Abstract
Depression symptoms are associated with impairments in functioning and have substantial health and economic consequences. Universal substance misuse prevention programs have shown effects on non-targeted mental health-related symptoms, but long-term effects are understudied. This cluster randomized controlled trial examined effects of both the LifeSkills Training (LST) and Strengthening Families Program: For Parents and Youth 10–14 (SFP 10–14) interventions, delivered during seventh grade, on age 22 young adult depression symptoms. The study was conducted in US rural Midwestern communities with a randomly-selected sample from a larger study (N= 670). Experimental conditions were LST+SFP 10–14, LST-only, and a control condition. Effects on age 22 depression symptoms were hypothesized as mediated through effects on age 21 relationship problems and illicit use of substances. Structural equation modeling with manifest and latent variables was conducted to test hypotheses; the intervention conditions were combined and compared with the control condition because analyses indicated a comparable pattern of effects between intervention conditions. Significant indirect intervention effects were found on age 22 depression symptoms via effects on the mediating variables (indirect effect: β=−0.06, 95 % CI [−0.10, −0.01], p=0.011). Effect sizes for the young adult variables were between d=0.17 and 0.29, which can be considered small, but nontrivial, especially in the context of public health benefits. Results support scaled-up implementation of school-based and family-focused universal substance misuse preventive interventions.
Keywords: Preventive intervention, Depression symptoms, Young adult, Mediation
Young adulthood is a critical time to examine depression symptoms because there is increased incidence of major depression during this stage of development, likely influenced by the tasks, transitions and social role changes that occur (Schulenberg and Zarrett 2006). Depression symptoms are associated with impairment in functioning (Rudolph et al. 2006) and with both direct and indirect economic costs. These costs include related medical expenditures, reduced productivity, unemployment, and absenteeism, estimated at more than $75 billion annually (Wade and Häring 2010). Risk factors for depression symptoms include parent–child relationship problems (Hicks et al. 2009), family dysfunction (Côté et al. 2009), and substance misuse (Brook et al. 2002). Because these risk factors are targeted by universal substance misuse preventive interventions, cross-over effects on non-targeted mental health problems have been examined. For example, family-focused universal substance misuse preventive interventions have been shown to significantly affect adolescent and young adult internalizing symptoms (Mason et al. 2007; Trudeau et al. 2007, 2012). However, important research gaps remain regarding developmentally-appropriate mediators of intervention effects. Research indicates that relationship problems and substance misuse predict young adult depression symptoms (Mason et al. 2008; Rao et al. 2000). In addition, these predictors may be influenced by preventive interventions (Atkins et al. 2009; Spoth et al. 2008a), suggesting an important direction for research focusing on the mechanisms of intervention effects.
To address this need, we tested a developmental model that examined the effects of adolescent universal substance misuse preventive interventions on depression symptoms at age 22, mediated through young adult relationship problems and illicit use of substances measured 1 year earlier. We also evaluated developmental sequences, such as reciprocal effects between depression symptoms and the putative mediators during young adulthood (Needham 2008).
Depression Symptoms, Substance Misuse, and Preventive Interventions
Studies have documented the association between depression symptoms and substance misuse (see a review by O’Neil et al. 2011). Mueser and colleagues (2006) articulated four explanatory theoretical models that could apply to the relationship between psychological symptoms and substance misuse: (a) a common factor model (i.e., the association results from shared etiology); (b) a self-medication model (i.e., substances are used to ameliorate existing psychological symptoms); (c) a symptom exacerbation model (i.e., substance misuse can induce subsequent psychological symptoms); and (d) a bidirectional model (i.e., psychological symptoms and substance misuse mutually or sequentially influence one another). Mixed results from causal modeling suggest that explanatory mechanisms may vary by developmental stage, subpopulation, and specific symptom categories (O’Neil et al. 2011). O’Neil et al. have suggested that research examining prevention efforts targeting either substance misuse or internalizing symptoms also examine effects on the non-targeted outcome. Based on findings linking illicit substance use to depression (Substance Abuse and Mental Health Services Administration 2010a), and earlier research demonstrating intervention effects on illicit substances (Spoth et al. 2005, 2014), the current study tested young adult past year illicit use of substances—marijuana, other illicit substances, prescription drug misuse—as a mediator of intervention effects on depression symptoms and also examined the bidirectional, or reciprocal influences, model.
Some meta-analytical reviews evaluating preventive intervention studies targeting depression found stronger effects for interventions conducted with selective or indicated populations than for universal interventions (Horowitz and Garber 2006; Stice et al. 2009). However, a recent Cochrane collaboration review of depression prevention programs (Merry et al. 2011) found that universal preventive interventions are as effective as selective or indicated interventions. In support of Merry et al.’s conclusions, a meta-analysis of programs targeting adolescent substance misuse indicated that universal preventive interventions produced larger effect sizes on tobacco and marijuana use than selective or indicated interventions when analyzed for population-level effects, indicating the public health value of the universal programs (Shamblen and Derzon 2009). In the current study, we expected to find effect sizes comparable to those reported in meta-analyses (i.e., effect sizes at follow-up averaged 0.11; Horowitz and Garber 2006; Stice et al. 2009).
Young Adult Transitions, Tasks, and Relationship Formations
Age 22 typically marks the beginning of major transitions for individuals and their contexts (Schulenberg and Maggs 2002). Many young adults have completed their post-secondary education and are entering the work force full-time (Schulenberg and Zarrett 2006). Typically, those who begin work post-high school, rather than attending post-secondary education, will have established more stable employment by that time (Hamilton and Hamilton 2006). Other major developmental tasks in young adulthood include formation of adult friendships and romantic partner relationships, along with managing changes in family-of-origin relationships (Collins and van Dulmen 2006). These tasks can be influenced by both antecedent and concurrent factors (Atkins et al. 2009), such as substance misuse, history of depression, and family conflict (Mason et al. 2008). Importantly, research has shown that poor young adult interpersonal functioning, especially within a marital relationship, can contribute to depression symptoms (Davila 2011; Whisman 2001); and, conversely, depression expressed in behavioral interactions can lead to problems in interpersonal relationships (Joiner and Timmons 2009).
Preventive interventions have demonstrated influence on a range of relationship skills, encompassing interactions involving family, friends, and romantic partners. Greenberg (2006) suggested that preventive interventions can enhance interpersonal skills by improving executive functions (e.g., inhibitory control, planning, problem solving skills, and emotional regulation). Universal substance misuse preventive interventions also directly address interpersonal relationship skills training (e.g., communication, conflict management, assertiveness; Greco and Morris 2005; Lawrence et al. 2008). Thus, this study posited relationship problems as a mediator of intervention effects on depression symptoms, and also examined the reciprocal relationship between depression and relationship problems.
