Abstract
Background
Out-of-hospital cardiac arrest (OHCA) remains a major public health issue and research has shown that large regional variation in outcomes exists. Of the interventions associated with survival, the provision of bystander CPR is one of the most important modifiable factors. The aim of this study is to identify census areas with high incidence of OHCA and low rates of bystander CPR in Victoria, Australia
Methods
We conducted an observational study using prospectively collected population-based OHCA data from the state of Victoria in Australia. Using ArcGIS (ArcMap 10.0), we linked the location of the arrest using the dispatch coordinates (longitude and latitude) to Victorian Local Government Areas (LGAs). We used Bayesian hierarchical models with random effects on each LGA to provide shrunken estimates of the rates of bystander CPR and the incidence rates.
Results
Over the study period there were 31,019 adult OHCA attended, of which 21,436 (69.1%) cases were of presumed cardiac etiology. Significant variation in the incidence of OHCA among LGAs was observed. There was a 3 fold difference in the incidence rate between the lowest and highest LGAs, ranging from 38.5 to 115.1 cases per 100,000 person-years. The overall rate of bystander CPR for bystander witnessed OHCAs was 62.4%, with the rate increasing from 56.4% in 2008–2010 to 68.6% in 2010–2013. There was a 25.1% absolute difference in bystander CPR rates between the highest and lowest LGAs.
Conclusion
Significant regional variation in OHCA incidence and bystander CPR rates exists throughout Victoria. Regions with high incidence and low bystander CPR participation can be identified and would make suitable targets for interventions to improve CPR participation rates.
Introduction
Out-of-hospital cardiac arrest (OHCA) remains a major public health issue [1]. The high case fatality rate of OHCA (>90%) in most communities[2,3], indicates the importance of developing appropriate interventional strategies [4].
Efforts to improve out-of-hospital cardiac arrest outcomes focus on improving the chain of survival [5,6]. This includes early recognition of cardiac arrest symptoms, early CPR, early defibrillation and early advanced post-resuscitation care [7]. Of the interventions associated with survival, the provision of bystander CPR is one of the most important modifiable factors[8–14]. Improvements in bystander CPR rates through system changes, such as simplification of CPR instructions in the emergency call, have been reported[15]. However, whole-of-community interventions have shown mixed results[16], suggesting that such interventions might be better placed in communities with a high incidence of OHCA and a low prevalence of bystander CPR.
Research in the US has shown that these ‘high-risk’ census tracts can be identified by geocoding OHCA registry data[17,18]. However, it is unknown if such high-risk areas exist in the Australian community and whether these communities remain at constant high-risk over time. Therefore, the aim of this study is to identify census areas with high incidence of OHCA and low rates of bystander CPR in Victoria, Australia. In addition, this study aims to evaluate changes in these measures over time.
Methods
Study Design and Setting
We conducted an observational study using prospectively collected population-based OHCA data from the state of Victoria in Australia. Victoria has a current population of 5.6 million, 75% of whom reside in the metropolitan region of Melbourne. Ambulance Victoria (AV) is the sole provider of Emergency Medical Services (EMS) in the state. AV delivers a two-tiered EMS system, with Advanced Life Support Paramedics and Intensive Care Ambulance Paramedics. Fire fighters and volunteer Community Emergency Response Teams provide a first response in select areas of Victoria.
The Victorian Ambulance Cardiac Arrest Registry (VACAR)
AV maintains the Victorian Ambulance Cardiac Arrest Registry (VACAR), which registers and collects EMS clinical and outcome data for all OHCA attended by EMS in the state of Victoria[19]. Data collection is standardized using the Utstein definitions[20]. The Victorian Department of Health Human Research Ethics Committee (HREC) has approved VACAR (No. 08/02) data collection. Ethics approval for the current study was received from the Monash University Human Research Ethics Committee (CF12/3410–2012001638).
Inclusion and Exclusion Criteria
The VACAR was searched and data was extracted for OHCA cases occurring between January 2008 and December 2013. To match with available population data, cases were included if they were aged greater than 20 years and the arrest was presumed to be of cardiac etiology based on EMS documentation (i.e. no other obvious cause recorded such as trauma, hanging, drowning, etc.).
Local Government Areas (LGAs) and Geospatial Mapping
Australia has a federal system of government under which state governments preside in each of the eight states and territories. Beneath this are local governments, for which there are 79 local government areas (LGAs) in the state of Victoria.
Using ArcGIS (ArcMap 10.0), we linked the location of the arrest using the dispatch coordinates (longitude and latitude) to Victorian LGAs.
Statistical Analysis
We restricted the calculation of bystander CPR rates to those arrests that were witnessed by a bystander (not a paramedic). We coded cases in which the patient received bystander chest compressions, even if ‘stated as inadequate or poor’, as having received bystander CPR. We defined the absence of bystander CPR as those cases that received no bystander chest compressions, or who received ventilation only. We excluded cases that were coded as ‘unknown’ or ‘not stated’ from estimates of bystander CPR rates (259, 4.1%).
We calculated the incidence of OHCA in Victorian LGAs using yearly population data from the Australian Bureau of Statistics, and bystander CPR rates for each LGA[21]. We used Bayesian hierarchical models with random effects on each LGA to provide shrunken estimates of the rates of bystander CPR and the incidence rates. We adjusted for relative socio-economic advantage and disadvantage using the 2011 Socio-Economic Indexes for Areas, ‘SEIFA index’, for each LGA[22]. The rates were modelled using a mixed-effects logit model for bystander CPR and a mixed-effects Poisson model for the OHCA incidence rate, where the random effect was assumed to be normally distributed with a mean of zero. These models estimate the ‘shrunken’ LGA rate as a weighted average of the pooled estimate (adjusted by SEIFA index) and the LGA-specific estimate [23]. The weights that contribute to this average are the inverse variances of the pooled estimate and the LGA-specific estimate. Thus an LGA with considerably fewer OHCA events will shrink toward the pooled estimate more than an LGA with many observed events. In this way, those LGAs with very few events are shrunken considerably toward the pooled estimate (or adjusted mean) regardless of their observed rates.
