Abstract
Background
Internal medicine (IM) residents participate in cardiopulmonary resuscitation events (or “codes”), stressful events that involve the death or near death of patients. Experiencing traumatic stress can lead to posttraumatic stress disorder (PTSD).
Objective
We examined whether IM residents who participate in codes developed PTSD symptoms.
Methods
We conducted this research as a 2-phase, mixed methods study. In the first phase, we analyzed interview transcripts from 25 IM residents at 9 institutions for content relevant to PTSD. In the second phase, we surveyed 82 IM residents at 1 midwestern institution for symptoms reported post-code that are associated with PTSD (post-code PTSD symptoms).
Results
A total of 7 of 25 residents (28%) interviewed characterized codes as traumatic or described experiencing PTSD symptoms, including intrusive thoughts about the code, avoidance and emotional numbing, and hyperarousal, irritability, or hypervigilance. Of the 82 residents, 51 (62%) responded to the questionnaire. Of the 42 respondents who had participated in a code, 6 (14%) reported at least 1 PTSD symptom, and 3 (7%) women screened positive for potential PTSD with 2 or more PTSD symptoms. Endorsing any PTSD symptom was associated with residents' perception that code participation negatively affected their work performance.
Conclusions
Our study found that some IM residents reported symptoms of PTSD after being involved in a code.
Introduction
Internal medicine (IM) residents participate in and lead cardiopulmonary resuscitation events or “codes,” which are unpredictable, stressful events that involve the death or near death of patients.1–3 Experiencing traumatic situations can cause posttraumatic stress disorder (PTSD),4 and prior studies have linked physicians' experiences in some settings to elevated PTSD rates.5–11 Physicians with PTSD symptoms may experience anxiety, depression, and burnout.6 Exposure to medical trauma has also been associated with decreased job performance and quality of life.6,12 This is the first study, to our knowledge, to explore the occurrence of PTSD symptoms in IM residents after code participation (post-code PTSD symptoms).
Methods
This study used a mixed methods design. Phase 1 was a qualitative analysis of interview text from IM residents from 9 institutions. In phase 2, we administered a questionnaire to IM residents at a single site. The University of Wisconsin Health Sciences Institutional Review Board approved all facets of this study.
Phase 1: Qualitative Thematic Analysis of Interview Data
We interviewed 25 IM residents from 9 programs about their experiences leading codes.13 Participant recruitment, data collection, and initial analytic plan have previously been reported.13 “Codes as trauma” emerged as a content area, but was not further explored in the original study. For the present study, 2 researchers (C.K., M.B.) reanalyzed the text to identify remarks that described codes as trauma, referenced symptoms in 1 of the 3 symptom clusters of PTSD,14 or described factors that mitigated or aggravated post-code stress. Consensus was reached in classifying segments of text through repeated discussions. Dual analysis of 5 transcripts indicated ≥ 97% interrater agreement (Cohen κ coefficient = 0.647).15 Qualitative software (NVivo 10, QSR International Inc) was used for the analysis.
