Abstract
Backgrounds
Sleep and circadian rhythm disruptions are prominent, trait-like features of bipolar disorder (BD) which precede the onset of mood episodes. Neurocognitive impairments also characterize BD not only during acute phases of the illness but also during remission. Although the relationship between these two debilitating aspects of the illness might seem intuitive, very little is known about their relationship. We examined the association between sleep dysfunction and neurocognition in BD.
Methods
In a sample of 117 BD patients(mean age = 45.0±10.7; 59.0% (n=69) male), neurocognitive functioning was assessed using the MATRICS Consensus Cognitive Battery (MCCB). Sleep quality data were collected using the Epworth Sleepiness Scale (ESS) and the Pittsburgh Sleep Quality Index (PSQI). Partial Pearson correlations tested for a relationship between sleep and neurocognition. Path analyses were conducted to examine the hypothesized direct influence of sleep disruption on neurocognition.
Results
Higher levels of sleep disruptions were associated with a more severe clinical presentation and poorer performance in social cognition, visual learning and working memory. Social cognition and working memory were directly (negatively) predicted by sleep disruptions.
Limitations
The study was limited by a relatively small sample size and the lack of behavioral and biological objectives measure of activity/rest cycles.
Conclusions
Our study suggests that in patients with BD, sleep disruptions have a detrimental effect on general level of psychopathology and contribute directly to impaired cognitive functioning in the domains of social cognition and working memory. More research using objective measurement of sleep should be pursued to support these data and to further investigate the causal relationship between these disabling aspects of the illness.
Keywords: sleep disruption, sleep quality, neurocognition, bipolar disorder
INTRODUCTION
Bipolar disorder (BD) is characterized by fluctuating depression and mania with presumed inter-episode recovery; however, data clearly document that neither complete symptomatic remission nor functional recovery are the norm (Altshuler et al., 2002). Among the most persistent symptoms are circadian-based sleep and daytime activity abnormalities, often associated with anergia and psychomotor retardation (Mitchell and Malhi, 2004). Deficits in certain aspects of neurocognition are also common during remission (Golberg and Burdick, 2008). The presence of these continuing symptoms has a profound impact on quality of life, with a direct influence on clinical course and functional outcome (Marangell et al., 2009; Martínez-Arán et al., 2004).
Circadian Abnormalities in Euthymic BD
It has been long understood that changes in sleep and daytime activity/energy are cardinal features of acute mania and depression, with more recent data suggesting that these symptoms may represent trait-related risk factors for BD (Plante and Winkelman, 2008). Approximately 70% of remitted BD patients report diminished sleep efficiency and decreased daytime activity levels (Harvey et al., 2005). Euthymic patients with BD demonstrate increased sleep latency, a persistent pattern of insomnia and hypersomnia, and heightened sensitivity to shifts in circadian rhythms as compared with healthy controls (Ritter et al., 2012) and participants at increased risk for BD report a similar pattern, suggesting that circadian abnormalities represent a core illness feature that precede the onset of frank mood episodes.
A decreased need for sleep (maintenance of energy without adequate sleep) presents prior to the illness onset and during the prodromal period (Skjelstad et al., 2010). Unaffected offspring of BD patients demonstrate disrupted sleep/activity levels vs. controls without a family history (Ankers and Jones, 2009), supporting circadian abnormalities as a genetically-mediated feature of BD. Indeed, several genes that are known to regulate circadian functions (e.g. CLOCK, PERIOD) are risk loci for BD (Dallaspezia and Benedetti, 2009; Shi et al., 2008). A CLOCK gene polymorphism moderates features of the illness such as diurnal preference (Katzenberg et al., 1998), levels of evening activity, and delayed sleep onset in BD (Benedetti et al., 2007). The same variant has been linked with anterior cingulate activation in BD patients performing an emotional decision-making task (Benedetti et al., 2008). These convergent data suggest that biological rhythm abnormalities are core features of BD implicated in its pathophysiology.
Importantly, data suggest that impaired sleep quality in BD is associated with reduced quality of life. Gruber et al. (2004) assessed the relationship between sleep and clinical features in 2024 BD patients enrolled in NIMH STEP-BD (Gruber et al., 2004). Abnormal sleep duration was associated with poor functional outcome and quality of life. Patients with BD report significant anxiety related to their sleep, and cite circadian stability as an important goal of treatment (Ritter et al., 2012; Suto et al., 2010). In a study of 21 euthymic BD patients, sleep inefficiency and variability in total wake-time were associated with a greater number of lifetime depressive episodes and higher levels of current subthreshold depression and mania (Eidelman et al., 2010). Even subtle changes in sleep-wake patterns in BD can result in rapid destabilization and the onset of acute episodes (Plante and Winkelman, 2008). These data support the need to normalize biological rhythms to improve clinical status and quality of life in patients with BD.
Cognitive Impairment in BD
In addition to chronic neurovegetative symptoms, many BD patients are cognitively impaired during euthymia, particularly in the domains of attention, verbal memory, and executive functioning (Arts et al., 2008; Bowie et al., 2010; Golberg and Burdick, 2008). Although less severe than in neurocognition, deficits in social cognition (a broad domain encompassing different subcomponents such as the ability to recognize and respond appropriately to emotional stimuli, understanding emotions in the self and in the others, and awareness of social roles and behaviors) have been reported in euthymic BD (Lee et al., 2013; Samamé et al., 2012). Taken together deficits on neurocognition, similar to the effects of sleep disruption on quality of life, contribute significantly to functional disability in BD (Bowie et al., 2010), making them a critical treatment target for future studies (Burdick et al., 2012, 2007; Perez-Rodriguez et al., 2015).