We considered two time periods to examine changes over time, 2008–2010 versus 2011–2013. These time periods also correspond with the introduction of the 2010 ILCOR guidelines. We plotted the shrunken estimates of the rates of bystander CPR and the incidence of OHCA in each LGA.
Results
Over the study period there were 31,019 adult OHCA attended, of which 21,436 (69.1%) cases were of presumed cardiac etiology. For those cases of presumed cardiac etiology, the overall incidence of OHCA was 64.6 cases per 100,000 person-years. The crude incidence declined from 66.6 cases per 100,000 person-years in 2008–2010 to 62.6 cases per 100,000 person-years in 2011–2013 (p<0.001).
The overall rate of bystander CPR for bystander witnessed OHCAs was 62.4%, with the rate increasing from 56.4% in 2008–2010 to 68.6% in 2010–2013.
Regional OHCA Incidence
Among LGAs, the median crude annual incidence rate of OHCA was 71.3 cases per 100,000 person-years (IQR: 58.5–79.0).
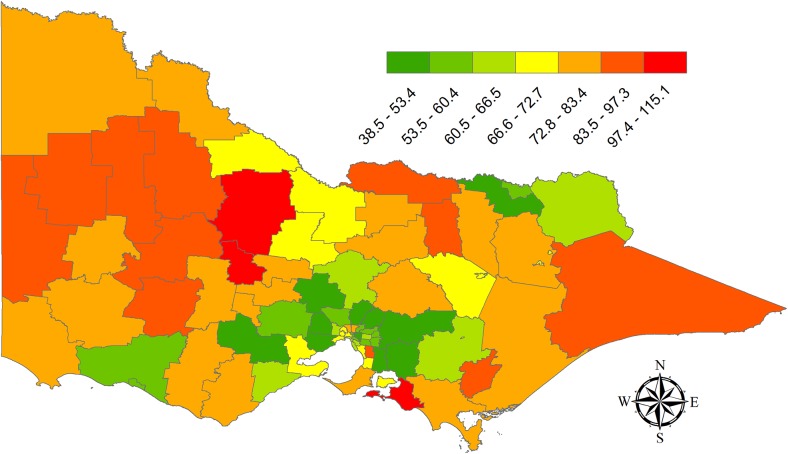
The map shown in Fig 1 provides the shrunken estimate of the incidence in each LGA. Significant variation among LGAs was observed with a 3 fold difference in the incidence rate between the lowest and highest LGAs. The highest incidence rates were seen in two neighboring rural LGAs (Central Goldfields LGA = 115.1 cases per 100,000 person-years; Loddon LGA = 110.6 cases per 100,000 person-years). The lowest incidence rates were generally in outer suburban areas surrounding Melbourne, with the lowest incidence rate found in the North-East of Melbourne in the Shire of Nillumbik (38.5 cases per 100,000 person-years).
Fig 1. Shrunken estimate of OHCA incidence rate (per 100,000 person years) for Victorian Local Government Areas 2008–2013.
Regional Bystander CPR
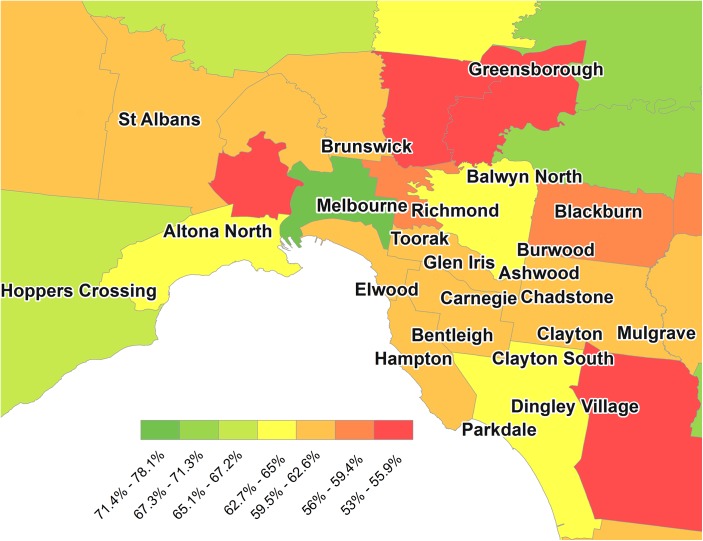
The median estimate of bystander CPR among LGAs was 63.2% (IQR: 60.5%-65.7%) over the entire study period. Fig 2 provides a map of Melbourne City and surrounding local government areas. Even across the metropolitan regions, large disparities in the rate of bystander CPR can be seen. There was a 25.1% absolute difference in bystander CPR rates between the highest and lowest LGAs. The highest rate of bystander CPR was in Melbourne city with a rate of 78.1%. In contrast the rate of bystander CPR was lowest in Greater Dandenong, South-East of Melbourne with a rate of 53.0%.
Fig 2. Prevalence of Bystander CPR in Melbourne and surrounding areas, 2008–2013 by Victorian Local Government Area.
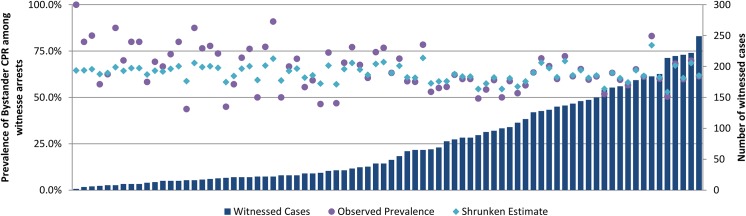
Fig 3 provides the observed OHCA events, the crude rate of bystander CPR and the shrunken estimate in each LGA during the study period. While crude rates varied from 43.8% to 100%, these were in LGAs with a very small number of OHCA events.
