Abstract
Objectives
Urinary tract infection (UTI) often represents a diagnostic challenge in the emergency department (ED) where urine culture results are generally not available, and other tests demonstrate limited sensitivity and specificity. Antimicrobial peptides (AMPs) are components of the innate immune system that have demonstrated increased urinary levels in response to infection both in children and in adults with chronic UTI. The objective of this study was to determine the relationship between urinary AMP levels and positive urine cultures in adult ED patients with suspected UTI.
Methods
This was a prospective, observational study of adult ED patients with suspected UTI. Enzyme-linked immunosorbent assays (ELISA) were performed to measure urine levels of AMPs: human neutrophil peptides 1–3 (HNP1-3), human α-defensin 5 (HD5), human beta defensin 2 (hBD-2), and cathelicidin (LL-37). Comparisons between positive and negative cultures were performed using Wilcoxon rank sum tests and receiver operating characteristic (ROC) curves, with calculation of area under the curve (AUC). Data were also analyzed for the older adult subgroup.
Results
Of 40 patients enrolled, 23 (58%) were ≥ 65 years, 25 were female (64%), and seven (17%) were non-white. Cultures were positive in 13 (32%), including seven in those ≥ 65 years old. HNP1-3, HD5, and hBD-2 levels were significantly higher in those with positive than negative urine cultures. Median HNP1-3 was 5.39 ng/mg (interquartile range [IQR] 2.74 to 11.09) in positive vs. 0.81 ng/mg (IQR 0.06 to 3.87) in negative cultures. Median HD5 was 4.75 pg/mg (IQR 1.6 to 22.7) in positive vs. 0.00 pg/mg (IQR 0 to 2.60) in negative cultures, and median hBD-2 was 0.13 pg/mg (IQR 0.08 to 0.17) in positive vs. 0.02 pg/mg (IQR 0 to 0.04) in negative cultures (p < 0.05 for all). Findings were similar for adults ≥ 65 years. The AUC was ≥ 0.75 for all three AMPs, both overall and in the older adult subgroup. LL-37 was not significantly higher in patients with positive urine culture. However, LL-37 expression is vitamin D dependent, and inadequate serum levels (< 30 ng/mL) were present in 72% of those tested.
Conclusions
Urinary levels of HNP1-3, HD5, and hBD-2 are significantly greater in the presence of positive urine cultures in ED patients with suspected UTI. These findings are maintained in the high-risk subgroup of older adults.
INTRODUCTION
Over three million patients are diagnosed with urinary tract infection (UTI) (cystitis and pyelonephritis) in U.S. emergency departments (EDs) each year.1 These patients represent a substantial diagnostic challenge, as urine culture results are generally not available, and both urine reagent strips and urinalysis with microscopy demonstrate poor test characteristics in ED patients.2,3 UTI diagnoses in older adults is particularly challenging due to atypical presentations, asymptomatic bacteriuria, and even worse test performance, compared to younger adults.2,3 As a result, it is difficult to accurately and rapidly diagnose acute UTIs in the ED.
One potential strategy to improve diagnostic accuracy uses the innate immune response.4 Antimicrobial peptides (AMPs) are key effectors of innate immunity in the urinary tract that have antimicrobial activity through several mechanisms, including inhibition of bacterial binding, cell lysis, and induction of other immune components.4 Preliminary studies have documented increased urinary levels of several AMPs in response to infection.4 Human neutrophil peptides 1–3 (HNP1-3) are bactericidal alpha-defensins expressed in neutrophils and the kidney that increase in the setting of pyelonephritis.5 Human α-defensin 5 (HD5) is produced in urinary tract epithelial cells and is increased in UTI in children.5 Human beta defensin 2 (hBD-2) is produced in distal nephron epithelial cells, and becomes detectable in UTI.5 Cathelicidin (LL-37) displays vitamin D dependent expression in neutrophils and epithelial cells, and is induced with UTI.4–6
Our goal was to determine if urinary levels of AMPs increase with positive urine cultures in ED adults. We hypothesized that AMP levels would be greater in those with positive culture, including the older adult subgroup.
METHODS
Study Design
This was a prospective observational study. Institutional review board approval was obtained from the Ohio State University (which includes Nationwide Children’s Hospital through a cooperative agreement) and the Massachusetts General Hospital. Informed consent was obtained from all subjects.
Study Setting and Population
The study included a convenience sample of adult patients with suspected UTI presenting to our urban, academic ED (OSU Wexner Medical Center) from January 1, 2014 through March 30, 2014. Inclusion criteria were age older than 17 years and completion of a urine culture. Exclusion criteria included incarceration, suicidal or homicidal ideation, prior enrollment, and presenting as a trauma alert.
