficiency and lipid peroxidation. Rad Res. 1979;80:494–501. doi: 10.2307/3574991. [DOI] [PubMed] [Google Scholar]
- 14.Arvindakshan M, Sitasawad S, Debsikdar V, Ghate M, Evans D, Horrobin DF. et al. Essential polyunsaturated fatty acid and lipid peroxide levels in never-medicated and medicated schizophrenia patients. Biol Psychiat. 2003;53:56–64. doi: 10.1016/S0920-9964(02)00284-0. [DOI] [PubMed] [Google Scholar]
- 15.Atmaca M, Kuloglu M, Tezcan E, Ustundag B. Antioxidant enzyme and malondialdehyde levels in patients with social phobia. Psychiat Res. 2008;199:95–100. doi: 10.1016/j.psychres.2002.12.004. [DOI] [PubMed] [Google Scholar]
- 16.Dahle LK, Hill EG, Holman RT. The thiobarbituric acid reaction and the autoxidations of polyunsaturated fatty acid methyl esters. Arch Biochem Biophys. 1962;98:253–61. doi: 10.1016/0003-9861(62)90181-9. [DOI] [PubMed] [Google Scholar]
- 17.Banerjee U, Dasgupta A, Rout JK, Singh OP. Effects of lithium therapy on Na+-K+-ATPase activity and lipid peroxidation. Prog Neuro-Psychopharmacol Biol Psychiat. 2012;37:56–61. doi: 10.1016/j.pnpbp.2011.12.006. [DOI] [PubMed] [Google Scholar]
- 18. Cayman commercial kit, Cayman Chemical Company, Ann Arbor, MI, USA.
- 19.de Sousa RT, Zarate CA Jr, Zanetti MV, Costa AC, Talib LL. et al. Oxidative stress in early stage bipolar disorder and the association with response to lithium. J Psychiat Res. 2014;50:36–41. doi: 10.1016/j.jpsychires.2013.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gama CS, Salvador M, Andreazza AC, Kapczinski F, Silva Belmonte-de-Abreu P. Elevated serum superoxide dismutase and thiobarbituric acid reactive substances in schizophrenia: A study of patients treated with haloperidol or clozapine. Prog Neuro-Psychopharmacol Biol Psychiat. 2006;30:512–5. doi: 10.1016/j.pnpbp.2005.11.009. [DOI] [PubMed] [Google Scholar]
- 21.Gama CS, Salvador M, Andreazza AC, Lobato MI, Berk M, Kapczinski F. et al. Elevated serum thiobarbituric acid reactive substances in clinically symptomatic schizophrenic males. Neurosci Lett. 2008;433:270–3. doi: 10.1016/j.neulet.2008.01.018. [DOI] [PubMed] [Google Scholar]
- 22.Ohkawa H, Ohishi N, Yagi K. Assay for lipid peroxides in animal tissues by thiobarbitoric acid reaction. Anal Biochem. 1979;95:351–8. doi: 10.1016/0003-2697(79)90738-3. [DOI] [PubMed] [Google Scholar]
- 23.Huang TL, Liou CW, Lin TK. Serum thiobarbitoric acid-reactive substances and free thiol levels in schizophrenia patients: Effects of antipsychotic drugs. Psychiat Res. 2010;177:18–21. doi: 10.1016/j.psychres.2009.01.017. [DOI] [PubMed] [Google Scholar]
- 24.Kapczinski F, Dal-Pizzol F, Teixeria AL, Magalhaes PVS, Anna MKS, Klamt F. et al. Peripheral biomarkers and illness activity in bipolar disorder. J Psychiat Res. 2011;45:156–61. doi: 10.1016/j.jpsychires.2010.05.015. [DOI] [PubMed] [Google Scholar]
- 25.Khairova R, Pawar R, Salvadore G, Juruena MF, de Sousa RT, Soeiro-de-Souza MG, Salvador M, Zarate CA, Gattaz WF, Machado-Vieira R. Effects of lithium on oxidative stress parameters in healthy subjects. Mol Med Reports. 2012;5:680–2. doi: 10.3892/mmr.2011.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kuloglu M, Ustundag B, Atmaca M, Cantan H, Tezcan AE, Cinkilinc N. Lipid peroxidation and antioxidant enzyme levels in patients with schizophrenia and bipolar disorder. Cell Biochem Funct. 2002;20:171–5. doi: 10.1002/cbf.940. [DOI] [PubMed] [Google Scholar]
- 27.Kunz M, Gama CS, Andreazza AC, Salvador M, Cereser KM, Gomes FA. et al. Elevated serup superoxide dismutase and thiobarbitoric acid reactive substances in different phases of bipolar disorder and in schizophrenia. Prog Neuro-Psychopharmacol Biol Psychiat. 2008;32:1677–81. doi: 10.1016/j.pnpbp.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 28.Machado-Vieira R, Andreazza AC, Viale CI, Zanatto V, Cereser V Jr, Vargas RS. et al. Oxidative stress parameters in unmedicated and treated bipolar subjects during initial manic episode: A possible role for lithium antioxidant effects. Neurosci Lett. 2007;421:33–6. doi: 10.1016/j.neulet.2007.05.016. [DOI] [PubMed] [Google Scholar]