Fig 3. Bystander witnessed OHCA cases by Victorian Local Government Area with the Observed Prevalence and shrunken estimate of Bystander CPR among witnessed arrests, 2008–2013.
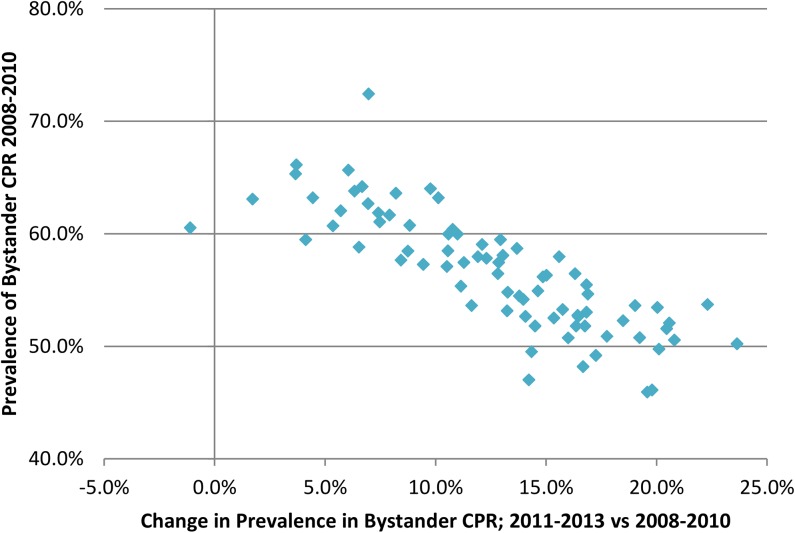
In all but one LGA the rates of bystander CPR improved during the study period. Fig 4 shows the change in the estimated rate from 2008–2010 to 2011–2013. The largest improvements in bystander CPR occurred in the LGAs with the lowest rates in 2008–2010. (p<0.001)
Fig 4. Prevalence of Bystander CPR in 2008–2010, and change between 2008–2010 and 2011–2013 by Victorian Local Government Area.
Fig 5 shows the incidence of OHCA against the prevalence of bystander CPR for the period 2011–2013 in each LGA. The lower right quadrant indicates those regions with an incidence rate higher than the median with bystander CPR rates that are lower than the median.
Fig 5. Incidence of OHCA and the prevalence of Bystander CPR 2011–2013 by Victorian Local Government Area.
Tables 1 and 2 provide a complete list of the incidence (Table 1) and bystander CPR rates (Table 2) for each LGA for the entire period, as well as split into the first half and second half of the study period.
Table 1. Shrunken estimate of Out-of Hospital Cardiac Arrest incidence rate by Victorian Local Government Area, 2008–2013.
| Incidence Rate (shrunken estimate per 100,000 person years) | 2013 Population over 20 years | ||||
|---|---|---|---|---|---|
| LGA Name | LGA Code | 2008–2010 | 2010–2013 | 2008–2013 | |
| Alpine (S) | 20110 | 80.4 | 75.5 | 80.3 | 12 044 |
| Ararat (RC) | 20260 | 82.3 | 101.2 | 97.3 | 11 207 |
| Ballarat (C) | 20570 | 85.2 | 67.9 | 76.6 | 98 684 |
| Banyule (C) | 20660 | 56.7 | 63.4 | 60.2 | 124 475 |
| Bass Coast (S) | 20740 | 103.9 | 97.3 | 105.5 | 31 010 |
| Baw Baw (S) | 20830 | 64.1 | 62.9 | 62.5 | 45 205 |
| Bayside (C) | 20910 | 65.1 | 55.2 | 61.1 | 98 368 |
| Benalla (RC) | 21010 | 92.5 | 79.1 | 88.5 | 13 719 |
| Boroondara (C) | 21110 | 56.2 | 48.6 | 52.6 | 170 553 |
| Brimbank (C) | 21180 | 71.2 | 63.0 | 66.5 | 195 469 |
| Buloke (S) | 21270 | 82.4 | 85.1 | 88.5 | 6 221 |
| Campaspe (S) | 21370 | 77.9 | 67.3 | 71.8 | 36 919 |
| Cardinia (S) | 21450 | 47.5 | 57.9 | 51.7 | 84 065 |
| Casey (C) | 21610 | 49.1 | 45.7 | 46.6 | 275 116 |
| Central Goldfields (S) | 21670 | 111.1 | 106.7 | 115.1 | 12 602 |
| Colac-Otway (S) | 21750 | 69.9 | 82.3 | 76.1 | 20 694 |
| Corangamite (S) | 21830 | 70.4 | 76.9 | 74.4 | 16 137 |
| Darebin (C) | 21890 | 80.4 | 70.1 | 75.5 | 146 797 |
| East Gippsland (S) | 22110 | 92.3 | 85.2 | 90.3 | 43 413 |
| Frankston (C) | 22170 | 74.2 | 68.4 | 71.4 | 133 560 |
| Gannawarra (S) | 22250 | 67.0 | 81.1 | 72.7 | 10 326 |
| Glen Eira (C) | 22310 | 67.2 | 54.4 | 61.1 | 141 519 |
| Glenelg (S) | 22410 | 74.4 | 82.0 | 78.6 | 19 521 |
| Golden Plains (S) | 22490 | 57.3 | 54.3 | 52.9 | 20 151 |
| Greater Bendigo (C) | 22620 | 71.9 | 69.1 | 70.4 | 105 332 |
| Greater Dandenong (C) | 22670 | 87.9 | 84.5 | 86.2 | 146 727 |
| Greater Geelong (C) | 22750 | 68.6 | 70.6 | 69.6 | 221 515 |
| Greater Shepparton (C) | 22830 | 75.8 | 75.3 | 75.4 | 62 784 |