Study Protocol
Study staff identified patients in real time on weekdays from 8AM to 9PM. Patients completed an initial survey covering demographics, symptoms, and medical history, and provided urine and blood samples. Electronic medical record chart review (EPIC, EPIC Systems Corp., Verona, WI) was used to record vital signs, diagnostic study results, and disposition.
Urine was collected using standard clinical procedures (clean-catch or catheter). Both urine and serum were centrifuged and stored at −80°C. Enzyme-linked immunosorbent assays (ELISA) were performed using HNP1-3 Human ELISA Kit (Hycult Biotech-Plymouth Meeting, PA), Defensin-5 ELISA kit (Lifeome Biolabs-Oceanside, CA), Human Beta Defensin 2 ELISA Kit (Lifeome Biolabs), and LL-37 Human Elisa Kit (Hycult Biotech). For all but HNP 1-3, ELISA results were divided by urine creatinine (measured using the Oxford Biomedical Research creatinine microplate assay, Rochester Hills, MI) to standardize for urine concentration. Samples were run in duplicate. Serum 25-hydroxyvitamin D (25OHD) levels were measured by liquid chromatography-tandem mass spectrometry.
Measures
Because the traditional cutoff of 105 cfu/mL may be overly restrictive in symptomatic patients, a positive urinary culture was defined as >104 cfu/mL of one to two organisms from a female clean-catch specimen, or >103 cfu/mL from a catheterized specimen, a male specimen, or a specimen from a chronic indwelling catheter.7,8 Urinary tract symptoms included fever, urgency, frequency, suprapubic pain, dysuria, flank pain, hematuria, or new incontinence. In patients with chronic catheterization, they also included fever or altered mental status without other source.
Data Analysis
Analyses were performed using STATA v.12. Descriptive statistics are reported as proportions, means with standard deviation (±SD), or medians with interquartile range (IQR). Continuous variables were tested for normality using the Shapiro-Wilk test. Comparisons between groups were performed using Wilcoxon rank sum tests. We constructed receiver operating characteristic (ROC) curves and calculated area under the curve (AUC) with 95% confidence intervals (CI). Results are also reported for the older adult subgroup. Because this was the first study of its kind and AMP levels were unknown, we were unable to perform a priori power calculations, but chose a sample size of 40 subjects based on capacity of the ELISA plates used in the study.
RESULTS
We enrolled 40 patients with mean age of 57 years (SD ±21 years). Twenty-three (58%) were ≥ 65 years, 25 were female (64%), and 33 (83%) were white. Comorbidities included diabetes in 12 (31%), cardiac disease (myocardial infarction or heart failure) in eight (20%), stroke in five (12%), and immunosuppression in 18 (45%), including 11 with cancer and three with organ transplant. Thirty (75%) reported at least one urinary symptom, including fever (n = 11, 27%), urgency (18, 45%), frequency (13, 32%), suprapubic pain or dysuria (15, 38%), flank pain (6, 29%), hematuria (9, 22%), incontinence (8, 20%), or confusion (12, 30%).
Thirty-eight patients had microscopic urinalyses: 20 (53%) had leukocyte esterase, three (7.9%) had nitrites, and 14 (27%) had bacteria. Cultures were positive in 13 of 40 (32%), one with two organisms. Seven of 23 older adults had positive cultures. Identified organisms included Escherichia coli (3), Citrobacter (2), Klebsiella pneumoniae (2), Morganella morganii (1), Lactobacillus-like (1), Staphylococcus aureus (2), Staphylococcus saprophyticius (1), Enterococcus faecalis (1), and Gardnerella vaginalis-like (1). Patients ≥ 65 years accounted for seven of the 13 positive cultures (54%). Urinary symptoms were present in 12 of 13 with positive cultures.
