Abstract
Objective
Research has demonstrated the effect of adverse childhood experiences (ACE) on later physiologic function and illness development. In the urologic literature, the relationship between bladder dysfunction and neuropsychiatric disorders is well documented. Observations in pediatric urology clinical practice suggest that a blend of these two areas of research can inform care of patients with voiding dysfunction.
Methods
Retrospective review of 216 patients seen in a single pediatric urology clinic by a single provider over a 24-month period. A descriptive, correlational study design was used to assess the extent to which ACEs and neuropsychiatric disorders affected resolution of symptoms when patients were treated with a bowel and bladder retraining program. Patients were selected using diagnostic codes related to voiding dysfunction and a retrospective chart review was conducted.
Results
A majority of patients who were seen for voiding dysfunction (60%) had at least one psychosocial factor. There is a greater prevalence of ACEs (51%) than neuropsychiatric disorders (25%). Children with psychosocial factors dropped out of treatment at a higher rate than those with no factors. When factors were looked at separately, neuropsychiatric disorders were more likely to impede treatment progress than ACEs.
Conclusions
ACEs and neuropsychiatric disorders affect patients’ ability to make progress with bowel and bladder retraining and to stay in treatment. Efforts specifically aimed at maintaining therapeutic relationships with patients who have ACEs are needed to fully treat this group, which typically has a high drop-out rate but high rate of resolution if they are able to stay involved in treatment.
Introduction
Among children with lower urinary tract symptoms (LUTS), it is recognized that there is an increased rate of psychological and behavioral disorders, and that the presence of these factors interferes with treatment and results in less favorable outcomes [1]. For example, among children with voiding dysfunction, those with attention deficit hyperactivity disorder (ADHD) have more extensive LUTS [2,3], and are more difficult to treat [4]. Children who postpone voiding and who have urge incontinence are known to have increased rates of withdrawn, aggressive, and delinquent behaviors [5]. Children with more severe voiding dysfunction are known to exhibit more internalizing, externalizing, and overall psychosocial difficulties [6]. The emphasis of research in this area to date has been on the rates and treatment success among children with psychological and behavioral disorders, and has generally found that children with these factors have lower rates of treatment success.
For the purpose of this study, the authors grouped psychological, behavioral, and neurobiological disorders into one group termed neuropsychiatric disorders, which includes: ADHD, learning disability, dyslexia, developmental delay, severe seizure disorders, autism and Asperger’s, mental retardation, bipolar disorder, depression, and anxiety. The authors acknowledge the wide array of severity and neurodevelopmental or neurochemical etiologies of the disorders in this group. However, these are all known diagnoses that patients have prior to referral to pediatric urology, and they all present a high suspicion in clinical work for barriers to treatment progress, which can be tested out in this study when compared with patients who do not have these diagnoses.
Quite separately, and often in addition to psychological and behavioral disorders, are the adverse life experiences that children with LUTS have had. In pediatric urologic clinical work there is a notably high rate of patient experience with adversity (including having experienced neglect, abuse, divorce, adoption, multiple family relocations, incarceration of a parent, etc.).
Adverse childhood experiences (ACEs) have been an increasingly well-studied area outside of urology since the 1990s, with demonstration of the lasting effect of ACEs (such as psychological, physical, or sexual abuse; violence against mother, living with household members who were substance abusers, mentally ill or suicidal, or ever imprisoned) on adult health (including 12-fold increased health risks for alcoholism, drug abuse, depression and suicide attempt, increased rates of smoking and poor self-rated health, and increased rates of multiple adult diseases) [7]. Increased rates of chronic physical conditions are known to occur among women with histories of physical and sexual abuse [8]. Focus has recently begun to shift to investigation of markers of chronic stress during childhood. Adverse events in middle childhood predicted increased levels of C reactive protein at age 10 and in mid-adolescence [9].
The increasingly understood, broad implications of ACEs on adult and childhood health risks suggests that pediatric urology clinical work may be informed by awareness of patients’ histories of ACEs as well as neuropsychiatric and behavioral disorders. Recent research has begun to suggest screening for life stressors in addition to psychological disorders in pediatric urology clinical work [10].
With this in mind, the authors sought to assess the rates of ACEs as well as neuropsychiatric disorders among patients with LUTS. The primary purpose of this study was to test the clinical observation that there are a number of patients with LUTS who have both ACEs and neuropsychiatric disorders, but there are also a number of patients who have ACEs and no neuropsychiatric disorders. It is this latter group that has not been previously described in detail in urology literature.