| Hepburn (S) | 22910 | 68.0 | 79.2 | 74.4 | 14 843 |
| Hindmarsh (S) | 22980 | 83.7 | 95.4 | 95.3 | 5 695 |
| Hobsons Bay (C) | 23110 | 77.5 | 66.4 | 72.3 | 89 111 |
| Horsham (RC) | 23190 | 78.0 | 69.9 | 74.4 | 19 687 |
| Hume (C) | 23270 | 64.7 | 57.2 | 60.1 | 183 263 |
| Indigo (S) | 23350 | 55.1 | 58.2 | 53.2 | 15 372 |
| Kingston (C) | 23430 | 72.0 | 65.0 | 68.9 | 151 686 |
| Knox (C) | 23670 | 51.7 | 59.1 | 55.2 | 154 909 |
| Latrobe (C) | 23810 | 88.2 | 94.0 | 92.1 | 73 846 |
| Loddon (S) | 23940 | 98.4 | 102.8 | 110.6 | 7 443 |
| Macedon Ranges (S) | 24130 | 48.9 | 58.2 | 52.9 | 44 098 |
| Manningham (C) | 24210 | 55.8 | 52.1 | 54.0 | 117 537 |
| Mansfield (S) | 24250 | 76.2 | 65.7 | 72.0 | 8 185 |
| Maribyrnong (C) | 24330 | 71.5 | 70.1 | 71.0 | 79 302 |
| Maroondah (C) | 24410 | 59.9 | 55.0 | 57.1 | 109 575 |
| Melbourne (C) | 24600 | 77.7 | 60.7 | 69.5 | 116 447 |
| Melton (S) | 24650 | 46.6 | 48.9 | 46.2 | 122 909 |
| Mildura (RC) | 24780 | 70.6 | 83.1 | 76.4 | 52 685 |
| Mitchell (S) | 24850 | 61.0 | 64.5 | 61.5 | 37 366 |
| Moira (S) | 24900 | 92.7 | 89.0 | 93.2 | 28 675 |
| Monash (C) | 24970 | 58.6 | 55.5 | 57.0 | 182 485 |
| Moonee Valley (C) | 25060 | 74.5 | 64.8 | 70.2 | 115 097 |
| Moorabool (S) | 25150 | 67.4 | 56.7 | 60.4 | 30 320 |
| Moreland (C) | 25250 | 78.6 | 69.2 | 74.1 | 160 029 |
| Mornington Peninsula (S) | 25340 | 76.7 | 74.1 | 76.0 | 152 260 |
| Mount Alexander (S) | 25430 | 76.9 | 75.4 | 77.5 | 17 994 |
| Moyne (S) | 25490 | 63.3 | 57.8 | 58.7 | 16 277 |
| Murrindindi (S) | 25620 | 72.8 | 75.1 | 75.8 | 13 494 |
| Nillumbik (S) | 25710 | 39.8 | 40.5 | 38.5 | 62 724 |
| Northern Grampians (S) | 25810 | 80.6 | 103.4 | 96.4 | 11 799 |
| Port Phillip (C) | 25900 | 65.9 | 57.5 | 62.3 | 102 501 |
| Pyrenees (S) | 25990 | 67.5 | 90.6 | 78.9 | 6 770 |
| Queenscliffe (B) | 26080 | 69.5 | 66.2 | 76.0 | 3 058 |
| South Gippsland (S) | 26170 | 77.4 | 71.2 | 75.2 | 27 930 |
| Southern Grampians (S) | 26260 | 76.1 | 76.9 | 78.6 | 16 145 |
| Stonnington (C) | 26350 | 61.9 | 51.1 | 56.9 | 103 187 |
| Strathbogie (S) | 26430 | 75.8 | 85.0 | 83.4 | 9 706 |
| Surf Coast (S) | 26490 | 59.8 | 60.7 | 61.5 | 28 282 |
| Swan Hill (RC) | 26610 | 73.6 | 76.2 | 74.1 | 20 867 |
| Towong (S) | 26670 | 65.1 | 69.0 | 66.0 | 5 889 |
| Unincorporated Vic | 29399 | 66.0 | 64.7 | 67.8 | 758 |
| Wangaratta (RC) | 26700 | 79.0 | 72.0 | 76.0 | 27 197 |
| Warrnambool (C) | 26730 | 57.1 | 62.9 | 57.7 | 33 300 |
| Wellington (S) | 26810 | 77.7 | 73.2 | 75.7 | 42 319 |
| West Wimmera (S) | 26890 | 79.0 | 78.8 | 85.0 | 4 089 |
| Whitehorse (C) | 26980 | 69.6 | 61.0 | 65.7 | 161 724 |
| Whittlesea (C) | 27070 | 54.6 | 51.1 | 51.8 | 179 261 |
| Wodonga (RC) | 27170 | 64.4 | 59.8 | 59.9 | 37 345 |
| Wyndham (C) | 27260 | 48.0 | 45.2 | 45.4 | 189 618 |
| Yarra (C) | 27350 | 61.2 | 56.9 | 58.9 | 83 593 |
| Yarra Ranges (S) | 27450 | 54.9 | 53.0 | 53.4 | 149 538 |
| Yarriambiack (S) | 27630 | 80.9 | 85.1 | 86.2 | 7 018 |
Cities (C), Rural Cities (RC), Boroughs (B) and Shires (S)
Table 2. Shrunken estimate of bystander CPR rate by Victorian Local Government Area, 2008–2013.
