Abstract
Each year, about six million children, including 1.5 million infants, in the United States undergo surgery with general anesthesia, often requiring repeated exposures. However, a crucial question remains of whether neonatal anesthetics are safe for the developing central nervous system (CNS). General anesthesia encompasses the administration of agents that induce analgesic, sedative, and muscle relaxant effects. Although the mechanisms of action of general anesthetics are still not completely understood, recent data have suggested that anesthetics primarily modulate two major neurotransmitter receptor groups, either by inhibiting N-methyl-D-aspartic acid (NMDA) receptors, or conversely by activating γ-aminobutyric acid (GABA) receptors. Both of these mechanisms result in the same effect of inhibiting excitatory activity of neurons. In developing brains, which are more sensitive to disruptions in activity-dependent plasticity, this transient inhibition may have longterm neurodevelopmental consequences. Accumulating reports from preclinical studies show that anesthetics in neonates cause cellular toxicity including apoptosis and neurodegeneration in the developing brain. Importantly, animal and clinical studies indicate that exposure to general anesthetics may affect CNS development, resulting in long-lasting cognitive and behavioral deficiencies, such as learning and memory deficits, as well as abnormalities in social memory and social activity. While the casual relationship between cellular toxicity and neurological impairments is still not clear, recent reports in animal experiments showed that anesthetics in neonates can affect neurogenesis, which could be a possible mechanism underlying the chronic effect of anesthetics. Understanding the cellular and molecular mechanisms of anesthetic effects will help to define the scope of the problem in humans and may lead to preventive and therapeutic strategies. Therefore, in this review, we summarize the current evidence on neonatal anesthetic effects in the developmental CNS and discuss how factors influencing these processes can be translated into new therapeutic strategies.
Keywords: Anesthesia, Neonate, Neuroprotection, Cytotoxicity, Cognitive Impairment, Neurogenesis
2. Introduction
In medicine, pain is one of the most primary symptoms to avoid or treat. Whether the therapeutic approach involves opioids, non-steroidal anti-inflammatory drugs (NSAIDs), such as aspirin, or in extreme cases, general anesthesia, the minimization of pain is always one of top priorities. This is the case both in humans and in animal models, in which the Institutional Animal Care and Use Committee (IACUC) explicitly requires the maximum reduction of pain in surgeries (Koch, 2003). It is not surprising that anesthesia has become such a prevalent component of the field of medicine, with a dedicated subset of specialists whose area of expertise is the administering and monitoring of anesthesia. In developed nations, general anesthesia comes standard with surgeries for both children and adult patients, although the decision to administer anesthesia to neonates remains contentious and situational. At least for adults, the complications are usually very minor, including nausea and vomiting in a small subset of patients, and mortalities only occur in 1:100,000 cases (Jenkins and Baker, 2003). The complications are far outweighed by the benefits of anesthesia, which spans beyond just analgesic effects. Anesthesia also encompasses sedation and muscle relaxation, which are both highly relevant both in and outside the realm of surgery. In neonates, the anesthetic effects may have long-term neurodevelopmental sequelae, which is the primary focus of this review.
Newborns receive anesthesia for a variety of reasons. Sometimes neonates need to undergo hernia repair or open chest surgery to fix congenital heart defects or pulmonary defects (Menghraj, 2012). Other times, newborn patients need to be anesthetized in order to be immobilized prior to receiving an MRI scan. Nevertheless, general anesthesia is usually reserved as a last resort in neonates. In fact, most neonatal males receiving circumcision surgeries remain unanesthetized. Aside from cost, general anesthesia carries potentially permanent drawbacks. There is an emerging body of evidence that indicates adverse long-term neurological effects of general anesthesia in the young susceptible brain (Flick et al., 2011; Flick et al., 2014; Ing et al., 2014; Sprung et al., 2012; Vutskits et al., 2012; Wilder et al., 2009). It is clear, both in animal models and to an extent through retrospective studies in human patients, that the effects of anesthesia are sensitively correlated with the age of exposure. In terms of behavior deficits, general anesthesia is most detrimental in the two extreme age groups, neonates/infants and the elderly. Both are similar in that they possess nervous systems that are more fragile. The developing brain is primed to undergo apoptosis in order to prune away redundant neurons and establish healthy neural circuitry, while the aged brain faces accelerated neurodegeneration due to senescence and buildup of deleterious byproducts, such as beta-amyloid (Aβ) protein. Both of these two groups are more susceptible to the neurodegenerative insults carried by general anesthesia, leading to widespread apoptotic neurodegeneration and learning impairments that are not otherwise observed in the adult age group (Culley et al., 2003; Erasso et al., 2013; Perouansky and Hemmings, 2009; Stratmann et al., 2009b). Interestingly, the effects are the stark opposite in the adult brain. Instead of inducing learning deficits, general anesthetics can actually reversibly enhance the learning function of 4–5 month old mice via an upregulation of the N-methyl-D-aspartic acid (NMDA) receptors, which promotes long-term potentiation (Rammes et al., 2009).
It is worth emphasizing that while animal studies have conclusively implicated the neurodegenerative effects related to early general anesthesia exposure, retrospective studies within human patient populations have not been able to conclusively and reproducibly demonstrate similar deficits. Furthermore, general anesthesia still confers many benefits, such as pain relief and muscle relaxation, which in some cases are essential to neonates undergoing surgery or medical imaging. This review aims to objectively compare the current body of evidence available for both animal and human studies in order to provide an updated assessment of the effects of general anesthesia on neurodevelopment, as well as to briefly provide the implications of these studies towards clinical practice.
3. The Mode of Action of General Anesthetics
3.1. Brief history of general anesthetics
The term “anesthesia” was first used in 1846 by Oliver Wendell Holmes, a Greek surgeon, to describe a patient who, after inhaling ether vapor, underwent surgery without any apparent suffering (Kissin, 1997; Nuland, 1989). General anesthesia is a combination of medicines that is inhaled or injected intravenously in order to induce a state of unconsciousness (also termed hypnosis) throughout the whole body (Grasshoff et al., 2005; Mashour et al., 2005). Under anesthesia, general anesthetics bring about a reversible loss of consciousness and loss of pain (analgesia) during the surgery or operative procedure. Additionally, general anesthesia also causes forgetfulness (amnesia), immobility, loss of control of autonomic responses (e.g. reflexes), and relaxation of muscles throughout the body. Volatile anesthetics, such as sevoflurane, isoflurane, and desflurane, induce a similar physiological response in the body as intravenous anesthetics (Sonner et al., 2003). The major differences between volatile and intravenous anesthetics are that volatile anesthetics are inhaled and generally possess a much shorter induction and emergence phase, resulting in faster recovery times. Furthermore, they demonstrate an ease of monitoring, making them the more common anesthetic agent of choice used in clinical practice. This is the case not only in adult patients, but in pediatric patients as well. Volatile anesthetics have been widely selected for induction of anesthesia in pediatric patients and for maintenance of anesthesia in adult patients (Palmer, 2013).
3.2. Mechanism of general anesthetics
Although anesthetics are commonly used in clinical practice, the mechanisms of action for induction of anesthesia are still not completely understood. The earliest theory for anesthetic mechanism is the lipid solubility/anesthetic potency (Meyer-Overton) correlation, in which the anesthetic potency of general anesthetics strongly correlates with their solubility in a solvent representing the hydrophobic interior of the cell membrane (Rudolph and Antkowiak, 2004). However, recent findings have suggested that there are the exceptions to the rule. For example, non-immobilizers with similar chemical structures and lipid solubility didn’t show general anesthetic properties (Koblin et al., 1994). In addition, enantiomers with the same solubility exert different anesthetic potencies (Franks and Lieb, 1991). These results have suggested that other mechanisms of action should be studied to provide a more thorough explanation for the induction of anesthetics.
In the last decade, the other promising mechanism for induction of anesthetics is the effect of anesthesia on neurotransmission in the central nervous system. Previous data have shown that two major neurotransmitter receptor classes are involved in induction of anesthetics. One is the glutamate receptor, NMDA receptor, which is known to mediate excitatory signals, while the other is the γ-aminobutyric acid (GABA) receptor, which is known to transmit inhibitory signals (Cechova and Zuo, 2006; Olsen and Li, 2011). Most classes of general anesthetics, such as volatile anesthetics and benzodiazepines and barbiturates, act by enhancing GABA receptor activity, in particular GABAA receptor. Specific sites (such as S270) of GABAA receptors can be a crucial factor to induce the anesthetics-mediated GABAA receptor activity (Nishikawa and Harrison, 2003). Additionally, GABAA receptor antagonists were able to reverse the effects of anesthesia, indicating that the GABAA receptor is a key receptor for the mechanism of action of anesthesia induction (Nelson et al., 2002).
GABAA receptor enhancement, however, explains only half of the story of general anesthesia. Evidence has proposed that NMDA receptors are also involved in the induction of anesthetics. Certain classes of general anesthetics, such as ketamine, can act as NMDA receptor antagonists (Arhem et al., 2003; Chiao and Zuo, 2014). The knockout or blockade of NMDA receptors reduced the anesthetic potency after exposure to nitrous oxide or ketamine (Harrison and Simmonds, 1985; Sato et al., 2005). Recent reports have shown that voltage-gated channels and neurotransmitter transporters can also be important factors for induction of anesthetics (Arhem et al., 2003; Lee et al., 2010; Sonner et al., 2003). Physiological factors such as sex and weight may additionally impact drug sensitivities and metabolism related to anesthesia induction (Mawhinney et al., 2013).
3.3. General anesthesia in neonates
Neonates undergoing a wide variety of procedures may require general anesthesia. There are two main considerations in the selection of general anesthetics: 1) hemodynamic control – generally volatile anesthetics or propofol are the preferred agents of choice, but if resuscitation is required, ketamine and opiates may be selected in order to protect cardiac output, and 2) postoperative pain relief, in which a combined regiment of regional and general anesthetics would be optimal. Volatile anesthetics, propofol, and ketamine are agents that are commonly administered to neonates. Propofol is a short-acting hypnotic agent that is administered intravenously and can be used for both induction and maintenance of general anesthesia. Propofol has largely supplanted the barbiturate sodium thiopental as a drug of choice for induction of anesthesia, due to its extremely rapid induction and recovery times. Benzodiazepines, such as midazolam and diazepam, are psychoactive drugs that are commonly used as anti-epileptics and anxiolytics, but are also used for their sedative purposes for anesthesia. Their primary mechanism of action is enhancement of GABAA receptor activity. Volatile anesthetics, such as isoflurane, desflurane, and sevoflurane, are inhalable agents that are commonly used amongst neonates and infants given their rapid induction and recovery times. They have been extensively studied in both retrospective analyses and animal models in order to assess its effects on the neuroapoptosis within the developing brain, and whether this leads to future long-term cognitive and learning deficits. Ketamine is commonly used for induction and maintenance of anesthesia, as well as for post-operative pain. Its primary mechanism of action is through noncompetitive antagonism of NMDA receptors, but it also acts weakly on opioid receptors (Kohrs and Durieux, 1998).
4. Differences between the Adult and Neonate Brain
4.1. The developing brain
The developing brain is in a dynamic state of establishing and strengthening neural connections; most of this neural network assembly occurs via activity-dependent mechanisms. The neural activity during periods of maximal synaptogenesis and neuronal pruning may contribute to the neural network organization (Ikonomidou et al., 1999; Poo, 2001). This process is especially prevalent during the developmental window in which axons are growing and finding appropriate targets, and corresponding synapses are being formed, including the late gestational phase to the early neonatal phase. The time points of these windows are different across species. In rodents, such as mice and rats, this range includes the late embryological phase until postnatal day 10–17 (P10–17) (Petit et al., 1988). In nonhuman primates, such as macaques, the most critical time window is from just before birth until around P5–7 (Malkova et al., 2006). In humans, this can range from late gestation until ~3 years of life (Dobbing and Sands, 1978). Even afterwards, children’s brains are still susceptible because of the ongoing synaptic plasticity during learning and memory formation, although the level of plasticity is not as high as during the first 2 years of life. Anesthetic agents interrupt this activity mainly through either N-methyl-D-aspartate (NMDA) glutamate receptor blockade or enhancement of the inhibitory gamma-aminobutyric acid (GABAA) receptor. As a result, the anomalous disruption of the neural activity causes widespread neuroapoptosis and chronic impairments in synaptogenesis later in life (Ikonomidou et al., 1999; Perouansky and Hemmings, 2009).