Phase 2: Quantitative Questionnaire
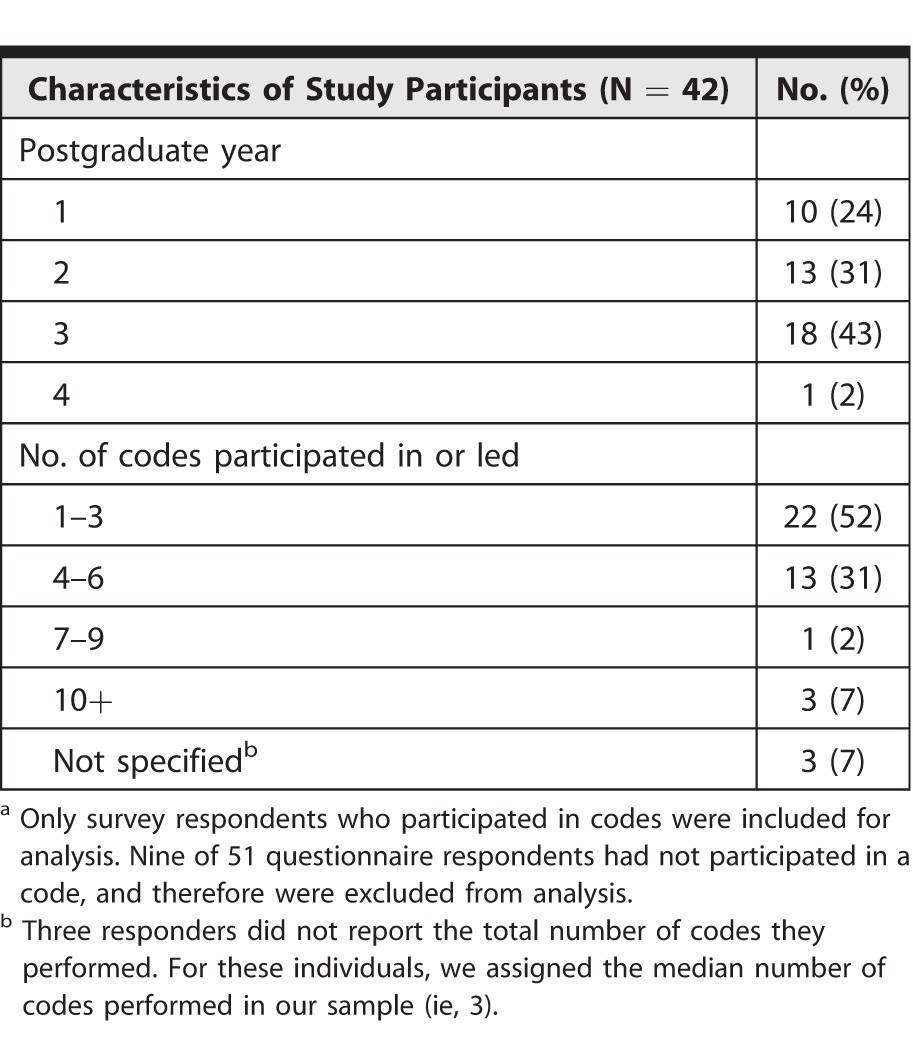
In October 2013, we invited all IM residents at the University of Wisconsin Hospitals and Clinics to participate in an anonymous, online survey. Participation was voluntary. Of 82 eligible residents, 51 (68% of female residents and 58% of male residents) completed the 5-item questionnaire, and 42 (19 women, 23 men) reported participation in a code and were included in analysis (table 1). The questionnaire included the 4-item Primary Care PTSD Screen (PC-PTSD),14 with the only modification being a focus on code participation. The questionnaire assessed whether residents had participated in a code during their residency that was so frightening, horrible, or upsetting that in the past month they (1) had nightmares about the code or thought about the code when they did not want to; (2) tried hard not to think about the code or went out of their way to avoid situations that reminded them of the code; (3) were constantly on guard, watchful, or easily startled; or (4) felt numb or detached from others, activities, or their surroundings.14 As recommended for the PC-PTSD,14 endorsing 2 or more symptoms indicated a positive screen for PTSD. Residents responded to a fifth question, which asked if they felt that their past participation in a code had “a negative impact on some aspect(s) of their performance as a resident.” The response used a Likert scale (1, not at all, to 5, extremely).
TABLE 1.
Phase 2 Questionnaire Study Participantsa
We assessed the association between screening positive for PTSD and reporting that code participation negatively impacted work performance through univariate analysis of variance (ANOVA), with PTSD screen as an independent variable, and the impact of code participation scale as a dependent variable. Regression analysis examined the association between the number of PTSD symptoms and the reported impact of code participation. Alpha values were set at α = 0.05 level for tests of significance. All statistical analysis used SPSS Statistics for Windows version 21.0 (IBM Corp).