Relationship between Circadian and Cognitive Impairment in BD
The relationship between sleep quality, daytime wakefulness, and neurocognition seems intuitive, with sleep deprivation resulting in lower energy and impaired cognition in animals and humans (Gerstner et al., 2009). Although few studies have assessed the possible association between circadian and cognitive dysfunction in BD, given their persistent impairment during euthymia and what is known from prior work in other clinical samples, it is reasonable to assume that they are closely linked. A study evaluated the deleterious cognitive effects of biological rhythm disruption in BD and demonstrated that circadian disruption is highly prevalent (approximately 80%) in inter-episode patients and that sleep disruption was the strongest predictor of everyday function including work and social outcome (Giglio et al., 2010). Moreover, although only a single task of executive functioning was administered, results indicated significant correlations between performance on this measure and biological rhythms. Likewise, a recent study reported that BD patients with more severe cognitive dysfunction report higher rates of insomnia compared to patients with intact cognitive functioning (Volkert et al., 2015). Although in this latter study the sleep disruptions were evaluated by using a non-sleep specific measure (rather from a depressive symptom rating scale) the results support the presence of an association between sleep disruption and cognitive dysfunction in BD (Volkert et al., 2015). To the best of our knowledge there is no study addressing the relationship between sleep disruption and social cognition in BD yet.
Taken together, these data suggest that these commonly co-occurring symptoms in remitted BD may be directly linked with one another. A better understanding of their relationship may shed light on a shared neurobiology and point toward novel pharmacological and psychotherapeutic strategies that could successfully target both domains simultaneously. In an effort to evaluate this relationship, we have assessed a cohort of stable BD patients on measures of sleep dysfunction, daytime sleepiness, and cognitive functioning and have tested the hypothesis that core bipolar disorder symptomatology and sleep disruptions would have both direct and mediating effects on cognitive functioning.
METHODS
Participants
The sample was composed of 117 BD outpatients from two sites: 89 patients from the Icahn School of Medicine at Mount Sinai and 28 from the Zucker Hillside Hospital – North Shore Long Island Jewish Health System (NSLIJHS). Inclusion criteria were: 1) Diagnosis of BD I or BD II or BD NOS; 2) 18-65 years old; 3) Current affective stability as measured by a score of less than 15 on the Hamilton Rating Scale for Depression [HRSD; (Hamilton, 1967)] and a score of less than 8 on the Clinician Administered Rating Scale for Mania [CARS-M; (Altman et al., 1994)]. Exclusion criteria were: 1) history of CNS trauma, neurological disorder, and ADHD or Learning Disability diagnosed in childhood; 2) diagnosis of recent substance abuse/dependence (past 3 months); 3) active, unstable medical problem; 4) ECT in the past 12 months. All procedures were approved by the local IRB and written informed consent was obtained from all participants.
Clinical Measures
DSM-IV diagnosis of BD was ascertained and confirmed by a consensus panel using the Structured Clinical Interview for DSM-IV (SCID). Numbers of life-time mood episodes were collected during the diagnostic interview; current depressive and manic symptoms were evaluated using the HRSD and the CARS-M. Severity of general psychiatric symptoms was assessed through the Brief Psychiatric Rating Scale [BPRS; (Pull and Overall, 1977)] and trait levels of impulsivity were measured using the Barratt Impulsiveness Scale [BIS-11; (Patton et al., 1995)].
Neurocognitive Measures
The MATRICS (Measurement and Treatment Research to Improve Cognition in Schizophrenia) Consensus Cognitive Battery [MCCB; (Nuechterlein et al., 2008)] was used to evaluate neurocognitive performance. The MCCB includes several tests that give rise to 7 cognitive domains: 1) Processing Speed [Brief Assessment of Cognition in Schizophrenia (BACS) and Trail Making Test part A]; 2) Attention/Vigilance [Continuous Performance Test—Identical Pairs (CPT-IP)]; 3) Working Memory [Wechsler Memory Scale (spatial and letter-number span)]; 4) Verbal Learning [Hopkins Verbal Learning Test—Revised (HVLT-R)]; 5) Visual Learning [Brief Visuospatial Memory Test—Revised (BVMT-R)]; 6) Reasoning and Problem Solving [Neuropsychological Assessment Battery (NAB) Mazes subtest]; and 7) Social Cognition [Mayer–Salovey–Caruso Emotional Intelligence Test (MSCEIT)]. The battery takes approximately 70 minutes to complete and testing was done in a single session. Scores are expressed in t-scores with a mean of 50 and a standard deviation (SD) of 10. The Wide Range Achievement Test (WRAT)-3 (Wilkinson, 1993) was used to obtain the estimated premorbid intelligence.
Sleep/Activity Assessment
The Epworth Sleepiness Scale [ESS(Johns, 1991)] and the Pittsburgh Sleep Quality Index [PSQI; (Buysse et al., 1989)] were used to evaluate daytime wakefulness and sleep quality.
The ESS is a self-report questionnaire that measures daytime sleepiness/wakefulness. Subjects rate the probability of falling asleep on a scale of increasing probability from 0 to 3 in eight situations (e.g. sitting and reading, watching TV, talking to someone, or in car as a passenger). The ESS total score (ESS Total) ranges from 0 to 24.
The PSQI is a self-report instrument measuring the quality and pattern of sleep in adults. It is not intended for the diagnosis of sleep disorders, but rather to identify ‘good’ and ‘bad sleepers’. Subjects rate their sleep habits within the past month by reporting the frequency with which a specific sleep habit occurs. The test gives rise to 7 subscales (Sleep Duration, Sleep Disturbances, Sleep Latency, Daytime Dysfunction, Sleep Efficiency, Overall Sleep Quality and Use of Sleeping Medication), of which we were most interested in the functionally-relevant subscales measuring sleep disturbances and daytime dysfunction and overall sleep quality (PSQI Total). Scores range from 0 to 3 for the subscales and from 0 to 21 for the total PSQI score. For both the ESS and PSQI higher scores indicate more severe sleep disruption.