4.2. Cardiovascular limitations
Aside from the developing nervous system, there are major differences between neonates/infants and adults in other organ systems as well that are indirectly connected to brain function and development. The cardiovascular system is a prime example. In the adult heart, the cardiac output is highly flexible to adjust for changes in both the blood supply and energy demand of the body. The output can be increased by either intensifying heart contractility or accelerating heart rate. In the developing heart, however, the modulation of cardiac output is not as multimodal, due to the lower ventricular compliance and limited contractility of the neonatal heart (Barash, 2009). As a result, neonates depend more on the heart rate in order to modulate their cardiac output. This physiological difference makes neonates more susceptible to the global systemic depressant effects of general anesthesia. Newborns have more difficulties in compensating for the hypoxemia-induced slowed heart rate, or bradycardia, following general anesthesia induction. This could further exacerbate the neurotoxic effects associated with anesthesia, because the brain requires disproportionately more oxygenation than the rest of the body, and the sudden and prolonged reduction in perfusion may create adverse long-term effects on the developing brain.
4.3. Minimal Alveolar Concentration (MAC)
The MAC is an important consideration when administering inhalational anesthetics. The MAC is the equivalent of the anesthetic “potency” and is defined as the minimum concentration of anesthesia in the lung alveoli that will prevent movement in 50% of patients. There are many factors affecting MAC, including gender, age, and weight. In the extremely young age range, however, the MAC is exquisitely sensitive to age. In general, neonates have a lower MAC requirement than that of infants (Barash, 2009). In premature babies, the MAC is even lower (LeDez and Lerman, 1987). Because minimizing the amount and duration of anesthesia is a priority in neonates/infants, understanding the MAC at various ages is essential and will contribute to reducing neurodevelopmental delays or damage.
5. Neuroprotection and Cytotoxicity in Neonatal Anesthesia
5.1 Neuroprotective effects of neonatal anesthesia
In previous reports from adult animals and patients, more and more data have shown that general anesthetics have a neuroprotective effect through prevention or reduction of apoptosis, neurodegeneration, traumatic brain injury, and ischemic injury (Burchell et al., 2013; Schifilliti et al., 2010; Wells et al., 1963; Yokobori et al., 2013; Yu et al., 2010). Sevoflurane preconditioning protects neurons and blood-brain-barrier against brain ischemia (Anrather and Hallenbeck, 2013; Gidday, 2010; Wang et al., 2011; Yu et al., 2011). Isoflurane administration shows a strong neuroprotective effect in various adult stroke models including subarachnoid hemorrhage or middle cerebral artery occlusion (MCAo), although there were controversial data about the long-lasting effects (Altay et al., 2012; Kawaguchi et al., 2000; Sakai et al., 2007). The neuroprotective effect occurs both when anesthetics are administered before (preconditioning) or after stroke (postconditioning) (Anrather and Hallenbeck, 2013; Chen et al., 2011; Dezfulian et al., 2013).
However, in the neonatal brain, most papers suggest that only preconditioning administration of anesthetics, but not postconditioning, shows a neuroprotective effect in experimental strokes. In neonatal rats, isoflurane (1–1.5%) preconditioning (24 hr before stroke) exhibited a reduction in brain tissue loss via inhibition of nitric oxide synthase (NOS) or activation of P38 mitogen-activated protein kinases (Dobbing and Sands, 1973; Zhao and Zuo, 2004; Zheng and Zuo, 2004). Consistent with this result, another study showed that preconditioning with 1.5% isoflurane not only reduced brain mass but also improved motor function after stroke (Zhao et al., 2007). On the other hand, only one paper showed that prolonged exposure to Isoflurane ameliorated infarction severity in the rat pup model of neonatal hypoxia-ischemia (Chen et al., 2011). Although there have been minimal investigations into neuroprotection of general anesthetics in human pediatric population, many clinicians have accepted the data supporting beneficial effects of anesthetic preconditioning in stroke and heart attacks, and they are beginning to implement these strategies in the clinics for the pediatric population.
Various mechanisms have been proposed for the neuroprotection induced by anesthetic agents. For one, anesthetics reduce metabolic rate, resulting in better tolerance to ischemia by allowing for more efficient use of available oxygen and nutrients (Warner, 2000). In addition, anesthetics cause inhibition of glutamate receptors, modulation of calcium concentration, activation of mitochondrial adenosine-5′-triphosphate (ATP) sensitive potassium channels, and preservation of calcium/calmodulin dependent protein kinase II (CaMKII) levels (Bickler and Fahlman, 2006; Jevtovic-Todorovic et al., 1998; McMurtrey and Zuo, 2010).
5.2. Cytotoxic effects of neonatal anesthesia
Based on recently published papers, it is well-accepted that general anesthetics such as isoflurane, sevoflurane, ketamine, and propofol in neonates can lead to significant degeneration of developing neurons in various animals, including mice, rats, and non-human primates (Fredriksson et al., 2004; Fredriksson et al., 2007; Jevtovic-Todorovic et al., 2003; Loepke et al., 2009; Lu et al., 2010; Pesic et al., 2009; Rizzi et al., 2008; Satomoto et al., 2009; Shen et al., 2013; Slikker et al., 2007; Tao et al., 2014; Yon et al., 2005; Young et al., 2005; Zhang et al., 2014). Although the patterns of neonatal anesthesia-induced neurodegeneration are not consistently identified, the vulnerable areas have been implicated. They may include the primary visual cortex, temporal/somatosensory cortices, frontal cortex, and hippocampus (Brambrink et al., 2010; Rothstein et al., 2008). In the following sections, we will summarize the possible mechanisms of anesthesia-induced impairments of neuronal development.
5.2.1. NMDA and GABA in neonatal anesthesia toxicity
Given their critical roles in both neurodevelopment and the mechanism of action of general anesthesia, we will first review neonatal neurotoxicity related to GABA and NMDA receptors. As we mentioned above, GABA receptors and NMDA glutamate receptors are the major inhibitory and excitatory receptors, respectively. Previous findings have shown that some anesthetics such as ketamine are antagonists of the NMDA receptor (Liu and Sharp, 2012; Olney, 2002). Ketamine exposure caused a significant increase of NR1 expression and neuronal cell death in perinatal rhesus monkeys (Slikker et al., 2007). In rat pups, exposure to multiple injections of ketamine caused neuronal cell death in the frontal cortex and increased NR1 mRNA and proteins (Slikker et al., 2007). These findings suggests that antagonism of NMDA receptors may induce compensatory response such as upregulated NR1 expression and increased glutamate level during development, consequently leading to neuronal damage due to excitotoxicity. To further corroborate this theory, another study found that repeated exposure to isoflurane, a volatile anesthetic that enhances GABAA activity, during the neurodevelopmental stage increased glutamate levels in the posterior cortex, suggesting a compensatory response (Kulak et al., 2010).
During development, NMDA receptors play key roles in the establishment and maturation of synapses (Colonnese et al., 2005). Another report demonstrated that MK-801, another common antagonist of NMDA receptors, triggered widespread apoptotic neurodegeneration in the developing rat brain, suggesting that a tonic basal activity of the NMDA receptor and appropriate Ca2+ homeostasis are essential for neuronal survival in the developing brain (Ikonomidou et al., 1999). Taken together, these findings suggest that the anesthesia-induced neurodegeneration might be in part due to inhibition of NMDA receptor, especially during the critical stage in neonates in which activity-dependent synaptic plasticity mediates neuronal survival (Habas et al., 2006; Hack et al., 1993; Jiang et al., 2005; Lafon-Cazal et al., 2002).
GABA is typically an inhibitory neurotransmitter. However, in the immature nervous system of neonates, its properties are reversed and it acts as an excitatory neurotransmitter. Generally, GABAA receptor activation leads to an influx of Cl− into the cell, resulting in hyperpolarization. As mentioned above, the hyperpolarization via the regulation of GABA A receptor activation can lead to neuroprotection in stroke model. However, in the developing brain, activation of GABAA receptor results in Cl− efflux and depolarization of the neuron due to high intracellular concentration of Cl−. General anesthetics such as propofol and benzodiazepines can act as GABAA receptor agonist (Franks and Lieb, 1994). Consequently, GABAA receptor agonism leads to an increase of calcium concentration following excess depolarization in developmental stage, resulting in excitotoxicity-induced neurodegeneration.
5.2.2. Oxidative stress and mitochondrial damage in neonatal anesthesia toxicity
Another possible mechanism of anesthetic-induced neurotoxicity in neonates is an excess production of reactive oxygen species (ROS). It was recently reported that anesthesia containing a sedative dose of midazolam followed by a combination of nitrous oxide and isoflurane administration causes 30% upregulation of ROS, accompanied by a downregulation of the scavenging enzyme superoxide dismutase (Boscolo et al., 2013). An imbalance between mitochondrial fission with dynamin-related protein 1 (Drp-1) and fusion with mitofusin-2 (Mfn-2) leads to disturbed mitochondrial morphogenesis and then neurodegeneration. In addition, the impaired mitochondrial morphogenesis lead to increased autophagy activity, decreased mitochondrial density, and long-lasting disturbances in inhibitory synaptic neurotransmission (Sanchez et al., 2011). It was suggested that dysfunction of complex IV in the electron transport chain causes electron leakage from the mitochondria, thereby increasing ROS production, which reacts with macromolecules, including DNA, lipids, and protein, causing cellular injury. In another animal study, the synthetic ROS scavenger, EUK-134, effectively inhibits anesthesia-induced ROS production, resulting in decreased neurodegeneration associated with neonatal anesthetic exposure (Boscolo et al., 2012). Also, it was reported that exposure to sevoflurane (3%) for 6 hr increased cleaved caspase-3 and PARP, markers of apoptotic cell death, and 4-hydroxy-2-nonenal, a marker of lipid peroxidation and oxidative stress (Yonamine et al., 2013). A co-administration of 1.3% hydrogen gas and sevoflurane significantly reduced oxidative stress, resulting in reduced neurodegeneration. These results suggest that neonatal anesthetic exposure could lead to cellular damages through impaired mitochondrial morphogenesis, integrity, and function, leading to induction of oxidative stress during neurodevelopment, suggesting that mitochondrial impairment and subsequent ROS release may be key factors in anesthesia-induced neurodegeneration in the developing brain.
5.2.3. Inflammation in neonatal anesthesia toxicity
Inflammation may be a critical response in various brain pathologies (Chen et al., 2014b; Hall and Pennypacker, 2010; Hosaka and Hoh, 2014; Zhou et al., 2014). However, a relationship between neonatal inflammation and anesthesia has still not been thoroughly investigated. Accumulating data reveals that the commonly used anesthetic agents can induce neuroinflammation. However, although recent report showed that 3% sevoflurane for 2 h daily for 3 days induced cognitive impairment and neuroinflammation, most of studies were carried out in adult (Shen et al., 2013; Wu et al., 2012). In adult animals, tumor necrosis factor-α (TNF-α), interleukin-6 (IL-6), and IL-1β, the proinflammatory cytokines, are upregulated by isoflurane exposures. Furthermore, isoflurane induces activation of nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) through enhancement of NF-κB transcription. Interestingly, the isoflurane-induced NF-κB activation is cell-type dependent, occurring in microglia, but not neurons, indicating that isoflurane specifically targets microglia to induce inflammation (Zhang et al., 2013). Administration of isoflurane has been shown to increase the expression of the pro-inflammatory cytokine, IL-1β, in the cortex of rat pups (Lu et al., 2010). Sevoflurane, another volatile anesthetic, increases TNF-α levels, caspase activation, apoptosis, tau phosphorylation, glycogen synthase kinase 3β activation, and Aβ protein levels in an Alzheimer’s disease model of transgenic neonatal mice (Dong et al., 2009; Jiang and Jiang, 2015; Tao et al., 2014). Moreover, mice subjected to formalin-induced nociceptive pain along with prolonged anesthesia exposure produced significantly more apoptosis than prolonged anesthesia alone in neonates (Shu et al., 2012). However, some reports did not observe noticeable inflammation associated with anesthetics (El Azab et al., 2002; Helmy and Al-Attiyah, 2000; Lahat et al., 1992; Schneemilch and Bank, 2001). Although some of the data remain controversial, these findings should facilitate future studies of the potential effects of anesthetics on neuroinflammation in neonates, as well as the underlying mechanisms. Also, it remains to be determined if the inflammation is due to surgery alone or due to both surgery and anesthesia.