Results
Phase 1: Qualitative Thematic Analysis of Interview Data
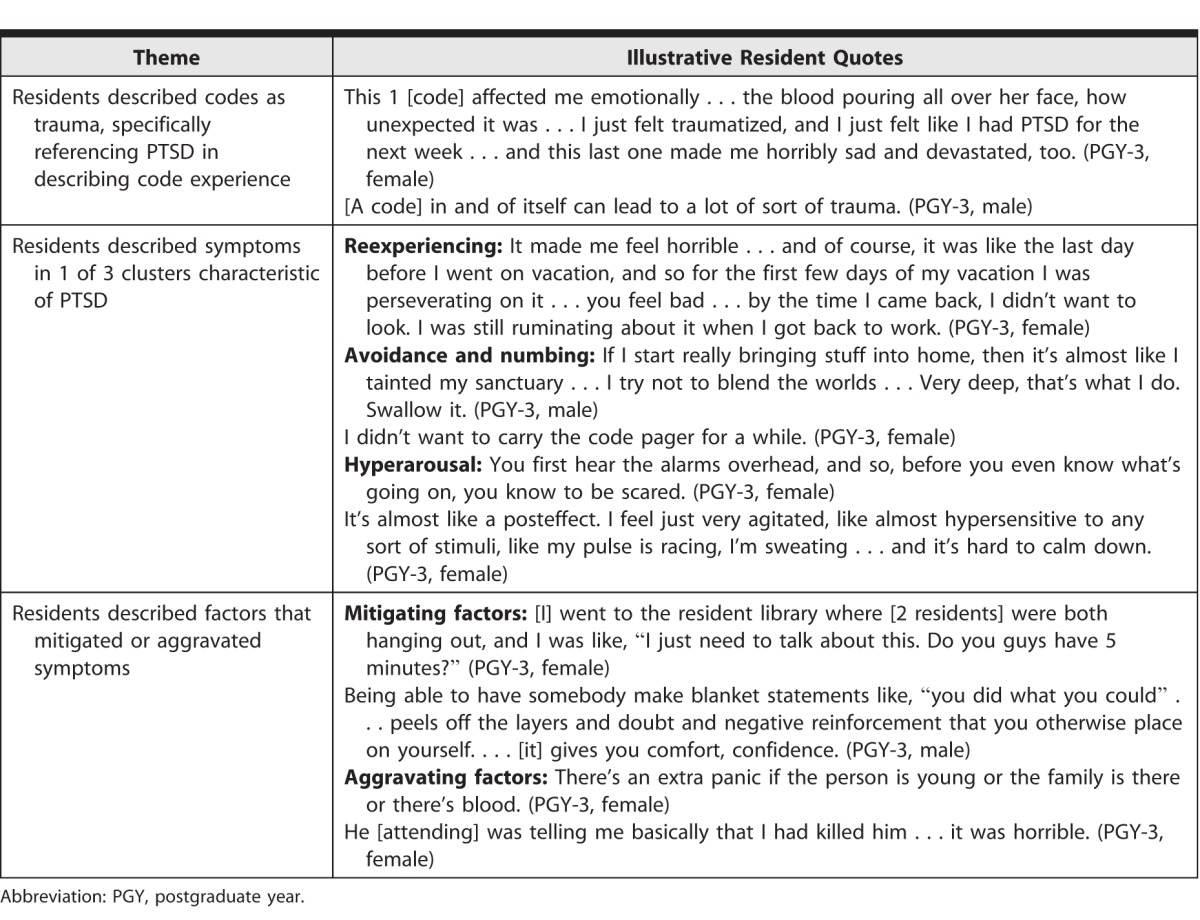
A total of 7 of 25 (28%) residents (all postgraduate year [PGY]-3s, 5 women) characterized codes as traumatic events or described PTSD symptoms. In describing how they dealt with PTSD symptoms, residents described trying to suppress thoughts and images of a code experience. Some also described ways in which supervisors were helpful in reducing or contributing to the trauma of a code. Illustrative text from resident interviews is shown in table 2.