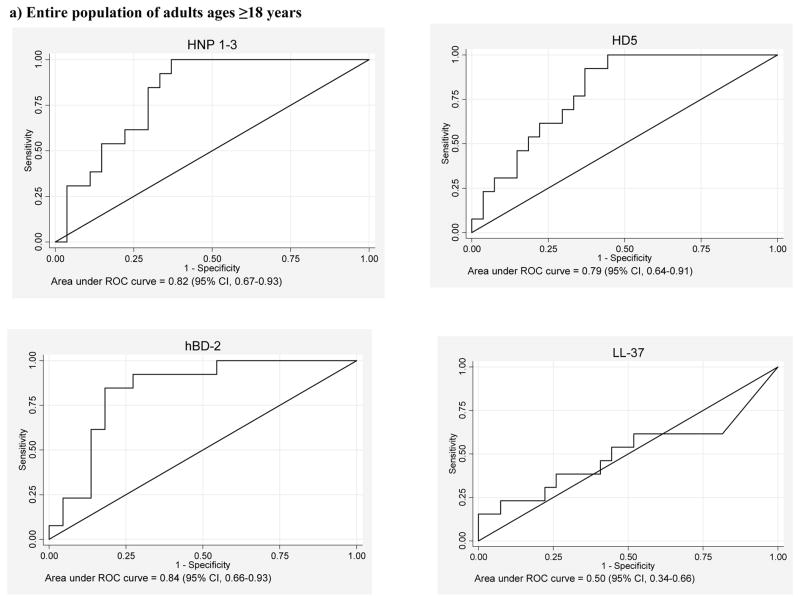
HNP 1-3, HD5, and hBD-2 levels were significantly higher in those with positive than negative urine cultures, and AUCs were > 0.75 (Figure 1). In patients with positive compared to negative cultures, median HNP1-3 was 5.39 ng/mg (IQR 2.74 to 11.09) vs. 0.81ng/mg (IQR 0.06 to 3.87) (p = 0.001). Median HD5 was 4.75 pg/mg (IQR 1.6 to 22.7) vs. 0.00 pg/mg (IQR 0 to 2.60) (p = 0.002). Median hBD-2 was 0.13 pg/mg (IQR 0.08 to 0.17) vs. 0.02 pg/mg (IQR 0 to 0.04) (p = 0.001). hBD-2 was analyzed in only 35 patients due to a technical problem with the assay.
Figure 1.
Receiver operating curves for urinary antimicrobial peptide detection of positive urine cultures in ED adults
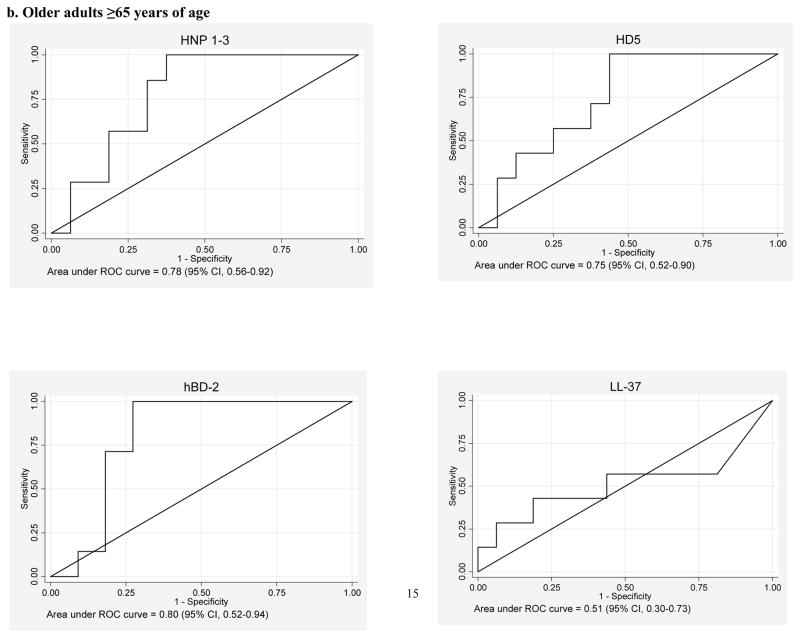
Findings were similar in the older adult subgroup. Median HNP1-3 was 5.39 ng/mg (IQR 2.70 to 12.68) in positive vs. 0.71 ng/mg (IQR 0.02 to 4.42) in negative cultures (p = 0.032). Median HD5 was 4.75 pg/mg (IQR 1.6-to 38.20) vs. 0.06 pg/mg (IQR 0.00 to 7.60) (p = 0.056). Median hBD-2 was 0.13 pg/mg (IQR 0.08 to 0.17) vs. 0.01 pg/mg (IQR 0.00 to 0.09) (p = 0.032). Although HD5 was non-significant, given the mean HD5 and assuming an alpha of 0.05, we had a power of only 0.21 for this comparison.
LL-37 was not significantly higher in patients with positive cultures. Inadequate serum 25(OH)D levels were present in 16 of the 22 subjects (72%) in whom serum was obtained, including eight < 20 ng/mL and eight 20 to 30 ng/mL.
DISCUSSION
Our findings provide the first evidence in an adult, ED population that AMPs may be markers of positive urine culture. If confirmed, AMP levels could result in more timely and accurate UTI diagnosis in acute care, leading to decreases in morbidity, unnecessary antibiotics, and health care costs. These findings represent the recommended first step in the evaluation of novel biomarkers: demonstration of a difference in levels between subjects with and without the outcome.9
Consistent with prior work in other populations, urine levels of HNP 1-3, HD-5, and hBD-2 in patients with positive urine culture were five times or more greater than in culture negative patients. In one study, urine levels of HNP1-3 increased eight-fold in chronic pyelonephritis vs. both controls and patients with glomerulonephritis.5 Urinary HD5 increases in children with bacterial UTI, and hBD-2 becomes detectable in chronic pyelonephritis.5 The extension of these findings to the ED provides novel evidence of the potential use of AMPs as a diagnostic marker in acute care settings.
