Abstract
Background:
Middle cerebral artery (MCA) fenestration is a very rare anatomical variant of the MCA, incidentally found during magnetic resonance or computed tomography angiography. It has an incidence of 0.6%. Unlike fenestration of the posterior cerebral arterial circulation, fenestration of the anterior cerebral arterial circulation has not been well described.
Methods:
We present the rare case of a patient who was admitted for a ruptured aneurysm of the MCA arising at the site of the fenestration of the MCA and also an unruptured fusiform aneurysm of the right posterior communicating artery and a distal anterior cerebral artery (ACA) aneurysm.
Results:
The patient underwent craniotomy with microsurgical aneurysm clipping and the previously undiagnosed ruptured aneurysm, at the site of the fenestration of the MCA, arose immediately. Postoperatively, the patient awoke without a deficit. After treatment of postoperative bacterial meningitis, he was discharged on the 26th postoperative day in good condition without any neurologic deficit. Six months after the first surgery, he was operated for the distal azygos ACA aneurysm.
Conclusion:
Anomalies of the intracranial vasculature are common, and we describe a rare case of left MCA fenestration with an associated ruptured aneurysm at the site of the fenestration. In the literature, cases of fenestration of the MCA are sporadically reported and are only incidental findings.
Keywords: Aneurysm, anterior cerebral artery, fenestration, middle cerebral artery
INTRODUCTION
Anomalies of the intracranial circulation are important for the cerebrovascular surgeons and neurointerventionalists to recognize, especially when the patient is symptomatic. Middle cerebral artery (MCA) variants are encountered less frequently than variants of other intracranial arteries.[5,20,31]
According the literature review, there are three variations of the MCA: Duplicated MCA,[10,12,26] accessory MCA,[10,11,13,16,23,24,25] and fenestrated MCA.[6,17,28,30] A fenestrated MCA is a rare anatomical anomaly, with an incidence of 1% at autopsy and 0.17% on cerebral angiography.[8,9,21,22,29] Fenestration is defined as the division of the lumen of an arterial segment into two distinct parallel channels.[4,7,22] Most probably, the mechanism leading to MCA fenestration is thought to be closely related to the interference in the evolution process during embryonic development.[22]
The fenestrated MCA is usually found incidentally, either during an angiography or an operation performed for pathology, and symptomatic intracranial hemorrhage is very rare.[3,8,21,22] To the best of our knowledge, there have been few reports on the presences of an aneurysm at the site of the fenestration that had been presented with subarachnoid hemorrhage (SAH). We describe a very rare case of multiple aneurysms with a ruptured aneurysm of the MCA, arising at the site of the fenestration of the MCA and another at the site of the right azygos A2 segment.
CASE REPORT
A 52-year-old man was transferred to our emergency room with the loss of consciousness and history of a first episode of seizure, 2 h earlier. He had a history of headache during the past several days. He had no previous history of seizure or neurologic signs. In the brief evaluation, his Glasgow Comma Scale was 11, without a focal neurologic deficit. The vital signs were within normal ranges. Emergent computed tomographic (CT) scan revealed SAH in the basal cisterns and both sylvian fissures and anterior interhemispheric region [Figure 1]. Dilated lateral ventricle and interstitial edema due to acute hydrocephalus were demonstrated. The patient was transferred to the operation room, and external ventricular drainage was placed in the right frontal horn of the lateral ventricle urgently. The patient was admitted to the Intensive Care Unit. Brain CT angiography and digital subtraction angiography of both internal carotid arteries (ICAs) and both vertebral arteries demonstrated a ruptured aneurysm of the left MCA and an unruptured fusiform aneurysm of right posterior communicating artery and an aneurysm at the site of the distal azygos anterior cerebral artery (ACA) [Figure 2]. Furthermore, another vascular variant reported in our patient was the azygos ACA in the A2 segment.
Figure 1.

Brain computed tomography scan revealed subarachnoid hemorrhage in basal cisterns and both sylvian fissures and anterior interhemispheric region. Dilated lateral ventricles and interstitial edema due to acute hydrocephalus is obvious
Figure 2.
