Abstract
Background
In China, varicella vaccine has been available in the private sector to children ≥12 months of age since 1998 with a single-dose indication. In December 2006, varicella became a notifiable disease in Beijing. We used surveillance data to describe varicella vaccine uptake from 2005 to 2010 and varicella epidemiology in Beijing from 2007 to 2010.
Methods
Limited sociodemographic and clinical information was available from the passive surveillance system. Varicella vaccine coverage was estimated for each year for children born between 2004 and 2008 using the number of children in the immunization registry of each birth year as the denominator without adjustment for history of varicella.
Results
Vaccine coverage increased within each birth cohort between 2005 and 2010. The coverage at 2 years of age increased from 62.4% in 2005 to 74.1% in 2010 and was 80.4% in children 3–6 years of age in 2010. Between 2007 and 2010, 15,544 to 18,256 varicella cases were reported annually with stable overall incidence (range: 1.0–1.1/1000 persons), but the incidence in children 1–4 years of age decreased significantly from 6.2 per 1000 children in 2007 to 4.4 per 1000 children in 2010 (P < 0.001). Among adults (≥20 years of age), there were significant increases in the number and proportion of cases from 2557 (16.5%) in 2007 to 4277 (23.4%) in 2010 (P < 0.001).
Conclusions
Moderately high 1-dose vaccine coverage in young children has been achieved with declining disease incidence, but varicella remains a common, seasonal disease in the population. Current epidemiology suggests that a government-funded varicella vaccine program that includes catch-up vaccination for older children, adolescents and adults needs consideration.
Keywords: chickenpox, varicella vaccine, outbreak
Varicella (chickenpox) is a highly contagious disease caused by the varicella zoster virus, which, in the absence of vaccination, is a universal infection acquired mainly in childhood. Varicella vaccines are widely available globally; in Beijing, 3 vaccines are available: Varilrix of GlaxoSmithKline Biologicals (Rixensart, Belgium), licensed in 1998, and 2 vaccines manufactured in China (Changchun Keygen Biological Products Co., Ltd, Jilin, China and Shanghai Institute of Biological Products, Shanghai, China), which were both licensed in 2000. Currently, varicella vaccine is not included in the Expanded Program on Immunization in China, but is available for private purchase for individuals ≥12 months of age with a single-dose indication. In Beijing, varicella became a notifiable disease in December 2006. Since mid-2006, free varicella vaccine has been provided to affected schools in response to school outbreaks. We used data from varicella passive surveillance, reported outbreaks and the Beijing immunization registry to describe varicella epidemiology from 2007 to 2010 and varicella vaccine coverage since 2005.
METHODS
Varicella Definition and Reporting
For surveillance purposes, varicella is defined as a clinically diagnosed illness with acute onset of a diffuse maculopapulovesicular rash without other apparent cause. All clinical practitioners are required to report varicella cases electronically via the National Notifiable Infectious Diseases Reporting Information System within 24 hours to the local health department. Information collected from cases includes name, sex, date of birth, profession, address, date of rash onset and date of diagnosis. In Beijing, a varicella outbreak is defined as ≥5 cases in a school or other setting within 1 week. School outbreaks are investigated to collect detailed information on cases’ clinical presentations and vaccination status. Free varicella vaccine is provided for outbreak control to school students without a history of varicella or vaccination in kindergarten, elementary, middle and high schools. We used estimated census data as denominators to calculate the overall varicella incidence in Beijing. However, because of concern with age-specific population estimates derived from modeled census data in Beijing during the study period, we calculated annual varicella incidence in children aged 1–4 years between 2007 and 2010 using a denominator of children identified from birth registrations (Beijing residents) and children of the migrant population (<6 months of residence in Beijing during the year who are enumerated) during yearly outreach immunization campaigns for vaccine-preventable diseases covered by the Expanded Program on Immunization.
Vaccine Delivery and Varicella Vaccine Coverage Estimation
In Beijing, administration of all private and publically funded vaccines occurs in approximately 600 immunization clinics. In 2008, Beijing established an electronic immunization registry and requested that immunization providers record every vaccine administered to children 0–6 years of age including privately purchased vaccines, in the registry. In addition, retrospective records of vaccines administered in clinics since 2004 were entered into the registry. Varicella vaccine doses administered in schools for outbreak control are not recorded in the immunization registry. We used the children enrolled in the immunization registry in early 2011 to define birth cohorts from 2004 to 2008. We calculated varicella vaccination coverage using the cumulative number of children who had received varicella vaccine in each birth cohort each year divided by the total number of children in the corresponding birth cohorts in the registry in early 2011 without excluding those with prior varicella disease history because this information was not available.