| Bystander CPR (Shrunken proportion of bystander witnessed arrests due to presumed cardiac aetiology) | 2013 Population over 20 years | ||||
|---|---|---|---|---|---|
| LGA Name | LGA Code | 2008–2010 | 2010–2013 | 2008–2013 | |
| Alpine (S) | 20110 | 60.0% | 70.5% | 65.9% | 12 044 |
| Ararat (RC) | 20260 | 61.7% | 69.6% | 66.4% | 11 207 |
| Ballarat (C) | 20570 | 52.7% | 69.1% | 60.4% | 98 684 |
| Banyule (C) | 20660 | 46.1% | 65.9% | 55.9% | 124 475 |
| Bass Coast (S) | 20740 | 52.7% | 69.2% | 60.6% | 31 010 |
| Baw Baw (S) | 20830 | 65.3% | 69.0% | 68.1% | 45 205 |
| Bayside (C) | 20910 | 57.3% | 66.7% | 61.3% | 98 368 |
| Benalla (RC) | 21010 | 53.0% | 69.9% | 61.6% | 13 719 |
| Boroondara (C) | 21110 | 62.1% | 67.8% | 64.7% | 170 553 |
| Brimbank (C) | 21180 | 54.2% | 68.1% | 60.5% | 195 469 |
| Buloke (S) | 21270 | 56.3% | 71.3% | 65.8% | 6 221 |
| Campaspe (S) | 21370 | 51.6% | 72.0% | 62.1% | 36 919 |
| Cardinia (S) | 21450 | 64.0% | 73.8% | 71.3% | 84 065 |
| Casey (C) | 21610 | 66.1% | 69.8% | 68.5% | 275 116 |
| Central Goldfields (S) | 21670 | 49.8% | 69.9% | 59.2% | 12 602 |
| Colac-Otway (S) | 21750 | 63.2% | 67.6% | 65.6% | 20 694 |
| Corangamite (S) | 21830 | 60.4% | 71.2% | 67.2% | 16 137 |
| Darebin (C) | 21890 | 49.5% | 63.9% | 54.7% | 146 797 |
| East Gippsland (S) | 22110 | 53.2% | 66.4% | 58.8% | 43 413 |
| Frankston (C) | 22170 | 54.9% | 69.5% | 61.9% | 133 560 |
| Gannawarra (S) | 22250 | 58.1% | 71.1% | 65.8% | 10 326 |
| Glen Eira (C) | 22310 | 59.5% | 63.6% | 60.6% | 141 519 |
| Glenelg (S) | 22410 | 58.0% | 69.9% | 64.3% | 19 521 |
| Golden Plains (S) | 22490 | 50.8% | 70.0% | 59.4% | 20 151 |
| Greater Bendigo (C) | 22620 | 51.8% | 68.6% | 58.7% | 105 332 |
| Greater Dandenong (C) | 22670 | 47.0% | 61.2% | 53.0% | 146 727 |
| Greater Geelong (C) | 22750 | 50.2% | 73.9% | 61.8% | 221 515 |
| Greater Shepparton (C) | 22830 | 52.7% | 66.7% | 58.7% | 62 784 |
| Hepburn (S) | 22910 | 52.1% | 72.6% | 64.0% | 14 843 |
| Hindmarsh (S) | 22980 | 58.5% | 69.0% | 64.4% | 5 695 |
| Hobsons Bay (C) | 23110 | 63.1% | 64.8% | 63.4% | 89 111 |
| Horsham (RC) | 23190 | 51.8% | 68.2% | 58.3% | 19 687 |
| Hume (C) | 23270 | 63.8% | 70.1% | 67.2% | 183 263 |
| Indigo (S) | 23350 | 57.4% | 68.7% | 63.2% | 15 372 |
| Kingston (C) | 23430 | 61.1% | 68.5% | 64.7% | 151 686 |
| Knox (C) | 23670 | 58.8% | 65.3% | 61.8% | 154 909 |
| Latrobe (C) | 23810 | 48.2% | 64.9% | 54.6% | 73 846 |
| Loddon (S) | 23940 | 55.5% | 72.3% | 65.4% | 7 443 |
| Macedon Ranges (S) | 24130 | 58.0% | 73.5% | 68.6% | 44 098 |
| Manningham (C) | 24210 | 63.6% | 71.8% | 68.7% | 117 537 |
| Mansfield (S) | 24250 | 56.4% | 69.3% | 62.4% | 8 185 |
| Maribyrnong (C) | 24330 | 45.9% | 65.5% | 54.6% | 79 302 |
| Maroondah (C) | 24410 | 49.2% | 66.4% | 57.5% | 109 575 |
| Melbourne (C) | 24600 | 72.4% | 79.4% | 78.1% | 116 447 |
| Melton (S) | 24650 | 57.1% | 67.6% | 62.6% | 122 909 |
| Mildura (RC) | 24780 | 50.5% | 71.4% | 60.8% | 52 685 |
| Mitchell (S) | 24850 | 51.8% | 66.3% | 57.5% | 37 366 |
| Moira (S) | 24900 | 53.6% | 72.7% | 63.3% | 28 675 |
| Monash (C) | 24970 | 55.3% | 66.5% | 60.4% | 182 485 |
| Moonee Valley (C) | 25060 | 53.3% | 69.0% | 60.9% | 115 097 |
| Moorabool (S) | 25150 | 62.7% | 69.6% | 67.2% | 30 320 |
| Moreland (C) | 25250 | 52.3% | 70.8% | 61.7% | 160 029 |
| Mornington Peninsula (S) | 25340 | 52.5% | 67.9% | 60.8% | 152 260 |
| Mount Alexander (S) | 25430 | 50.9% | 68.6% | 58.8% | 17 994 |
| Moyne (S) | 25490 | 60.0% | 70.9% | 66.8% | 16 277 |
| Murrindindi (S) | 25620 | 60.8% | 69.6% | 65.5% | 13 494 |
| Nillumbik (S) | 25710 | 64.2% | 70.9% | 69.1% | 62 724 |
| Northern Grampians (S) | 25810 | 56.4% | 72.8% | 66.8% | 11 799 |
| Port Phillip (C) | 25900 | 57.7% | 66.1% | 61.3% | 102 501 |
| Pyrenees (S) | 25990 | No cases | 68.2% | 62.6% | 6 770 |
| Queenscliffe (B) | 26080 | 57.4% | 70.3% | 64.7% | 3 058 |
| South Gippsland (S) | 26170 | 53.4% | 73.5% | 65.0% | 27 930 |
| Southern Grampians (S) | 26260 | 63.2% | 73.3% | 70.9% | 16 145 |
| Stonnington (C) | 26350 | 54.5% | 68.3% | 60.8% | 103 187 |
| Strathbogie (S) | 26430 | 59.1% | 71.2% | 66.8% | 9 706 |
| Surf Coast (S) | 26490 | 56.2% | 71.0% | 65.3% | 28 282 |
| Swan Hill (RC) | 26610 | 59.5% | 72.4% | 68.6% | 20 867 |
| Towong (S) | 26670 | 57.8% | 70.1% | 65.2% | 5 889 |
| Unincorporated Vic | 29399 | No cases | 70.3% | 64.6% | 758 |
| Wangaratta (RC) | 26700 | 58.5% | 67.2% | 61.9% | 27 197 |
| Warrnambool (C) | 26730 | 54.8% | 68.1% | 60.7% | 33 300 |
| Wellington (S) | 26810 | 58.7% | 72.4% | 67.1% | 42 319 |
| West Wimmera (S) | 26890 | 61.9% | 69.3% | 66.3% | 4 089 |
| Whitehorse (C) | 26980 | 53.6% | 65.3% | 58.1% | 161 724 |
| Whittlesea (C) | 27070 | 60.7% | 66.0% | 63.3% | 179 261 |
| Wodonga (RC) | 27170 | 50.7% | 66.7% | 57.1% | 37 345 |
| Wyndham (C) | 27260 | 53.7% | 76.0% | 65.8% | 189 618 |
| Yarra (C) | 27350 | 60.5% | 59.4% | 57.6% | 83 593 |