The Current Study: Preventive Interventions, Moderation, and Hypotheses
To address important gaps in the literature we examined mediators relevant to the young adult developmental stage and extended the follow-up evaluation 10 years past baseline, much farther from intervention implementation than followup studies included in existing meta-analyses (Horowitz and Garber 2006; Merry et al. 2011; Stice et al. 2009). The current study is both a replication and extension of a separate project evaluating effects of the Iowa Strengthening Families Program (Kumpfer et al. 1996) on internalizing symptoms into young adulthood, mediated by adolescent internalizing symptom growth factors (Trudeau et al. 2012). We followed recommendations to examine intervention effects within a developmental framework—longitudinally, examining potential mediators appropriate to a specific stage of development (O’Connell et al. 2009; Sandler et al. 2011).
In combination, the family-focused and school-based universal substance misuse preventive interventions tested in this study focus on parent/adolescent relationships and adolescent socio-emotional skills that are expected to influence both substance misuse and depression symptoms (Biglan et al. 2012; O’Neil et al. 2011). The interventions have demonstrated positive effects on parenting behaviors (Spoth et al. 1998), adolescent skills (Lillehoj et al. 2004; Trudeau et al. 2003), and both substance misuse (Spoth et al. 2008a, b, 2009, 2014) and internalizing symptoms (Trudeau et al. 2007, 2012) in adolescence and young adulthood. The most recent substance misuse outcome study from this project (Spoth et al. 2014), documents effects of the school-based and family-focused interventions on trajectories of adolescent substance initiation (drunkenness, marijuana, inhalants, and tobacco) that predict to effects on substance misuse frequency in young adulthood, ages 19–22 (i.e., drunkenness, alcohol-related problems, cigarettes, and illicit substances). Combined, the intervention effects across time on substance misuse trajectories, related variables (e.g., conduct problems), and the parent/adolescent skills taught in the programs, support the evaluation of long-term effects on depression symptoms, along with the putative mediators.
Although not the primary focus, gender is important to consider. The gender difference in depression symptoms is well-established, with females demonstrating higher levels of depression symptoms beginning around age 12 (Angold et al. 2002). However, research findings on gender differences across predictive factors have not been consistent. Regarding relationship problems and depression, some studies have found that interpersonal stress is a stronger risk factor for depression in women than in men (Nolen-Hoeksema and Hilt 2009; Rudolph 2002), whereas others have found that family relationships have effects on depression for both genders (Eshbaugh 2008; Meadows et al. 2006). Regarding substance misuse and depression, some studies have found that depressed males are more likely to report alcohol and drug use (Marcus et al. 2005) and other studies have demonstrated that both males and females who engage in substance misuse are more likely to exhibit depression (Hallfors et al. 2004). Mixed results also have been found in response to preventive interventions (Mason et al. 2009; Trudeau et al. 2007). These mixed results render it difficult to formulate a predictive hypothesis; therefore, examination of gender differences in this study is exploratory.
Additional risk factors for depression symptoms include earlier substance misuse, family history of depression, and previous depression symptoms (Brook et al. 2002; Downey and Coyne 1990; O’Neil et al. 2011). Baseline measures of these factors were included as control variables.
Based on the literature reviewed above, we hypothesized that (a) participants assigned to the school-based and family-focused intervention conditions would exhibit reduced age 21 relationship problems and illicit use of substances, relative to those in the control condition, (b) age 21 relationship problems and illicit use of substances would be positively associated with age 22 depression symptoms, and (c) there would be an indirect intervention effect on depression symptoms via the hypothesized young adult mediators. We estimated intervention effects on age 20 depression symptoms, both to test for earlier intervention effects and as a means of exploring reciprocal effects between depression symptoms and the young adult mediator variables. Gender differences also were examined.
Method
Sample, Study Design, and Procedures
Initially, participants were seventh grade students and their parents from 36 rural Northeast Iowa school districts. (The earlier study had been conducted in southern Iowa; Trudeau et al. 2007, 2012.) School inclusion criteria were: district rates of free or reduced-cost school lunch program participation ≥20 %, district enrollment <1200, and middle school grades (6–8) located in one building. Guided by a randomized block design, schools were assigned to one of three experimental conditions; those offered the school-based LifeSkills Training (LST) intervention plus the family-focused Strengthening Families Program: For Parents and Youth 10–14 (SFP 10–14) intervention, those offered the LST intervention only, and a minimal contact control condition. Following random assignment, school district staff and families were informed of their experimental condition.
Approximately 20 randomly selected families per school were recruited for in-home assessments (analyzed N=670; 21 individuals were eliminated from the analyzed sample because they changed experimental conditions while in school). A shorter assessment was conducted in schools with additional participants, but did not include several of the measures used in this study. Baseline assessments were conducted during the first semester of seventh grade in 1997, and the age 22 follow-up was conducted in 2008 (N=578; 86.3 % of baseline). At baseline, participants averaged 12.3 years of age, 54 % were male, 99 % were White, and 83 % lived with both biological parents. Median household income was $42,837. At age 22, approximately 13 % reported living with a spouse or romantic partner and approximately 5 % reported living with their child or children. Approximately 64 % reported attending school during the past year. The types of school the participants reported attending most during the past year were: 1 % working for a high school equivalency (GED); 31 % trade school, business school, or community college, and 32 % 4 year college or university. Approximately 35 % reported working full time and approximately 60 % reported working part-time. In addition, approximately 2 % were in the military.
No significant differences were found between the analyzed sample and an earlier survey of eligible families (N=1260) on baseline demographic variables (e.g., income, race, marital status, parents’ education and employment) and child behavior problems. Additionally, no significant differences were found between conditions on demographics. Attrition analyses indicated no significant condition by dropout status differences on demographic measures and no differences on baseline covariates.
The university Institutional Review Board approved the study and APA ethical standards were followed; family members signed consent forms and were compensated for their time. Adolescent participants and their parents completed written questionnaires independently during in-home interviews. Following the 12th grade, young adult data collection was conducted via computer-assisted telephone interviews, supplemented by mailed questionnaires. The primary interventions were conducted in the seventh grade, following baseline data collection; booster programs also were offered.
Interventions
LifeSkills Training (LST)
LST is based on social learning theory (Bandura 1977) and problem behavior theory (Jessor and Jessor 1977). The goal is to promote skill development (e.g., substance use refusal skills, self-management, general social skills; Botvin 2000). The 15-session program was taught by trained teachers during 40 to 45 min classroom periods who used interactive techniques (e.g., coaching, role modeling, feedback, reinforcement), plus homework assignments and out-of-class behavioral rehearsal. All seventh grade students were offered the LST intervention; a passive consent procedure allowed parents to decline participation for their child, and children were allowed to refuse consent on their own. Although attendance at LST sessions was not monitored, participation in the in-school assessments was high (3.6 % were not consented).