The secondary purpose of this study was to compare treatment success among patients with ACEs and neuropsychiatric disorders. Clinical work by the primary author with patients experiencing LUTS suggested that ACEs and neuropsychiatric disorders are prominent, are important factors in successful treatment, and may affect follow-up rate, but are not always barriers to success as previously documented by other researchers.
This study was reviewed by the authors’ institutional review board (committee for the protection of human subjects) and was deemed to be exempt from further review.
Methods
Design
A descriptive analysis was performed to assess the extent to which ACEs, neuropsychiatric disorders, or both, affected resolution of symptoms when patients undertook a bowel and bladder retraining program.
Subjects
A retrospective chart review was conducted on 216 patients seen by a single nurse practitioner over a period of 2 years. Of the 216 patients, 55% were female, 45% were male. Patients ranged in age from 3 to 18 years, with a mean of 9.7. Patients were selected using diagnostic codes related to voiding dysfunction, including: urgency, frequency, incontinence, dysuria, urinary tract infection, hesitancy or straining to urinate, diurnal enuresis, and nocturnal enuresis. Patients with neurogenic bladder and cerebral palsy were excluded. All patients had been started on a bladder and bowel retraining program involving a combination of a bowel clean out, prompted voiding every 2 hours, pelvic floor relaxation while voiding (with prompted simulation of a squatting body position with feet on a high stool, legs spread, deep breaths to relax, and taking time to empty adequately), and fluid restriction in evenings if the patient experienced nocturnal enuresis. A minority of patients were also prescribed medications such as oxybutynin, desmopressin, and tolterodine. Patients were routinely seen for a follow-up visit 2–4 weeks after the initial consult, and then were seen 1–3 months later, and as progress occurred, at 3–6 month intervals as needed.
After patients were selected by diagnostic criteria, information was collected via retrospective chart review regarding the presence or absence of adverse life experiences. The single clinician treating these patients had specifically asked each patient at the initial consult about ACEs including: divorce, abuse, adoption, moving multiple times, or recent death of a family member, and then encouraged report of other stressors seen as significant by the child or parent. A health history form asked specifically about neuropsychiatric disorders recorded including: diagnosed ADHD, autism spectrum, Asperger’s syndrome, mental retardation, dyslexia, learning disabilities, developmental delay, severe seizure disorder, anxiety, depression, and bipolar disorder.
Statistical analyses were performed using SPSS Windows version 16.0 (SPSS Inc, Chicago, IL, USA). Psychosocial data were expressed as counts and percentages. Demographic data were expressed as mean, median, mode, and percentages.
Results
ACEs
Adverse childhood experiences were analyzed as a group which included: neglect, abuse, divorce, adoption, multiple family relocations, incarceration of a parent, and other factors that parent or child saw as significantly stressful. Fifty-one percent of patients had one or more ACE. The largest group among these (38%) had experienced recent divorce or were in a shared custody arrangement. Fourteen percent had moved in the past 2 years, and 7% had moved multiple times. Thirteen percent had experienced or witnessed domestic abuse. Seven percent had been adopted or been in foster care. Eight percent had recently had a death in the family. See Table 1 for a graphic depiction of this distribution. Many patients had experienced multiple ACEs.
Table 1.
Distribution of ACEs
| N (%) | |
|---|---|
| Total having ACEs | 110 (51) |
| Divorce/Shared custody | 73 (38) |
| Domestic abuse (experienced/witnessed) | 25 (13) |
| Moved in the past 2 years | 26 (14) |
| Moved multiple times | 14 (7) |
| Adoption/foster | 13 (7) |
| Recent death in family | 16 (8) |
| Family member incarcerated | 2 (1) |
| Other | 22 (12) |
Neuropsychiatric disorders
For the purpose of grouping non-ACE factors which prominently appear to be barriers to treatment progress, psychological, behavioral, and neurobiological disorders were merged into one group termed neuropsychiatric disorders, which includes: ADHD, learning disability, dyslexia, developmental delay, severe seizure disorders, autism and Asperger’s, mental retardation, bipolar disorder, depression, and anxiety. Twenty-five percent of voiding dysfunction patients had a neuropsychiatric disorder. Thirty-seven percent of these had a learning disability, a severe seizure disorder or developmental disorder. Thirty percent had ADHD. Thirteen percent had anxiety, depression or bipolar disorder. Eleven percent had autism, Asperger’s, dyslexia or mental retardation. See Table 2 for a graphic depiction of this distribution.
Table 2.
Distribution of neuropsychiatric disorders
| N (%) | |
|---|---|
| Total having neuropsychiatric disorders | 59 (25) |
| ADD_ADHD | 25 (30) |
| Autism, Asperger’s, mental retardation | 9 (11) |
| Learning disability, developmental delay, dyslexia, severe seizure disorder | 30 (37) |
| Anxiety, depression, bipolar | 11 (13) |
| Other | 4 (5) |
Sixty percent of patients had either ACEs, neuropsychiatric disorders, or both.