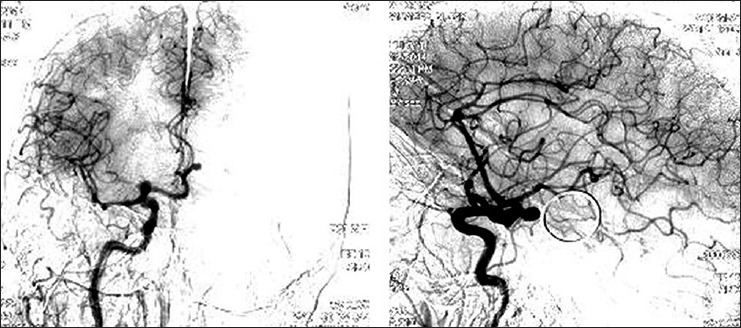
Four vessels digital subtraction angiography demonstrated a ruptured aneurysm of the left middle cerebral artery, an unruptured fusiform aneurysm of the right posterior communicating artery and an aneurysm at the site of the distal azygos anterior cerebral artery
The patient underwent surgery, with the left pterional approach. A left frontotemporal craniotomy was performed, and an aneurysm was exposed through the sylvian fissure. The saccular aneurysm, with superior projection in the bifurcation of the left MCA, was clipped with a 7 mm straight clip. After dissection of the aneurysm, fenestration of the MCA was exposed immediately at the aneurysm's site [Figure 3]. The postoperative course was complicated with bacterial meningitis that was treated with antibiotic therapy. After 26 days, the patient was discharged without neurologic deficit.
Figure 3.

Postoperative computed tomography angiography revealed an aneurysm at the site of the fenestration of the middle cerebral artery
Follow-up angiography performed 3 months postoperatively showed complete obstruction of the previous left MCA aneurysms. The second surgery was done 6 months after first surgery. The neurosurgeons opted for a right interhemispheric approach and a saccular aneurysm, with superolateral projection beneath the cingulate gyrus and 15 mm before bifurcation of the pericallosal and callosomarginal arteries was clipped with a 6 mm mini-clip [Figure 4].
Figure 4.

Postoperative computed tomography angiography revealed an aneurysm at the site of the right azygos A2 artery
Monoparesis of left hand occurred as a complication of the second surgery. Patient muscle force in its left hand was 4/5, with mild spasticity at 4 months follow-up after surgery.
DISCUSSION
According to Teal et al. study,[27] accessory MCA, duplicated MCA and fenestrated MCA are variations in MCA. An accessory MCA is classically described as arising from the A1 segment of the ACA, and angiographic studies have shown that accessory MCAs most commonly arise from the distal A1. A duplicate MCA occurs when two vessels arise directly from the ICA supplying the ipsilateral MCA territory.[2,20,27,31]
Fenestration is a rare finding, and it is mostly found in the anterior communicating artery (ACoA) or the vertebrobasilar system.[1,7,21,29] The low incidence of this anomaly, based on cerebral angiography or magnetic resonance angiography (MRA) up to date may have been underestimated because it is often missed by poor quality angiography or MRA.[22] Embryologic development of the MCA is first recognized in 7-12 mm embryos, as small buds originating proximal to the ACA on the primitive ICA. At an embryonal length of 16–18 mm, the MCA becomes more prominent and develops branches in the cerebral hemisphere.[26] Despite the embryologic understanding of MCA development in relation to surrounding vasculature, the causative factors for the development of MCA anomalies have yet to be elucidated.[14]
Okudera et al.[18] classified the fenestrated MCA into three types: The “proximal type” at the proximal portion of M1, the “intermediate type” in the central portion of the M1, and the “distal type” at the portion just before the division of M2. They reported that the proximal type was the most common type. Our case was the distal type, at the site of the MCA bifurcation.
According to the previous reports, the MCA variants have been regarded to have no clinical significance.[14,22,28] Uchino et al. reported that clinical manifestations of the aneurysm were more common in accessory MCA than duplicated or fenestrated MCA.[28] There are several reports in the literature about the presence of an aneurysm in MCA with the above variations.[12,13,17,23,26,30] Aneurysm in fenestrated MCA is less common than other variations,[28] and according to our knowledge, no aneurysm at the site of the fenestration has been previously reported.
Rarely, fenestrated MCA can be associated with a major territory infarction from occlusion of the fenestrated segment. Aggressive manipulations during interventional procedures should be avoided to prevent devastating results by arterial rupture.[22] Jeong et al.[7] reported five cases of MCA fenestration associated with cerebral infarction or ischemia, including one case of lacunar infarction and four cases of transient ischemic attack.
Based on Hager Paget's article,[19] at 35 days (12-14 mm stage), the primitive anterior division of the ICA develops a distinct distal branch, which is the stem of the ACA. By 40 days (16-18 mm stage), the stem of the ACA elongates medially toward its counterpart. At 44 days (20-24 mm stage), the channels of the midline cluster of plexiform anastomoses coalesce and form one or more ACoAs. In addition, the coalescing channels of the midline cluster of plexiform anastomoses give rise to a median ACA that originates from the ACA.
An anomaly in this stage is the azygos artery or solitary A2 segment that arises when the paired ACAs regress after formation and enlargement of the median ACA. Lin et al.[15] expressed that 41.1% of azygos A2 segments have a terminal aneurysm, which is most commonly located at the bifurcation of the pericallosal and callosomarginal arteries, and less frequently is found at the site of origin of the frontopolar or orbitofrontal branches of the ACA. In our case, a sacccular aneurysm was proximal to the azygos artery.