| Yarra Ranges (S) | 27450 | 65.6% | 71.7% | 69.6% | 149 538 |
| Yarriambiack (S) | 27630 | 54.6% | 71.5% | 64.3% | 7 018 |
Cities (C), Rural Cities (RC), Boroughs (B) and Shires (S)
Discussion
Our study, using geocoding of Victorian OHCA registry data, found significant regional variation in both the incidence of OHCA and rates of bystander CPR rates for witnessed arrests. This variation was seen across the entire state, with differences seen in neighboring communities in both metropolitan Melbourne and regional areas. Areas with high incidence and low bystander CPR were able to be identified.
Reported OHCA incidence rates are known to vary both within and across countries[3], including in previous reports from Australia[24,25]. Our data suggests some of this variation may be explained by the regions examined and in the periods of time studied. We found significant sub-State variation in OHCA incidence rates, which is consistent with reports across census tracts in the United States[26–28]. To our knowledge, ours is the first study to include rural regions with low and very low density populations (<200/km2), some of which had the highest incidence rates across the state. Our study also noted a decline in the overall incidence over the study period, which was also reported in another Australian study[29], but this decline was not consistently seen across the state. The fluctuations in incidence rates over time in our study is contrary to a previous US study[26], which found incidence rates across census tracts to be stable between two consecutive 2-year periods. However, it’s worth noting that we compared periods of different length (2 years vs 3 years), and different years (2005–2009 vs 2008–2013) to the Semple study. Similar to our study though, Semple et al. [26] did report changes in bystander CPR rates across census tracks over time [26].
Our study restricted the examination of bystander CPR rates to bystander witnessed OHCAs. We did this as witnessed arrests are strongly associated with bystander CPR[30], and rates of witnessed arrests have fluctuated over time with our region[19,31]. Increases in bystander CPR rates occurred in all but one region over the study period. This increase is difficult to explain as telephone-CPR instructions remained constant over the study period[15]. Rural regions changed from a manual system of emergency call taking to an electronic emergency call taking algorithm in 2010–11[19]. This change may have improved the recognition of OHCA in the emergency call[32] or possibly the compliance with the protocols, but does not explain the increase seen in metropolitan regions. Alternatively, it’s possible that there were changes in CPR training following the 2010 guidelines or shifts in the underlying demographics of the regions which may impact rates.
Studies based in the US and Asia have identified demographics factors that differ between low and high-risk regions. These areas tend to have specific racial compositions, and lower levels of education and income[18,33,34]. The next phase of our study intends to explore the demographic factors seen in our high risk regions and whether shifts in the population are responsible for the changes seen over time in our study. However, that these high-risk areas can change over time is an important consideration in the development and testing of community-based interventions targeting these regions. Thus interventions may choose to focus on those areas at persistently high-risk over time[26], and consider changes in relevant underlying characteristics during any evaluation period.
This study has a number of limitations. Firstly, we assigned arrests to the regions in which they occurred. This means that estimates in the regions where people commute to work may over estimate that incidence. This is particularly likely to affect the Melbourne central business district; however it’s worth noting that bystander CPR rates in this region are the highest in the state and thus unlikely to be targeted for interventions to improve bystander CPR participation. Secondly, it’s possible that the incidence of OHCA and bystander CPR rates may be correlated with population density. Thus it’s possible that estimates in rural areas may have been biased too heavily toward the mean. Although ours is a conservative approach, small-area estimation models which better explain the heterogeneity may improve estimates for data sparse regions[35].
Conclusion
Our data supports reports of regional variation in OHCA incidence and bystander CPR rates–which in our case occurred even across a large metropolitan city and among bystander witnessed OHCAs. Identifying lower bystander CPR rates in the context of higher OHCA incidence identifies those regions where there is the greatest potential to improve survival–particularly in regions where high-risk status persists.