5.2.4. Calcium imbalance in neonatal anesthesia toxicity
Imbalance of calcium homeostasis can induce neuronal degeneration (Song and Yu, 2014). It is well known that preservation of Ca2+ is an important factor in maintenance and stability of cytoskeletal components, synapse formation, and production of neurotransmitters. Previous reports have shown that Ca2+ modulators such as MK-801, BAPTA (a Ca2+ chelator), and thapsigargin (an endoplasmic reticulum (ER) Ca2+-ATPase inhibitor) could lead to disruption of Ca2+ homeostasis, impacting on neuronal maturation (e.g. growth cone expansion, neurite length, and neurite complexity) (Ringler et al., 2008). In addition, the elevated neuronal cell death induced by ketamine may involve a compensatory upregulation of NMDA receptor subunits and subsequent overactivation of the glutamatergic system (Liu et al., 2011; Slikker et al., 2007; Wang et al., 2005). Increased glutamate release leads to greater intracellular Ca2+ levels in the neurons, resulting in excitotoxicity-mediated neuronal death (Choi, 1994; Ramanantsoa et al., 2013). Although there are a few reports in neonates, studies in adult have shown that volatile anesthetics including isoflurane and sevoflurane could activate Ca2+ ATPase by increasing membrane fluidity, inhibiting multiple voltage-gated Ca2+ calcium currents, and inducing significant release of Ca2+ from the ER, which increases cytosolic and mitochondrial Ca2+, all of which contributes to neuronal degeneration (Study, 1994; Yang et al., 2008; Zhang et al., 2008a).
In developing brains, the activation of GABAA receptor can depolarize the membrane potential, resulting in Ca2+ influx and enhance the current from GABAA receptor-mediated voltage-dependent Ca2+ channels (Allene and Cossart, 2010). Isoflurane leads to increase Ca2+ level by increasing GABAA receptor activity, resulting in activated caspase-3 levels and increased neuronal degeneration in the immature hippocampal pyramidal neurons (Zhao et al., 2011). In addition, isoflurane also increased cytosolic Ca2+ released from the ER via activation of inositol triphosphate (IP3), a downstream signal of GABA receptors (Wei et al., 2007). Taken together, these observations suggest that anesthesia-mediated calcium imbalance is an ionic mechanism underlying neonatal anesthesia toxicity.
5.2.5. Effect of general anesthesia on non-neuronal cells
While its neurotoxic effects on neurons in the cortex and hippocampus have been well-characterized, general anesthesia also impairs other cell types aside from neurons, such as oligodendrocytes and astrocytes (Brambrink et al., 2012; Culley et al., 2013; Ryu et al., 2014). Of these cells, astrocytes are particularly important as supportive cells for immature neurons during development. For one, they help release neurotrophins such as brain-derived neurotrophic factor (BDNF) that promote neuronal survival and synaptic strengthening. Furthermore, astrocytes provide structural support to mediate neuronal migration and axon growth. An interference of astrocyte function would result in abnormalities with neuronal maturation and neural circuitry assembly. Recent studies have shown astrocytes are not immune to anesthetic agents. Administration of isoflurane into co-cultures of astrocytes and neurons resulted in 30% reduction in axon growth, possibly as a result of decreased BDNF release (Brambrink et al., 2012). Furthermore, isoflurane disrupts the cytoskeletal network of astrocytes, which could also contribute to its dysfunction during brain development (Culley et al., 2013). Isoflurane also may impede axon growth and guidance, possibly through a GABAA receptor mediated mechanism (Mintz et al., 2013). Because many of the other anesthetics act through an almost identical mechanism of enhancing the activity of GABAA receptor, this finding may be extrapolated into other agents as well, such as barbiturates, benzodiazepines, and propofol.
5.2.6. Effects of combined administration of anesthetics
While many studies investigate anesthetic agents individually in order to maintain consistency and maximize simplicity of the experimental design, the reality in the clinics is that oftentimes different agents may be administered together in concert. For example, propofol may be used for induction, but an additional agent such as inhalable anesthetics may also be used. Therefore, in order to maximize face validity of anesthesia exposure, it may be important to assess combination regiments of general anesthesia. However, this makes comparisons of different groups more difficult, especially in animal models, in which the dosage and durations are all operated on a different scale than in humans. These studies, however, are particularly beneficial because they holistically assess the long-term neurodevelopmental effects of the combination regiment, which would have a stronger effect than the data possibly obtained from studying an individual agent.
Several studies have investigated the effects of inhalable anesthetics in conjunction with other anesthetics, such as the benzodiazepine midazolam, and propofol. Midazolam, propofol, and isoflurane are all common anesthetic agents that are administered to either neonates or infants. When administered to neonatal P7 rats, the rats developed significantly greater levels of apoptosis throughout the brain, as well as hippocampal synaptic dysfunction, and associated learning and memory impairments (Jevtovic-Todorovic et al., 2003). Another study used the combination of midazolam, isoflurane, and nitrous oxide, and also showed significant neurodegeneration, possibly as a result of mitochondrial instability and heightened autophagy activity (Sanchez et al., 2011). Midazolam, as well as other benzodiazepines, is commonly used as an anti-epileptic drug as well, but because of its sedative effects, it can be used to augment general anesthesia. Benzodiazepines, such as midazolam and diazepam, have been shown to affect neurodevelopment, including disruption of synaptic integrity and synaptic transmission and induction of apoptosis (Bittigau et al., 2002; Fredriksson et al., 2004; Fredriksson et al., 2007; Jevtovic-Todorovic et al., 2003; Young et al., 2005). However, the cognitive deficits are less characterized. When midazolam or other anti-epileptic drugs are given at the dosages necessary to control seizures, they seem to have long-term cognitive deficits and cause a decreased brain size. When midazolam is given to children prior to surgeries, however, they have much fewer negative behavioral changes in the first week following the procedure (Kain et al., 1999).
5.2.7. Other possible mechanisms in neonatal anesthesia toxicity
Recent report showed that neonatal mice pups exposed to ketamine decreased levels of phosphorylated extracellular signal-regulated protein kinases 1 and 2 (ERK1/2) and AKT, a serine/threonine protein kinase (Straiko et al., 2009). Also, sevoflurane administration resulted in greater hippocampal neuronal death, upregulation of Protein kinase C α (PKCα) and phosphorylated c-Jun N-terminal kinase (p-JNK), and downregulation of p-ERK and FOS protein levels in the hippocampus of P0, P7, and P14 rats, suggesting that sevoflurane induces developmental neurotoxicity in rats through regulation of PKCα, p-JNK, p-ERK, and FOS proteins (Wang et al., 2012). Phosphorylated ERK and AKT helps neuronal survival through activation of various factors such as CaMKII and BDNF and inactivation of glycogen synthase kinase 3β (GSK-3β) (De Koninck and Schulman, 1998; Lu et al., 2006). These results indicate that some anesthetics may downregulate factors that mediate neuronal survival in developmental stage, resulting in premature neuronal degeneration.
We and other groups have shown important roles of hypoxia inducible factor-1α (HIF-1α) as a homeostatic pathway against hypoxic ischemic injury (Ogle et al., 2012; Souvenir et al., 2014; Wang and Semenza, 1993, 1995). When HIF-1α is unhydroxylated, the stable protein accumulates, and translocates to the nucleus, resulting in promotion of cell survival, angiogenesis, anaerobic metabolism, and neurogenesis (Forsythe et al., 1996; Gidday, 2010; Semenza, 1994; Yu et al., 2013). However, during normal oxygen perfusion, prolyl hydroxylase (PHD) constitutively hydroxylates HIF-1α on two conserved proline residues (Epstein et al., 2001), mediating the interaction of HIF-1α with the E-3 ubiquitin ligase von Hippel Lindau (Ivan et al., 2001; Jaakkola et al., 2001). Therefore, under normal oxygen tension, hydroxylated HIF-1α is poly-ubiquitinated and targeted for proteasomal degradation (Sutter et al., 2000). Isoflurane increases HIF-1α expression in primary cultured neurons and in the developing rat brain (Jiang et al., 2012). In that study, HIF-1α knockdown prevented neural degeneration via inhibition of isoflurane-induced increase in cleaved caspase-3 and poly-(ADP-ribose) polymerase (PARP).
6. Behavioral and Cognitive Impairments Associated with Neonatal Anesthesia
The following sections will focus on these four major groups of anesthetics that are commonly administered to neonates and infants: volatile anesthetics, ketamine, benzodiazepines, and propofol. We will review current literature about these agents to assess their neurodevelopmental effects, including learning, memory, and social behavior.
6.1. Learning and memory deficits and underlying cellular mechanism
Neonatal mice or rats are typically defined as newborn mice/rats that are within the postnatal day 10 range. Most neonatal models of anesthesia exposure utilize P7 mice or rats in order to represent the state of maximal synaptogenesis and susceptibility within the developing brain. In animal models, isoflurane induces widespread apoptosis in many areas of the developing brain, leading to a wide array of phenotypic effects, from cognitive deficits to social abnormalities (Istaphanous et al., 2013; Johnson et al., 2008; Kong et al., 2012; Sanchez et al., 2011). In studies investigating the effects of isoflurane in P7–14 rats, it is clear that both the duration of exposure and frequency of exposure play a critical role in determining the extent of neurodevelopmental damage. For example, in an experiment using P7 rats, 4-hr exposure to isoflurane was needed to develop impairments in spatial reference memory and spatial working memory (Stratmann et al., 2009a). However, if the exposure frequency was increased from a one-time 2-hr exposure to four repetitive sessions of 2-hr exposures, then the pups developed learning and memory deficits (Murphy and Baxter, 2013). The frequency appears to be more important than the duration, because a 4-time exposure of just 35-min duration was enough to induce deficits in object recognition and associative memory in P14 rats (Zhu et al., 2010).
Aside from isoflurane, desflurane and sevoflurane are two other commonly used inhalational anesthetic agents, and both of them have been implicated to cause apoptosis in mouse and rat pups (Kodama et al., 2011; Lee et al., 2014; Zhang et al., 2008b; Zhou et al., 2012). In fact, desflurane has been shown to induce more robust levels of apoptosis and working memory deficits than isoflurane or sevoflurane (Kodama et al., 2011). The cognitive profiles of the animals reflect this difference in cellular damage. When comparing isoflurane and sevoflurane, desflurane exposure resulted in a much greater immediate deficit in cognitive function as assessed by performance on a working memory task (Kodama et al., 2011). General anesthesia also affects fear and associative memory. Exposure to isoflurane or sevoflurane resulted in suppression of the fear response despite training to either tone or context (Dutton et al., 2002; Satomoto et al., 2009; Stratmann et al., 2009b). More specifically, isoflurane induces anterograde amnesia and interferes with the animal’s ability to form novel memories (Dutton et al., 2002).
Ketamine is a common general anesthetic that is administered to neonates and infants intravenously, and displays similar dosage-, duration-, and frequency-dependent apoptotic effects as inhalable anesthetics (Hayashi et al., 2002; Scallet et al., 2004; Soriano et al., 2010; Zou et al., 2009). In P7 rats, the frequency of administration again appears to be the most important factor. In one study, a single dosage of 25, 50, or 75 mg/kg of ketamine was not sufficient to induce differences in apoptosis, but repeated injections (every 90 min over 9 hr) resulted in frequency-dependent increases in neurodegeneration (Hayashi et al., 2002). Another study found that repeated doses of just 20 mg/kg were sufficient to increase levels of neurodegeneration (Scallet et al., 2004). In P5 macaques, the duration threshold for increasing apoptosis appears to be between 3–9 hr of continuous ketamine infusion. When the duration exceeded this range, significantly greater levels of apoptosis were observed in the frontal cortex.
Importantly, the cellular degenerative effects may translate into long-term behavioral changes as well. P10 mice exposed to ketamine displayed disrupted spontaneous activity and decreased learning into adulthood (Fredriksson et al., 2007; Viberg et al., 2008). Another study showed that P10 mouse pups display the most profound degeneration in the parietal cortex following ketamine administration, and later performed markedly worse on acquisition learning and retention memory tasks such as the radial arm maze-learning task and the circular swim maze-learning task (Fredriksson et al., 2004). These cognitive deficits were also observed in non-human primates. Both macaques on gestational day 120–123 and P5–6 macaques received a single dose of ketamine displayed deficits in operant training learning, as well as color and position tasks, and had slower response speeds as adults (Paule et al., 2011).