Statistical Analyses
We used the Kruskal–Wallis or Mantel–Haenszel χ2 tests to evaluate the distribution of continuous or categorical variables related to varicella disease from 2007 to 2010. Geographic regions within Beijing were defined as rural, suburb and urban according to the level of urbanization in each county. All statistical analyses were performed with SAS V9.3 (SAS Institute, Cary, NC).
RESULTS
Epidemiology and Seasonality of the Varicella Disease
Between 2007 and 2010, 15,544 to 18,256 varicella cases were reported annually (Table 1). Fifty-six percent of the cases were male with a median age of 9 years (range: 0 month to 85 years). Twenty-one percent of the cases were <5 years of age, 29.6% were 5–9 years of age, 11.9% were 10–14 years of age and 37.2% were ≥15 years of age. The majority (68.3%) of the cases were students in kindergarten, elementary, middle or high schools. Adults (≥20 years of age) comprised 19.9% of the cases, of whom 3.9% (526) were healthcare workers. There was little change in the overall incidence from 2007 to 2010 (range: 1.0–1.1/1000 persons). However, the incidence in children 1–4 years of age decreased significantly from 6.2 per 1000 children in 2007 to 4.4 per 1000 children in 2010 (P < 0.001).
TABLE 1.
Sociodemographic Characteristics of the Reported Varicella Cases in Beijing, 2007 to 2010
| Total 2007 to 2010 (n = 67,326) n (%) |
2007 (n = 15,544) n (%) |
2008 (n = 17,219) n (%) |
2009 (n = 16,307) n (%) |
2010 (n = 18,256) n (%) |
|
|---|---|---|---|---|---|
| Incidence (/1000 persons) | NA | 1.0 | 1.1 | 1.0 | 1.0 |
| Sex | |||||
| Male | 37,778 (56.1) | 8903 (57.3) | 9630 (55.9) | 9237 (56.6) | 10,008 (54.8) |
| Female | 29,548 (43.9) | 6641 (42.7) | 7589 (44.1) | 7070 (43.4) | 8248 (45.2) |
| Age (yr) | |||||
| <1 | 2689 (4.0) | 455 (2.9) | 894 (5.2) | 647 (4.0) | 693 (3.8) |
| 1–4 | 11,726 (17.4) | 2673 (17.2) | 2943 (17.1) | 3127 (19.2) | 2983 (16.3) |
| 5–9 | 19,915 (29.6) | 4856 (31.2) | 4881 (28.3) | 4524 (27.7) | 5654 (31.0) |
| 10–14 | 7980 (11.9) | 2200 (14.2) | 2026 (11.8) | 1773 (10.9) | 1981 (10.9) |
| 15–19 | 11,648 (17.3) | 2803 (18.0) | 3345 (19.4) | 2832 (17.4) | 2668 (14.6) |
| ≥20 | 13,368 (19.9) | 2557 (16.5) | 3130 (18.2) | 3404 (20.8) | 4277 (23.4) |
| Geographic regions | |||||
| Urban | 6261 (9.3) | 1408 (9.1) | 1606 (9.3) | 1460 (9.0) | 1787 (9.8) |
| Suburb | 32,130 (47.7) | 7221 (46.5) | 8176 (47.5) | 8172 (50.1) | 8561 (46.9) |
| Rural | 28,686 (42.6) | 6877 (44.2) | 7404 (43.0) | 6604 (40.5) | 7801 (42.7) |
| Unknown | 249 (0.4) | 38 (0.2) | 33 (0.2) | 71 (0.4) | 107 (0.6) |
| Student (kindergartens, middle and high schools)* | 45,937 (68.2) | 11,351 (73.0) | 11,729 (68.1) | 10,825 (66.4) | 12,032 (65.9) |
| Healthcare workers | 526 (0.8) | 76 (0.5) | 131 (0.8) | 131 (0.8) | 188 (1.0) |
Significant trend from 2007 to 2010 compared with other groups (P < 0.001).
NA, not applicable.