Diagnosis of UTI in older adults is a particular challenge due to frequent absence of UTI symptoms. In addition, in older ED patients, 30% of reagent strips in the presence of positive culture are negative for both nitrites and leukocyte esterase, and > 50% of positive strips are associated with negative cultures.2 In our subset of older adults, AMP levels were also greater in those with positive cultures.
LL-37 was not increased with positive cultures, which is inconsistent with prior findings where urinary LL-37 increased with bacteriuria.10 However, LL-37 expression is vitamin D dependent, and 67% of study patients had 25(OH)D < 30 ng/mL. Further study is required to understand the relationship between urinary LL-37, vitamin D status, and UTI.
LIMITATIONS
We were unable to control for potential confounders of AMP levels due to the limited sample size in this pilot study. We report positive urinary cultures as distinct from symptomatic urinary tract infection. It is unclear how asymptomatic bacteriuria may affect AMPs, but only one patient had asymptomatic bacteriuria, and removing this patient from the analysis did not change conclusions. We did not examine differences in AMPs in pyelonephritis versus cystitis. However, as only six patients reported flank pain, the observed increases in AMPs included a substantial proportion of patients with cystitis. We were also unable to determine what effects seasonality could have on AMPs, for example by altering serum vitamin D status.
CONCLUSIONS
Urinary levels of HNP1-3, HD-5, and hBD-2 are significantly greater in the presence of positive urine cultures in ED patients with suspected urinary tract infection. These findings were maintained in the subgroup of older adults.
Footnotes
Presentations: none
Disclosures: Dr. Caterino’s work on this study was supported in part by 1K23AG038351-01 from the National Institute on Aging.
References
- 1.Caterino JM, Ting SA, Sisbarro SG, Espinola JA, Camargo CA., Jr Age, nursing home residence, and presentation of urinary tract infection in U.S. emergency departments, 2001–2008. Acad Emerg Med. 2012;19:1173–80. doi: 10.1111/j.1553-2712.2012.01452.x. [DOI] [PubMed] [Google Scholar]
- 2.Ducharme J, Neilson S, Ginn JL. Can urine cultures and reagent test strips be used to diagnose urinary tract infection in elderly emergency department patients without focal urinary symptoms? CJEM. 2007;9:87–92. doi: 10.1017/s1481803500014846. [DOI] [PubMed] [Google Scholar]
- 3.Lammers RL, Gibson S, Kovacs D, Sears W, Strachan G. Comparison of test characteristics of urine dipstick and urinalysis at various test cutoff points. Ann Emerg Med. 2001;38:505–12. doi: 10.1067/mem.2001.119427. [DOI] [PubMed] [Google Scholar]
- 4.Zasloff M. Antimicrobial peptides, innate immunity, and the normally sterile urinary tract. J Am Soc Nephrol. 2007;18:2810–6. doi: 10.1681/ASN.2007050611. [DOI] [PubMed] [Google Scholar]
- 5.Spencer JD, Schwaderer AL, Becknell B, Watson J, Hains DS. The innate immune response during urinary tract infection and pyelonephritis. Pediatr Nephrol. 2014;29:1139–49. doi: 10.1007/s00467-013-2513-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chromek M, Slamova Z, Bergman P, et al. The antimicrobial peptide cathelicidin protects the urinary tract against invasive bacterial infection. Nature Med. 2006;12:636–41. doi: 10.1038/nm1407. [DOI] [PubMed] [Google Scholar]
- 7.Hooton TM, Roberts PL, Cox ME, Stapleton AE. Voided midstream urine culture and acute cystitis in premenopausal women. New Eng J Med. 2013;369:1883–91. doi: 10.1056/NEJMoa1302186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hooton TM, Bradley SF, Cardenas DD, et al. Diagnosis, prevention, and treatment of catheter-associated urinary tract infection in adults: 2009 International Clinical Practice Guidelines from the Infectious Diseases Society of America. Clin Infect Dis. 2010;50:625–63. doi: 10.1086/650482. [DOI] [PubMed] [Google Scholar]
- 9.Hlatky MA, Greenland P, Arnett DK, et al. Criteria for evaluation of novel markers of cardiovascular risk: a scientific statement from the American Heart Association. Circulation. 2009;119:2408–16. doi: 10.1161/CIRCULATIONAHA.109.192278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van der Starre WE, van Nieuwkoop C, Thomson U, et al. Urinary proteins, vitamin D and genetic polymorphisms as risk factors for febrile urinary tract infection and relation with bacteremia: a case control study. PloS One. 2015;10:e0121302. doi: 10.1371/journal.pone.0121302. [DOI] [PMC free article] [PubMed] [Google Scholar]