Data Availability
Due to ethical restrictions set by Ambulance Victoria regarding patient confidentiality, data are available upon request. Requests for data may be sent to Karen Smith (karen.smith@ambulance.vic.gov.au).
Funding Statement
LS, BB, JB and JF receive salary support from the NHMRC Australian Resuscitation Outcomes Consortium (Aus-ROC) Centre of Research Excellence (CRE) (ID:1029983, https://www.ausroc.org.au). KD is supported by a National Health and Medical Research Council (NHMRC) Public Health Postgraduate Research Scholarship (ID: 1075456) and a scholarship funded through the NHMRC Aus-ROC CRE. JB receives an early career researcher fellowship from the NHMRC and the Heart Foundation. JF receives salary support from St John Ambulance Western Australia.
References
- 1. Ornato JP, Becker LB, Weisfeldt ML, Wright BA. Cardiac arrest and resuscitation: an opportunity to align research prioritization and public health need. Circulation. 2010;122: 1876–1879. 10.1161/CIRCULATIONAHA.110.963991 [DOI] [PubMed] [Google Scholar]
- 2. Sasson C, Rogers MAM, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3: 63–81. 10.1161/CIRCOUTCOMES.109.889576 [DOI] [PubMed] [Google Scholar]
- 3. Berdowski J, Berg RA, Tijssen JGP, Koster RW. Global incidences of out-of-hospital cardiac arrest and survival rates: Systematic review of 67 prospective studies. Resuscitation. 2010;81: 1479–1487. 10.1016/j.resuscitation.2010.08.006 [DOI] [PubMed] [Google Scholar]
- 4. Brooks SC, Schmicker RH, Rea TD, Aufderheide TP, Davis DP, Morrison LJ, et al. Out-of-hospital cardiac arrest frequency and survival: evidence for temporal variability. Resuscitation. 2010;81: 175–181. 10.1016/j.resuscitation.2009.10.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lund-Kordahl I, Olasveengen TM, Lorem T, Samdal M, Wik L, Sunde K. Improving outcome after out-of-hospital cardiac arrest by strengthening weak links of the local Chain of Survival; quality of advanced life support and post-resuscitation care. Resuscitation. 2010;81: 422–6. 10.1016/j.resuscitation.2009.12.020 [DOI] [PubMed] [Google Scholar]
- 6. Iwami T, Nichol G, Hiraide A, Hayashi Y, Nishiuchi T, Kajino K, et al. Continuous Improvements in “Chain of Survival” Increased Survival After Out-of-Hospital Cardiac Arrests A Large-Scale Population-Based Study. Circulation. 2009;119: 728–734. 10.1161/CIRCULATIONAHA.108.802058 [DOI] [PubMed] [Google Scholar]
- 7. Nolan J, Soar J, Eikeland H. The chain of survival. Resuscitation. 2006;71: 270–271. 10.1016/j.resuscitation.2006.09.001 [DOI] [PubMed] [Google Scholar]
- 8. Bossaert L, Van Hoeyweghen R. Bystander cardiopulmonary resuscitation (CPR) in out-of-hospital cardiac arrest. Resuscitation. 1989;17, Supplement: S55–S69. 10.1016/0300-9572(89)90091-9 [DOI] [PubMed] [Google Scholar]
- 9. Gallagher E, Lombardi G, Gennis P. EFfectiveness of bystander cardiopulmonary resuscitation and survival following out-of-hospital cardiac arrest. JAMA. 1995;274: 1922–1925. 10.1001/jama.1995.03530240032036 [DOI] [PubMed] [Google Scholar]
- 10. Ritter G, Wolfe RA, Goldstein S, Landis JR, Vasu CM, Acheson A, et al. The effect of bystander CPR on survival of out-of-hospital cardiac arrest victims. American Heart Journal. 1985;110: 932–937. 10.1016/0002-8703(85)90187-5 [DOI] [PubMed] [Google Scholar]
- 11. O’Keeffe C, Nicholl J, Turner J, Goodacre S. Role of ambulance response times in the survival of patients with out-of-hospital cardiac arrest. Emerg Med J. 2011;28: 703–706. 10.1136/emj.2009.086363 [DOI] [PubMed] [Google Scholar]
- 12. Copley DP, Mantle JA, Rogers WJ, Russell RO, Rackley CE. Improved outcome for prehospital cardiopulmonary collapse with resuscitation by bystanders. Circulation. 1977;56: 901–905. 10.1161/01.CIR.56.6.901 [DOI] [PubMed] [Google Scholar]
- 13. Eisenberg M, Bergner L, Hallstrom A. Paramedic programs and out-of-hospital cardiac arrest: I. Factors associated with successful resuscitation. Am J Public Health. 1979;69: 30–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Roth R, Stewart RD, Rogers K, Cannon GM. Out-of-hospital cardiac arrest: factors associated with survival. Ann Emerg Med. 1984;13: 237–243. [DOI] [PubMed] [Google Scholar]
- 15. Bray JE, Deasy C, Walsh J, Bacon A, Currell A, Smith K. Changing EMS dispatcher CPR instructions to 400 compressions before mouth-to-mouth improved bystander CPR rates. Resuscitation. 2011;82: 1393–1398. 10.1016/j.resuscitation.2011.06.018 [DOI] [PubMed] [Google Scholar]
- 16. Vaillancourt C, Stiell IG, Wells GA. Understanding and improving low bystander CPR rates: a systematic review of the literature. CJEM. 2008;10: 51–65. [DOI] [PubMed] [Google Scholar]
- 17. Sasson C, Cudnik MT, Nassel A, Semple H, Magid DJ, Sayre M, et al. Identifying High-risk Geographic Areas for Cardiac Arrest Using Three Methods for Cluster Analysis. Academic Emergency Medicine. 2012;19: 139–146. 10.1111/j.1553-2712.2011.01284.x [DOI] [PubMed] [Google Scholar]