General anesthesia may show impacts on activity-dependent synaptogenesis and neurogenesis. For one, anesthetics modulate excitability, albeit only on the order of hours, via glutamatergic or GABAergic pathways. If they are administered during the critical period during neural development in which glutamatergic/GABAergic signaling are crucial for the synthesis and strengthening of synapses, or activity-dependent plasticity, then anesthetics may have an effect on neural circuitry assembly. In fact, certain general anesthetics, such as barbiturates, ketamine, and propofol, can increase dendritic budding and synaptogenesis in developing pyramidal neurons, possibly through a homeostatic plasticity mechanism (De Roo et al., 2009). Although the behavioral effects of these synaptic enhancements are unclear, it is possible that having too many spines and synapses may interfere with the synaptic pruning and strengthening that occurs during the early developmental phase. However, other anesthetic agents, such as halothane, can impair neural circuitry assembly by decrease the number of synaptic inputs, and stalling the timeline of synaptogenesis (Quimby et al., 1974; Uemura et al., 1985). Certain volatile anesthetics cause an adverse effect on synaptogenesis, and this may be partially due to a rapid and pathological increase in dendritic spine density, which could interfere with synaptic contact formation (Briner et al., 2010). Isoflurane also results in impairments in mitochondrial morphology and membrane integrity, which could contribute both to increased apoptosis, as well as reduced synaptic transmission (Sanchez et al., 2011). Finally, isoflurane may adversely affect neuroregeneration, by decreasing the neural stem cell pool and attenuating neurogenesis (Stratmann et al., 2009b). While the mechanism is not elucidated, ion channel activity is critical for proper neural stem cell proliferation and differentiation (Chen et al., 2014a). Therefore, disruption of excitatory channels may interfere with neurogenesis during development, as well as possibly more delayed effects, such as learning and memory deficits later in life.
6.2. Abnormalities in social memory and social activity
In addition to the learning and memory impairments associated with neonatal anesthesia, more investigations have begun to probe into the associated aberrances in social memory and behavior as well. A 6-hr exposure of neonatal mice to sevoflurane (3%) caused not only learning deficits but also abnormal social behaviors, such as impaired social memory and decreased interaction in spite of normal olfactory activity (Satomoto et al., 2009). Consistent with this finding, a recent in vivo animal study showed that 6 hr sevoflurane exposure in the hippocampus of P5 mice caused the reduced expressions of oxytocin and arginine vasopressin levels, which are known to be key regulators of social activity (Heinrichs and Domes, 2008; Zhou et al., 2014). These results demonstrated that anesthesia causes impaired social recognition memory formation and social discrimination ability in juvenile mice.
7. The Plausible Link between Cellular Neurotoxicity and Cognitive Impairments
If the neuronal death itself were directly linked to cognitive impairment, behavioral impairment would be expected immediately after anesthesia-mediated neuronal death. However, animal studies have shown that when anesthesia-induced cell death was observed, cognitive deficits did not occur until about 6 weeks after the exposure (Jevtovic-Todorovic et al., 2003; Satomoto et al., 2009; Stratmann et al., 2009b). Interestingly, these behavioral deficits, including social behavior and spatial learning and memory persist until at least 8 months of age (Fredriksson et al., 2004; Jevtovic-Todorovic et al., 2003; Satomoto et al., 2009; Stratmann et al., 2009a; Stratmann et al., 2009b). These findings might imply that there may be a disconnection between the anesthesia-induced neuronal death and the delayed neurocognitive dysfunction. Alternatively and perhaps more likely, the cell death-triggered consequent events are more directly associated with behavioral deficits. One emerging theory is that anesthesia may affect the stem cell pool and endogenous neurogenesis, which would create a late-onset and progressive neurocognitive decline. This may be why the primary cognitive deficit associated with neonatal anesthesia exposure is learning and memory. Children and adults require the constant supply of new neurons in the hippocampus to establish new memories (Schmidt-Hieber et al., 2004). These neurons come from the neural stem cell niche of the subgranular zone, the hippocampal dentate gyrus, and early anesthesia exposure may have long-term detrimental effects on this neurogenesis (Zhu et al., 2010).
Recent findings have provided some evidence that neuronal death may not be a prerequisite for delayed neurocognitive impairment (Stratmann et al., 2009a). They administered isoflurane in P7 rats for 1, 2, or 4 hr and then measured cell death in the brain 12 hr after anesthesia, and then assessed neurocognitive outcomes at 8 weeks after anesthesia. They found that a minimum of 2 hr of isoflurane exposure was required to induce cytotoxicity, but this was not enough to produce a neurocognitive deficit. Only after 4 hr of isoflurane exposure was a neurocognitive deficit observed in spatial reference memory and spatial working memory tests. Others showed that prolonged isoflurane or midazolam exposure caused neuronal death but not spatial memory deficits (Fredriksson et al., 2004; Loepke et al., 2009). A 6-hr isoflurane exposure in P7 mice did not lead to decreased neuronal density 3 months after anesthesia although neonatal neuronal death occurred (Loepke et al., 2009). It is likely that the ultimate functional consequence of anesthetic exposure is largely dependent on the balance between neuronal cell death and neurogenesis. In the event that sufficient neurogenetic activities remain sufficient to replace dead cells, the long-term behavioral development may be corrected or not be affected.
Recent clinical studies have shown that anesthetic exposure before 4 years old could affect the development of reading, writing, and math skills, as well as increase the risk of learning disabilities (Wilder et al., 2009). These findings suggest that further investigations should be conducted to study the link between anesthesia-induced neurotoxicity and delayed functional abnormalities. However, a causal connection between brain cell death and delayed neurocognitive impairment remains unclear (Stratmann, 2011).
8. Potential Therapeutic Strategies and Implication in Clinical Stage
One of the benefits of animal models is that they help us to probe into the mechanisms of neurotoxicity, due to the wide array of cellular and molecular biological techniques available. This can improve our understanding of the pathophysiology of anesthesia-associated neurodevelopmental deficits and provide clinical targets for future treatments. For the translational purpose, however, the animal models do not have optimal face validity, due to the differences in the developmental timeline between rodents and primates/humans (Dobbing and Sands, 1978; Malkova et al., 2006; Petit et al., 1988). Furthermore, there are significant differences in anatomy, anatomical regionalization, synaptic density, spine density, and the tissue level neural networks; all of which are much more sophisticated and complex in humans.
Although general anesthesia has been clearly shown to induce a frequency- and duration-dependent neurotoxicity, whether or not this translates into cognitive impairments in humans is inconclusive. Recently there has been a surge of retrospective and preclinical studies into the effects of general anesthesia in neonates. However, by virtue of the majority of these studies being retrospective, the outcomes are not preemptively chosen by the investigator, and so the findings may not be as meaningful as blind, randomized, controlled studies. Furthermore, many of these studies employ different modes of cognitive assessments, from standardized tests, to academic achievements, to neuropsychological abnormalities, such as personality disorders. The lack of a consistent and universal assessment of neurodevelopment makes it difficult to interpret the results of the studies with respect to clinical application. Additionally, sometimes the results may be ambiguous. For example, one clinical study showed that anesthesia exposure prior to the age of three resulted in no differences in academic performance (Hansen et al., 2011). However, exposure does lead to an increased risk of deficit on a neuropsychological clinical outcome measure (Ing et al., 2014). There were other studies that resulted in negative findings between anesthesia exposure and proper neurodevelopment, but that may because the studies implemented broad assessments of learning, such as group test of academic performance (Flick et al., 2011; Ing et al., 2014). One study did find that early anesthesia exposure lead to a significantly greater risk of learning disabilities. Another confounding factor in these studies, despite being paired or sibling-matched, is that the anesthesia exposure group always receives a surgery, such as hernia repair (Hansen et al., 2011). The effects of the surgery, both immediate and psychological, may play an important role in the developmental outcome of the child.
The inconsistencies of the results of animal studies vs. the retrospective studies calls for a need to conduct more controlled investigations into the effects of early anesthesia exposure in humans. There are several ongoing clinical trials that may provide more conclusive results towards corroborating the results of the animal studies, as well as for determining the course of action for future neonatal anesthesia projects. These studies include the Pediatric Anesthetic NeuroDevelopmental Assessment (PANDA), the Mayo Safety in Kids study (MASK), and the General Anesthesia and Spinal (GAS) study. These studies will provide the first set of neurocognitive and behavioral data that will be prospectively collected, as well as provide more information on the age ranges of greatest susceptibility and the importance of toxicity factors, such as frequency and duration. The results of these trials will be critical for developing appropriate guidelines for assessing developmental benchmarks and neurological deficits, as well as towards implementing appropriate protocols for anesthesia administration in neonates and infants.
9. Summary and Conclusion
The development of anesthetics has revolutionized modern medicine. Tens of millions of surgeries are performed under anesthesia every year in the US alone, approximately six million of which are on pediatric populations (DeFrances et al., 2007). Anesthetics can prolong the quality and longevity of human life by enabling increasingly complex surgeries and procedures. However, over recent years, the safety has come under contention after new evidence revealed that anesthesia exposure in immature animals can cause neuronal degeneration, long-lasting cognitive and behavioral deficiencies (Cao et al., 2012; Jevtovic-Todorovic et al., 2003). This has led to an urgent movement to try to resolve this question and develop new measures to handle neonatal anesthesia in clinics. Current data agree that general anesthetics can cause apoptotic neuronal cell death in the developing brain, while the association or the mediator between the cytotoxicity and the long-term, long-lasting cognitive and behavioral deficiencies is unclear. Finally, a few papers have demonstrated the detrimental effects of neonatal anesthesia on endogenous neurogenesis and stem cell survival, and this may provide a mechanism to fill the knowledge gap between the acute cytotoxicity of anesthesia and the delayed neurological impairments. The observations in animal models and its relevance to humans also remain unclear and require substantial investigative effort. The upcoming results from several clinical trials will help to improve the understanding of the effects of general anesthetics in young population and the improvement of clinical application of general anesthetic.
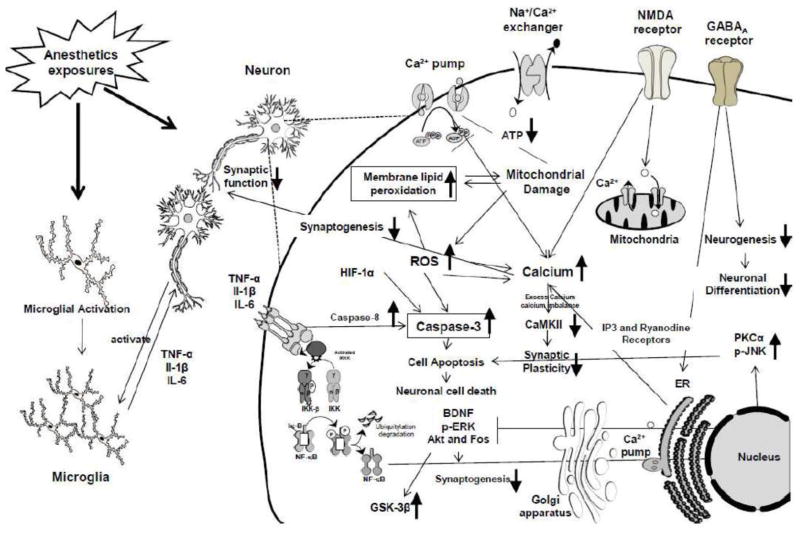
Figure 1. Schematic diagram on possible mechanisms in neonatal anesthesia toxicity.