Skill development is accomplished through five curriculum components: 1) the cognitive component presents information about the consequences of substance use, substance use norms, and social acceptability; 2) the self-improvement component entails the formation of self-image and the process of self-image improvement; 3) the decision-making component addresses a strategy for decision-making, social pressures influencing decision-making, and recognizing persuasive strategies; 4) the coping with anxiety component is designed to recognize anxiety-inducing situations and practice strategies to cope with anxiety; and 5) the social skills training component includes material on communication, assertiveness, boy-girl relationships, and resisting peer pressure. Trained observers evaluated each teacher on two or three occasions; the average rate of adherence to instructional content was 85 %.
Students participated in five booster sessions in eighth grade to promote skill development—primarily social resistance skills, self-management skills, and generic social skills; the average rate of adherence was 82 %. Four booster sessions focusing on social interaction skills (e.g., assertiveness, conflict resolution, and coping with anxiety and anger) were conducted during 11th grade for a randomly-selected half of the schools; average adherence rate was 77%. More detail regarding implementation fidelity can be found in Spoth et al. (2002a).
Strengthening Families Program: For Parents and Youth 10–14 (SFP 10–14)
SFP 10–14 is a seven-session, interactive program based upon empirically-supported family risk and protective factors (Molgaard et al. 2000). Goals include enhancement of parental skills in nurturing, limit-setting, and communication, as well as youth prosocial behaviors. All families selected for the in-home assessments were recruited to participate in SFP 10–14 and other families were allowed to participate as well (eight non-assessed families participated). Of the original in-home assessed 223 LST+SFP 10–14 condition families, 127 (57 %) families attended at least one session, 115 (89 %) of those families attended four or more sessions, and 82 (64 %) attended six or all seven sessions. Recruitment rates for similar studies have averaged between 3 and 35 % participation (Spoth et al. 2007).
SFP 10–14 sessions included a separate, concurrent 1-h parent and youth skills-building curriculum, followed by a 1-h conjoint family curriculum during which parents and youth practiced skills learned in their separate sessions. Sessions were interactive and used videotapes that model positive behavior to build skills. The youth sessions focused on strengthening future goals, dealing with stress and strong emotions, enhancing responsibility, and responding appropriately to peer pressure. Parent sessions included discussion of social influences and developmental characteristics of youth, providing nurturing support, setting appropriate limits, and following through with consequences. Each session required three trained facilitators, one for the parent session and two for the youth session. Trained observers evaluated adherence, which averaged 98 % in the family sessions, 92 % in the parent sessions, and 94 % in the youth sessions.
Four SFP 10–14 booster sessions were offered the following year. Ninety of the families attending at least one of the earlier sessions also attended at least one booster session (70 %), and 80 (62 %) attended all four booster sessions. Observer-based adherence assessments averaged 97 % for the family sessions, 94 % for the parent sessions, and 96 % for the youth sessions. More detail regarding implementation fidelity can be found in Spoth et al. (2002a).
SFP 10–14 booster sessions also were offered to six of the 12 LST+SFP 10–14 condition schools in the 11th grade (in addition to the LST 11th grade booster sessions). Boosters included: (a) a parenting videotape plus a self-assessment questionnaire—78 (68 %) questionnaires were returned; (b) a family-school resource fair and resource directory—attended (by at least one family member) by 110 individuals (40 % of all eligible families); and (c) a goal-setting seminar presented to 180 students (65 % of those eligible). It is important to note that earlier analyses of differences between schools that received 11th grade boosters and those that did not have not revealed any differences in later rates of substance misuse.
Minimal Contact Control Condition
Control group families were mailed a handout describing aspects of adolescent development.
Measures
Young Adult Depression Symptoms
The Diagnostic Interview Schedule (Helzer and Robins 1988), administered by trained computer assisted telephone interviewers (CATI), assessed depression symptoms. Presence of each symptom was scored 0 = (no) or 1 = (yes) and summed for each of four categories that formed indicators for the latent Depression Symptoms variable measured at ages 20 and 22. General Symptoms included seven items, such as “In the last 2 years, have you ever had 2 weeks or longer when nearly every day you felt sad, empty, or depressed for most of the day?” (α=0.85). Eating and Sleeping Problems had seven items, with the stem “When you were feeling sad, empty or depressed or had lost interest in most things you usually enjoyed…” Items included “Did you have less appetite than usual almost every day?” (α=0.80). The Cognitive Problems category had eight items with the same stem as the eating/sleeping problems items, such as “Did your thoughts come much slower than usual or seem mixed up?” (α=0.90). The Self-harm category included four items with the same stem, such as “Did you think a lot about death?” (α=0.70).
Age 21 Relationship Problems
Four relationship-specific items were taken from a mail-in questionnaire that presented a list of past year life events and were scored 0 = (no) or 1 = (yes) for whether or not the event occurred. The item stem was “During the past 12 months did you…” Items were (1) “Get a divorce or separate from a spouse or romantic partner you lived with because of relationship difficulties?” (2) “Have a steady, romantic relationship breakup?” (3) “Have any serious, ongoing tensions, conflicts, or arguments with a close friend or romantic partner?” and (4) “Have any serious, ongoing tensions, conflicts, or arguments with a family or household member?” Items were summed; 67% reported no relationship problems. Cronbach’s alpha was 0.58. A high degree of internal consistency was not necessarily expected, as this type of scale is composed of causal indicators that may or may not be related to one another (Streiner 2003). Also, this measure could be viewed as a relationship checklist, assessing multiple relationship dimensions such as friendship, romantic and familial; these may or may not be associated but are important to assess (Herbert and Cohen 1996).
Age 21 Illicit Use of Substances
This latent variable was comprised of three indicators assessed during the CATI interview. Marijuana Use was assessed with the question, “In the past year, how many times have you used marijuana?” To improve the distributional quality, the open-ended question was rescaled so that 1=(0), 2=(1–2), 3=(3–6), 4=(7–12), and 5=(13+). Other Illicit Drug Use was assessed with a series of open-ended questions with the stem “In the past year, how many times have you used…” and addressed the use of cocaine, ecstasy, methamphetamine, and hallucinogens. Responses to each question were coded 0 = (0) or 1 = (once or more) and summed. Prescription Drug Misuse was assessed with a series of questions using the same stem and included the use of Vicodin, amphetamines, barbiturates, and tranquilizers, “…not under a doctor’s order.” Responses to each question were coded 0 = (0) or 1 = (once or more) and summed. For the three Illicit Use of Substances indicator items, combined Cronbach’s alpha, based on standardized composite scores, was 0.69. Approximately 80 % reported no illicit use of substances.