Statistical Analyses
The associations between sleep measures (total score obtained from the ESS, the PSQI total and subscale scores) and both age and clinical data (depressive and manic symptoms, premorbid IQ, level of general psychopathology and impulsiveness) were tested using bivariate Pearson correlations. Bivariate Pearson correlations were done to evaluate the potential association between neurocognitive performance and psychotropic medications; also comparison in neurocognitive performance between patients taking vs those not taking medication was examined using independent sample t-test. We explored the association between sleep measures and neurocognitive functioning in a dimensional manner using bivariate Pearson correlations. . Significant (p value <.05) and trend-level correlations (p value < .10) were followed up using a series of path analyses to test the direct and indirect relationships between clinical symptoms, sleep disruption and neurocognitive functioning.
Path analysis is a statistical technique that tests hypotheses about the causal connections between a set of variables. Model selection was done through an iterative procedure. Starting from a saturated model (where all variables are interrelated), we gradually excluded those pathway correlations that are not significant until a good-fitting model was reached. Goodness of fit was assessed by examining three indices: the Chi-square, the Comparative Fit Index (CFI) and the Root Mean Square of Error Approximation (RMSEA). A good model is defined by a not significant Chi-Square test (p value ≥.5), a CFI equal or higher than .9 and a RMSEA lower or equal to .6. A ratio of five cases to each parameter in the path analysis is necessary for appropriate statistical power. Our saturated models included no more than 25 parameters, therefore statistical power with a sample of 117 was considered satisfactory. Further retrospective power analysis based on the RMSEA indices (MacCallum et al., 1996) obtained from the path analysis showed that with our current sample size we achieve a statistical power of 0.9 for both models investigating the predictive power of sleep disruption on working memory and on social cognition.
The model was structured such that the direct and indirect effects of clinical symptoms (symptoms of mania and depression as well as trait impulsivity; top tier of model) and sleep quality (second tier) on cognition (third tier) could be tested.
RESULTS
The mean age of the participants was 45.0 (SD= 10.7), 59.0% (n=69) were males; and 27.4% (n=32) were Caucasian. The mean premorbid IQ (WRAT-3) was 96.1 (SD=13.7), indicating normal intellectual functioning. The mean score for current depressive symptoms (HRSD total) was 9.7 (SD=8.4) and the mean rating for manic symptoms (CARS-M total) was 4.5 (SD=5.6), consistent with affective stability (only 10% of the sample presented with subthreshold mood symptoms that did not meet strict euthymia criteria). The average rating for general psychopathology (BPRS total) was 24.1 (SD=6.1). Eighty-two patients had a diagnosis of BD I [n=32 (27.4%) with psychotic features]; 28 patients had a diagnosis of BD II ([n=8 (6.8%) with psychotic features]; and 7 patients (6.0%) had a diagnosis of BD NOS. The mean number of manic and hypomanic episodes was 12.9 (SD= 14.1); the mean number of depressive episodes was 14.5 (SD=15.1). Level of general impulsivity, as assessed by the BIS-11, was 70.3 (SD=11.3) (Table 1). As reported in Table 2 scores on the MCCB domains ranged around 1 SD below the mean of the general population, with poorest performance in the Working Memory Domain (mean T-score =38.4; SD=12.9). Correlational analyses between total number of psychotropic medications [mean=1.3 (SD=1.2)] and neurocognition were non-significant across all domains. When patients who were taking medications (N=37) were compared with those not currently taking medications (N=16), no significant differences were noted Due to complex medication regimens, a more sophisticated investigation of effects of specific types of medications on cognition was not possible.
Table 1.
Demographic and Clinical Characteristics of the Sample (n=117)
| N | % | |
|---|---|---|
| Sex (M/F) | 69/48 | 59/41 |
| Mean | SD | |
|---|---|---|
| Age | 45.0 | 10.7 |
| Premorbid Intellectual Functioning (WRAT-3) | 96.1 | 13.7 |
| Hamilton Rating Scale for Depression (HRSD) - 24 | 9.7 | 8.4 |
| Clinician Administered Rating Scale for Mania (CARS-M) | 4.5 | 5.6 |
| Brief Psychiatric Rating Scale (BPRS) | 24.1 | 5.7 |
| Number of Depressive Episodes | 14.5 | 15.1 |
| Number of Manic Episodes | 12.9 | 14.1 |
| Barratt Impulsiveness Scale (BIS) Impulsivity - Total Score | 70.3 | 11.3 |
| N | % | |
|---|---|---|
| Psychotropic Medications (N=53) | ||
| Antipsychotic (no/yes) | 28/25 | 52.8/47.2 |
| Lithium (no/yes) | 46/7 | 86.8/13.2 |
| Anticonvulsant (no/yes) | 38/15 | 71.7/28.3 |
| Antidepressant (no/yes) | 36/16 | 67.9/32.1 |
| Antianxiety (no/yes) | 48/5 | 90.6/9.4 |
Table 2.
Cognitive Performance, Mean Score of Daytime Sleepiness (ESS) and Sleep Quality (PSQI) in BD Patients
| MATRICS Cognitive Consensus Battery (MCCB) | Mean T-score | SD |
|---|---|---|
| Processing Speed (n=112) | 41.1 | 11.6 |
| Attention and Vigilance (n=110) | 40.1 | 11.7 |
| Working Memory (n=113) | 38.4 | 12.9 |
| Verbal Learning (n=55) | 39.1 | 7.7 |
| Visual Learning (n=112) | 39.9 | 12.9 |
| Reasoning & Problem Solving (n=112) | 42.0 | 9.4 |
| Social Cognition (n=113) | 41.3 | 11.8 |
| Mean Z-score | SD | |
|---|---|---|
| Epworth Sleepiness Scale (ESS; Daytime Sleepiness; n=116) | −.19 | 1.19 |
| Pittsburgh Sleep Quality Index (PSQI) | ||
| Sleep Disturbance (n=113) | −1.7 | 1.8 |
| Day Dysfunction (n=112) | −2.0 | 1.7 |
| Sleep Quality Total Score (n=114) | −3.8 | 2.6 |
A negative mean score on both ESS and PSQI corresponds to a more severe sleep disruption
Sleep Measures
Subjects had a mean ESS total score of 9.2 (SD= 4.9), which was significantly correlated with the PSQI day dysfunction (r=.224; p=.018) and the PSQI sleep disturbance (r=.250; p=.008) subscales from the PSQI. Scores on the ESS [(based upon normative data from a non-psychiatric sample without sleep disorders (Sanford et al., 2006)] showed that BD subjects in our sample reported negligible daytime sleepiness (mean z-score=-.19 +/−1.8; Table 2). Conversely BD subjects compared to normative US population (Buysse et al., 1989) reported severe impairment on the day dysfunction (z=-2.0+/−1.7) and sleep disturbance PSQI subscales (z=−1.7+/−1.8) with an overall level of sleep quality (PSQI total score) well below the mean of the healthy population (z=−3.8+/−2.6; Table 2). Indeed 85.7% of the BD subjects reported day dysfunction and all but one of the subjects (97.3%) reported sleep disturbance.