From 2007 to 2010, the proportion and reported number of adults cases ≥20 years of age increased significantly from 16.5% (2557 cases) in 2007 to 23.4% (4277 cases) in 2010 (P < 0.001 for trend). Little change was observed in geographic distribution of the cases from 2007 to 2010, except some yearly fluctuation (Table 1). The proportions of cases that were adults was highest in urban, followed by suburban and rural areas (P < 0.001 for trend), and these proportions increased in all areas from 22.1%, 18.8%, 12.9% of all cases in 2007 to 32.9%, 25.2% and 19.2% in 2010, respectively (P < 0.001).
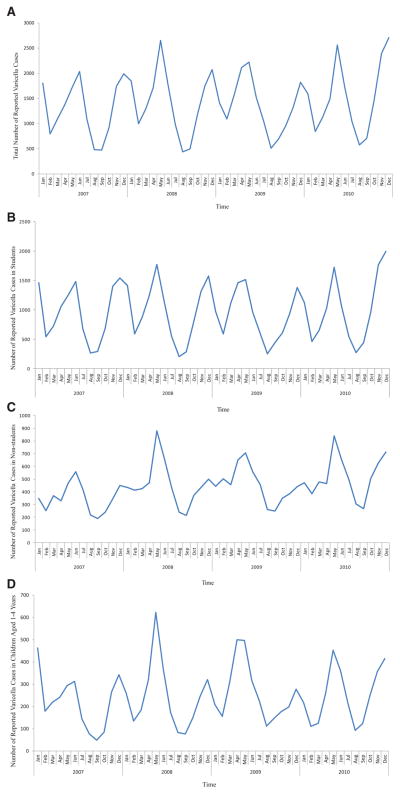
Varicella had a seasonal pattern with 2 incidence peaks (April to June and November to January) and 2 troughs (February and August to September) each year (Fig. 1A). The 2-peak seasonality was most prominent in cases reported among students, (Fig. 1B), and least prominent, with only 1 major peak per year in the nonstudent cases (Fig. 1C). From 2007 to 2010, there was no change in pattern of seasonality in any of the age groups, even in those 1–4 years of age (Fig. 1D).
FIGURE 1.
Monthly reported varicella cases in Beijing, 2007 to 2010. A, all reported cases; B, student cases only; C, nonstudent cases only; D, cases aged 1–4 years.
Varicella Outbreaks
A total of 303 outbreaks with 3845 cases (5.7% of total reported cases) were reported from 2007 to 2010. There was no significant change in the number of outbreaks or outbreak-related cases, the average size of the outbreaks or the proportion of outbreaks with <10 cases. Approximately 67.7% of the reported outbreaks occurred in elementary schools and correspondingly, more than half (61.4%–74.7%) of the outbreak cases were 5–9 years of age. The proportion of outbreak cases that were vaccinated was higher in kindergartens and elementary schools than in middle and high schools (65.8% versus 27.3%; P < 0.001); this proportion increased from 60.6% to 78.2% of kindergarten student cases and from 48.6% to 77.7% of elementary school student cases (P < 0.001 for both) during 2007 to 2010 (Fig. 2). In contrast, in outbreaks in middle and high schools, most cases were unvaccinated or had unknown vaccination status; however, the proportion of vaccinated cases increased from 23.8% in 2007 to 37.9% in 2010 (P = 0.02; Fig. 2). The proportion of outbreak cases with mild rash (<50 lesions) increased significantly from 65.8% in 2007 to 75.2% in 2010 in all outbreak cases (P < 0.001).
FIGURE 2.
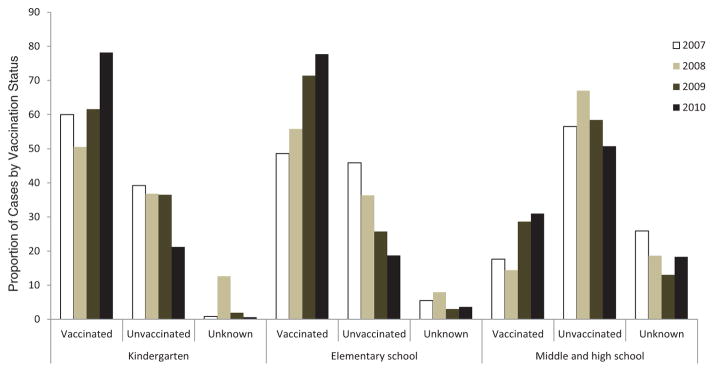
Changes in proportion of outbreak cases by vaccination status from 2007 to 2010 in different school settings.