Abbreviation: ATP: Adenosine triphosphate; ROS: Reactive oxygen species; NMDA receptor: N-methyl-D-aspartate; GABAA receptor: Gamma-aminobutyric acid type A receptor; TNF-α: Tumor necrosis factor-α; IL-1β: Interleukin-1β; IL-6: Interleukin-6; IP3 receptor: Inositol triphosphate receptor; BDNF: Brain-derived; Akt: Phosphorylated serine/threonine-specific protein kinase; CaMK II: Calcium/calmodulin-dependent Protein Kinase II; ERK: extracellular signal-regulated protein kinase; PKC: Protein kinase C; p-JNK: Phosphorylated c-Jun N-terminal kinase; GSK-3β: Glycogen synthase kinase 3β; IKK: IκB kinase; NF-κB: nuclear factor kappa-light-chain-enhancer of activated B cells); ER: endoplasmic reticulum; Ca2+: Calcium ion. ↑: increase; ↓: decrease; ┤: block or inhibit.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Allene C, Cossart R. Early NMDA receptor-driven waves of activity in the developing neocortex: physiological or pathological network oscillations? J Physiol. 2010;588:83–91. doi: 10.1113/jphysiol.2009.178798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altay O, Suzuki H, Hasegawa Y, Caner B, Krafft PR, Fujii M, Tang J, Zhang JH. Isoflurane attenuates blood-brain barrier disruption in ipsilateral hemisphere after subarachnoid hemorrhage in mice. Stroke. 2012;43:2513–2516. doi: 10.1161/STROKEAHA.112.661728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anrather J, Hallenbeck JM. Biological networks in ischemic tolerance - rethinking the approach to clinical conditioning. Transl Stroke Res. 2013;4:114–129. doi: 10.1007/s12975-012-0244-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arhem P, Klement G, Nilsson J. Mechanisms of anesthesia: towards integrating network, cellular, and molecular level modeling. Neuropsychopharmacology : official publication of the American College of Neuropsychopharmacology. 2003;28(Suppl 1):S40–47. doi: 10.1038/sj.npp.1300142. [DOI] [PubMed] [Google Scholar]
- Barash PG, Cullen BF, Stoelting RK, Calahan MK, Stock MC. Clinical Anesthesia. 6. Wolters Kluwer Lippincott Williams & Wilkins; Philadelphia: 2009. [Google Scholar]
- Bickler PE, Fahlman CS. The inhaled anesthetic, isoflurane, enhances Ca2+-dependent survival signaling in cortical neurons and modulates MAP kinases, apoptosis proteins and transcription factors during hypoxia. Anesth Analg. 2006;103:419–429. doi: 10.1213/01.ane.0000223671.49376.b2. table of contents. [DOI] [PubMed] [Google Scholar]
- Bittigau P, Sifringer M, Genz K, Reith E, Pospischil D, Govindarajalu S, Dzietko M, Pesditschek S, Mai I, Dikranian K, Olney JW, Ikonomidou C. Antiepileptic drugs and apoptotic neurodegeneration in the developing brain. Proc Natl Acad Sci U S A. 2002;99:15089–15094. doi: 10.1073/pnas.222550499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boscolo A, Milanovic D, Starr JA, Sanchez V, Oklopcic A, Moy L, Ori CC, Erisir A, Jevtovic-Todorovic V. Early exposure to general anesthesia disturbs mitochondrial fission and fusion in the developing rat brain. Anesthesiology. 2013;118:1086–1097. doi: 10.1097/ALN.0b013e318289bc9b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boscolo A, Starr JA, Sanchez V, Lunardi N, DiGruccio MR, Ori C, Erisir A, Trimmer P, Bennett J, Jevtovic-Todorovic V. The abolishment of anesthesia-induced cognitive impairment by timely protection of mitochondria in the developing rat brain: the importance of free oxygen radicals and mitochondrial integrity. Neurobiol Dis. 2012;45:1031–1041. doi: 10.1016/j.nbd.2011.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brambrink AM, Back SA, Riddle A, Gong X, Moravec MD, Dissen GA, Creeley CE, Dikranian KT, Olney JW. Isoflurane-induced apoptosis of oligodendrocytes in the neonatal primate brain. Ann Neurol. 2012;72:525–535. doi: 10.1002/ana.23652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brambrink AM, Evers AS, Avidan MS, Farber NB, Smith DJ, Zhang X, Dissen GA, Creeley CE, Olney JW. Isoflurane-induced neuroapoptosis in the neonatal rhesus macaque brain. Anesthesiology. 2010;112:834–841. doi: 10.1097/ALN.0b013e3181d049cd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briner A, De Roo M, Dayer A, Muller D, Habre W, Vutskits L. Volatile anesthetics rapidly increase dendritic spine density in the rat medial prefrontal cortex during synaptogenesis. Anesthesiology. 2010;112:546–556. doi: 10.1097/ALN.0b013e3181cd7942. [DOI] [PubMed] [Google Scholar]
- Burchell SR, Dixon BJ, Tang J, Zhang JH. Isoflurane provides neuroprotection in neonatal hypoxic ischemic brain injury. J Investig Med. 2013;61:1078–1083. doi: 10.231/JIM.0b013e3182a07921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao L, Li L, Lin D, Zuo Z. Isoflurane induces learning impairment that is mediated by interleukin 1beta in rodents. PloS one. 2012;7:e51431. doi: 10.1371/journal.pone.0051431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cechova S, Zuo Z. Inhibition of glutamate transporters increases the minimum alveolar concentration for isoflurane in rats. Br J Anaesth. 2006;97:192–195. doi: 10.1093/bja/ael152. [DOI] [PubMed] [Google Scholar]
- Chen D, Yu SP, Wei L. Ion channels in regulation of neuronal regenerative activities. Transl Stroke Res. 2014a;5:156–162. doi: 10.1007/s12975-013-0320-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen H, Burris M, Fajilan A, Spagnoli F, Tang J, Zhang JH. Prolonged exposure to isoflurane ameliorates infarction severity in the rat pup model of neonatal hypoxia-ischemia. Transl Stroke Res. 2011;2:382–390. doi: 10.1007/s12975-011-0081-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen S, Yang Q, Chen G, Zhang JH. An Update on Inflammation in the Acute Phase of Intracerebral Hemorrhage. Transl Stroke Res. 2014b doi: 10.1007/s12975-014-0384-4. [DOI] [PubMed] [Google Scholar]
- Chiao S, Zuo Z. A double-edged sword: volatile anesthetic effects on the neonatal brain. Brain Sci. 2014;4:273–294. doi: 10.3390/brainsci4020273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi DW. Glutamate receptors and the induction of excitotoxic neuronal death. Prog Brain Res. 1994;100:47–51. doi: 10.1016/s0079-6123(08)60767-0. [DOI] [PubMed] [Google Scholar]
- Colonnese MT, Zhao JP, Constantine-Paton M. NMDA receptor currents suppress synapse formation on sprouting axons in vivo. J Neurosci. 2005;25:1291–1303. doi: 10.1523/JNEUROSCI.4063-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Culley DJ, Baxter M, Yukhananov R, Crosby G. The memory effects of general anesthesia persist for weeks in young and aged rats. Anesth Analg. 2003;96:1004–1009. doi: 10.1213/01.ANE.0000052712.67573.12. table of contents. [DOI] [PubMed] [Google Scholar]
- Culley DJ, Cotran EK, Karlsson E, Palanisamy A, Boyd JD, Xie Z, Crosby G. Isoflurane affects the cytoskeleton but not survival, proliferation, or synaptogenic properties of rat astrocytes in vitro. Br J Anaesth. 2013;110(Suppl 1):i19–28. doi: 10.1093/bja/aet169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Koninck P, Schulman H. Sensitivity of CaM kinase II to the frequency of Ca2+ oscillations. Science. 1998;279:227–230. doi: 10.1126/science.279.5348.227. [DOI] [PubMed] [Google Scholar]
- De Roo M, Klauser P, Briner A, Nikonenko I, Mendez P, Dayer A, Kiss JZ, Muller D, Vutskits L. Anesthetics rapidly promote synaptogenesis during a critical period of brain development. PloS one. 2009;4:e7043. doi: 10.1371/journal.pone.0007043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeFrances CJ, Cullen KA, Kozak LJ. National Hospital Discharge Survey: 2005 annual summary with detailed diagnosis and procedure data. Vital Health Stat Series 13, Data from the National Health Survey. 2007:1–209. [PubMed] [Google Scholar]
- Dezfulian C, Garrett M, Gonzalez NR. Clinical application of preconditioning and postconditioning to achieve neuroprotection. Transl Stroke Res. 2013;4:19–24. doi: 10.1007/s12975-012-0224-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dobbing J, Sands J. Quantitative growth and development of human brain. Arch Dis Child. 1973;48:757–767. doi: 10.1136/adc.48.10.757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dobbing J, Sands J. Head circumference, biparietal diameter and brain growth in fetal and postnatal life. Early Hum Dev. 1978;2:81–87. doi: 10.1016/0378-3782(78)90054-3. [DOI] [PubMed] [Google Scholar]
- Dong Y, Zhang G, Zhang B, Moir RD, Xia W, Marcantonio ER, Culley DJ, Crosby G, Tanzi RE, Xie Z. The common inhalational anesthetic sevoflurane induces apoptosis and increases beta-amyloid protein levels. Arch Neurol. 2009;66:620–631. doi: 10.1001/archneurol.2009.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutton RC, Maurer AJ, Sonner JM, Fanselow MS, Laster MJ, Eger EI., 2nd Isoflurane causes anterograde but not retrograde amnesia for pavlovian fear conditioning. Anesthesiology. 2002;96:1223–1229. doi: 10.1097/00000542-200205000-00027. [DOI] [PubMed] [Google Scholar]
- El Azab SR, Rosseel PM, De Lange JJ, van Wijk EM, van Strik R, Scheffer GJ. Effect of VIMA with sevoflurane versus TIVA with propofol or midazolam-sufentanil on the cytokine response during CABG surgery. Eur J Anaesthesiol. 2002;19:276–282. doi: 10.1017/s0265021502000443. [DOI] [PubMed] [Google Scholar]
- Epstein AC, Gleadle JM, McNeill LA, Hewitson KS, O’Rourke J, Mole DR, Mukherji M, Metzen E, Wilson MI, Dhanda A, Tian YM, Masson N, Hamilton DL, Jaakkola P, Barstead R, Hodgkin J, Maxwell PH, Pugh CW, Schofield CJ, Ratcliffe PJ. C. elegans EGL-9 and mammalian homologs define a family of dioxygenases that regulate HIF by prolyl hydroxylation. Cell. 2001;107:43–54. doi: 10.1016/s0092-8674(01)00507-4. [DOI] [PubMed] [Google Scholar]
- Erasso DM, Camporesi EM, Mangar D, Saporta S. Effects of isoflurane or propofol on postnatal hippocampal neurogenesis in young and aged rats. Brain Res. 2013;1530:1–12. doi: 10.1016/j.brainres.2013.07.035. [DOI] [PubMed] [Google Scholar]
- Flick RP, Katusic SK, Colligan RC, Wilder RT, Voigt RG, Olson MD, Sprung J, Weaver AL, Schroeder DR, Warner DO. Cognitive and behavioral outcomes after early exposure to anesthesia and surgery. Pediatrics. 2011;128:e1053–1061. doi: 10.1542/peds.2011-0351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flick RP, Nemergut ME, Christensen K, Hansen TG. Anesthetic-related neurotoxicity in the young and outcome measures: the devil is in the details. Anesthesiology. 2014;120:1303–1305. doi: 10.1097/ALN.0000000000000249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forsythe JA, Jiang BH, Iyer NV, Agani F, Leung SW, Koos RD, Semenza GL. Activation of vascular endothelial growth factor gene transcription by hypoxia-inducible factor 1. Mol Cell Biol. 1996;16:4604–4613. doi: 10.1128/mcb.16.9.4604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franks NP, Lieb WR. Stereospecific effects of inhalational general anesthetic optical isomers on nerve ion channels. Science. 1991;254:427–430. doi: 10.1126/science.1925602. [DOI] [PubMed] [Google Scholar]
- Franks NP, Lieb WR. Molecular and cellular mechanisms of general anaesthesia. Nature. 1994;367:607–614. doi: 10.1038/367607a0. [DOI] [PubMed] [Google Scholar]