More severe sleep disruptions were associated with an overall more severe clinical presentation (Supplemental Material 1). Although patients were affectively stable at the time of assessment several associations with severity of subthreshold symptoms and sleep measures emerged. More severe depressive symptoms were associated with greater impairment on PSQI sleep disturbance (r =.223, p =.018) and PSQI day dysfunction (r=.335, p<.001). Likewise, a higher level of general psychopathology was also associated with greater impairment on sleep disturbance (r =.260, p =.005) and day dysfunction (r =.244, p =.010). Impairment on the sleep disturbance subscale was also associated with more severe manic symptoms (r =.326, p <.001), lower premorbid IQ (r =−.238, p =.013) and higher impulsivity (BIS Total score; r =.310, p =.001). The PSQ total score was strongly associated with more severe depression (r =.449, p<.001) and mania (r =.214, p=.022). There was no significant association between age and sleep disruptions.
Neurocognition and Sleep Disruption
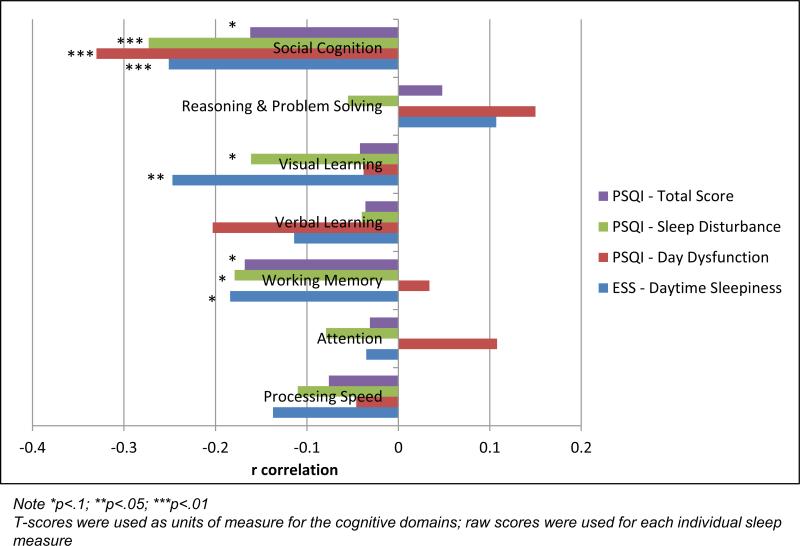
Correlational analyses indicated significant associations between cognitive performance and sleep disruptions (Figure 1; Supplemental Material 1). Performance on social cognitive measures was negatively associated with ESS total (daytime sleepiness; r=−.251, p =.008), PSQI sleep disturbance (r =−.273, p =.004), and PSQI day dysfunction (r =−.330, p<.001). Performance on a visual learning measure was also associated with ESS daytime sleepiness (r =−.247, p =.009). We found trend-level relationships between working memory performance and ESS daytime sleepiness (r=−.184, p =.052), PSQI sleep disturbance (r=−.179, p=.061) and PSQ total score (r=−.168, p=.078). Trend-level associations were also noted between visual learning performance and PSQI sleep disturbance (r=−.161, p=.094); and between social cognition and PSQ total score (r=−.162, p=.089). Based upon these correlational results we tested three potential models using pathway analyses to evaluate whether these aspects of cognition can be predicted by clinical symptomatology (depressive/manic symptoms, and impulsivity) and/or sleep disruption and to begin to address the direction of these relationships.
Figure 1.
Bivariate Correlations between Cognitive Domains (T-score units) and Sleep Measures (raw score for each individual measures)
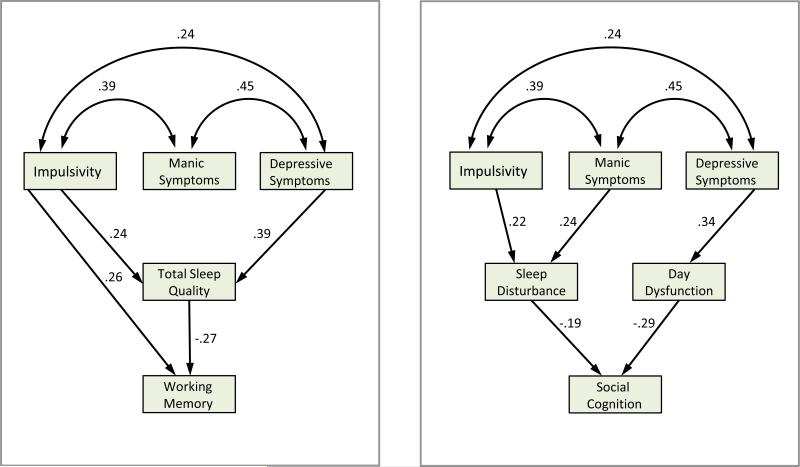
Path analyses supported good-fit predictive models for social cognition and working memory (indices of fit statistics reported in Table 3); however, the visual learning model did not achieve an adequate fit. Social cognition was directly predicted by PSQI sleep disturbance (regression weight=−.19) and PSQI day dysfunction (regression weight=−.29), while clinical symptoms only influenced cognition through an indirect pathway via their effects on sleep (i.e. impulsivity and manic symptoms directly influenced PSQI sleep disturbance, and depressive symptoms had direct effects on PSQI day dysfunction). PSQI total sleep quality had a direct effect (regression weight=−.27) on working memory performance and impulsivity had both direct (regression weight=.26) and indirect (via effects on PSQI sleep quality) effects on working memory. Depression indirectly impacted working memory via effects on PSQI sleep quality (direct and total standard effect are presented in Supplemental Material 2).