Intervention and Control Variables
Intervention Condition was coded 0 = (control) or 1 = (LST+SFP 10–14 plus LST-only) and Gender was coded 0 = (female) or 1 = (male). Control variables at baseline included Adolescent Depression Symptoms, assessed with six items from the Child Behavior Checklist-Youth Self-Report (Achenbach and Rescorla 2001), e.g., “I cry a lot,” “I deliberately try to hurt or kill myself,” (α=0.69). Parent Depression Symptoms were assessed with 13 items from the Symptom Check List-Revised (SCL-90-R; Derogatis 1983), such as “Feeling low in energy or slowed down,” “Feeling hopeless about the future.” Mother and father reports were averaged if both parents’ reports were available; otherwise, one parent’s report was used (combined mother and father α=0.90). Adolescent Substance Initiation was assessed with items that were scored 0 = (no initiation) or 1 = (initiation) for the following: alcohol (more than just a few sips), drunkenness, tobacco (cigarettes, chew, cigars), marijuana, and inhalants. Items were summed to form a scale ranging from 0 to 5. Approximately 74 % had not initiated any substances at baseline. We did not control for earlier levels of relationship problems, because the only proxy available in our data – baseline parent–child affective quality – was not significantly related to age 21 relationship problems (r=−0.02, p=0.708).
Data Analysis
Table 1 presents the means, standard deviations, and correlations of the ages 20–22 study variables by intervention condition. All participants were included in the analyses, whether or not they attended the intervention programs (i.e., intent-to-treat analyses). Hypotheses were investigated utilizing structural equation modeling (SEM) conducted with Mplus 7.11 (Muthén and Muthén 1998–2010), using MLR (i.e., maximum likelihood robust) estimation with robust standard errors and a mean-adjusted chi-square test statistic to adjust for non-normality. Analyses controlled for multilevel effects, that is, nesting within school districts, by using the TYPE = COMPLEX command, specifying the school district as the unit of clustering and adjusting the standard errors accordingly (Raudenbush and Bryk 2002). Full-information maximum likelihood estimation addressed missing data (Allison 2003; Schafer and Graham 2002). Latent variables were utilized for constructs where possible, thereby limiting measurement error and increasing statistical power (McClelland and Judd 1993). Model fit was assessed using chi-square and the CFI and RMSEA fit indices (CFI >0.95 and RMSEA <0.06 are considered good fit; Hu and Bentler 1999).
Table 1.
Means, standard deviations, and correlations of young adult variables by intervention condition
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | Mean | SD |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 Marijuana use (age 21) | – | 0.53 | 0.48 | 0.07 | 0.19 | 0.22 | 0.24 | 0.13 | 0.27 | 0.21 | 0.30 | 0.29 | 1.372 | 1.013 |
| 2 Other illicit drug use (age 21) | 0.30 | – | 0.72 | 0.09 | −0.05 | 0.05 | 0.01 | 0.05 | 0.17 | 0.18 | 0.19 | 0.20 | 0.084 | 0.416 |
| 3 Prescription drug misuse (age 21) | 0.26 | 0.48 | – | 0.05 | 0.01 | 0.05 | 0.02 | −0.03 | 0.08 | 0.13 | 0.09 | 0.08 | 0.100 | 0.431 |
| 4 Relationship problems (age 21) | 0.05 | 0.01 | −0.03 | – | 0.11 | 0.15 | 0.17 | 0.06 | 0.28 | 0.40 | 0.34 | 0.16 | 0.646 | 0.938 |
| 5 General depression (age 20) | 0.11 | −0.02 | 0.02 | 0.22 | – | 0.84 | 0.84 | 0.42 | 0.26 | 0.23 | 0.28 | 0.13 | 0.968 | 1.758 |
| 6 Eat/sleep symptoms (age 20) | 0.14 | 0.00 | 0.03 | 0.15 | 0.84 | – | 0.83 | 0.36 | 0.19 | 0.22 | 0.24 | 0.30 | 0.732 | 1.390 |
| 7 Cognitive symptoms (age 20) | 0.12 | 0.02 | 0.06 | 0.22 | 0.88 | 0.78 | – | 0.41 | 0.19 | 0.22 | 0.24 | 0.19 | 1.147 | 2.170 |
| 8 Self-harm symptoms (age 20) | 0.17 | 0.01 | 0.01 | 0.24 | 0.45 | 0.34 | 0.51 | – | 0.27 | 0.13 | 0.30 | 0.33 | 0.116 | 0.421 |
| 9 General depression (age 22) | 0.18 | 0.01 | −0.02 | 0.19 | 0.38 | 0.26 | 0.35 | 0.30 | – | 0.83 | 0.90 | 0.64 | 0.715 | 1.596 |
| 10 Eat/sleep symptoms (age 22) | 0.12 | 0.10 | 0.10 | 0.19 | 0.31 | 0.27 | 0.32 | 0.22 | 0.80 | – | 0.80 | 0.36 | 0.503 | 1.169 |
| 11 Cognitive symptoms (age 22) | 0.15 | 0.05 | 0.04 | 0.20 | 0.39 | 0.27 | 0.37 | 0.29 | 0.87 | 0.81 | – | 0.65 | 0.834 | 2.055 |
| 12 Self-harm symptoms (age 22) | 0.18 | 0.08 | 0.05 | 0.18 | 0.30 | 0.25 | 0.33 | 0.19 | 0.54 | 0.51 | 0.61 | – | 0.104 | 0.467 |
| Mean | 1.431 | 0.054 | 0.021 | 0.443 | 0.791 | 0.579 | 0.899 | 0.086 | 0.510 | 0.414 | 0.569 | 0.076 | ||
| SD | 1.019 | 0.286 | 0.159 | 0.783 | 1.614 | 1.248 | 2.009 | 0.380 | 1.230 | 1.107 | 1.534 | 0.403 |
Significant correlations (p<0.05) are in boldface. Correlations for the control group participants (n=219) are presented above the diagonal and correlations for intervention group participants (n=451) are presented below the diagonal. Means and standard deviations for the control group participants are presented in the vertical columns and means and standard deviations for the intervention group participants are presented in the horizontal rows. For all scales, higher scores are indicative of a greater degree of the constructs assessed.
Gender moderation was evaluated using a two-group model. Structural parameters were constrained to equality across the groups and then allowed to vary. Model fit for the comparison utilized the Yuan-Bentler T2* test statistic, an empirically-supported test developed to adjust for clustered sampling and conditions of multivariate non-normality (Fouladi 2000; Muthén and Muthén 1998–2010).
Results
For purposes of this study, the two preventive intervention conditions were combined and compared with the control condition for three reasons: (a) a non-significant difference between the two intervention conditions was found on age 22 depression symptoms (t(383)=1.16, p=0.246), (b) a stacked model revealed a non-significant difference in the structural parameters between the two intervention conditions (Δχ2, (19)=24.20, p=0.188), and (c) models conducted with each intervention separately versus the control condition produced the same pattern of results and significance levels as the combined condition model. For example, the indirect intervention effect on age 22 depression symptoms was β=−0.07, p=0.014 for LST+SFP 10–14 vs. control and β=−0.07, p=0.003 for LST only vs. control.