Rate of treatment progress
To gauge degree of progress toward resolution of symptoms, three categories were used during the chart review: no progress, some progress, and complete resolution of symptoms. The degree of progress that occurred over the entire patient care relationship was evaluated for this study. Patients with neuropsychiatric disorders experienced lower rates of progress than patients with neither ACEs nor neuropsychiatric disorders as factors. Patients with only ACEs had nearly the same rate of total resolution of symptoms with treatment (48%) compared with patients with neither factor. However, patients with ACEs saw a higher rate of partial success (63%) compared with patients with neither factor. Patients who had both ACEs and neuropsychiatric disorders had higher rates of partial and complete resolution of symptoms compared with patients with no factors. See Figures 1, 2, and 3 for graphic representation of the varying rates of progress for each group of patients.
Figure 1.
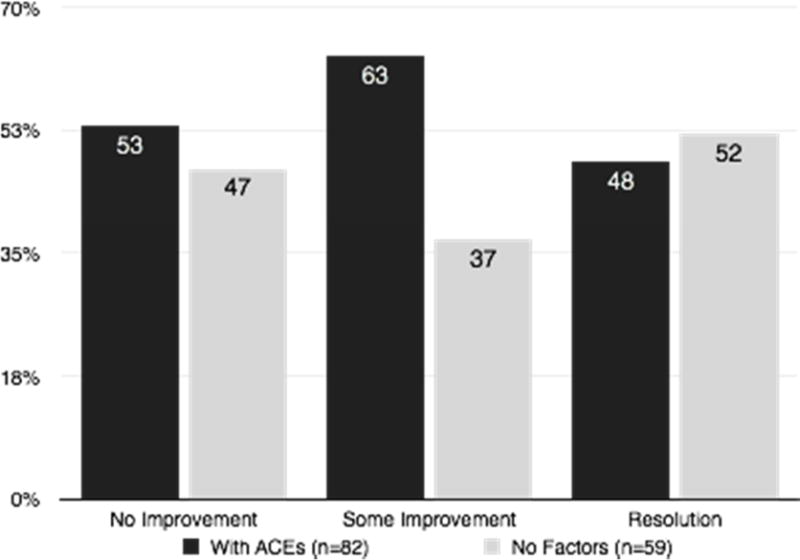
Rates of treatment progress for patients with ACEs compared with patients with no neuropsychiatric disorders or ACEs.
Figure 2.
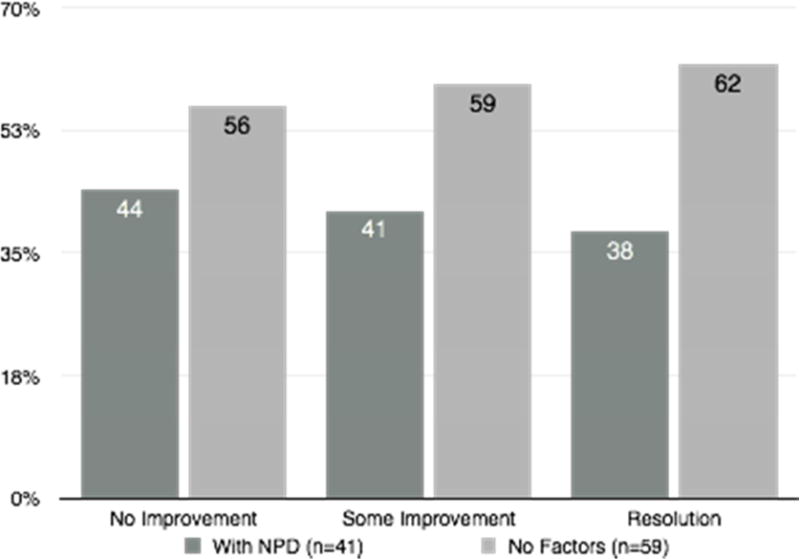
Rates of treatment progress for patients with neuropsychiatric disorders compared with patients with no neuropsychiatric disorders or ACEs.
Figure 3.