Table 3.
Indices for the Final Model and the Independence Modela testing the Relationship between Clinical Symptoms, Sleep Disruption and Cognition in Bipolar Disorder
| Goodness of Fit | |||||
|---|---|---|---|---|---|
| Outcome Measure | X2 | df | p value | CFI | RMSEA |
| Working Memory | |||||
| Final Model | 1.808 | 3 | .613 | 1.000 | .000 |
| Independence Model | 91.339 | 15 | <.001 | .000 | .209 |
| Social Cognition | |||||
| Final Model | 9.501 | 7 | .219 | .969 | .055 |
| Independence Model | 102.694 | 21 | <.001 | .000 | .183 |
The independence model is a null model that assumes that all the variables are uncorrelated with the dependent variable
To assess the directionality of our hypothesis and results, we also tested the reverse hypothesis that cognitive impairment in BD might be driving the expression of sleep or cognitive problems via direct or indirect effects on clinical symptomatology and sleep disruption. We tested an alternate model wherein cognition served as the endogenous variable influencing clinical symptoms and sleep disruption. As expected, this model was not statistically meaningful and was therefore rejected.
DISCUSSION
To our knowledge, this study is among the first to directly investigate the relationship between sleep disruption and neurocognition in BD. Our findings corroborate previous data noting sleep disruption as a prominent feature of BD (Harvey et al., 2005) and extend prior work to suggest that more severe cognitive impairment in BD is associated with higher rates of sleep dysfunction (Volkert et al., 2015). Data from the PSQI, which measures a broad range of sleep dimensions, suggest that the vast majority of patients with BD report major sleep disruptions even during affective remission. We further found that more severe sleep disruptions were associated more severe clinical symptoms and with lower premorbid IQ.
Next we explored the relationship between sleep dysfunction and neurocognition and found, as might be expected, that more severe sleep disruptions were associated with poorer cognitive performance. Specifically, performance on measures of working memory, visual learning, and social cognition was correlated with patient ratings of sleep quality (PSQI) and daytime sleepiness (ESS). When we applied path analysis to these variables in an effort to determine directionality of the relationships, we found valid predictive models for both working memory and social cognition. Working memory performance was best predicted by direct effects of sleep quality (PSQI total) and trait impulsivity (BIS-11). While the deleterious effects of poor sleep quality on cognition seems intuitive, the effects of impulsivity in this model are somewhat counterintuitive as they have a positive weight, suggesting a potential beneficial effect of higher trait impulsivity on working memory in our BD patients. The relationship between impulsivity and sleep quality (higher trait impulsivity associated with more impaired sleep quality) further suggests that sleep disruptions are associated with a more severe clinical presentation in BD, consistent with evidence from healthy subjects suggesting that sleep disturbance is associated with higher level of impulsivity. Specifically prior work suggests that sleep deprived healthy adult subjects report higher risk taking behaviors compared to non-sleep deprived individuals (Killgore et al., 2006; McKenna et al., 2007).
Social cognitive performance was best predicted by direct effects of sleep disturbance and day dysfunction, with no direct effects attributed to any of the clinical symptoms. Current severity of affective symptoms only contributed to social cognitive performance via their effects on sleep quality (Figure 2).
Figure 2.
Prediction of Social Cognition (left) and Working Memory (right) with Clinical Symptoms and Sleep Disruptions in Bipolar Disorder
Together, these results suggest that sleep disruption and cognitive functioning may share a common neuropathological mechanism in BD. Previous studies in healthy subjects have demonstrated that once sleep is recovered following deprivation, energy and activity levels return to baseline and normal cognition is restored (Benca et al., 2009); however, the persistent nature of sleep abnormalities in BD suggests a more chronic circadian disruption. In preclinical work, Craig and McDonald (Craig and McDonald, 2008) demonstrated hippocampus-based learning and memory deficits in rats that were exposed to repeated phase shifts and recoveries but no such deficit in rats who underwent only acute phase shift and recovery, suggesting that it may be the chronicity of the circadian disruption that leads to the persistent cognitive dysfunction seen in the remitted phase of BD.
The specific nature of the circadian abnormality in BD is not known; however, Dallaspezia and Benedetti described two related hypotheses: 1) Patients with BD have a biological clock that is detached from environmental variables that act to regulate circadian rhythms; and/or 2) The normal sleep-wake cycle in BD is not in phase with other biological rhythms (e.g. melatonin release) (Dallaspezia and Benedetti, 2009). Data in BD support a high rate of an “eveningness” chronotype, a preference for later bedtimes/wake-times, and for carrying out mental and physical activity in the evening as opposed to the morning (Volkert et al., 2015; Wood et al., 2009). Eveningness is associated with a circadian phase delay, a shift in the normal temperature reduction and melatonin secretion that triggers onset of the circadian-based sleep cycle, as well as waking times that are misaligned to circadian phase (Duffy et al., 1999). Such circadian desynchronization results in elevated melatonin, a sleep-promoting hormone, early in the day thereby impairing wakefulness and vigilance.
