Abstract
Background
Point-of-care ultrasound is a rapidly evolving component of internal medicine (IM) residency training. The optimal approach for teaching this skill remains unclear.
Objective
We sought to determine whether the addition of a longitudinal ultrasound curriculum to a stand-alone workshop for ultrasound training improved knowledge retention in IM residents.
Methods
We conducted an observational cohort study from July to December 2013. All postgraduate year (PGY)-1 IM residents attended an ultrasound workshop during orientation. Ability to identify static images of ascites, kidney, thyroid, pleural fluid, inferior vena cava, and internal jugular vein was assessed immediately after the workshop. An ultrasound curriculum, including morning report and ultrasound rounds, was initiated during the inpatient medicine rotation. PGY-1 residents were randomly assigned to participate in the longitudinal curriculum. Six months later, we conducted a follow-up survey with all PGY-1 residents.
Results
Forty-eight PGY-1 residents (67%) completed the postworkshop test and the 6-month follow-up test. Of these, 50% (24 of 48) had participated in the ultrasound curriculum. Residents not exposed to the curriculum showed a decline in the identification of ascites, pleural effusion, and internal jugular vein at 6 months (P < .05), whereas those who participated in the curriculum maintained their performance (P < .05).
Conclusions
Six months after exposure to a longitudinal ultrasound curriculum, residents were more likely to correctly identify ultrasound images of ascites, kidney, and pleural effusion. The addition of a longitudinal ultrasound curriculum may result in improved knowledge retention in IM residents.
Introduction
Point-of-care ultrasound is gaining popularity among internal medicine (IM) residency programs,1 and is commonly used for invasive bedside procedures resulting in decreased complications and improved patient safety.2,3 It can improve physical examination findings and diagnostic accuracy, and result in potential changes to management.4–6 Prior studies have shown that ultrasound knowledge and skill can be acquired through dedicated training.7,8 Various specialties, such as anesthesia,9 orthopedics,10 and emergency medicine,11 have implemented formal ultrasound training. Additionally, medical schools have added ultrasound as an educational tool in the gross anatomy laboratory with favorable results.12
Most studies on ultrasound education have included a 1-time training workshop. The literature suggests that point-of-care ultrasound knowledge, skills, and self-reported confidence decline over time.8,13,14 Research studies that focus on methods to foster retention of ultrasound knowledge and skills are lacking, so the aim of our study was to evaluate the impact of a longitudinal ultrasound curriculum on the long-term knowledge retention among postgraduate year (PGY)-1 IM residents.
Methods
We conducted an observational cohort study with retrospective analysis of all 72 PGY-1 residents (48 categorical and 24 preliminary) at our program. All participated in a half-day, simulation-based ultrasound workshop.7,8 The workshop consists of a 1-hour didactic session on the fundamentals of ultrasound, followed by 3 hours of hands-on education using both cadavers and live human subjects. The PGY-1 residents completed preworkshop and postworkshop examinations in which they reviewed static ultrasound images and were assessed on their ability to identify the following findings or structures: ascites, kidney, thyroid, pleural fluid, inferior vena cava, and internal jugular vein. The test was not multiple choice, and no background information was provided. Examination content was developed with the input of investigators (D.J.K., J.T.R., A.B.) with experience in point-of-care ultrasound, and was adapted from prior research.8 The workshop was previously shown to improve confidence7 and knowledge8 in identifying static ultrasound images.
Beginning July 2013, a longitudinal ultrasound curriculum was introduced in the inpatient general medicine services. Residents were randomly assigned by office staff to participate in the curriculum. The curriculum consisted of a monthly morning report and afternoon ultrasound rounds. The morning report was a didactic session of case-based images and small group discussion. There were 2 afternoon ultrasound rounding sessions per month led by 1 staff member and 1 or 2 chief residents (teacher-learner ratio of 1:3). The curriculum used an open-house format of hands-on scan time for residents on 2 medicine teams, allowing residents to come and go as patient care duties allowed. Patients were selected based on interesting findings and/or availability. Duration of rounds varied between 2 and 3 hours, and each session had a different ultrasound theme, the most common being pleural effusions, ascites, inferior vena cava assessment, kidneys, gallbladder, liver, and spleen. Teaching activities during these sessions included review of “knobology,” image acquisition, scanning planes, sonographic anatomy, image interpretation, independent scanning, and point-of-care decision making. Six months after the workshop, a follow-up test, identical to the prior test, was sent to all PGY-1 residents. Assessment of the test was blinded.
The study was deemed exempt by the Mayo Clinic Institutional Review Board.
To assess changes in image identification from postworkshop to 6 months later, we used the Cochran-Mantel-Haenszel statistics and P values for a general association alternative hypothesis. Fisher exact test was used to assess differences in correct image identification between groups at a single point in time. An α level of .05 was used for significance. All calculations were performed using SAS statistical software version 9.3 (SAS Institute Inc).