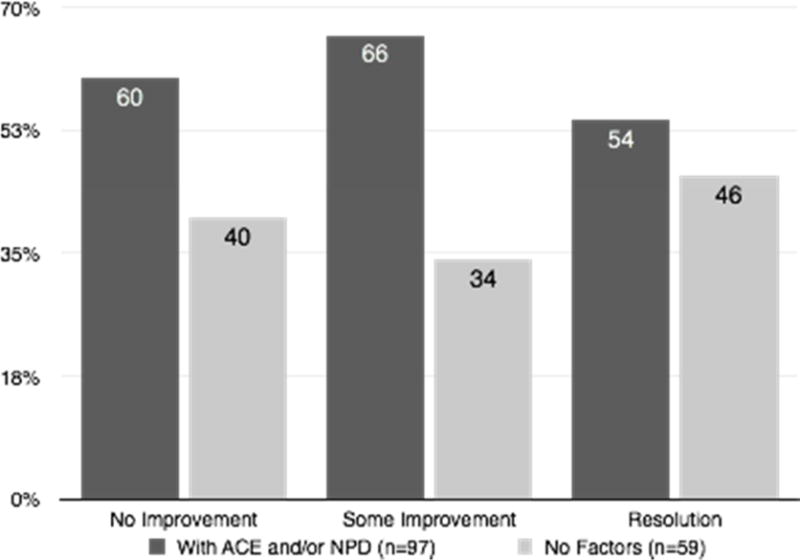
Rates of treatment progress for patients with neuropsychiatric disorders, ACEs or both compared with patients with no neuropsychiatric disorders or ACEs.
Rate of drop-out from treatment
The total number of patients who dropped out of treatment was 49 (or 23%). Of these, 61% had ACEs or neuropsychiatric disorders. Thirty-nine percent of patients who dropped out of treatment did not have either. Because of a lack of response by families in the scheduling process, the reason for drop-out was not recorded in this study.
Discussion
This study demonstrates that among patients with voiding dysfunction there is a high rate of ACEs in children who do not have diagnosed psychological or behavioral problems. Von Gontard [11] has sorted the various types of incontinence and enuresis by their most common psychological presentations, and this type of paired discussion of psychological and urologic symptoms is very informative for clinicians working with children experiencing LUTS. The present study offers additional information about non-urologic factors that frequently accompany urinary symptoms. Lower urinary tract symptoms may be the presenting symptom for children struggling with the effects of adverse childhood experiences, perhaps occurring even in the absence of other behavioral or psychological symptoms. Further study in this area will require consistent definition of the term ‘adverse childhood experiences’ [12].
Greater clarity is also needed of the physiologic cascade of events that occurs during chronic stress in terms of how it affects pelvic floor dysfunction. Studies with rat models have documented social stress causing urinary retention and bladder dysfunction by increasing corticotropin releasing factor (CRF) and CRF-immunoreactive neurons in Barrington’s nucleus of the spine [13]. However, an equivalent explanation of the stress response as it relates to urine holding and pelvic floor function is not readily found in urologic literature. Such an explanation would improve understanding of the physiologic interaction of chronic stress, life events, and voiding dysfunction.
The authors recognize that the broad variety of conditions grouped together in this study as ‘neuropsychiatric disorders’ in some ways have little in common with one another aside from their clinical prominence as factors that seem to impede progress with bowel and bladder retraining. The focus of this study was to focus on ACEs, with NPDs as a point of comparison as they were already known to present barriers to treatment success. However, future study dividing these neuropsychiatric disorders into neurological and non-neurological would provide further understanding for clinical purposes.
The findings of this study support previous findings that patients with neuropsychiatric disorders have lower rates of progress with treatment and a higher rate of drop-out from treatment. Patients with ACEs share the higher drop-out rate, but despite this, patients with ACEs made good progress in treatment. These patients saw a higher rate of partial resolution of symptoms than patients with no factors, and experienced total resolution of symptoms at nearly the same rate. This is an important difference and likely highlights the cognitive involvement of some of the neuropsychiatric disorders, whereas ACEs may simply affect behavior which is more easily influenced in structured treatment.
The findings of this study demonstrate the need for further research in pediatric urology to describe and clarify the cascade of events that occurs in the midst of ACEs, including chronic stress, elevated cortisol level, and the specific way that this affects pelvic floor function, leading to bowel and bladder dysfunction. This series of events involved in chronic stress is well explained in ACE research, but less so in urology research where the complex interplay of cortisol level, bowel and bladder sensation, and pelvic floor tension are involved.
Finally, the rate of drop-out from treatment for patients with ACEs and/or neuropsychiatric disorders was higher than in patients with no factors. Admittedly, the meaning of drop-out rate is unclear. Patients may drop-out because they have been remarkably successful after beginning bowel and bladder retraining, and no longer need support of the clinician. Conversely, dropout may be caused by inability of the family to carry out recommendations, inability to obtain transportation to follow-up appointments, inability to afford cost of visits, or any number of other reasons.