The potential to target sleep dysfunction and neurocognitive impairments using either pharmacological approaches or therapy will be an important consideration moving forward. There is not yet an effective class of medications able to target both deficits simultaneously. However, there are encouraging data suggesting that wake-promoting drugs that increase dopamine and serotonin activity in the cortex (e.g. modafinil) may have an enhancing effect on cognition in healthy, sleep-disordered and other psychiatric disorders (Minzenberg and Carter, 2008). Psychosocial interventions that incorporate psychoeducation and careful monitoring of social rhythms and sleep patterns, particularly Interpersonal Social Rhythms Therapy (IPSRT), have also been shown to be effective in reducing episode recurrence in BD over 2-years (Frank et al., 2005).
There are several limitations to acknowledge. The lack of a healthy control sample for purposes of direct comparison makes it more difficult to interpret the degree of sleep disruption in our BD sample; we did however include published normative data as a reference. While the mood state of our sample was defined as affectively remitted based upon standard mood ratings criteria, it remains likely that some degree of subsyndromal mood symptoms were present in a subset of our patients, which could partially account for sleep problems. Importantly, we utilized subjective self-report measures of sleep quality (ESS and PSQI). Future studies should extend this research to include objective behavioral (actigraphy) or biological measures [melatonin; cortisol] of activity/rest cycles and critical sleep-relevant hormones. Larger, strictly euthymic samples will be important in clarifying the nature of the circadian abnormalities and their relationship with cognition in BD.
In summary, our results seem to suggest that sleep disruption might have an adverse effect on neurocognition in BD. We provide statistical evidence to suggest that sleep problems may be driving neurocognitive impairments in BD, at least in some domains (working memory and social cognition). Further research using longitudinal designs and in individuals at risk for bipolar disorder will be important in establishing a causal relationship among these disabling aspect of the illness.
Supplementary Material
Highlights.
Sleep disruptions in BD are correlated with a more sever clinical presentation;
Higher levels of sleep disruptions are associated with a poorer performance in social cognition, visual learning and working memory;
Our results suggest that social cognition and working memory were directly (negatively) predicted by sleep disruptions.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Altman EG, Hedeker DR, Janicak PG, Peterson JL, Davis JM. The Clinician-Administered Rating Scale for Mania (CARS-M): development, reliability, and validity. Biol. Psychiatry. 1994;36:124–134. doi: 10.1016/0006-3223(94)91193-2. [DOI] [PubMed] [Google Scholar]
- Altshuler LL, Gitlin MJ, Mintz J, Leight KL, Frye MA. Subsyndromal depression is associated with functional impairment in patients with bipolar disorder. J. Clin. Psychiatry. 2002;63:807–811. doi: 10.4088/jcp.v63n0910. [DOI] [PubMed] [Google Scholar]
- Ankers D, Jones SH. Objective assessment of circadian activity and sleep patterns in individuals at behavioural risk of hypomania. J. Clin. Psychol. 2009;65:1071–1086. doi: 10.1002/jclp.20608. doi:10.1002/jclp.20608. [DOI] [PubMed] [Google Scholar]
- Arts B, Jabben N, Krabbendam L, van Os J. Meta-analyses of cognitive functioning in euthymic bipolar patients and their first-degree relatives. Psychol. Med. 2008;38:771–785. doi: 10.1017/S0033291707001675. doi:10.1017/S0033291707001675. [DOI] [PubMed] [Google Scholar]
- Benca R, Duncan MJ, Frank E, McClung C, Nelson RJ, Vicentic A. Biological rhythms, higher brain function, and behavior: Gaps, opportunities, and challenges. Brain Res. Rev. 2009;62:57–70. doi: 10.1016/j.brainresrev.2009.09.005. doi:10.1016/j.brainresrev.2009.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benedetti F, Dallaspezia S, Fulgosi MC, Lorenzi C, Serretti A, Barbini B, Colombo C, Smeraldi E. Actimetric evidence that CLOCK 3111 T/C SNP influences sleep and activity patterns in patients affected by bipolar depression. Am. J. Med. Genet. Part B Neuropsychiatr. Genet. Off. Publ. Int. Soc. Psychiatr. Genet. 2007;144B:631–635. doi: 10.1002/ajmg.b.30475. doi:10.1002/ajmg.b.30475. [DOI] [PubMed] [Google Scholar]
- Benedetti F, Radaelli D, Bernasconi A, Dallaspezia S, Falini A, Scotti G, Lorenzi C, Colombo C, Smeraldi E. Clock genes beyond the clock: CLOCK genotype biases neural correlates of moral valence decision in depressed patients. Genes Brain Behav. 2008;7:20–25. doi: 10.1111/j.1601-183X.2007.00312.x. doi:10.1111/j.1601-183X.2007.00312.x. [DOI] [PubMed] [Google Scholar]