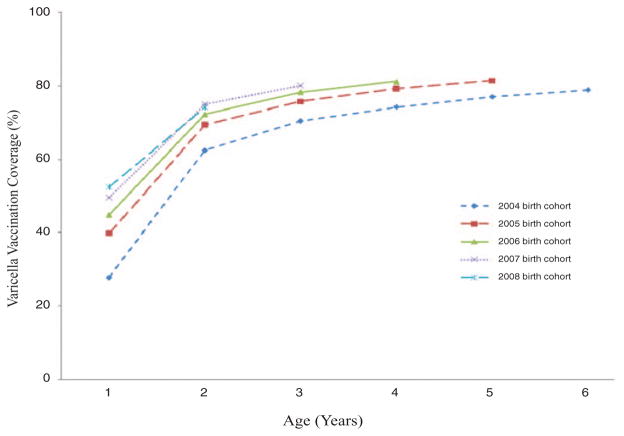
Single-dose Varicella Vaccination Coverage
Among children 1 year of age, vaccine coverage ranged from 27.9% in 2005 to 52.4% in 2009. By 2010, vaccine coverage was 79.2% in children 2–6 years of age (range: 74.1% for children 2 years of age to 81.5% for children 5 years of age; Fig. 3). The doses of privately purchased vaccines ranged from 161,560 doses in 2007 to 186,695 doses in 2010; however, doses for outbreak control decreased by 55% from 112,639 in 2007 to 50,288. Consequently, the proportion of all doses that were administered for outbreak control decreased from 41% in 2007 to 21% in 2010.
FIGURE 3.
Varicella vaccine coverage from 2007 to 2010 in children born between 2004 and 2008.
DISCUSSION
Using data collected from passive varicella surveillance and the Beijing immunization registry, our study provides the first description of current varicella epidemiology and coverage levels for varicella vaccine in Beijing. The unique biphasic pattern of disease is driven by school-aged children who have 2 breaks per year: the first trough in incidence in February coincides with the 4-week school break for Chinese New Year—a long enough time period to interrupt ongoing student transmission with the second trough during the summer when school is in recess, as described globally.1,2
Uptake of varicella vaccine in Beijing has been fairly rapid with moderately high 1-dose coverage (approximately 80%) among children 3–6 years of age by 2010. Factors that may contribute to this high coverage include the lower price of domestic vaccines in Beijing (25 US dollars for domestic vaccines, considerably cheaper than approximately 50 US dollars for Varilrix globally) and the fact that kindergartens and elementary schools recommend that parents consider vaccinating their children to avoid missing school and to reduce the likelihood of school closures during outbreaks.
In contrast to the experience in the United States where evidence of vaccine impact was present across the age spectrum,3 these levels of coverage among preschool children appear to have impacted varicella incidence among children aged 1–4 years, but have had little impact on overall disease incidence and on varicella seasonality as detected through this surveillance system. This may be due to inaccurate vaccine coverage assessment using registry data or less catch-up vaccination among school children who drive the disease seasonality. Limitations of the surveillance system with inability to track incidence in all age groups restricts our ability to interpret early signs of vaccine impact in other age groups and changing varicella epidemiology. Although the number and proportion of varicella cases among adults are increasing, incidence may not be increasing. These findings among adults may reflect the effect of rapidly changing population dynamics in Beijing. Beijing’s population has increased 42% over the past decade from 14 million in 2000 to 20 million in 2010 mainly due to migrants, predominantly young adults, from rural areas. The low income level of the migrants makes them less likely to get vaccinated before or after moving to Beijing. Supporting this explanation is the fact that the highest proportion of adult cases occurred in urban, followed by suburb and rural areas over this surveillance period; migrants are more likely to work in the urban/suburban areas. The proportion of varicella cases occurring in adults merits close follow-up as varicella has a higher rate of complications and mortality among adults. A government-funded vaccination program that includes catch-up vaccination for adults, as well as older children and adolescents, might be warranted.4–7 Vaccination of healthcare workers should be considered as a priority. The increasing proportion of breakthrough cases in the outbreaks reported, and reported outbreaks in schools with high single-dose coverage,8 indicate that a 2-dose vaccine regimen may need consideration for outbreak control or for routine childhood vaccination in Beijing.
