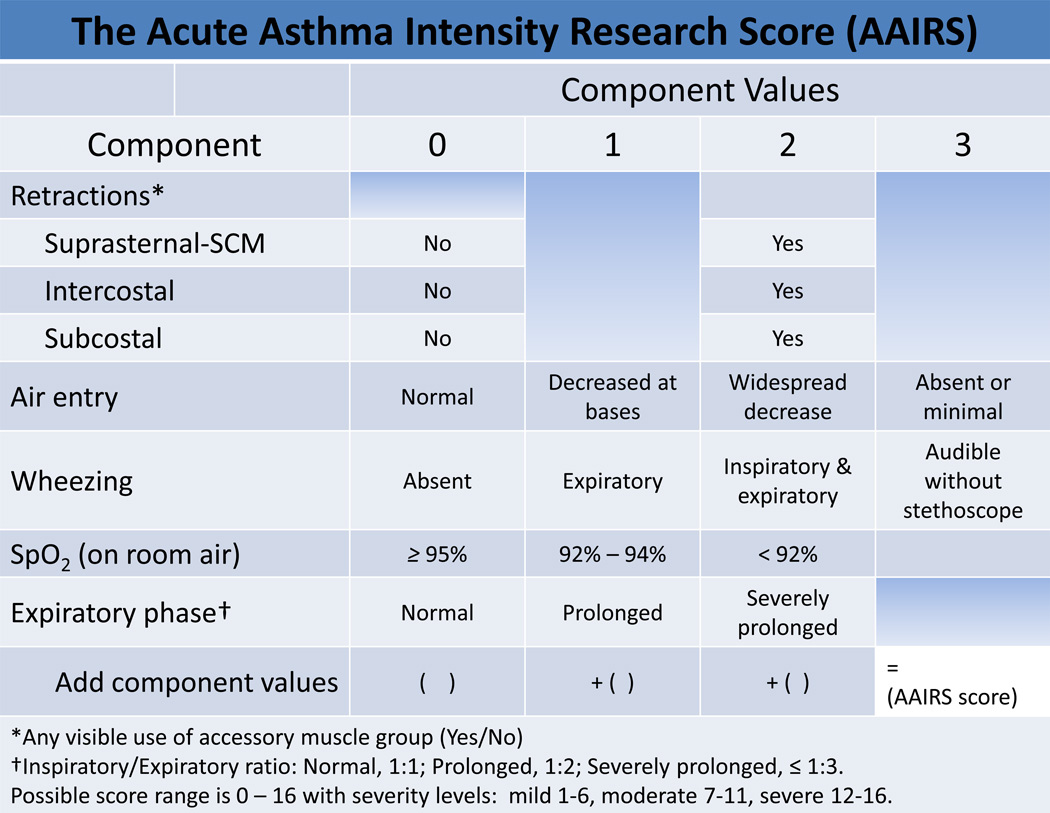
Pediatric acute asthma exacerbations are responsible for 640,000 emergency department (ED) visits each year and are the most frequent reason for childhood hospitalization in the United States.1 Expert panel guidelines recommend that treatment and hospitalization decisions be made based on assessment of severity and response to treatment. However, these guidelines specify severity assessment that includes spirometry for peak expiratory flow measurement (FEV1), measures that are generally unavailable or difficult for pediatric patients to perform during exacerbations.2–4 The Acute Asthma Intensity Research Score (AAIRS) is a 17-point (0 to 16, with 16 most severe) bedside severity score that uses readily evaluated physical signs (Figure 1) and that has been validated against the criterion standard %-predicted FEV1.5, 6 We are not aware of training videos published in the peer-review literature for acute asthma severity scores. The accompanying video follows the course of a young child with a moderately severe asthma exacerbation over several hours of ED care to demonstrate the seven physical signs comprising the AAIRS and how they are to be evaluated for AAIRS scoring. The protocol under which the AAIRS was developed was approved by our institutional review board, and development of the training video was a quality improvement initiative requested by our clinical leadership.
Figure 1.
The Acute Asthma Intensity Research Score (AAIRS)
Acknowledgments
Disclosures: Funding for development of the AAIRS was provided by the National Institutes of Health, K23 HL80005.
Footnotes
Video available at: Link to submission: https://vimeo.com/122443037 (click “AAIRS Scoring System”)
REFERENCES
- 1.Akinbami LJ, Moorman JE, Liu X. Asthma prevalence, health care, use, mortality: United States, 2005–2009. Natl Health Stat Report. 2011;12(32):1–14. [PubMed] [Google Scholar]
- 2.National Heart Lung and Blood Institute. Expert Panel Report 3: guidelines for the diagnosis and management of asthma. [Accessed Aug 1, 2015];National Asthma Education and Prevention Program. Available at: https://www.nhlbi.nih.gov/health-pro/guidelines/current/asthma-guidelines/full-report.
- 3.Arnold DH, Gebretsadik T, Abramo TJ, Hartert TV. Noninvasive testing of lung function and inflammation in pediatric patients with acute asthma exacerbations. J Asthma. 2012;49:29–35. doi: 10.3109/02770903.2011.637599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gorelick MH, Stevens MW, Schultz T, Scribano PV. Difficulty in obtaining peak expiratory flow measurements in children with acute asthma. Pediatr Emerg Care. 2004;20:22–26. doi: 10.1097/01.pec.0000106239.72265.16. [DOI] [PubMed] [Google Scholar]
- 5.Arnold DH, Saville BR, Wang W, Hartert TV. Performance of the Acute Asthma Intensity Research Score (AAIRS) for acute asthma research protocols. Ann Allergy Asthma Immunol. 2012;109:78–79. doi: 10.1016/j.anai.2012.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arnold DH, O'Connor AM, Hartert T. Acute Asthma Intensity Research Score: updated performance characteristics for prediction of hospitalization and lung function. Ann Allergy Asthma Immunol. 2015;115(1):69–70. doi: 10.1016/j.anai.2015.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]