Testing the Hypothesized Mediating Model
Direct Effects
First, before testing our mediating hypotheses, we empirically established the direct effect of the interventions on age 22 depression symptoms by testing an unmediated direct effect SEM, including control variables. Results revealed a significant intervention effect on age 22 depression symptoms; β=−0.08, 95 % CI [−0.16, −0.00], p=0.042.
Hypothesized Indirect Effects
Next, a SEM was used to test the hypothesized mediating relationships. Figure 1 illustrates the tested model; arrows represent the regression paths and bold represents statistical significance. The regression pathways depict: the influence of the intervention conditions (versus the control condition) on age 20 depression symptoms, age 21 relationship problems, and age 21 illicit use of substances; in turn, pathways depict the influences of age 21 relationship problems and age 21 illicit use of substances on age 22 depression symptoms, representing the mediational pathways. The path from age 20 depression symptoms to age 22 depression symptoms represents the stability coefficient.
Fig. 1.
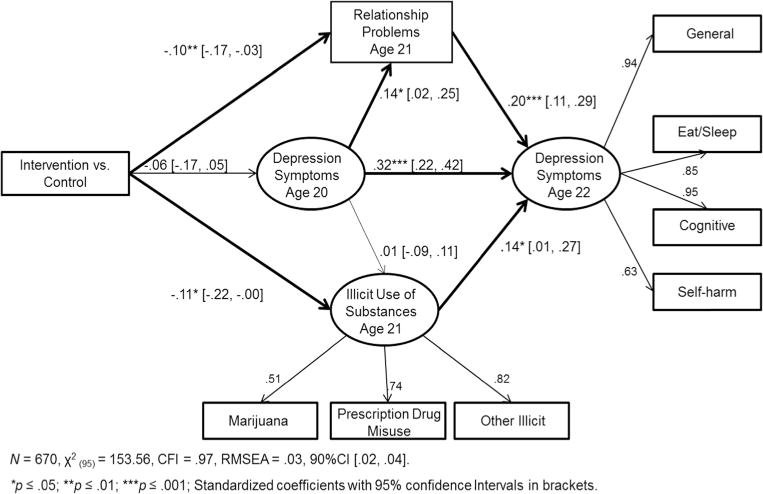
Effects of universal preventive interventions on young adult depression symptoms
Note: Age 20 Depression Symptoms were measured with indicators identical to Age 22 Depression Symptoms (not depicted). Correlations between Age 21 variables were allowed, as were correlations between Depression Symptom indicators at Age 20 and 22. Intervention indirect effects on Age 22 Depression Symptoms: β = −.06 [−.10, −.01], t= −2.55, p = .011.
Model fit was good (χ2, (95)=153.36, p<0.001), CFI=0.97, RMSEA=0.03, 90 % CI [0.02, 0.04]). Although the chi-square was significant, the CFI and RMSEA were indicative of a good fit. Findings included a non-significant negative path from intervention condition to age 20 depression symptoms (β=−0.06, n.s.) and significant negative paths from intervention condition to age 21 relationship problems (β=−0.10, p≤0.01) and age 21 illicit use of substances (β=−0.11, p≤0.05). In turn, significant paths were found from relationship problems (β=0.20, p≤0.001) and illicit use of substances (β=0.14, p≤0.05) to age 22 depression symptoms, along with a significant stability coefficient from age 20 to age 22 depression symptoms (β=0.32, p≤0.001). The indirect effect from intervention condition through the mediators to depression symptoms was significant; β=−0.06, p=0.011. Covariates were taken into account by regressing the age 20 and 21 variables on all covariates; however, age 22 depression symptoms was not regressed on the covariates because there was very little additional variance accounted for by including the covariates (Δχ2, (4)=2.39, p=0.664) and the difference in the beta weights for the variables of interest was negligible.
Last, to further substantiate the findings for the hypothesized mediation of the intervention effects on age 22 depression symptoms, a direct path was added to the indirect effects model from intervention condition to age 22 depression symptoms. The direct path, although not zero, was non-significant (p=0.430), model fit did not improve (Δχ2, (1)=0.60, p=0.438), and the indirect effect remained significant, suggesting the intervention effect on depression symptoms was primarily mediated (see Fritz and MacKinnon 2007; the percentage of mediation was approximately 71 %.) Thus, our three hypotheses were confirmed: (a) participants assigned to the school-based and family-focused intervention conditions exhibited reduced age 21 relationship problems and illicit use of substances, relative to those in the control condition; (b) age 21 relationship problems and illicit use of substances were positively associated with age 22 depression symptoms; and (c) there was an indirect intervention effect on depression symptoms via the hypothesized young adult mediators.
Examining Reciprocal Effects, Moderation, and Practical Significance
A reciprocal effect was found between depression symptoms and relationship problems; age 20 depression symptoms were positively related to age 21 relationship problems (β=0.14, p≤0.05), and, in turn, age 21 relationship problems were positively related to age 22 depression symptoms. The relationship between illicit use of substances and depression, however, was unidirectional; age 21 illicit use of substances was positively related to age 22 depression symptoms, but age 20 depression symptoms did not significantly influence age 21 illicit use of substances (β=0.01, n.s.)
To evaluate gender differences, a two-group model was tested. There was a non-significant overall gender difference (Δχ2, (8)=4.36, p=0.823), and no single pathway was significantly different across gender groups. Results indicated that the interventions influenced the mediators similarly for males and females, and that relationship problems and illicit use of substances influenced depression symptoms similarly across genders as well.
In order to more clearly assess the practical significance for population-level impact of the interventions, effect sizes were calculated from the path model, stacked by intervention condition, utilizing estimates of manifest and latent variable means and variances. For relationship problems, the effect size was d=0.25. For the illicit use of substances latent variable, the effect size was d=0.29. The age 22 depression symptom latent variable effect size was d=0.17. All effect sizes were in the small range (around d=0.20).
Discussion
This study addresses a gap in the literature on the prevention of depression symptoms, which are associated with impairments in functioning and substantial health and economic consequences. The literature has supported the efficacy of universal preventive interventions for depression, but a limited number of studies have followed participants long-term, up to 10 years past baseline, as we have in this study. We have also contributed to the literature by evaluating developmentally-appropriate intervention mediators.