Conclusion
There is broad recognition among urology providers that children with LUTS have elevated rates of neuropsychiatric and behavioral disorders. This study encourages urology providers to obtain a broader and more thorough understanding of their patients’ risk factors for treatment failure and drop-out rate by considering ACEs separately, and in addition to neuropsychiatric and behavioral disorders. The presence of ACEs may precede presentation of psychological or behavioral problems.
By spending time in the initial consult collecting a thorough history of ACEs as well as neuropsychiatric disorders, pediatric urology nurses, nurse practitioners, and surgeons can focus efforts and plan on specific strategies to increase follow-up rate and treatment success and decrease rates of regression of LUTS, particularly for patients with neuropsychiatric disorders who have a higher rate of drop-out from treatment.
Acknowledgments
Funding: This study was supported in part by the New Hampshire IDeA Network of Biological Research Excellence (NH-INBRE) with grants from the National Center for Research Resources (5P20RR030360-03) and the National Institute of General Medical Sciences (8P20GM103506-03), National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest: None.
References
- 1.von Gontard A, Baeyens D, Van Hoecke E, Warzak W, Bachmann C. Psychological and psychiatric Issues in urinary and fecal incontinence. J Urol. 2011;185:1432–1437. doi: 10.1016/j.juro.2010.11.051. [DOI] [PubMed] [Google Scholar]
- 2.Schast A, Zderic S, Richter M, Berry A, Carr M. Quantifying demographic, urological and behavioral characteristics of children with lower urinary tract symptoms. J Pediatric Urol. 2008;4:127–133. doi: 10.1016/j.jpurol.2007.10.007. [DOI] [PubMed] [Google Scholar]
- 3.Duel BP, Steinberg-Epstein R, Hill M, Lerner M. A survey of voiding dysfunction in children with attention deficit-hyperactivity disorder. J Urol. 2003;170:1521–1523. doi: 10.1097/01.ju.0000091219.46560.7b. [DOI] [PubMed] [Google Scholar]
- 4.Crimmins CR, Rathburn SR, Husmann DA. Management of urinary incontinence and nocturnal enuresis in attention-deficit hyperactivity disorder. J Urol. 2003;170:1347. doi: 10.1097/01.ju.0000084669.59166.16. [DOI] [PubMed] [Google Scholar]
- 5.Lettgen B, von Gontard A, Olbing H, Heiken-Lowenau C, Schmitz I. Urge incontinence and voiding postponement in children: somatic and psychosocial factors. Acta Paediatr. 2002;91:978–984. doi: 10.1080/080352502760272696. [DOI] [PubMed] [Google Scholar]
- 6.Wolfe-Christensen C, Veenstra A, Kovacevic L, Elder J, Lakshmanan Y. Psychosocial difficulties in children referred to pediatric urology: A closer look. Urology. 2012;80:907–913. doi: 10.1016/j.urology.2012.04.077. [DOI] [PubMed] [Google Scholar]
- 7.Felitti V, Anda R, Nordenberg D, Williamson D, Spitz A, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) study. Am J Prev Med. 1998;14:245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 8.Romans S, Belaise C, Martin J, Morris E, Raffi A. Childhood abuse and later medical disorders in women. Psychother Psychosom. 2002;71:141–150. doi: 10.1159/000056281. [DOI] [PubMed] [Google Scholar]
- 9.Slopen N, Kubzansky L, McLaughlin K, Koenen K. Childhood adversity and inflammatory processes in youth: a prospective study. Psychoneuroendocrinology. 2012;38:188–200. doi: 10.1016/j.psyneuen.2012.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Oliver J, Campigotto M, Coplen D, Traxel E, Austin P. Psychosocial comorbidities and obesity are associated with lower urinary tract symptoms among children with voiding dysfunction. J Urol. 2013;190:511–515. doi: 10.1016/j.juro.2013.02.025. [DOI] [PubMed] [Google Scholar]
- 11.von Gontard A. Does psychological stress affect LUT function in children? ICI-RS 2011. Neurourol Urodyn. 2012;31:344–348. doi: 10.1002/nau.22216. [DOI] [PubMed] [Google Scholar]
- 12.Kalmakis K, Chandler C. Adverse childhood experiences: towards a clear conceptual meaning. J Adv Nurs. 2013 doi: 10.1111/jan.12329. preprint, submitted November 9, 2013. [DOI] [PubMed] [Google Scholar]
- 13.Wood S, Baez M, Bhatnagar S, Valentino R. Social stress-induced bladder dysfunction: potential role of corticotropin-releasing factor. Am J Physiol Regul Integr Comp Physiol. 2009;296:R1671–1678. doi: 10.1152/ajpregu.91013.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]