- Fredriksson A, Archer T, Alm H, Gordh T, Eriksson P. Neurofunctional deficits and potentiated apoptosis by neonatal NMDA antagonist administration. Behav Brain Res. 2004;153:367–376. doi: 10.1016/j.bbr.2003.12.026. [DOI] [PubMed] [Google Scholar]
- Fredriksson A, Ponten E, Gordh T, Eriksson P. Neonatal exposure to a combination of N-methyl-D-aspartate and gamma-aminobutyric acid type A receptor anesthetic agents potentiates apoptotic neurodegeneration and persistent behavioral deficits. Anesthesiology. 2007;107:427–436. doi: 10.1097/01.anes.0000278892.62305.9c. [DOI] [PubMed] [Google Scholar]
- Gidday JM. Pharmacologic preconditioning: translating the promise. Transl Stroke Res. 2010;1:19–30. doi: 10.1007/s12975-010-0011-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grasshoff C, Rudolph U, Antkowiak B. Molecular and systemic mechanisms of general anaesthesia: the ‘multi-site and multiple mechanisms’ concept. Curr Opin Anaesthesiol. 2005;18:386–391. doi: 10.1097/01.aco.0000174961.90135.dc. [DOI] [PubMed] [Google Scholar]
- Habas A, Kharebava G, Szatmari E, Hetman M. NMDA neuroprotection against a phosphatidylinositol-3 kinase inhibitor, LY294002 by NR2B-mediated suppression of glycogen synthase kinase-3beta-induced apoptosis. J Neurochem. 2006;96:335–348. doi: 10.1111/j.1471-4159.2005.03543.x. [DOI] [PubMed] [Google Scholar]
- Hack N, Hidaka H, Wakefield MJ, Balazs R. Promotion of granule cell survival by high K+ or excitatory amino acid treatment and Ca2+/calmodulin-dependent protein kinase activity. Neuroscience. 1993;57:9–20. doi: 10.1016/0306-4522(93)90108-r. [DOI] [PubMed] [Google Scholar]
- Hall AA, Pennypacker KR. Implications of immune system in stroke for novel therapeutic approaches. Transl Stroke Res. 2010;1:85–95. doi: 10.1007/s12975-009-0003-y. [DOI] [PubMed] [Google Scholar]
- Hansen TG, Pedersen JK, Henneberg SW, Pedersen DA, Murray JC, Morton NS, Christensen K. Academic performance in adolescence after inguinal hernia repair in infancy: a nationwide cohort study. Anesthesiology. 2011;114:1076–1085. doi: 10.1097/ALN.0b013e31820e77a0. [DOI] [PubMed] [Google Scholar]
- Harrison NL, Simmonds MA. Quantitative studies on some antagonists of N-methyl D-aspartate in slices of rat cerebral cortex. Br J Pharmacol. 1985;84:381–391. doi: 10.1111/j.1476-5381.1985.tb12922.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayashi H, Dikkes P, Soriano SG. Repeated administration of ketamine may lead to neuronal degeneration in the developing rat brain. Paediatr Anaesth. 2002;12:770–774. doi: 10.1046/j.1460-9592.2002.00883.x. [DOI] [PubMed] [Google Scholar]
- Heinrichs M, Domes G. Neuropeptides and social behaviour: effects of oxytocin and vasopressin in humans. Prog Brain Res. 2008;170:337–350. doi: 10.1016/S0079-6123(08)00428-7. [DOI] [PubMed] [Google Scholar]
- Helmy SA, Al-Attiyah RJ. The effect of halothane and isoflurane on plasma cytokine levels. Anaesthesia. 2000;55:904–910. doi: 10.1046/j.1365-2044.2000.01472-2.x. [DOI] [PubMed] [Google Scholar]
- Hosaka K, Hoh BL. Inflammation and cerebral aneurysms. Transl Stroke Res. 2014;5:190–198. doi: 10.1007/s12975-013-0313-y. [DOI] [PubMed] [Google Scholar]
- Ikonomidou C, Bosch F, Miksa M, Bittigau P, Vockler J, Dikranian K, Tenkova TI, Stefovska V, Turski L, Olney JW. Blockade of NMDA receptors and apoptotic neurodegeneration in the developing brain. Science. 1999;283:70–74. doi: 10.1126/science.283.5398.70. [DOI] [PubMed] [Google Scholar]
- Ing CH, DiMaggio CJ, Malacova E, Whitehouse AJ, Hegarty MK, Feng T, Brady JE, von Ungern-Sternberg BS, Davidson AJ, Wall MM, Wood AJ, Li G, Sun LS. Comparative analysis of outcome measures used in examining neurodevelopmental effects of early childhood anesthesia exposure. Anesthesiology. 2014;120:1319–1332. doi: 10.1097/ALN.0000000000000248. [DOI] [PubMed] [Google Scholar]
- Istaphanous GK, Ward CG, Nan X, Hughes EA, McCann JC, McAuliffe JJ, Danzer SC, Loepke AW. Characterization and quantification of isoflurane-induced developmental apoptotic cell death in mouse cerebral cortex. Anesth Analg. 2013;116:845–854. doi: 10.1213/ANE.0b013e318281e988. [DOI] [PubMed] [Google Scholar]
- Ivan M, Kondo K, Yang H, Kim W, Valiando J, Ohh M, Salic A, Asara JM, Lane WS, Kaelin WG., Jr HIFalpha targeted for VHL-mediated destruction by proline hydroxylation: implications for O2 sensing. Science. 2001;292:464–468. doi: 10.1126/science.1059817. [DOI] [PubMed] [Google Scholar]
- Jaakkola P, Mole DR, Tian YM, Wilson MI, Gielbert J, Gaskell SJ, von Kriegsheim A, Hebestreit HF, Mukherji M, Schofield CJ, Maxwell PH, Pugh CW, Ratcliffe PJ. Targeting of HIF-alpha to the von Hippel-Lindau ubiquitylation complex by O2-regulated prolyl hydroxylation. Science. 2001;292:468–472. doi: 10.1126/science.1059796. [DOI] [PubMed] [Google Scholar]
- Jenkins K, Baker AB. Consent and anaesthetic risk. Anaesthesia. 2003;58:962–984. doi: 10.1046/j.1365-2044.2003.03410.x. [DOI] [PubMed] [Google Scholar]
- Jevtovic-Todorovic V, Hartman RE, Izumi Y, Benshoff ND, Dikranian K, Zorumski CF, Olney JW, Wozniak DF. Early exposure to common anesthetic agents causes widespread neurodegeneration in the developing rat brain and persistent learning deficits. J Neurosci. 2003;23:876–882. doi: 10.1523/JNEUROSCI.23-03-00876.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jevtovic-Todorovic V, Todorovic SM, Mennerick S, Powell S, Dikranian K, Benshoff N, Zorumski CF, Olney JW. Nitrous oxide (laughing gas) is an NMDA antagonist, neuroprotectant and neurotoxin. Nat Med. 1998;4:460–463. doi: 10.1038/nm0498-460. [DOI] [PubMed] [Google Scholar]
- Jiang H, Huang Y, Xu H, Sun Y, Han N, Li QF. Hypoxia inducible factor-1alpha is involved in the neurodegeneration induced by isoflurane in the brain of neonatal rats. J Neurochem. 2012;120:453–460. doi: 10.1111/j.1471-4159.2011.07589.x. [DOI] [PubMed] [Google Scholar]
- Jiang J, Jiang H. Effect of the inhaled anesthetics isoflurane, sevoflurane and desflurane on the neuropathogenesis of Alzheimer’s disease(Review) Mol Medicine Rep. 2015 doi: 10.3892/mmr.2015.3424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang X, Tian F, Mearow K, Okagaki P, Lipsky RH, Marini AM. The excitoprotective effect of N-methyl-D-aspartate receptors is mediated by a brain-derived neurotrophic factor autocrine loop in cultured hippocampal neurons. J Neurochem. 2005;94:713–722. doi: 10.1111/j.1471-4159.2005.03200.x. [DOI] [PubMed] [Google Scholar]
- Johnson SA, Young C, Olney JW. Isoflurane-induced neuroapoptosis in the developing brain of nonhypoglycemic mice. J Neurosurgical Anesth. 2008;20:21–28. doi: 10.1097/ANA.0b013e3181271850. [DOI] [PubMed] [Google Scholar]
- Kain ZN, Mayes LC, Wang SM, Hofstadter MB. Postoperative behavioral outcomes in children: effects of sedative premedication. Anesthesiology. 1999;90:758–765. doi: 10.1097/00000542-199903000-00018. [DOI] [PubMed] [Google Scholar]
- Kawaguchi M, Kimbro JR, Drummond JC, Cole DJ, Kelly PJ, Patel PM. Isoflurane delays but does not prevent cerebral infarction in rats subjected to focal ischemia. Anesthesiology. 2000;92:1335–1342. doi: 10.1097/00000542-200005000-00023. [DOI] [PubMed] [Google Scholar]
- Kissin I. A concept for assessing interactions of general anesthetics. Anesth Analg. 1997;85:204–210. doi: 10.1097/00000539-199707000-00036. [DOI] [PubMed] [Google Scholar]
- Koblin DD, Chortkoff BS, Laster MJ, Eger EI, 2nd, Halsey MJ, Ionescu P. Polyhalogenated and perfluorinated compounds that disobey the Meyer-Overton hypothesis. Anesth Analg. 1994;79:1043–1048. doi: 10.1213/00000539-199412000-00004. [DOI] [PubMed] [Google Scholar]
- Koch VW. The Animal Welfare Act, U SDA, & research. Contemp Top Lab Anim Sci. 2003;42:58, 62, 64. [PubMed] [Google Scholar]
- Kodama M, Satoh Y, Otsubo Y, Araki Y, Yonamine R, Masui K, Kazama T. Neonatal desflurane exposure induces more robust neuroapoptosis than do isoflurane and sevoflurane and impairs working memory. Anesthesiology. 2011;115:979–991. doi: 10.1097/ALN.0b013e318234228b. [DOI] [PubMed] [Google Scholar]
- Kohrs R, Durieux ME. Ketamine: teaching an old drug new tricks. Anesth Analg. 1998;87:1186–1193. doi: 10.1097/00000539-199811000-00039. [DOI] [PubMed] [Google Scholar]
- Kong FJ, Ma LL, Hu WW, Wang WN, Lu HS, Chen SP. Fetal exposure to high isoflurane concentration induces postnatal memory and learning deficits in rats. Biochem Pharmacol. 2012;84:558–563. doi: 10.1016/j.bcp.2012.06.001. [DOI] [PubMed] [Google Scholar]
- Kulak A, Duarte JM, Do KQ, Gruetter R. Neurochemical profile of the developing mouse cortex determined by in vivo 1H NMR spectroscopy at 14.1 T and the effect of recurrent anaesthesia. J Neurochem. 2010;115:1466–1477. doi: 10.1111/j.1471-4159.2010.07051.x. [DOI] [PubMed] [Google Scholar]
- Lafon-Cazal M, Perez V, Bockaert J, Marin P. Akt mediates the anti-apoptotic effect of NMDA but not that induced by potassium depolarization in cultured cerebellar granule cells. Eur J Neurosci. 2002;16:575–583. doi: 10.1046/j.1460-9568.2002.02124.x. [DOI] [PubMed] [Google Scholar]
- Lahat N, Zlotnick AY, Shtiller R, Bar I, Merin G. Serum levels of IL-1, IL-6 and tumour necrosis factors in patients undergoing coronary artery bypass grafts or cholecystectomy. Clin Exp Immunol. 1992;89:255–260. doi: 10.1111/j.1365-2249.1992.tb06941.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeDez KM, Lerman J. The minimum alveolar concentration (MAC) of isoflurane in preterm neonates. Anesthesiology. 1987;67:301–307. doi: 10.1097/00000542-198709000-00004. [DOI] [PubMed] [Google Scholar]
- Lee BH, Chan JT, Hazarika O, Vutskits L, Sall JW. Early exposure to volatile anesthetics impairs long-term associative learning and recognition memory. PloS one. 2014;9:e105340. doi: 10.1371/journal.pone.0105340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee SN, Li L, Zuo Z. Glutamate transporter type 3 knockout mice have a decreased isoflurane requirement to induce loss of righting reflex. Neuroscience. 2010;171:788–793. doi: 10.1016/j.neuroscience.2010.09.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu DZ, Sharp FR. Excitatory and Mitogenic Signaling in Cell Death, Blood-brain Barrier Breakdown, and BBB Repair after Intracerebral Hemorrhage. Transl Stroke Res. 2012;3:62–69. doi: 10.1007/s12975-012-0147-z. [DOI] [PubMed] [Google Scholar]
- Liu F, Paule MG, Ali S, Wang C. Ketamine-induced neurotoxicity and changes in gene expression in the developing rat brain. Curr Neuropharmacol. 2011;9:256–261. doi: 10.2174/157015911795017155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loepke AW, Istaphanous GK, McAuliffe JJ, 3rd, Miles L, Hughes EA, McCann JC, Harlow KE, Kurth CD, Williams MT, Vorhees CV, Danzer SC. The effects of neonatal isoflurane exposure in mice on brain cell viability, adult behavior, learning, and memory. Anesth Analg. 2009;108:90–104. doi: 10.1213/ane.0b013e31818cdb29. [DOI] [PubMed] [Google Scholar]