TABLE 2.
Themes Relevant to Posttraumatic Stress Disorder (PTSD) and Code Participation With Illustrative Resident Quotes
Phase 2: Quantitative Questionnaire
The 4-item screening questionnaire showed moderate evidence of reliability with a Cronbach α value of 0.65 (0.70 recommended for scale reliability).16 The majority of the sample (36 of 42, 86%) answered “no” to all 4 scale items. Six of 42 responders (14%) answered “yes” to 1 or more items, and 3 (7%) screened positive for PTSD symptoms by endorsing 2 or more scale items. All were women.
The ANOVA results suggested that residents who screened positive for PTSD reported that code participation had a significantly greater negative impact on their work performance (mean = 2.00, SD = 0) than residents who screened negative for PTSD (mean = 0.26; SD = 0.50; F1,40 = 6.53; P = .02; 95% CI −1.33 to −0.16). Regression analysis showed the number of PTSD symptoms endorsed was significantly associated with the level of negative impact reported (t3.62 = 40; P < .001; R2 = 0.25; 95% CI 0.28–0.98). Residents who endorsed more PTSD symptoms were more likely to indicate that code participation had a negative impact on their work performance.
Discussion
Our study suggests that some IM residents experience PTSD symptoms that may be associated with their participation on codes and that these symptoms may be associated with self-reported negative impact on work performance. Other studies have found that residents involved in medical traumas are susceptible to PTSD symptoms.7–9 Our study is the first, to our knowledge, to have residents describe their experience, attribute symptoms of traumatic stress to code involvement, and report how they dealt with the traumatic stress of code participation. Like earlier studies, this highlighted the benefit of talking with others to mitigate stress,17,18 and the role of attending physicians to mitigate the impact of traumatic code experiences.19–21 Our data suggest some residents use maladaptive coping strategies, such as thought suppression, when experiencing PTSD symptoms. This points to the need for interventions to reduce the traumatic impact of codes for some IM residents.
Despite the low overall prevalence of PTSD and the small sample in our study, we found PTSD symptoms were more often endorsed by women. While female residents may be more willing than male residents to endorse PTSD symptoms on a questionnaire, our results align with reports showing that women are more likely to meet the criteria for PTSD and to report greater increased PTSD than men for a single type of traumatic event.22,23 Previous work suggests the need to enact code leadership in a stereotypically masculine manner may induce additional code-related stress for female residents.13 Simply acknowledging the existence of sex-based assumptions and their potential impact could alleviate this added stress.24
Our findings support the need for IM residency programs to further investigate PTSD symptoms. Training on how to prevent and cope with post-code PTSD symptoms could include
-
•
Acknowledging that participating in codes is traumatic and that experiencing powerful emotions is normal,
-
•
Encouraging faculty to provide supportive statements during and/or after a code to reduce (and never reinforce) residents' feelings of self-blame,
-
•
Affirming that attempts to suppress traumatic thoughts can exacerbate and prolong post-code PTSD symptoms,
-
•
Encouraging access to social support that provides opportunities for discussing code events with peers and supervisors, and
-
•
Other strategies might include providing forums for residents to write about or discuss their experiences.
Our study has several limitations. Qualitative data is valuable in exploring human experience but is not generalizable. The questionnaire relies on self-report, has no established validity evidence in this population, and used a single question to capture the residents' perception of impact on work performance. Our findings also are from a single site, and our response rate was low, introducing the potential for sampling bias.
Conclusion
This mixed methods study found that some IM residents may be at risk for developing symptoms of PTSD that could negatively affect their work performance, and these residents may benefit from prevention and supportive measures during training.