- Bowie CR, Depp C, McGrath JA, Wolyniec P, Mausbach BT, Thornquist MH, Luke J, Patterson TL, Harvey PD, Pulver AE. Prediction of real-world functional disability in chronic mental disorders: a comparison of schizophrenia and bipolar disorder. Am. J. Psychiatry. 2010;167:1116–1124. doi: 10.1176/appi.ajp.2010.09101406. doi:10.1176/appi.ajp.2010.09101406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burdick KE, Braga RJ, Goldberg JF, Malhotra AK. Cognitive dysfunction in bipolar disorder: future place of pharmacotherapy. CNS Drugs. 2007;21:971–981. doi: 10.2165/00023210-200721120-00002. [DOI] [PubMed] [Google Scholar]
- Burdick KE, Braga RJ, Nnadi CU, Shaya Y, Stearns WH, Malhotra AK. Placebo-controlled adjunctive trial of pramipexole in patients with bipolar disorder: targeting cognitive dysfunction. J. Clin. Psychiatry. 2012;73:103–112. doi: 10.4088/JCP.11m07299. doi:10.4088/JCP.11m07299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Craig LA, McDonald RJ. Chronic disruption of circadian rhythms impairs hippocampal memory in the rat. Brain Res. Bull. 2008;76:141–151. doi: 10.1016/j.brainresbull.2008.02.013. doi:10.1016/j.brainresbull.2008.02.013. [DOI] [PubMed] [Google Scholar]
- Dallaspezia S, Benedetti F. Melatonin, circadian rhythms, and the clock genes in bipolar disorder. Curr. Psychiatry Rep. 2009;11:488–493. doi: 10.1007/s11920-009-0074-1. [DOI] [PubMed] [Google Scholar]
- Duffy JF, Dijk DJ, Hall EF, Czeisler CA. Relationship of endogenous circadian melatonin and temperature rhythms to self-reported preference for morning or evening activity in young and older people. J. Investig. Med. Off. Publ. Am. Fed. Clin. Res. 1999;47:141–150. [PMC free article] [PubMed] [Google Scholar]
- Eidelman P, Talbot LS, Gruber J, Harvey AG. Sleep, illness course, and concurrent symptoms in inter-episode bipolar disorder. J. Behav. Ther. Exp. Psychiatry. 2010;41:145–149. doi: 10.1016/j.jbtep.2009.11.007. doi:10.1016/j.jbtep.2009.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank E, Kupfer DJ, Thase ME, Mallinger AG, Swartz HA, Fagiolini AM, Grochocinski V, Houck P, Scott J, Thompson W, Monk T. Two-year outcomes for interpersonal and social rhythm therapy in individuals with bipolar I disorder. Arch. Gen. Psychiatry. 2005;62:996–1004. doi: 10.1001/archpsyc.62.9.996. doi:10.1001/archpsyc.62.9.996. [DOI] [PubMed] [Google Scholar]
- Gerstner JR, Lyons LC, Wright KP, Loh DH, Rawashdeh O, Eckel-Mahan KL, Roman GW. Cycling behavior and memory formation. J. Neurosci. Off. J. Soc. Neurosci. 2009;29:12824–12830. doi: 10.1523/JNEUROSCI.3353-09.2009. doi:10.1523/JNEUROSCI.3353-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giglio LMF, Magalhães PVS, Andersen ML, Walz JC, Jakobson L, Kapczinski F. Circadian preference in bipolar disorder. Sleep Breath. Schlaf Atm. 2010;14:153–155. doi: 10.1007/s11325-009-0301-3. doi:10.1007/s11325-009-0301-3. [DOI] [PubMed] [Google Scholar]
- Golberg JF, Burdick KE. Cognitive dysfunction in bipolar disorder. American Psychiatric Publishing; Arlington, VA.: 2008. [Google Scholar]
- Gruber SA, Rogowska J, Yurgelun-Todd DA. Decreased activation of the anterior cingulate in bipolar patients: an fMRI study. J. Affect. Disord. 2004;82:191–201. doi: 10.1016/j.jad.2003.10.010. doi:10.1016/j.jad.2003.10.010. [DOI] [PubMed] [Google Scholar]
- Hamilton M. Development of a rating scale for primary depressive illness. Br. J. Soc. Clin. Psychol. 1967;6:278–296. doi: 10.1111/j.2044-8260.1967.tb00530.x. [DOI] [PubMed] [Google Scholar]
- Harvey AG, Schmidt DA, Scarnà A, Semler CN, Goodwin GM. Sleep-related functioning in euthymic patients with bipolar disorder, patients with insomnia, and subjects without sleep problems. Am. J. Psychiatry. 2005;162:50–57. doi: 10.1176/appi.ajp.162.1.50. doi:10.1176/appi.ajp.162.1.50. [DOI] [PubMed] [Google Scholar]
- Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–545. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- Katzenberg D, Young T, Finn L, Lin L, King DP, Takahashi JS, Mignot E. A CLOCK polymorphism associated with human diurnal preference. Sleep. 1998;21:569–576. doi: 10.1093/sleep/21.6.569. [DOI] [PubMed] [Google Scholar]
- Killgore WDS, Balkin TJ, Wesensten NJ. Impaired decision making following 49 h of sleep deprivation. J. Sleep Res. 2006;15:7–13. doi: 10.1111/j.1365-2869.2006.00487.x. doi:10.1111/j.1365-2869.2006.00487.x. [DOI] [PubMed] [Google Scholar]
- Lee J, Altshuler L, Glahn DC, Miklowitz DJ, Ochsner K, Green MF. Social and Nonsocial Cognition in Bipolar Disorder and Schizophrenia: Relative Levels of Impairment. Am. J. Psychiatry. 2013;170:334–341. doi: 10.1176/appi.ajp.2012.12040490. doi:10.1176/appi.ajp.2012.12040490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacCallum RC, Browne MW, Sugawara HM. Power analysis and determination of sample size for covariance structure modeling. Psychol. Methods. 1996;1:130–149. doi:10.1037/1082-989X.1.2.130. [Google Scholar]
- Marangell LB, Dennehy EB, Miyahara S, Wisniewski SR, Bauer MS, Rapaport MH, Allen MH. The functional impact of subsyndromal depressive symptoms in bipolar disorder: data from STEP-BD. J. Affect. Disord. 2009;114:58–67. doi: 10.1016/j.jad.2008.07.006. doi:10.1016/j.jad.2008.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martínez-Arán A, Vieta E, Reinares M, Colom F, Torrent C, Sánchez-Moreno J, Benabarre A, Goikolea JM, Comes M, Salamero M. Cognitive function across manic or hypomanic, depressed, and euthymic states in bipolar disorder. Am. J. Psychiatry. 2004;161:262–270. doi: 10.1176/appi.ajp.161.2.262. [DOI] [PubMed] [Google Scholar]