This case was very challenging due to the presence of three aneurysms, a ruptured aneurysm immediately at the fenestration site of the MCA, an azygos ACA in the A2 segment and a distal ACA aneurysm.
CONCLUSION
Although anomalies of the MCA are rare, neurosurgeons and neuroendovascular specialists should be familiar with the anatomic variations and the potential associated findings and sequels that can occur. Furthermore, in patients with multiple aneurysms, they should be aware about the presence of these variations when performing interventions. We suggest more in depth study about multiple aneurysms and variations in the cerebral circulation.
Footnotes
Contributor Information
Guive Sharifi, Email: gibnow@yahoo.com.
Mehrdad Hosseinzadeh Bakhtevari, Email: mhbakhtevari@yahoo.com.
Sofia Sabouri, Email: dr.sabouri@hotmail.com.
Omidvar Rezaei, Email: info@drrezaee.ir.
REFERENCES
- 1.Black SP, Ansbacher LE. Saccular aneurysm associated with segmental duplication of the basilar artery. A morphological study. J Neurosurg. 1984;61:1005–8. doi: 10.3171/jns.1984.61.6.1005. [DOI] [PubMed] [Google Scholar]
- 2.Crompton MR. The pathology of ruptured middle-cerebral aneurysms with special reference to the differences between the sexes. Lancet. 1962;2:421–5. doi: 10.1016/s0140-6736(62)90281-7. [DOI] [PubMed] [Google Scholar]
- 3.Deruty R, Pelissou-Guyotat I, Mottolese C, Bognar L, Laharotte JC, Turjman F. Fenestration of the middle cerebral artery and aneurysm at the site of the fenestration. Neurol Res. 1992;14:421–4. doi: 10.1080/01616412.1992.11740097. [DOI] [PubMed] [Google Scholar]
- 4.Gailloud P, Albayram S, Fasel JH, Beauchamp NJ, Murphy KJ. Angiographic and embryologic considerations in five cases of middle cerebral artery fenestration. AJNR Am J Neuroradiol. 2002;23:585–7. [PMC free article] [PubMed] [Google Scholar]
- 5.Gibo H, Carver CC, Rhoton AL, Jr, Lenkey C, Mitchell RJ. Microsurgical anatomy of the middle cerebral artery. J Neurosurg. 1981;54:151–69. doi: 10.3171/jns.1981.54.2.0151. [DOI] [PubMed] [Google Scholar]
- 6.Ito J, Maeda H, Inoue K, Onishi Y. Fenestration of the middle cerebral artery. Neuroradiology. 1977;13:37–9. doi: 10.1007/BF00335032. [DOI] [PubMed] [Google Scholar]
- 7.Jeong SK, Kwak HS, Cho YI. Middle cerebral artery fenestration in patients with cerebral ischemia. J Neurol Sci. 2008;275:181–4. doi: 10.1016/j.jns.2008.07.037. [DOI] [PubMed] [Google Scholar]
- 8.Kim MS, Hur JW, Lee JW, Lee HK. Middle cerebral artery anomalies detected by conventional angiography and magnetic resonance angiography. J Korean Neurosurg Soc. 2005;37:263–7. [Google Scholar]
- 9.Kim MS, Lee HK. The angiographic feature and clinical implication of accessory middle cerebral artery. J Korean Neurosurg Soc. 2009;45:289–92. doi: 10.3340/jkns.2009.45.5.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Komiyama M, Nakajima H, Nishikawa M, Yasui T. Middle cerebral artery variations: Duplicated and accessory arteries. AJNR Am J Neuroradiol. 1998;19:45–9. [PMC free article] [PubMed] [Google Scholar]
- 11.Komiyama M, Nishikawa M, Yasui T. The accessory middle cerebral artery as a collateral blood supply. AJNR Am J Neuroradiol. 1997;18:587–90. [PMC free article] [PubMed] [Google Scholar]
- 12.Koyama S, Kotani A, Sasaki J, Tazoe M, Tsubokawa T. Ruptured aneurysm at the origin of duplication of the middle cerebral artery – Case report. Neurol Med Chir (Tokyo) 1995;35:671–3. doi: 10.2176/nmc.35.671. [DOI] [PubMed] [Google Scholar]
- 13.Kuwabara S, Naitoh H. Ruptured aneurysm at the origin of the accessory middle cerebral artery: Case report. Neurosurgery. 1990;26:320–2. doi: 10.1097/00006123-199002000-00022. [DOI] [PubMed] [Google Scholar]