Results
Forty-eight of 72 residents (67%) completed the postworkshop test and 6-month follow-up. Of those, 24 (50%) participated in the longitudinal curriculum. Results for the images from the postworkshop test and the 6-month follow-up test, dichotomized by participation in the curriculum, are shown in the figure. Residents not exposed to the curriculum had a statistically significant decline in correct identification of ascites (−50%), thyroid (−29%), pleural effusion (−50%), and inferior vena cava (−30%) at the time of the follow-up test (all P < .02). The group that participated in the longitudinal curriculum was more likely to correctly identify the following ultrasound images 6 months after the workshop compared to those not enrolled: ascites (+45%, P = .003), kidney (+42%, P = .003), and pleural effusion (+50%, P = .001). There was no difference in identification of thyroid (+12%, P = .52), inferior vena cava (+9%, P = .77), internal jugular vein (+8%, P = .72), and the ability to identify the thyroid declined from initial test to the 6-month follow-up in the group exposed to the curriculum (−21%, P = .03).
FIGURE.
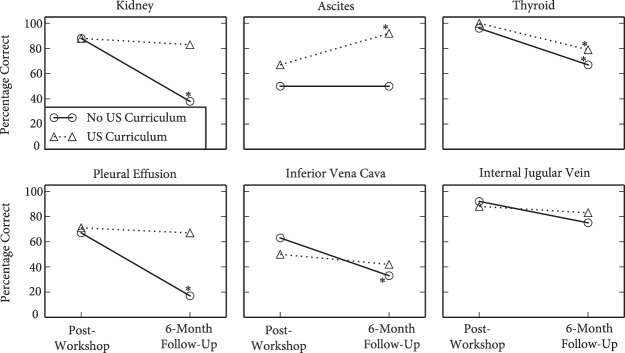
Percentage Correct Stratified by Image and Curriculum
Note: The average percentage correct is shown per ultrasound image for both the postworkshop test, the 6-month follow-up test for those in the ultrasound curriculum (dotted line) and for those without the curriculum (solid line). Those with a statistical significance (P < .05) are denoted by an asterisk (*).
Discussion
A longitudinal ultrasound curriculum, compared to a single workshop stand-alone, improved the ability of PGY-1 residents to correctly identify static ultrasound images at 6 months. We found no difference between the longitudinal curriculum group and the control group in the assessment of the thyroid, internal jugular vein, and inferior vena cava. One explanation for this finding may be that prior ultrasound training focused on the abdomen or lung, and as a result, exposure to the thyroid and internal jugular vein was limited. Another explanation may be the inherent degree of difficulty in identifying certain structures using ultrasound. A study evaluating medical students' ability to identify selected anatomic structures with ultrasound showed significant variance in skills, depending on the anatomic structure.15
While resident perceptions of the ultrasound curriculum were not measured, multiple learners provided unsolicited, positive feedback. Resources included equipment and faculty time. The cost of the equipment depends on machine configuration. Our equipment contains 3 probes, which enables higher and lower frequency range scanning, and costs approximately $30,000 (Sonosite M-Turbo). The IM residency supported faculty time, which consisted of 2 afternoons per month.
To our knowledge, this is the first study to measure the feasibility and impact of a longitudinal ultrasound curriculum on resident ultrasound knowledge and skills. Strengths include the objective assessment of the ability to identify ultrasound images with a previously published pre-post examination, a good response rate (76%) at follow-up, and a comparison group at the same level of training.
The study has several limitations. It was conducted at a single center, which limits generalizability. Additional ultrasound exposure during the follow-up period was not accounted for, and our sample may not have provided adequate power to detect small, clinically significant differences between groups. Finally, residents' ability to identify a static image in a test situation may not translate to performance at the bedside. Future studies should focus on how a longitudinal ultrasound curriculum may affect IM residents' clinical decision making and patient outcomes.
Conclusion
The addition of a longitudinal ultrasound curriculum for IM residents results in improved knowledge retention. An open-house format allowed residents to attend as their clinical responsibilities permitted. Required resources included ultrasound equipment and faculty time.
Footnotes
Diana J. Kelm, MD, is Instructor in Medicine and a Fellow, Division of Pulmonary Critical Care Medicine, Mayo Clinic, Rochester; John T. Ratelle, MD, is Instructor in Medicine and Senior Associate Consultant, Division of Hospital Internal Medicine, Mayo Clinic, Rochester; Nabeel Azeem, MD, is a Fellow, Division of Gastroenterology and Hepatology, University of California, San Francisco; Sara L. Bonnes, MD, is Instructor in Medicine and Senior Associate Consultant, Division of General Internal Medicine, Mayo Clinic, Rochester; Andrew J. Halvorsen, MS, is Project & Data Manager, Internal Medicine Residency Office of Educational Innovations, Department of Internal Medicine, Mayo Clinic, Rochester; Amy S. Oxentenko, MD, is Associate Professor of Medicine, Program Director, and Associate Chair, Department of Medicine, and Consultant, Division of Gastroenterology and Hepatology, Mayo Clinic, Rochester; and Anjali Bhagra, MBBS, is Associate Professor of Medicine and Consultant, Division of General Internal Medicine, Mayo Clinic, Rochester.
Funding: The authors report no external funding source for this study.