- 18. Fosbøl EL, Dupre ME, Strauss B, Swanson DR, Myers B, McNally BF, et al. Association of neighborhood characteristics with incidence of out-of-hospital cardiac arrest and rates of bystander-initiated CPR: implications for community-based education intervention. Resuscitation. 2014;85: 1512–1517. 10.1016/j.resuscitation.2014.08.013 [DOI] [PubMed] [Google Scholar]
- 19. Nehme Z, Bernard S, Cameron P, Bray JE, Meredith IT, Lijovic M, et al. Using a Cardiac Arrest Registry to Measure the Quality of Emergency Medical Service Care Decade of Findings From the Victorian Ambulance Cardiac Arrest Registry. Circ Cardiovasc Qual Outcomes. 2015;8: 56–66. 10.1161/CIRCOUTCOMES.114.001185 [DOI] [PubMed] [Google Scholar]
- 20. Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries. A statement for healthcare professionals from a task force of the international liaison committee on resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa). Resuscitation. 2004;63: 233–249. 10.1016/j.resuscitation.2004.09.008 [DOI] [PubMed] [Google Scholar]
- 21.Australian Bureau of Statistics. Population/People—Population/People [Internet]. Available: http://www.abs.gov.au/AUSSTATS/abs@nrp.nsf/Previousproducts/505Population/People12005-2009?opendocument&tabname=Summary&prodno=505&issue=2005-2009
- 22. Australian Bureau of Statistics. 2033.0.55.001—Census of Population and Housing: Socio-Economic Indexes for Areas (SEIFA), Australia, 2011 [Internet]. Canberra: Australian Bureau of Statistics; 2013. March Available: http://www.abs.gov.au/ausstats/abs@.nsf/mf/2033.0.55.001 [Google Scholar]
- 23. Introducing Multilevel Modeling. 1 edition London ; Thousand Oaks, Calif: SAGE Publications Ltd; 1998. [Google Scholar]
- 24. Finn JC, Jacobs IG, Holman CDJ, Oxer HF. Outcomes of out-of-hospital cardiac arrest patients in Perth, Western Australia, 1996–1999. Resuscitation. 2001;51: 247–255. 10.1016/S0300-9572(01)00408-7 [DOI] [PubMed] [Google Scholar]
- 25. Jennings PA, Cameron P, Walker T, Bernard S, Smith K. Out-of-hospital cardiac arrest in Victoria: rural and urban outcomes. Med J Aust. 2006;185: 135–139. [DOI] [PubMed] [Google Scholar]
- 26. Semple HM, Cudnik MT, Sayre M, Keseg D, Warden CR, Sasson C, et al. Identification of High-Risk Communities for Unattended Out-of-Hospital Cardiac Arrests Using GIS. J Community Health. 2012;38: 277–284. 10.1007/s10900-012-9611-7 [DOI] [PubMed] [Google Scholar]
- 27. Raun LH, Jefferson LS, Persse D, Ensor KB. Geospatial Analysis for Targeting Out-of-Hospital Cardiac Arrest Intervention. American Journal of Preventive Medicine. 2013;45: 137–142. 10.1016/j.amepre.2013.03.013 [DOI] [PubMed] [Google Scholar]
- 28. Sasson C, Keirns CC, Smith D, Sayre M, Macy M, Meurer W, et al. Small Area Variations in Out-of-Hospital Cardiac Arrest: Does the Neighborhood Matter? Ann Intern Med. 2010;153: 19–22. 10.7326/0003-4819-153-1-201007060-00255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bray JE, Di Palma S, Jacobs I, Straney L, Finn J. Trends in the incidence of presumed cardiac out-of-hospital cardiac arrest in Perth, Western Australia, 1997–2010. Resuscitation. 2014;85: 757–761. 10.1016/j.resuscitation.2014.02.017 [DOI] [PubMed] [Google Scholar]
- 30. Vaillancourt C, Lui A, De Maio VJ, Wells GA, Stiell IG. Socioeconomic status influences bystander CPR and survival rates for out-of-hospital cardiac arrest victims. Resuscitation. 2008;79: 417–423. 10.1016/j.resuscitation.2008.07.012 [DOI] [PubMed] [Google Scholar]
- 31. Nehme Z, Andrew E, Cameron PA, Bray JE, Bernard SA, Meredith IT, et al. Population density predicts outcome from out-of-hospital cardiac arrest in Victoria, Australia. Med J Aust. 2014;200 Available: https://www.mja.com.au/journal/2014/200/8/population-density-predicts-outcome-out-hospital-cardiac-arrest-victoria [DOI] [PubMed] [Google Scholar]
- 32. Heward A, Damiani M, Hartley-Sharpe C. Does the use of the Advanced Medical Priority Dispatch System affect cardiac arrest detection? Emerg Med J. 2004;21: 115–118. 10.1136/emj.2003.006940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Sasson C, Magid DJ, Chan P, Root ED, McNally BF, Kellermann AL, et al. Association of Neighborhood Characteristics with Bystander-Initiated CPR. New England Journal of Medicine. 2012;367: 1607–1615. 10.1056/NEJMoa1110700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Chiang W-C, Ko PC-I, Chang AM, Chen W-T, Liu SS-H, Huang Y-S, et al. Bystander-initiated CPR in an Asian metropolitan: Does the socioeconomic status matter? Resuscitation. 2014;85: 53–58. 10.1016/j.resuscitation.2013.07.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Srebotnjak T, Mokdad AH, Murray CJ. A novel framework for validating and applying standardized small area measurement strategies. Population Health Metrics. 2010;8: 26 10.1186/1478-7954-8-26 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Due to ethical restrictions set by Ambulance Victoria regarding patient confidentiality, data are available upon request. Requests for data may be sent to Karen Smith (karen.smith@ambulance.vic.gov.au).