We evaluated the effects of school-based and family-focused universal substance misuse preventive interventions, implemented during adolescence, on age 22 depression symptoms. Support was found for the mediational hypothesis; assignment to the intervention conditions was associated with significantly lower age 21 relationship problems and illicit use of substances, which, in turn, demonstrated significant effects on age 22 depression symptoms, yielding a negative indirect intervention effect on that outcome. Although indications of population-level effects (i.e., effect sizes) were relatively small (e.g., d=0.17 for depression symptoms, d=0.29 for illicit use of substances), they were similar to the average effect sizes reported in meta-analyses of preventive interventions specifically targeting depression that had follow-up reports of shorter duration (i.e., up to 3 years: Horowitz and Garber 2006, d=0.11; Stice et al. 2009, r=0.11). The average effect size for universal substance misuse prevention programs is estimated at d=0.20 (Shamblen and Derzon 2009). In this context, McCartney and Rosenthal (2003) suggest that the importance of an effect size is determined by logic, not just convention-related labels of a small, medium, or large effect. Small effects sizes suggest potential for public health impact when interventions are scaled-up, as has been indicated by earlier studies on aspirin use (Steering Committee of the Physicians’ Health Study Research Group 1989).
The fact that the interventions were designed to reduce substance misuse, rather than directly targeting depression symptoms, warrants further discussion. O’Neil and colleagues (2011), in a review article examining the empirical literature on the relationship between substance misuse and internalizing disorders, suggested that interventions targeting either one of these two problems be assessed for secondary effects on the other. The relationship between substance misuse and depression likely is complex and may be explained by multiple factors, including shared etiology, self-medication, substance misuse leading to depression symptoms, or bi-directionality (Mueser et al. 2006); there is, however, a body of work that supports the conclusion that shared etiology explains a large part of the co-occurrence of psychological and behavioral disorders (Biglan et al. 2012). These causal factors may help explain the cross-over effects of the interventions on depression symptoms. The SFP 10–14 and LST interventions address risk and protective factors that have been shown in past research to influence parenting and parent–child relationships (Spoth et al. 1998; Redmond et al. 2009), adolescent skills (Lillehoj et al. 2004; Redmond et al. 2009; Spoth et al. 2002a, b; Trudeau et al. 2003), and substance misuse (Spoth et al. 2005, 2008a; Spoth et al. 2009, 2014). Together, these factors likely led to a developmental cascade, whereby positive changes in one domain influenced positive changes in another (Masten and Cicchetti 2010). Interestingly, the intervention effect on age 20 depression symptoms did not reach significance, suggesting that effects may develop over time. Risks and vulnerabilities, as well as strengths and protective factors, can change across developmental stages (O’Connell et al. 2009). At age 22, many individuals had finished post-secondary education (including traditional 4-year college, junior college, trade school, military, or on-the-job training) and had begun establishing a career path and initiating more stable intimate relationships. Those who began work directly out of high school may also have stabilized their work activities 4 years past high school (Hamilton and Hamilton 2006) and perhaps entered into more stable relationships as well. Our results suggest an advantage for intervention condition participants during that transition.
Findings substantiate earlier research evidence of a strong association between relationship problems and depression symptoms (e.g., Aquilino 2006; Davila 2011) and support findings that relationship problems and depression symptoms reciprocally influence one another (Joiner and Timmons 2009; Needham 2008). Interpersonal distress can cause, intensify, or prolong depression symptoms, and depression symptoms create vulnerability to greater interpersonal distress through negative expectations regarding the behavior of others, erosion of support, and greater difficulty in normal role performance (Beach and O’Mahen 2000).
Intervention effects on illicit use of substances were expected, based on earlier evaluations that demonstrated effects on adolescent and young adult substance misuse (Spoth et al. 2005; 2008a; Spoth et al. 2009, 2014). Likewise, the influence of illicit use of substances on depression symptoms is consistent with earlier studies (O’Neil et al. 2011). Our analysis indicated that age 20 depression symptoms did not significantly influence age 21 illicit use of substances, but that age 21 illicit use of substances influenced age 22 depression symptoms, a developmental pattern consistent with some earlier research on the influence of these variables on one another across stages of development (Brook et al. 2002). The relationship between substance use and internalizing symptoms is complex, however, and likely varies across developmental stages, symptom categories, and subpopulations. Our developmental model’s specific measures of substance misuse and depression symptoms, along with intervention effects, control variables and time frame, adds to the literature regarding the relationship between these variables, but caution should be used in interpretation beyond the specifics of the study.
Gender moderation of the structural paths was evaluated and we found that pathways were not significantly different for males and females. Previous research has been mixed; some previous research has suggested females would demonstrate a stronger association between relationship problems and depression symptoms and males would be more likely to demonstrate a stronger association between illicit use of substances and depression symptoms (Marcus et al. 2005; Nolen-Hoeksema and Hilt 2009; Rudolph 2002). However, we found that, although females demonstrated a significantly higher level of overall depression symptoms, relationship problems and illicit use of substances had similar effects on depression symptoms for both males and females, consistent with other prior research (Eshbaugh 2008; Hallfors et al. 2004; Meadows et al. 2006). Differences in research results often can be attributed to differences in the populations studied (e.g., cohort or age-related differences, differences in sample location, differences in ethnicity or culture), differences in measurement, or other differences in methodology. While our study contributes to the body of research on this topic, it is important to note that studies with different populations and methodologies may differ in their results. A key finding from our study, however, is that intervention effects on both relationship problems and illicit use of substances were similar for males and females, supporting the implementation of these specific interventions to both genders in early adolescence.
The limitations of the study should be considered. First, study participants were White, rural Midwesterners from relatively small communities. Some studies have reported a lower level of illicit use of substances among rural populations (Substance Abuse and Mental Health Services Administration 2010b), while other studies indicate a more comparable use rate (Peen et al. 2010), or a higher use rate for certain illicit substances (e.g., methamphetamine; Lambert et al. 2008). Prevalence rates of depression have been found to be higher in rural populations in some studies (Probst et al. 2005), but higher in urban areas in other studies (Peen et al. 2010). Researchers have suggested that variations in poverty and other socio-economic factors are more influential than urban or rural place of residence (Judd et al. 2002). Replications with different demographic populations are recommended. Another limitation is the reliance on self-reports (although a variety of self-report methods were used). It is possible that alternative data collection methods and/or reporters of the constructs would yield somewhat different results. Note that the current study tested developmentally appropriate young adult mediators of intervention effects, rather than tests of intervention effects on adolescent mediators. Earlier research has found weak support for hypothesized intervention mechanisms across developmental stages (Stice et al. 2010). Further research is needed to test additional elements in the sequence of intervention-induced effects extending from adolescence into young adulthood and to examine other potential moderators, such as college attendance, along with further studies on the effects of the 11th grade booster sessions on young adult variables.