- 29.Mahadik SP, Mukherjee S, Scheffer R, Correnti EE, Mahadik JS. Elevated plasma lipid peroxides at the onset of nonaffective psychosis. Biol Psychiat. 1998;43:674–9. doi: 10.1016/S0006-3223(97)00282-5. [DOI] [PubMed] [Google Scholar]
- 30.Young IS, Trimble ER. Measurement of malondialdehyde in plasma by high performance liquid chromatography with fluorometric detection. Ann Clin Biochem. 1991;28:504–8. doi: 10.1177/000456329102800514. [DOI] [PubMed] [Google Scholar]
- 31.Draper HH, Hadley M. Malondialdehyde determination as index of lipid peroxidation. Methods Enzymol. 1990;186:421–31. doi: 10.1016/0076-6879(90)86135-I. [DOI] [PubMed] [Google Scholar]
- 32.Bulut M, Selek S, Gergeriloglu S, Savas HA, Yilmaz HR, Yuce M, Ekici G. Malondialdehyde levels in adult attention-deficit hyperactivity disorder. J Psychiatry Neurosci. 2007;32:435–8. [PMC free article] [PubMed] [Google Scholar]
- 33.Padurariu M, Ciobica A, Dobrin I, Stefanescu C. Evaluation of antioxidant enzymes activities and lipid peroxidation in schizophrenic patients treated with typical and atypical antipsychotics. Neurosci Lett. 2010;479:317–20. doi: 10.1016/j.neulet.2010.05.088. [DOI] [PubMed] [Google Scholar]
- 34.Ranjekar P, Hinge A, Hegde MV, Ghate M, Kale A, Sitasawad S. et al. Depressed antioxidant enzymes and membrane essential polyunsaturated fatty acids in schizophrenic and bipolar mood disorder patients. Psychiat Res. 2003;121:109–22. doi: 10.1016/S0165-1781(03)00220-8. [DOI] [PubMed] [Google Scholar]
- 35.Tsai MC, Huang TL. Thiobarbitoric acid reactive substances (TBARS) is a state biomarker of oxidative stress in bipolar patients in a manic phase. J Affective Disorders. 2015;173:22–6. doi: 10.1016/j.jad. [DOI] [PubMed] [Google Scholar]
- 36.Tsai MC, Liou CW, Lin TK, Lin IM, Huang TL. Changes in oxidative stress markers in patients with schizophrenia: The effect of antipsychotic drugs. Psychiat Res. 2013;209:284–90. doi: 10.1016/j.psychres.2013.01.023. [DOI] [PubMed] [Google Scholar]
- 37. Khoubnasabjafari M, Ansarin K, Jouyban A. Critical review of malondialdehyde analysis in biological samples. Cur Pharm Anal 2015, in press. doi: 10.2174/1573412911666150505185343.
- 38.Poubelle P, Chainti-Euil J, Besadoux J, Boitman F, Simon L, Crastes de Paulet A. Plasma lipoperoxides and aging critical assessment of the thiobarbituric acid method for the measurement of lipoperoxides and malondialdehyde. Biomedicine. 1982;36:164–6. [PubMed] [Google Scholar]
- 39.Gutteridge JMC. Free-radical damage to lipids, amino acids, carbohydrates and nucleic acids determined by thiobarbituric acid reactivity. Int J Biochem. 1982;14:649–53. doi: 10.1016/0020-711X(82)90050-7. [DOI] [PubMed] [Google Scholar]
- 40.Buege JA, Aust SD. Microsomal lipid peroxidation. Methods Enzymol. 1978;12:302–10. doi: 10.1016/S0076-6879(78)52032-6. [DOI] [PubMed] [Google Scholar]
- 41.Lepage P, Heckel C, Humbert S, Stahl S, Rautmann G. Preparative steps necessary for the accurate measurement of malondialdehyde by high-performance liquid chromatography. Anal Biochem. 1991;197:277–83. doi: 10.1016/0003-2697(91)90392-7. [DOI] [PubMed] [Google Scholar]
- 42.Hackett C, Linley-Adams M, Lloyd B, Walker V. Plasma malondialdehyde: A poor measure of in vivo lipid peroxidation. Clin Chem. 1988;34:208. [PubMed] [Google Scholar]
- 43.Wade CR, van Rij AM. Plasma malondialdehyde, lipid peroxides, and the thiobarbituric acid reaction. Clin Chem. 1989;35:336. [PubMed] [Google Scholar]
- 44.Nur Aksoy S, Saygili EI, Bulbul F, Bahar A, Savas H, Virit O, Altindag A, Bayram A, Taracioglu M. Myeloperoxidase enzyme levels and oxidative stress in bipolar disorder. Afr J Biotechnol. 2010;9:3318–23. doi: 10.5897/AJB10.067. [DOI] [Google Scholar]
- 45.Bulut M, Selek S, Bez Y, Kaya MC, Gunes M, Karababa F, Celik H, Savas HA. Lipid peroxidation markers in adult attention deficit hyperactivity disorder: New findings for oxidative stress. Psyciatry Res. 2013;209:638–42. doi: 10.1016/j.psychres.2013.02.025. [DOI] [PubMed] [Google Scholar]
- 46.Il’yasova D, Scarbrough P, Spasojevic I. Urinary biomarkers of oxidative status. Clin Chim Acta. 2012;413:1446–53. doi: 10.1016/j.cca.2012.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]