- McKenna BS, Dickinson DL, Orff HJ, Drummond SPA. The effects of one night of sleep deprivation on known-risk and ambiguous-risk decisions. J. Sleep Res. 2007;16:245–252. doi: 10.1111/j.1365-2869.2007.00591.x. doi:10.1111/j.1365-2869.2007.00591.x. [DOI] [PubMed] [Google Scholar]
- Minzenberg MJ, Carter CS. Modafinil: a review of neurochemical actions and effects on cognition. Neuropsychopharmacol. Off. Publ. Am. Coll. Neuropsychopharmacol. 2008;33:1477–1502. doi: 10.1038/sj.npp.1301534. doi:10.1038/sj.npp.1301534. [DOI] [PubMed] [Google Scholar]
- Mitchell PB, Malhi GS. Bipolar depression: phenomenological overview and clinical characteristics. Bipolar Disord. 2004;6:530–539. doi: 10.1111/j.1399-5618.2004.00137.x. doi:10.1111/j.1399-5618.2004.00137.x. [DOI] [PubMed] [Google Scholar]
- Nuechterlein KH, Green MF, Kern RS, Baade LE, Barch DM, Cohen JD, Essock S, Fenton WS, Frese FJ, Gold JM, Goldberg T, Heaton RK, Keefe RSE, Kraemer H, Mesholam-Gately R, Seidman LJ, Stover E, Weinberger DR, Young AS, Zalcman S, Marder SR. The MATRICS Consensus Cognitive Battery, part 1: test selection, reliability, and validity. Am. J. Psychiatry. 2008;165:203–213. doi: 10.1176/appi.ajp.2007.07010042. doi:10.1176/appi.ajp.2007.07010042. [DOI] [PubMed] [Google Scholar]
- Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. J. Clin. Psychol. 1995;51:768–774. doi: 10.1002/1097-4679(199511)51:6<768::aid-jclp2270510607>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Perez-Rodriguez MM, Mahon K, Russo M, Ungar AK, Burdick KE. Oxytocin and social cognition in affective and psychotic disorders. Eur. Neuropsychopharmacol. J. Eur. Coll. Neuropsychopharmacol. 2015;25:265–282. doi: 10.1016/j.euroneuro.2014.07.012. doi:10.1016/j.euroneuro.2014.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plante DT, Winkelman JW. Sleep disturbance in bipolar disorder: therapeutic implications. Am. J. Psychiatry. 2008;165:830–843. doi: 10.1176/appi.ajp.2008.08010077. doi:10.1176/appi.ajp.2008.08010077. [DOI] [PubMed] [Google Scholar]
- Pull CB, Overall JE. Adequacy of the Brief Psychiatric Rating Scale for distinguishing lesser forms of psychopathology. Psychol. Rep. 1977;40:167–173. doi: 10.2466/pr0.1977.40.1.167. doi:10.2466/pr0.1977.40.1.167. [DOI] [PubMed] [Google Scholar]
- Ritter PS, Marx C, Lewtschenko N, Pfeiffer S, Leopold K, Bauer M, Pfennig A. The characteristics of sleep in patients with manifest bipolar disorder, subjects at high risk of developing the disease and healthy controls. J. Neural Transm. Vienna Austria 1996. 2012;119:1173–1184. doi: 10.1007/s00702-012-0883-y. doi:10.1007/s00702-012-0883-y. [DOI] [PubMed] [Google Scholar]
- Samamé C, Martino DJ, Strejilevich SA. Social cognition in euthymic bipolar disorder: systematic review and meta-analytic approach. Acta Psychiatr. Scand. 2012;125:266–280. doi: 10.1111/j.1600-0447.2011.01808.x. doi:10.1111/j.1600-0447.2011.01808.x. [DOI] [PubMed] [Google Scholar]
- Sanford SD, Lichstein KL, Durrence HH, Riedel BW, Taylor DJ, Bush AJ. The influence of age, gender, ethnicity, and insomnia on Epworth sleepiness scores: a normative US population. Sleep Med. 2006;7:319–326. doi: 10.1016/j.sleep.2006.01.010. doi:10.1016/j.sleep.2006.01.010. [DOI] [PubMed] [Google Scholar]
- Shi J, Wittke-Thompson JK, Badner JA, Hattori E, Potash JB, Willour VL, McMahon FJ, Gershon ES, Liu C. Clock genes may influence bipolar disorder susceptibility and dysfunctional circadian rhythm. Am. J. Med. Genet. Part B Neuropsychiatr. Genet. Off. Publ. Int. Soc. Psychiatr. Genet. 2008;147B:1047–1055. doi: 10.1002/ajmg.b.30714. doi:10.1002/ajmg.b.30714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skjelstad DV, Malt UF, Holte A. Symptoms and signs of the initial prodrome of bipolar disorder: a systematic review. J. Affect. Disord. 2010;126:1–13. doi: 10.1016/j.jad.2009.10.003. doi:10.1016/j.jad.2009.10.003. [DOI] [PubMed] [Google Scholar]
- Suto M, Murray G, Hale S, Amari E, Michalak EE. What works for people with bipolar disorder? Tips from the experts. J. Affect. Disord. 2010;124:76–84. doi: 10.1016/j.jad.2009.11.004. doi:10.1016/j.jad.2009.11.004. [DOI] [PubMed] [Google Scholar]
- Volkert J, Kopf J, Kazmaier J, Glaser F, Zierhut KC, Schiele MA, Kittel-Schneider S, Reif A. Evidence for cognitive subgroups in bipolar disorder and the influence of subclinical depression and sleep disturbances. Eur. Neuropsychopharmacol. J. Eur. Coll. Neuropsychopharmacol. 2015;25:192–202. doi: 10.1016/j.euroneuro.2014.07.017. doi:10.1016/j.euroneuro.2014.07.017. [DOI] [PubMed] [Google Scholar]
- Wilkinson GS. WRAT-3 : wide range achievement test administration manual. Wide Range, Inc.; Wilmington, Del.: 1993. [Google Scholar]
- Wood J, Birmaher B, Axelson D, Ehmann M, Kalas C, Monk K, Turkin S, Kupfer DJ, Brent D, Monk TH, Nimgainkar VL. Replicable differences in preferred circadian phase between bipolar disorder patients and control individuals. Psychiatry Res. 2009;166:201–209. doi: 10.1016/j.psychres.2008.03.003. doi:10.1016/j.psychres.2008.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.