Footnotes
Christine Kolehmainen, MD, MS, is a Physician, William S. Middleton Memorial Veterans Hospital, and Clinical Adjunct Assistant Professor, Department of Medicine, University of Wisconsin School of Medicine and Public Health; Anne Stahr, MS, is Education Program Manager, Advanced Fellowship in Women's Health National HUB, William S. Middleton Memorial Veterans Hospital; Anna Kaatz, PhD, MPH, is Director of Computational Sciences, Center for Women's Health Research, University of Wisconsin; Meghan Brennan, MD, MS, is a Quality Scholar Fellow, William S. Middleton Memorial Veterans Hospital, and Clinical Instructor, Department of Medicine, University of Wisconsin School of Medicine and Public Health; Bennett Vogelman, MD, is Professor of Medicine and Vice Chair for Education, Department of Medicine, University of Wisconsin School of Medicine and Public Health; Jessica Cook, PhD, is Assistant Professor, University of Wisconsin-Madison School of Medicine and Public Health, Investigator, University of Wisconsin-Madison Center for Tobacco Research and Intervention, and Clinical Psychologist, William S. Middleton Memorial Veterans Hospital; and Molly Carnes, MD, MS, is Professor of Medicine, Psychiatry, and Industrial & Systems Engineering, and Director of the Center for Women's Health Research, University of Wisconsin, and Director of Women Veterans Health, William S. Middleton Memorial Veterans Hospital.
Funding: The authors report no external funding source for this study.
Conflict of interest: The authors declare they have no competing interests.
This study was presented as a poster abstract at the Annual Congress of Women's Health in Washington, DC, April 4–6, 2014.
The authors would like to thank the internal medicine residents who took the time to participate in this study, Michelle Kipp at the University of Wisconsin Internal Medicine Residency Program who aided in the questionnaire distribution and data collection, and Carol Isaac for her guidance with qualitative research reporting.
The contents do not represent the views of the Department of Veterans Affairs or the US government.
References
- 1.Fang F, Kemp J, Jawandha A, Juros J, Long L, Nanayakkara S, et al. Encountering patient suicide: a resident's experience. Acad Psychiatry. 2007;31(5):340–344. doi: 10.1176/appi.ap.31.5.340. [DOI] [PubMed] [Google Scholar]
- 2.Heiner JD, Trabulsy ME. Coping with the death of a patient in the emergency department. Ann Emerg Med. 2011;58(3):295–298. doi: 10.1016/j.annemergmed.2010.12.022. [DOI] [PubMed] [Google Scholar]
- 3.Jackson VA, Sullivan AM, Gadmer NM, Seltzer D, Mitchell AM, Lakoma MD, et al. “It was haunting . . .”: physicians' descriptions of emotionally powerful patient deaths. Acad Med. 2005;80(7):648–656. doi: 10.1097/00001888-200507000-00007. [DOI] [PubMed] [Google Scholar]
- 4.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 5.Ben-Ezra M, Palgi Y, Essar N. Impact of war stress on posttraumatic stress symptoms in hospital personnel. Gen Hosp Psychiatry. 2007;29(3):264–266. doi: 10.1016/j.genhosppsych.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 6.Einav S, Shalev AY, Ofek H, Freedman S, Matot I, Weiniger CF. Differences in psychological effects in hospital doctors with and without post-traumatic stress disorder. Br J Psychiatry. 2008;193(2):165–166. doi: 10.1192/bjp.bp.108.051532. [DOI] [PubMed] [Google Scholar]
- 7.Klamen DL, Grossman LS, Kopacz D. Posttraumatic stress disorder symptoms in resident physicians related to their internship. Acad Psychiatry. 1995;19(3):142–149. doi: 10.1007/BF03341425. [DOI] [PubMed] [Google Scholar]
- 8.Mills LD, Mills TJ. Symptoms of post-traumatic stress disorder among emergency medicine residents. J Emerg Med. 2005;28(1):1–4. doi: 10.1016/j.jemermed.2004.05.009. [DOI] [PubMed] [Google Scholar]