In addition to lack of accurate denominator information that precluded examination of trends in age-specific incidence, other limitations should be considered when interpreting our data. Passive varicella surveillance in Beijing is likely to be incomplete, although it has proven to be adequate for monitoring trends of varicella in developed countries.9–11 Cases were not laboratory con-firmed, and laboratory confirmation becomes more important in monitoring varicella vaccination programs as more breakthrough cases with modified clinical presentations occur. Vaccination status and outcomes of cases including hospitalization and death were not recorded on the standard case investigation form, which limited our ability to examine trends in severe outcomes of varicella and to describe vaccination status of cases by age. Finally, vaccine coverage may be overestimated because unvaccinated children may be underrepresented in the immunization registry, or underestimated because doses administered for outbreak control were not included, and children with prior varicella were not excluded.
In summary, moderately high single-dose varicella vaccination coverage has been achieved in Beijing in young children and is resulting in declining varicella incidence in this age group. However, varicella is still common across the age spectrum suggesting much lower vaccine penetration in school children and other age groups. Improved surveillance and disease burden data are needed to guide and monitor vaccine policy decision making in Beijing. However, given that a considerable proportion of varicella cases are occurring among older adolescents and adults with the potential for an adverse shift in varicella epidemiology with declining varicella incidence in young children, a government-funded vaccination program that includes catch-up vaccination may need consideration.
Acknowledgments
The authors thank the clinical practitioners for timely reporting varicella cases and local health departments for outbreak investigations. The authors are also indebted to Dr. Stephanie Bialek for her scientific comments on the article.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention, US Department of Health and Human Services.
The authors have no funding or conflicts of interest to disclose.
References
- 1.Brisson M, Edmunds WJ, Law B, et al. Epidemiology of varicella zoster virus infection in Canada and the United Kingdom. Epidemiol Infect. 2001;127:305–314. doi: 10.1017/s0950268801005921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chang LY, Huang LM, Chang IS, et al. Epidemiological characteristics of varicella from 2000 to 2008 and the impact of nationwide immunization in Taiwan. BMC Infect Dis. 2011;11:352. doi: 10.1186/1471-2334-11-352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Seward JF, Watson BM, Peterson CL, et al. Varicella disease after introduction of varicella vaccine in the United States, 1995–2000. JAMA. 2002;287:606–611. doi: 10.1001/jama.287.5.606. [DOI] [PubMed] [Google Scholar]
- 4.Nguyen HQ, Jumaan AO, Seward JF. Decline in mortality due to varicella after implementation of varicella vaccination in the United States. N Engl J Med. 2005;352:450–458. doi: 10.1056/NEJMoa042271. [DOI] [PubMed] [Google Scholar]
- 5.Marin M, Zhang JX, Seward JF. Near elimination of varicella deaths in the US after implementation of the vaccination program. Pediatrics. 2011;128:214–220. doi: 10.1542/peds.2010-3385. [DOI] [PubMed] [Google Scholar]
- 6.Lopez AS, Zhang J, Brown C, et al. Varicella-related hospitalizations in the United States, 2000–2006: the 1-dose varicella vaccination era. Pediatrics. 2011;127:238–245. doi: 10.1542/peds.2010-0962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Seward JF, Marin M, Vázquez M. Varicella vaccine effectiveness in the US vaccination program: a review. J Infect Dis. 2008;197(suppl 2):S82–S89. doi: 10.1086/522145. [DOI] [PubMed] [Google Scholar]
- 8.Lu L, Suo L, Li J, et al. A varicella outbreak in a school with high one-dose vaccination coverage, Beijing, China. Vaccine. 2012;30:5094–5098. doi: 10.1016/j.vaccine.2012.05.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gabutti G, Rota MC, Guido M, et al. Seroepidemiology Group. The epidemiology of Varicella Zoster Virus infection in Italy. BMC Public Health. 2008;8:372. doi: 10.1186/1471-2458-8-372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pinot de Moira A, Nardone A ESEN2 group. Varicella zoster virus vaccination policies and surveillance strategies in Europe. Euro Surveill. 2005;10:43–45. [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. Decline in annual incidence of varicella--selected states, 1990–2001. MMWR Morb Mortal Wkly Rep. 2003;52:884–885. [PubMed] [Google Scholar]