- 14.LaBorde DV, Mason AM, Riley J, Dion JE, Barrow DL. Aneurysm of a duplicate middle cerebral artery. World Neurosurg. 2012;77:201.e1–4. doi: 10.1016/j.wneu.2011.03.038. [DOI] [PubMed] [Google Scholar]
- 15.Lin CL, Kwan AL, Howng SL. Surgical outcome of anterior communicating artery aneurysms. Kaohsiung J Med Sci. 1998;14:561–8. [PubMed] [Google Scholar]
- 16.Mueller DP, Sato Y, Yuh WT. Accessory middle cerebral artery as a source of collateral blood flow. AJNR Am J Neuroradiol. 1991;12:1223–4. [PMC free article] [PubMed] [Google Scholar]
- 17.Nakamura H, Takada A, Hide T, Ushio Y. Fenestration of the middle cerebral artery associated with an aneurysm – Case report. Neurol Med Chir (Tokyo) 1994;34:555–7. doi: 10.2176/nmc.34.555. [DOI] [PubMed] [Google Scholar]
- 18.Okudera H, Koike J, Toba Y, Kuroyanagi T, Kyoshima K, Kobayashi S. Fenestration of the middle cerebral artery associated with cerebral infarction. Report of two cases. Neurol Med Chir (Tokyo) 1987;27:559–63. doi: 10.2176/nmc.27.559. [DOI] [PubMed] [Google Scholar]
- 19.Padget DH. The development of the cranial arteries in the human embryo. Contrib Embryol. 1948;32:205–61. [Google Scholar]
- 20.Rhoton AL., Jr The supratentorial arteries. Neurosurgery. 2002;51(4 Suppl):S53–120. [PubMed] [Google Scholar]
- 21.Sanders WP, Sorek PA, Mehta BA. Fenestration of intracranial arteries with special attention to associated aneurysms and other anomalies. AJNR Am J Neuroradiol. 1993;14:675–80. [PMC free article] [PubMed] [Google Scholar]
- 22.Seo BS, Lee YS, Lee JH, Lee HG, Ryu KY, Kang DG. Mechanical thrombolysis using coil in acute occlusion of fenestrate m1 segment. J Cerebrovasc Endovasc Neurosurg. 2012;14:108–12. doi: 10.7461/jcen.2012.14.2.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sugita S, Yuge T, Miyagi J, Fujimura N, Shigemori M. Giant aneurysm at the origin of the accessory middle cerebral artery. Surg Neurol. 1995;44:128–30. doi: 10.1016/0090-3019(95)00128-x. [DOI] [PubMed] [Google Scholar]
- 24.Tacconi L, Johnston FG, Symon L. Accessory middle cerebral artery. Case report. J Neurosurg. 1995;83:916–8. doi: 10.3171/jns.1995.83.5.0916. [DOI] [PubMed] [Google Scholar]
- 25.Takahashi S, Hoshino F, Uemura K, Takahashi A, Sakamoto K. Accessory middle cerebral artery: Is it a variant form of the recurrent artery of Heubner? AJNR Am J Neuroradiol. 1989;10:563–8. [PMC free article] [PubMed] [Google Scholar]
- 26.Takahashi T, Suzuki S, Ohkuma H, Iwabuchi T. Aneurysm at a duplication of the middle cerebral artery. AJNR Am J Neuroradiol. 1994;15:1166–8. [PMC free article] [PubMed] [Google Scholar]
- 27.Teal JS, Rumbaugh CL, Bergeron RT, Segall HD. Anomalies of the middle cerebral artery: Accessory artery, duplication, and early bifurcation. AJR Am J Roentgenol. 1973;118:567–75. doi: 10.2214/ajr.118.3.567. [DOI] [PubMed] [Google Scholar]
- 28.Uchino A, Kato A, Takase Y, Kudo S. Middle cerebral artery variations detected by magnetic resonance angiography. Eur Radiol. 2000;10:560–3. doi: 10.1007/s003300050960. [DOI] [PubMed] [Google Scholar]
- 29.Uchino A, Takase Y, Nomiyama K, Egashira R, Kudo S. Fenestration of the middle cerebral artery detected by MR angiography. Magn Reson Med Sci. 2006;5:51–5. doi: 10.2463/mrms.5.51. [DOI] [PubMed] [Google Scholar]
- 30.Ueda T, Goya T, Wakisaka S, Kinoshita K. Fenestrations of the middle cerebral artery associated with aneurysms. AJNR Am J Neuroradiol. 1984;5:639–40. [PMC free article] [PubMed] [Google Scholar]
- 31.Umansky F, Dujovny M, Ausman JI, Diaz FG, Mirchandani HG. Anomalies and variations of the middle cerebral artery: A microanatomical study. Neurosurgery. 1988;22(6 Pt 1):1023–7. doi: 10.1227/00006123-198806010-00008. [DOI] [PubMed] [Google Scholar]