- 9.Naghavi SH, Shabestari O, Alcolado J. Post-traumatic stress disorder in trainee doctors with previous needlestick injuries. Occup Med (Lond) 2013;63(4):260–265. doi: 10.1093/occmed/kqt027. [DOI] [PubMed] [Google Scholar]
- 10.Shields J, Erdal K, Skrinjaric J, Majic G. Post-traumatic stress symptomatology among health care professionals in Croatia. Am J Orthopsychiatry. 1999;69(4):529–535. doi: 10.1037/h0080400. [DOI] [PubMed] [Google Scholar]
- 11.Wilberforce N, Wilberforce K, Aubrey-Bassler FK. Post-traumatic stress disorder in physicians from an underserviced area. Fam Pract. 2010;27(3):339–343. doi: 10.1093/fampra/cmq002. [DOI] [PubMed] [Google Scholar]
- 12.Czaja AS, Moss M, Mealer M. Symptoms of posttraumatic stress disorder among pediatric acute care nurses. J Pediatr Nurs. 2012;27(4):357–365. doi: 10.1016/j.pedn.2011.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kolehmainen C, Brennan M, Filut A, Isaac C, Carnes M. Afraid of being “witchy with a ‘b'”: a qualitative study of how gender influences residents' experiences leading cardiopulmonary resuscitation. Acad Med. 2014;89(9):1276–1281. doi: 10.1097/ACM.0000000000000372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Prins A, Ouimette P, Kimerling R, Cameron RP, Hugelschofer DS, Shaw-Hegwer J, et al. The primary care PTSD screen (PC-PTSD): development and operating characteristics. Primary Care Psychiatry. 2003;9(1):9–14. [Google Scholar]
- 15.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. [PubMed] [Google Scholar]
- 16.Streiner DL, Norman GR. Health Measurement Scales: A Practical Guide to Their Development and Use. New York, NY: Oxford University Press; 1989. [Google Scholar]
- 17.Cohen JS, Patten S. Well-being in residency training: a survey examining resident physician satisfaction both within and outside residency training and mental health in Alberta. BMC Med Ed. 2005;5:21. doi: 10.1186/1472-6920-5-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hu YY, Fix ML, Hevelone ND, Lipsitz SR, Greenberg CC, Weissman JS, et al. Physicians' needs in coping with emotional stressors: the case for peer support. Arch Surg. 2012;147(3):212–217. doi: 10.1001/archsurg.2011.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rhodes-Kropf J, Carmody SS, Seltzer D, Redinbaugh E, Gadmer N, Block SD, et al. “This is just too awful; I just can't believe I experienced that . . .”: medical students' reactions to their “most memorable” patient death. Acad Med. 2005;80(7):634–640. doi: 10.1097/00001888-200507000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Goebert D, Thompson D, Takeshita J, Beach C, Bryson P, Ephgrave K, et al. Depressive symptoms in medical students and residents: a multischool study. Acad Med. 2009;84(2):236–241. doi: 10.1097/ACM.0b013e31819391bb. [DOI] [PubMed] [Google Scholar]
- 21.Redinbaugh EM, Sullivan AM, Block SD, Gadmer NM, Lakoma M, Mitchell AM, et al. Doctors' emotional reactions to recent death of a patient: cross sectional study of hospital doctors. BMJ. 2003;327(7408):185. doi: 10.1136/bmj.327.7408.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tolin DF, Foa EB. Sex differences in trauma and posttraumatic stress disorder: a quantitative review of 25 years of research. Psychol Bull. 2006;132(6):959–992. doi: 10.1037/0033-2909.132.6.959. [DOI] [PubMed] [Google Scholar]
- 23.Yehuda R. Post-traumatic stress disorder. N Engl J Med. 2002;346(2):108–114. doi: 10.1056/NEJMra012941. [DOI] [PubMed] [Google Scholar]
- 24.Carnes M. Commentary: deconstructing gender difference. Acad Med. 2010;85(4):575–577. doi: 10.1097/ACM.0b013e3181d983de. [DOI] [PubMed] [Google Scholar]