In summary, this study supports the long-term effects of the LST and LST+SFP 10–14 interventions on young adult depression symptoms, mediated through earlier effects on relationship problems and illicit use of substances, supplementing research that has supported long-term intervention effects on substance misuse (Spoth et al. 2014). Although differences between the LST-only and LST+SFP 10–14 conditions were non-significant for the current studied outcomes, previous work has demonstrated added value for the combined interventions on several substance misuse variables at some time points; for example, alcohol, tobacco and marijuana initiation at 1 year follow-up (Spoth et al. 2002b), and at 2 year followup (Spoth et al. 2005), and prescription drug misuse in the 11th and 12th grades (Spoth et al. 2008b). In addition, an earlier study with a similar version of SFP 10–14 found stand-alone benefits on substance misuse, conduct problems, and internalizing without implementing an additional school-based intervention; however, the current study design doesn’t allow for disentangling effects of SFP 10–14 only (Spoth et al. 2009; Trudeau et al. 2007, 2012). This study further supports the potential public health impact of larger-scale implementation of the universal school-based and family-focused interventions evaluated in this report. A key conclusion in Shamblen and Derzon’s (2009) meta-analytical report is that universal prevention programs clearly can be more effective and cost effective than selective or indicated programs—both at the individual and population level. More generally, this study’s findings indicate the potential value of implementing preventive interventions shown to produce positive effects on a range of risk and protective factors (e.g., family functioning, adolescent socio-emotional and executive functioning skills) for the reduction of depression symptoms into young adulthood.
Acknowledgments
This research was supported by the National Institute on Drug Abuse, grant DA 010815, a longitudinal study known as the Capable Families and Youth study. The authors wish to thank the individuals and communities that participated in the study and the many staff members and associates who collected the data and assisted with data management and analyses.
Footnotes
Conflict of Interest
The authors declare that they have no conflict of interest.
Contributor Information
Linda Trudeau, Email: ltrudeau@iastate.edu, Partnerships in Prevention Science Institute, Iowa State University, 2625 N. Loop Drive, Suite 2400, Ames, IA 50010, USA.
Richard Spoth, Partnerships in Prevention Science Institute, Iowa State University, 2625 N. Loop Drive, Suite 2400, Ames, IA 50010, USA.
W. Alex Mason, Boys Town National Research Institute for Child and Family Studies, 14100 Crawford Street, Boys Town, NE 68010, USA.
G. Kevin Randall, Partnerships in Prevention Science Institute, Iowa State University, 2625 N. Loop Drive, Suite 2400, Ames, IA 50010, USA.
Cleve Redmond, Partnerships in Prevention Science Institute, Iowa State University, 2625 N. Loop Drive, Suite 2400, Ames, IA 50010, USA.
Lisa Schainker, Partnerships in Prevention Science Institute, Iowa State University, 2625 N. Loop Drive, Suite 2400, Ames, IA 50010, USA.
References
- Achenbach TM, Rescorla LA. Manual for the ASEBA school-age forms & profiles. Burlington: University of Vermont, Research Center for Children, Youth, & Families; 2001. [Google Scholar]
- Allison PD. Missing data techniques for structural equation modeling. Journal of Abnormal Psychology. 2003;112:545–557. doi: 10.1037/0021-843X.112.4.545. [DOI] [PubMed] [Google Scholar]
- Angold A, Erkanli A, Silberg J, Eaves L, Costello EJ. Depression scale scores in 8–17-year-olds: effects of age and gender. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2002;43:1052–1063. doi: 10.1111/1469-7610.00232. [DOI] [PubMed] [Google Scholar]
- Aquilino WS. Family relationships and support systems in emerging adulthood. In: Arnett JJ, Tanner JL, editors. Emerging adults in America: Coming of age in the 21st century. Washington, DC: American Psychological Association; 2006. pp. 193–218. [Google Scholar]
- Atkins DC, Dimidjian S, Bedics JD, Christensen A. Couple discord and depression in couples during couple therapy and in depressed individuals during depression treatment. Journal of Consulting and Clinical Psychology. 2009;77:1089–1099. doi: 10.1037/a0017119. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social learning theory. Englewood Cliffs: Prentice Hall; 1977. [Google Scholar]
- Beach SRH, O’Mahen HA. Depression in close relationships. In: Hendrick C, Hendrick SS, editors. Close relationships: A sourcebook. Thousand Oaks: Sage; 2000. pp. 345–358. [Google Scholar]
- Biglan A, Flay BR, Embry DD, Sandler IN. The critical role of nurturing environments for promoting human well-being. American Psychologist. 2012;67:257–271. doi: 10.1037/a0026796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Botvin GJ. Life skills training. Princeton; Princeton Health Press: 2000. [Google Scholar]
- Brook DW, Brook JS, Zhang C, Cohen P, Whiteman M. Drug use and the risk of major depressive disorder, alcohol dependence, and substance use disorders. Archives of General Psychiatry. 2002;59:1039–1044. doi: 10.1001/archpsyc.59.11.1039. [DOI] [PubMed] [Google Scholar]
- Collins WA, van Dulmen M. Friendships and romance in emerging adulthood: Assessing distinctiveness in close relationships. In: Arnett JJ, Tanner JL, editors. Emerging adults in America: Coming of age in the 21st century. Washington, DC: American Psychological Association; 2006. pp. 219–234. [Google Scholar]
- Côté SM, Boivin M, Liu X, Nagin DS, Zoccolillo M, Tremblay RE. Depression and anxiety symptoms: onset, developmental course and risk factors during early childhood. Journal of Child Psychology and Psychiatry. 2009;50:1201–1208. doi: 10.1111/j.1469-7610.2009.02099.x. [DOI] [PubMed] [Google Scholar]
- Davila J. Romantic relationships and mental health in emerging adulthood. In: Fincham FD, Cui M, editors. Romantic relationships in emerging adulthood. New York: Cambridge University Press; 2011. pp. 275–492. [Google Scholar]
- Derogatis LR. SCL-90-R Administration, scoring, and procedures manual II. Townsend: Clinical Psychometric Research; 1983. [Google Scholar]
- Downey G, Coyne JC. Children of depressed parents: an integrative review. Psychological Bulletin. 1990;108:50–76. doi: 10.1037/0033-2909.108.1.50. [DOI] [PubMed] [Google Scholar]
- Eshbaugh EM. Perceptions of family relationship factors and depressive symptoms in adolescents: what roles do parents and gender play? Journal of Child and Family Studies. 2008;17:127–139. [Google Scholar]
- Fouladi RT. Performance of modified test statistics in covariance and correlations structure analysis under conditions of multivariate nonnormality. Structural Equation Modeling. 2000;7:356–410. [Google Scholar]