Conflict of interest: The authors declare they have no competing interests.
References
- 1.Schnobrich DJ, Gladding S, Olson AP, Duran-Nelson A. Point-of-care ultrasound in internal medicine: a national survey of educational leadership. J Grad Med Educ. 2013;5(3):498–502. doi: 10.4300/JGME-D-12-00215.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Duncan DR, Morgenthaler TI, Ryu JH, Daniels CE. Reducing iatrogenic risk in thoracentesis: establishing best practice via experiential training in a zero-risk environment. Chest. 2009;135(5):1315–1320. doi: 10.1378/chest.08-1227. [DOI] [PubMed] [Google Scholar]
- 3.Wrightson JM, Fysh E, Maskell NA, Lee YC. Risk reduction in pleural procedures: sonography, simulation and supervision. Curr Opin Pulm Med. 2010;16(4):340–350. doi: 10.1097/MCP.0b013e32833a233b. [DOI] [PubMed] [Google Scholar]
- 4.Panoulas VF, Daigeler AL, Malaweera AS, Lota AS, Baskaran D, Rahman S, et al. Pocket-size hand-held cardiac ultrasound as an adjunct to clinical examination in the hands of medical students and junior doctors. Eur Heart J Cardiovasc Imaging. 2013;14(4):323–330. doi: 10.1093/ehjci/jes140. [DOI] [PubMed] [Google Scholar]
- 5.Mouratev G, Howe D, Hoppmann R, Poston MB, Reid R, Varnadoe J, et al. Teaching medical students ultrasound to measure liver size: comparison with experienced clinicians using physical examination alone. Teach Learn Med. 2013;25(1):84–88. doi: 10.1080/10401334.2012.741535. [DOI] [PubMed] [Google Scholar]
- 6.Mjolstad OC, Dalen H, Graven T, Kleinau JO, Salvesen O, Haugen BO. Routinely adding ultrasound examinations by pocket-sized ultrasound devices improves inpatient diagnostics in a medical department. Eur J Intern Med. 2012;23(2):185–191. doi: 10.1016/j.ejim.2011.10.009. [DOI] [PubMed] [Google Scholar]
- 7.Keddis MT, Cullen MW, Reed DA, Halvorsen AJ, McDonald FS, Takahashi PY, et al. Effectiveness of an ultrasound training module for internal medicine residents. BMC Med Educ. 2011;11:75. doi: 10.1186/1472-6920-11-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dulohery MM, Stoven S, Kurklinsky AK, Halvorsen A, McDonald FS, Bhagra A. Ultrasound for internal medicine physicians: the future of the physical examination. J Ultrasound Med. 2014;33(6):1005–1011. doi: 10.7863/ultra.33.6.1005. [DOI] [PubMed] [Google Scholar]
- 9.Tanzola RC, Walsh S, Hopman WM, Sydor D, Arellano R, Allard RV. Brief report—focused transthoracic echocardiography training in a cohort of Canadian anesthesiology residents: a pilot study. Can J Anaesth. 2013;60(1):32–37. doi: 10.1007/s12630-012-9811-8. [DOI] [PubMed] [Google Scholar]
- 10.Singhal R, Dheerendra SK, Charalambous CP, Waseem M. Teaching basic shoulder ultrasonography to orthopaedic postgraduate trainees—effectiveness of a training workshop. Med Ultrason. 2012;14(2):120–124. [PubMed] [Google Scholar]
- 11.Jacoby J, Cesta M, Axelband J, Melanson S, Heller M, Reed J. Can emergency medicine residents detect acute deep venous thrombosis with a limited, two-site ultrasound examination? J Emerg Med. 2007;32(2):197–200. doi: 10.1016/j.jemermed.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 12.Wittich CM, Montgomery SC, Neben MA, Palmer BA, Callahan MJ, Seward JB, et al. Teaching cardiovascular anatomy to medical students by using a handheld ultrasound device. JAMA. 2002;288(9):1062–1063. doi: 10.1001/jama.288.9.1062. [DOI] [PubMed] [Google Scholar]
- 13.Laack TA, Dong Y, Goyal DG, Sadosty AT, Suri HS, Dunn WF. Short-term and long-term impact of the central line workshop on resident clinical performance during simulated central line placement. Simul Healthc. 2014;9(4):228–233. doi: 10.1097/SIH.0000000000000015. [DOI] [PubMed] [Google Scholar]
- 14.Barsuk JH, Cohen ER, McGaghie WC, Wayne DB. Long-term retention of central venous catheter insertion skills after simulation-based mastery learning. Acad Med. 2010;85(suppl 10):9–12. doi: 10.1097/ACM.0b013e3181ed436c. [DOI] [PubMed] [Google Scholar]
- 15.Afonso N, Amponsah D, Yang J, Mendez J, Bridge P, Hays G, et al. Adding new tools to the black bag—introduction of ultrasound into the physical diagnosis course. J Gen Intern Med. 2010;25(11):1248–1252. doi: 10.1007/s11606-010-1451-5. [DOI] [PMC free article] [PubMed] [Google Scholar]