- Lu LX, Yon JH, Carter LB, Jevtovic-Todorovic V. General anesthesia activates BDNF-dependent neuroapoptosis in the developing rat brain. Apoptosis. 2006;11:1603–1615. doi: 10.1007/s10495-006-8762-3. [DOI] [PubMed] [Google Scholar]
- Lu Y, Wu X, Dong Y, Xu Z, Zhang Y, Xie Z. Anesthetic sevoflurane causes neurotoxicity differently in neonatal naive and Alzheimer disease transgenic mice. Anesthesiology. 2010;112:1404–1416. doi: 10.1097/ALN.0b013e3181d94de1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malkova L, Heuer E, Saunders RC. Longitudinal magnetic resonance imaging study of rhesus monkey brain development. Eur J Neurosci. 2006;24:3204–3212. doi: 10.1111/j.1460-9568.2006.05175.x. [DOI] [PubMed] [Google Scholar]
- Mashour GA, Forman SA, Campagna JA. Mechanisms of general anesthesia: from molecules to mind. Best Pract Res Clin Anaesthesiol. 2005;19:349–364. doi: 10.1016/j.bpa.2005.01.004. [DOI] [PubMed] [Google Scholar]
- Mawhinney LJ, Mabourakh D, Lewis MC. Gender-specific differences in the central nervous system’s response to anesthesia. Transl Stroke Res. 2013;4:462–475. doi: 10.1007/s12975-012-0229-y. [DOI] [PubMed] [Google Scholar]
- McMurtrey RJ, Zuo Z. Isoflurane preconditioning and postconditioning in rat hippocampal neurons. Brain Res. 2010;1358:184–190. doi: 10.1016/j.brainres.2010.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menghraj SJ. Anaesthetic considerations in children with congenital heart disease undergoing non-cardiac surgery. Indian J Anaesth. 2012;56:491–495. doi: 10.4103/0019-5049.103969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mintz CD, Barrett KM, Smith SC, Benson DL, Harrison NL. Anesthetics interfere with axon guidance in developing mouse neocortical neurons in vitro via a gamma-aminobutyric acid type A receptor mechanism. Anesthesiology. 2013;118:825–833. doi: 10.1097/ALN.0b013e318287b850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy KL, Baxter MG. Long-term effects of neonatal single or multiple isoflurane exposures on spatial memory in rats. Front Neurol. 2013;4:87. doi: 10.3389/fneur.2013.00087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson LE, Guo TZ, Lu J, Saper CB, Franks NP, Maze M. The sedative component of anesthesia is mediated by GABA(A) receptors in an endogenous sleep pathway. Nat Neurosci. 2002;5:979–984. doi: 10.1038/nn913. [DOI] [PubMed] [Google Scholar]
- Nishikawa K, Harrison NL. The actions of sevoflurane and desflurane on the gamma-aminobutyric acid receptor type A: effects of TM2 mutations in the alpha and beta subunits. Anesthesiology. 2003;99:678–684. doi: 10.1097/00000542-200309000-00024. [DOI] [PubMed] [Google Scholar]
- Nuland SB. Doctors : the biography of medicine. Vintage Books; New York: 1989. 1st Vintage Books. [Google Scholar]
- Ogle ME, Gu X, Espinera AR, Wei L. Inhibition of prolyl hydroxylases by dimethyloxaloylglycine after stroke reduces ischemic brain injury and requires hypoxia inducible factor-1alpha. Neurobiol Dis. 2012;45:733–742. doi: 10.1016/j.nbd.2011.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olney JW. New insights and new issues in developmental neurotoxicology. Neurotoxicology. 2002;23:659–668. doi: 10.1016/S0161-813X(01)00092-4. [DOI] [PubMed] [Google Scholar]
- Olsen RW, Li GD. GABA(A) receptors as molecular targets of general anesthetics: identification of binding sites provides clues to allosteric modulation. Can J Anaesth. 2011;58:206–215. doi: 10.1007/s12630-010-9429-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmer L. Anesthesia 101: everything you need to know. Plast Surgical Nurs. 2013;33:164–171. doi: 10.1097/01.ORN.0000431584.22992.aa. [DOI] [PubMed] [Google Scholar]
- Paule MG, Li M, Allen RR, Liu F, Zou X, Hotchkiss C, Hanig JP, Patterson TA, Slikker W, Jr, Wang C. Ketamine anesthesia during the first week of life can cause long-lasting cognitive deficits in rhesus monkeys. Neurotoxicol Teratol. 2011;33:220–230. doi: 10.1016/j.ntt.2011.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perouansky M, Hemmings HC., Jr Neurotoxicity of general anesthetics: cause for concern? Anesthesiology. 2009;111:1365–1371. doi: 10.1097/ALN.0b013e3181bf1d61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pesic V, Milanovic D, Tanic N, Popic J, Kanazir S, Jevtovic-Todorovic V, Ruzdijic S. Potential mechanism of cell death in the developing rat brain induced by propofol anesthesia. Int J Developmental Neuosci. 2009;27:279–287. doi: 10.1016/j.ijdevneu.2008.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petit TL, LeBoutillier JC, Gregorio A, Libstug H. The pattern of dendritic development in the cerebral cortex of the rat. Brain Res. 1988;469:209–219. doi: 10.1016/0165-3806(88)90183-6. [DOI] [PubMed] [Google Scholar]
- Poo MM. Neurotrophins as synaptic modulators. Nature reviews Neuroscience. 2001;2:24–32. doi: 10.1038/35049004. [DOI] [PubMed] [Google Scholar]
- Quimby KL, Aschkenase LJ, Bowman RE, Katz J, Chang LW. Enduring learning deficits and cerebral synaptic malformation from exposure to 10 parts of halothane per million. Science. 1974;185:625–627. doi: 10.1126/science.185.4151.625. [DOI] [PubMed] [Google Scholar]
- Ramanantsoa N, Fleiss B, Bouslama M, Matrot B, Schwendimann L, Cohen-Salmon C, Gressens P, Gallego J. Bench to cribside: the path for developing a neuroprotectant. Transl Stroke Res. 2013;4:258–277. doi: 10.1007/s12975-012-0233-2. [DOI] [PubMed] [Google Scholar]
- Rammes G, Starker LK, Haseneder R, Berkmann J, Plack A, Zieglgansberger W, Ohl F, Kochs EF, Blobner M. Isoflurane anaesthesia reversibly improves cognitive function and long-term potentiation (LTP) via an up-regulation in NMDA receptor 2B subunit expression. Neuropharmacology. 2009;56:626–636. doi: 10.1016/j.neuropharm.2008.11.002. [DOI] [PubMed] [Google Scholar]
- Ringler SL, Aye J, Byrne E, Anderson M, Turner CP. Effects of disrupting calcium homeostasis on neuronal maturation: early inhibition and later recovery. Cell Mol Neurobiol. 2008;28:389–409. doi: 10.1007/s10571-007-9255-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizzi S, Carter LB, Ori C, Jevtovic-Todorovic V. Clinical anesthesia causes permanent damage to the fetal guinea pig brain. Brain Patho. 2008;18:198–210. doi: 10.1111/j.1750-3639.2007.00116.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothstein S, Simkins T, Nunez JL. Response to neonatal anesthesia: effect of sex on anatomical and behavioral outcome. Neuroscience. 2008;152:959–969. doi: 10.1016/j.neuroscience.2008.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudolph U, Antkowiak B. Molecular and neuronal substrates for general anaesthetics. Nature reviews Neuroscience. 2004;5:709–720. doi: 10.1038/nrn1496. [DOI] [PubMed] [Google Scholar]
- Ryu YK, Khan S, Smith SC, Mintz CD. Isoflurane impairs the capacity of astrocytes to support neuronal development in a mouse dissociated coculture model. J Neurosurgical Anesth. 2014;26:363–368. doi: 10.1097/ANA.0000000000000119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakai H, Sheng H, Yates RB, Ishida K, Pearlstein RD, Warner DS. Isoflurane provides long-term protection against focal cerebral ischemia in the rat. Anesthesiology. 2007;106:92–99. doi: 10.1097/00000542-200701000-00017. discussion 98–10. [DOI] [PubMed] [Google Scholar]
- Sanchez V, Feinstein SD, Lunardi N, Joksovic PM, Boscolo A, Todorovic SM, Jevtovic-Todorovic V. General Anesthesia Causes Long-term Impairment of Mitochondrial Morphogenesis and Synaptic Transmission in Developing Rat Brain. Anesthesiology. 2011;115:992–1002. doi: 10.1097/ALN.0b013e3182303a63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sato Y, Kobayashi E, Murayama T, Mishina M, Seo N. Effect of N-methyl-D-aspartate receptor epsilon1 subunit gene disruption of the action of general anesthetic drugs in mice. Anesthesiology. 2005;102:557–561. doi: 10.1097/00000542-200503000-00013. [DOI] [PubMed] [Google Scholar]
- Satomoto M, Satoh Y, Terui K, Miyao H, Takishima K, Ito M, Imaki J. Neonatal exposure to sevoflurane induces abnormal social behaviors and deficits in fear conditioning in mice. Anesthesiology. 2009;110:628–637. doi: 10.1097/ALN.0b013e3181974fa2. [DOI] [PubMed] [Google Scholar]
- Scallet AC, Schmued LC, Slikker W, Jr, Grunberg N, Faustino PJ, Davis H, Lester D, Pine PS, Sistare F, Hanig JP. Developmental neurotoxicity of ketamine: morphometric confirmation, exposure parameters, and multiple fluorescent labeling of apoptotic neurons. Toxicol Sci. 2004;81:364–370. doi: 10.1093/toxsci/kfh224. [DOI] [PubMed] [Google Scholar]
- Schifilliti D, Grasso G, Conti A, Fodale V. Anaesthetic-related neuroprotection: intravenous or inhalational agents? CNS drugs. 2010;24:893–907. doi: 10.2165/11584760-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Schmidt-Hieber C, Jonas P, Bischofberger J. Enhanced synaptic plasticity in newly generated granule cells of the adult hippocampus. Nature. 2004;429:184–187. doi: 10.1038/nature02553. [DOI] [PubMed] [Google Scholar]
- Schneemilch CE, Bank U. Release of pro- and anti-inflammatory cytokines during different anesthesia procedures. Anaesthesiol Reanim. 2001;26:4–10. [PubMed] [Google Scholar]
- Semenza GL. Transcriptional regulation of gene expression: mechanisms and pathophysiology. Hum Mutat. 1994;3:180–199. doi: 10.1002/humu.1380030304. [DOI] [PubMed] [Google Scholar]
- Shen X, Dong Y, Xu Z, Wang H, Miao C, Soriano SG, Sun D, Baxter MG, Zhang Y, Xie Z. Selective anesthesia-induced neuroinflammation in developing mouse brain and cognitive impairment. Anesthesiology. 2013;118:502–515. doi: 10.1097/ALN.0b013e3182834d77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shu Y, Zhou Z, Wan Y, Sanders RD, Li M, Pac-Soo CK, Maze M, Ma D. Nociceptive stimuli enhance anesthetic-induced neuroapoptosis in the rat developing brain. Neurobiol Dis. 2012;45:743–750. doi: 10.1016/j.nbd.2011.10.021. [DOI] [PubMed] [Google Scholar]
- Slikker W, Jr, Zou X, Hotchkiss CE, Divine RL, Sadovova N, Twaddle NC, Doerge DR, Scallet AC, Patterson TA, Hanig JP, Paule MG, Wang C. Ketamine-induced neuronal cell death in the perinatal rhesus monkey. Toxicol Sci. 2007;98:145–158. doi: 10.1093/toxsci/kfm084. [DOI] [PubMed] [Google Scholar]
- Song M, Yu SP. Ionic regulation of cell volume changes and cell death after ischemic stroke. Transl Stroke Res. 2014;5:17–27. doi: 10.1007/s12975-013-0314-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonner JM, Antognini JF, Dutton RC, Flood P, Gray AT, Harris RA, Homanics GE, Kendig J, Orser B, Raines DE, Rampil IJ, Trudell J, Vissel B, Eger EI., 2nd Inhaled anesthetics and immobility: mechanisms, mysteries, and minimum alveolar anesthetic concentration. Anesth Analg. 2003;97:718–740. doi: 10.1213/01.ANE.0000081063.76651.33. [DOI] [PubMed] [Google Scholar]
- Soriano SG, Liu Q, Li J, Liu JR, Han XH, Kanter JL, Bajic D, Ibla JC. Ketamine activates cell cycle signaling and apoptosis in the neonatal rat brain. Anesthesiology. 2010;112:1155–1163. doi: 10.1097/ALN.0b013e3181d3e0c2. [DOI] [PubMed] [Google Scholar]
- Souvenir R, Flores JJ, Ostrowski RP, Manaenko A, Duris K, Tang J. Erythropoietin inhibits HIF-1alpha expression via upregulation of PHD-2 transcription and translation in an in vitro model of hypoxia-ischemia. Transl Stroke Res. 2014;5:118–127. doi: 10.1007/s12975-013-0312-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sprung J, Flick RP, Katusic SK, Colligan RC, Barbaresi WJ, Bojanic K, Welch TL, Olson MD, Hanson AC, Schroeder DR, Wilder RT, Warner DO. Attention-deficit/hyperactivity disorder after early exposure to procedures requiring general anesthesia. Mayo Clin Proc. 2012;87:120–129. doi: 10.1016/j.mayocp.2011.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Straiko MM, Young C, Cattano D, Creeley CE, Wang H, Smith DJ, Johnson SA, Li ES, Olney JW. Lithium protects against anesthesia-induced developmental neuroapoptosis. Anesthesiology. 2009;110:862–868. doi: 10.1097/ALN.0b013e31819b5eab. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stratmann G. Review article: Neurotoxicity of anesthetic drugs in the developing brain. Anesth Analg. 2011;113:1170–1179. doi: 10.1213/ANE.0b013e318232066c. [DOI] [PubMed] [Google Scholar]
- Stratmann G, May LD, Sall JW, Alvi RS, Bell JS, Ormerod BK, Rau V, Hilton JF, Dai R, Lee MT, Visrodia KH, Ku B, Zusmer EJ, Guggenheim J, Firouzian A. Effect of hypercarbia and isoflurane on brain cell death and neurocognitive dysfunction in 7-day-old rats. Anesthesiology. 2009a;110:849–861. doi: 10.1097/ALN.0b013e31819c7140. [DOI] [PubMed] [Google Scholar]
- Stratmann G, Sall JW, May LD, Bell JS, Magnusson KR, Rau V, Visrodia KH, Alvi RS, Ku B, Lee MT, Dai R. Isoflurane differentially affects neurogenesis and long-term neurocognitive function in 60-day-old and 7-day-old rats. Anesthesiology. 2009b;110:834–848. doi: 10.1097/ALN.0b013e31819c463d. [DOI] [PubMed] [Google Scholar]
- Study RE. Isoflurane inhibits multiple voltage-gated calcium currents in hippocampal pyramidal neurons. Anesthesiology. 1994;81:104–116. doi: 10.1097/00000542-199407000-00016. [DOI] [PubMed] [Google Scholar]
- Sutter CH, Laughner E, Semenza GL. Hypoxia-inducible factor 1alpha protein expression is controlled by oxygen-regulated ubiquitination that is disrupted by deletions and missense mutations. Proc Natl Acad Sci U S A. 2000;97:4748–4753. doi: 10.1073/pnas.080072497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tao G, Zhang J, Zhang L, Dong Y, Yu B, Crosby G, Culley DJ, Zhang Y, Xie Z. Sevoflurane induces tau phosphorylation and glycogen synthase kinase 3beta activation in young mice. Anesthesiology. 2014;121:510–527. doi: 10.1097/ALN.0000000000000278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uemura E, Levin ED, Bowman RE. Effects of halothane on synaptogenesis and learning behavior in rats. Exp Neurol. 1985;89:520–529. doi: 10.1016/0014-4886(85)90003-2. [DOI] [PubMed] [Google Scholar]
- Viberg H, Ponten E, Eriksson P, Gordh T, Fredriksson A. Neonatal ketamine exposure results in changes in biochemical substrates of neuronal growth and synaptogenesis, and alters adult behavior irreversibly. Toxicology. 2008;249:153–159. doi: 10.1016/j.tox.2008.04.019. [DOI] [PubMed] [Google Scholar]
- Vutskits L, Davis PJ, Hansen TG. Anesthetics and the developing brain: time for a change in practice? A pro/con debate. Paediatr Anaesth. 2012;22:973–980. doi: 10.1111/pan.12015. [DOI] [PubMed] [Google Scholar]
- Wang C, Sadovova N, Fu X, Schmued L, Scallet A, Hanig J, Slikker W. The role of the N-methyl-D-aspartate receptor in ketamine-induced apoptosis in rat forebrain culture. Neuroscience. 2005;132:967–977. doi: 10.1016/j.neuroscience.2005.01.053. [DOI] [PubMed] [Google Scholar]
- Wang GL, Semenza GL. General involvement of hypoxia-inducible factor 1 in transcriptional response to hypoxia. Proc Natl Acad Sci U S A. 1993;90:4304–4308. doi: 10.1073/pnas.90.9.4304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang GL, Semenza GL. Purification and characterization of hypoxia-inducible factor 1. J Biol Chem. 1995;270:1230–1237. doi: 10.1074/jbc.270.3.1230. [DOI] [PubMed] [Google Scholar]
- Wang H, Lu S, Yu Q, Liang W, Gao H, Li P, Gan Y, Chen J, Gao Y. Sevoflurane preconditioning confers neuroprotection via anti-inflammatory effects. Front Biosci. 2011;3:604–615. doi: 10.2741/e273. [DOI] [PubMed] [Google Scholar]
- Wang Y, Cheng Y, Liu G, Tian X, Tu X, Wang J. Chronic exposure of gestation rat to sevoflurane impairs offspring brain development. Neurol Sci. 2012;33:535–544. doi: 10.1007/s10072-011-0762-6. [DOI] [PubMed] [Google Scholar]
- Warner DS. Isoflurane neuroprotection: a passing fantasy, again? Anesthesiology. 2000;92:1226–1228. [PubMed] [Google Scholar]
- Wei H, Liang G, Yang H. Isoflurane preconditioning inhibited isoflurane-induced neurotoxicity. Neurosci Lett. 2007;425:59–62. doi: 10.1016/j.neulet.2007.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells BA, Keats AS, Cooley DA. Increased tolerance to cerebral ischemia produced by general anesthesia during temporary carotid occlusion. Surgery. 1963;54:216–223. [PubMed] [Google Scholar]
- Wilder RT, Flick RP, Sprung J, Katusic SK, Barbaresi WJ, Mickelson C, Gleich SJ, Schroeder DR, Weaver AL, Warner DO. Early exposure to anesthesia and learning disabilities in a population-based birth cohort. Anesthesiology. 2009;110:796–804. doi: 10.1097/01.anes.0000344728.34332.5d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu X, Lu Y, Dong Y, Zhang G, Zhang Y, Xu Z, Culley DJ, Crosby G, Marcantonio ER, Tanzi RE, Xie Z. The inhalation anesthetic isoflurane increases levels of proinflammatory TNF-alpha, IL-6, and IL-1beta. Neurobiol Aging. 2012;33:1364–1378. doi: 10.1016/j.neurobiolaging.2010.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang H, Liang G, Hawkins BJ, Madesh M, Pierwola A, Wei H. Inhalational anesthetics induce cell damage by disruption of intracellular calcium homeostasis with different potencies. Anesthesiology. 2008;109:243–250. doi: 10.1097/ALN.0b013e31817f5c47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yokobori S, Mazzeo AT, Hosein K, Gajavelli S, Dietrich WD, Bullock MR. Preconditioning for traumatic brain injury. Transl Stroke Res. 2013;4:25–39. doi: 10.1007/s12975-012-0226-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yon JH, Daniel-Johnson J, Carter LB, Jevtovic-Todorovic V. Anesthesia induces neuronal cell death in the developing rat brain via the intrinsic and extrinsic apoptotic pathways. Neuroscience. 2005;135:815–827. doi: 10.1016/j.neuroscience.2005.03.064. [DOI] [PubMed] [Google Scholar]
- Yonamine R, Satoh Y, Kodama M, Araki Y, Kazama T. Coadministration of hydrogen gas as part of the carrier gas mixture suppresses neuronal apoptosis and subsequent behavioral deficits caused by neonatal exposure to sevoflurane in mice. Anesthesiology. 2013;118:105–113. doi: 10.1097/ALN.0b013e318275146d. [DOI] [PubMed] [Google Scholar]
- Young C, Jevtovic-Todorovic V, Qin YQ, Tenkova T, Wang H, Labruyere J, Olney JW. Potential of ketamine and midazolam, individually or in combination, to induce apoptotic neurodegeneration in the infant mouse brain. Br J Pharmacol. 2005;146:189–197. doi: 10.1038/sj.bjp.0706301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu Q, Chu M, Wang H, Lu S, Gao H, Li P, Gan Y, Shi H, Liang W, Chen J, Gao Y. Sevoflurane preconditioning protects blood-brain-barrier against brain ischemia. Front Biosci. 2011;3:978–988. doi: 10.2741/e303. [DOI] [PubMed] [Google Scholar]
- Yu Q, Wang H, Chen J, Gao Y, Liang W. Neuroprotections and mechanisms of inhalational anesthetics against brain ischemia. Front Biosci. 2010;2:1275–1298. doi: 10.2741/e189. [DOI] [PubMed] [Google Scholar]
- Yu SP, Wei Z, Wei L. Preconditioning strategy in stem cell transplantation therapy. Transl Stroke Res. 2013;4:76–88. doi: 10.1007/s12975-012-0251-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang G, Dong Y, Zhang B, Ichinose F, Wu X, Culley DJ, Crosby G, Tanzi RE, Xie Z. Isoflurane-induced caspase-3 activation is dependent on cytosolic calcium and can be attenuated by memantine. J Neurosci. 2008a;28:4551–4560. doi: 10.1523/JNEUROSCI.5694-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J, Dong Y, Zhou C, Zhang Y, Xie Z. Anesthetic Sevoflurane Reduces Levels of Hippocalcin and Postsynaptic Density Protein 95. Mol Neurobio. 2014 doi: 10.1007/s12035-014-8746-1. [DOI] [PubMed] [Google Scholar]
- Zhang L, Zhang J, Yang L, Dong Y, Zhang Y, Xie Z. Isoflurane and sevoflurane increase interleukin-6 levels through the nuclear factor-kappa B pathway in neuroglioma cells. Br J Aneasth. 2013;110(Suppl 1):i82–91. doi: 10.1093/bja/aet115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X, Xue Z, Sun A. Subclinical concentration of sevoflurane potentiates neuronal apoptosis in the developing C57BL/6 mouse brain. Neurosci Lett. 2008b;447:109–114. doi: 10.1016/j.neulet.2008.09.083. [DOI] [PubMed] [Google Scholar]
- Zhao P, Peng L, Li L, Xu X, Zuo Z. Isoflurane preconditioning improves long-term neurologic outcome after hypoxic-ischemic brain injury in neonatal rats. Anesthesiology. 2007;107:963–970. doi: 10.1097/01.anes.0000291447.21046.4d. [DOI] [PubMed] [Google Scholar]
- Zhao P, Zuo Z. Isoflurane preconditioning induces neuroprotection that is inducible nitric oxide synthase-dependent in neonatal rats. Anesthesiology. 2004;101:695–703. doi: 10.1097/00000542-200409000-00018. [DOI] [PubMed] [Google Scholar]
- Zhao YL, Xiang Q, Shi QY, Li SY, Tan L, Wang JT, Jin XG, Luo AL. GABAergic excitotoxicity injury of the immature hippocampal pyramidal neurons’ exposure to isoflurane. Anesth Analg. 2011;113:1152–1160. doi: 10.1213/ANE.0b013e318230b3fd. [DOI] [PubMed] [Google Scholar]
- Zheng S, Zuo Z. Isoflurane preconditioning induces neuroprotection against ischemia via activation of P38 mitogen-activated protein kinases. Mol Pharmacol. 2004;65:1172–1180. doi: 10.1124/mol.65.5.1172. [DOI] [PubMed] [Google Scholar]
- Zhou X, Song FH, He W, Yang XY, Zhou ZB, Feng X, Zhou LH. Neonatal exposure to sevoflurane causes apoptosis and reduces nNOS protein expression in rat hippocampus. Mol Med Rep. 2012;6:543–546. doi: 10.3892/mmr.2012.976. [DOI] [PubMed] [Google Scholar]
- Zhou ZB, Yang XY, Yuan BL, Niu LJ, Zhou X, Huang WQ, Feng X, Zhou LH. Sevoflurane-Induced Down-regulation of Hippocampal Oxytocin and Arginine Vasopressin Impairs Juvenile Social Behavioral Abilities. J Mol Neurosci. 2014 doi: 10.1007/s12031-014-0468-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu C, Gao J, Karlsson N, Li Q, Zhang Y, Huang Z, Li H, Kuhn HG, Blomgren K. Isoflurane anesthesia induced persistent, progressive memory impairment, caused a loss of neural stem cells, and reduced neurogenesis in young, but not adult, rodents. J Cereb Blood Flow Metab. 2010;30:1017–1030. doi: 10.1038/jcbfm.2009.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou X, Patterson TA, Divine RL, Sadovova N, Zhang X, Hanig JP, Paule MG, Slikker W, Jr, Wang C. Prolonged exposure to ketamine increases neurodegeneration in the developing monkey brain. Int J Dev Neurosci. 2009;27:727–731. doi: 10.1016/j.ijdevneu.2009.06.010. [DOI] [PubMed] [Google Scholar]