- Fritz MS, MacKinnon DP. Required sample size to detect the mediated effect. Psychological Science. 2007;18:233–239. doi: 10.1111/j.1467-9280.2007.01882.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greco LA, Morris TL. Factors influencing the link between social anxiety and peer acceptance: contributions of social skills and close friendships during middle childhood. Behavior Therapy. 2005;36:197–205. [Google Scholar]
- Greenberg MT. Promoting resilience in children and youth: preventive interventions and their interface with neuroscience. Annals of the New York Academy of Sciences. 2006;1094:139–150. doi: 10.1196/annals.1376.013. [DOI] [PubMed] [Google Scholar]
- Hallfors DD, Waller MW, Ford CA, Halpern CT, Brodish PH, Iritani B. Adolescent depression and suicide risk: association with sex and drug behavior. American Journal of Preventive Medicine. 2004;27:224–230. doi: 10.1016/j.amepre.2004.06.001. [DOI] [PubMed] [Google Scholar]
- Hamilton SF, Hamilton MA. School, work, and emerging adulthood. In: Arnett JJ, Tanner JL, editors. Emerging adults in America: Coming of age in the 21st century. Washington, DC: American Psychological Association; 2006. pp. 257–278. [Google Scholar]
- Helzer JE, Robins LN. The diagnostic interview schedule: its development, evolution, and use. Social Psychiatry and Psychiatric Epidemiology. 1988;23:6–16. doi: 10.1007/BF01788437. [DOI] [PubMed] [Google Scholar]
- Herbert TB, Cohen S. Measurement issues in research on psychosocial stress. In: Kaplan HB, editor. Psychosocial stress: Perspectives on structure, theory, life-course, and methods. San Diego: Academic Press Inc.; 1996. pp. 295–332. [Google Scholar]
- Hicks BM, DiRago AC, Iacono WG, McGue M. Gene-environment interplay in internalizing disorders: consistent findings across six environmental risk factors. Journal of Child Psychology and Psychiatry. 2009;50:1309–1317. doi: 10.1111/j.1469-7610.2009.02100.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz JL, Garber J. The prevention of depressive symptoms in children and adolescents: a meta-analytic review. Journal of Consulting and Clinical Psychology. 2006;74:401–415. doi: 10.1037/0022-006X.74.3.401. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Jessor R, Jessor SL. Problem behavior and psychosocial development: A longitudinal study of youth. New York: Academic; 1977. [Google Scholar]
- Joiner TE, Timmons KA. Depression in its interpersonal context. In: Gottlib IH, Hammen CL, editors. Handbook of depression. New York: Guilford; 2009. pp. 322–339. [Google Scholar]
- Judd FK, Jackson HJ, Komiti A, Murray G, Hodgins G, Fraser C. High prevalence disorders in urban and rural communities. Australian and New Zealand Journal of Psychiatry. 2002;36:104–113. doi: 10.1046/j.1440-1614.2002.00986.x. [DOI] [PubMed] [Google Scholar]
- Kumpfer KL, Molgaard V, Spoth R. The strengthening families program for the prevention of delinquency and drug use. In: Peters RD, McMahon RJ, editors. Preventing childhood disorders, substance abuse, and delinquency. Thousand Oaks: Sage; 1996. pp. 41–267. [Google Scholar]
- Lambert D, Gale JA, Hartley D. Substance abuse by youth and young adults in rural America. The Journal of Rural Health. 2008;24:221–228. doi: 10.1111/j.1748-0361.2008.00162.x. [DOI] [PubMed] [Google Scholar]
- Lawrence E, Pederson A, Bunde M, Barry RA, Brock RL, Fazio E, Dzankovic S. Objective ratings of relationship skills across multiple domains as predictors of marital satisfaction trajectories. Journal of Social and Personal Relationships. 2008;25:445–466. doi: 10.1177/0265407508090868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lillehoj CJ, Trudeau L, Spoth R, Wickrama KAS. Internalizing, social competence, and substance initiation: influence of gender moderation and a preventive intervention. Substance Use & Misuse. 2004;39:1–28. doi: 10.1081/ja-120030895. [DOI] [PubMed] [Google Scholar]
- Marcus SM, Young EZ, Kerber KB, Kornstein S, Farabaugh AH, Mitchell J, et al. Gender differences in depression: findings from the STAR*D study. Journal of Affective Disorders. 2005;87:141–150. doi: 10.1016/j.jad.2004.09.008. [DOI] [PubMed] [Google Scholar]
- Mason WA, Kosterman R, Hawkins JD, Haggerty KP, Spoth RL, Redmond C. Influence of a family-focused substance use preventive intervention on growth in adolescent depressive symptoms. Journal of Research on Adolescence. 2007;17:541–564. [Google Scholar]
- Mason WA, Kosterman R, Haggerty KP, Hawkins JD, Redmond C, Spoth RL, Shin C. Dimensions of adolescent alcohol involvement as predictors of young adult major depression. Journal of Studies on Alcohol and Drugs. 2008;69:275–285. doi: 10.15288/jsad.2008.69.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason WA, Kosterman R, Haggerty KP, Hawkins JD, Redmond C, Spoth RL, Shin C. Gender moderation and social developmental mediation of the effect of a family-focused substance use preventive intervention on young adult alcohol abuse. Addictive Behaviors. 2009;34:599–605. doi: 10.1016/j.addbeh.2009.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masten AS, Cicchetti D. Editorial: developmental cascades. Development and Psychopathology. 2010;22:491–495. doi: 10.1017/S0954579410000222. [DOI] [PubMed] [Google Scholar]
- McCartney K, Rosenthal R. Effect size, practical importance, and social policy for children. Child Development. 2003;71:173–180. doi: 10.1111/1467-8624.00131. [DOI] [PubMed] [Google Scholar]
- McClelland GH, Judd CM. Statistical difficulties of detecting interactions and moderator effects. Psychology Bulletin. 1993;114:376–390. doi: 10.1037/0033-2909.114.2.376. [DOI] [PubMed] [Google Scholar]
- Meadows SO, Brown JS, Elder GH. Depressive symptoms, stress, and support: gendered trajectories from adolescence to young adulthood. Journal of Youth and Adolescence. 2006;35:93–103. [Google Scholar]
- Merry SN, Hetrick SE, Cox GR, Brudevold-Iversen T, Bir JJ, McDowell H. Psychological and educational interventions for preventing depression in children and adolescents (review). The Cochrane library, issue 12. Hoboken: Wiley; 2011. [DOI] [PubMed] [Google Scholar]
- Molgaard VM, Spoth R, Redmond C. Competency training: The strengthening families program: For parents and youth 10–14 OJJDP Juvenile Justice Bulletin (NCJ 182208) Washington, DC: U.S. Department of Justice, Office of Juvenile Justice and Delinquency Prevention; 2000. [Google Scholar]
- Mueser KT, Drake RE, Turner W, McGovern N. Cormorbid substance use disorders and psychiatric disorders. In: Miller WR, Carroll KM, editors. Rethinking substance abuse: What the science shows, and what we should do about it. New York: Guilford; 2006. pp. 115–133. [Google Scholar]
- Muthén LK, Muthén B. Mplus user’s guide: Statistical analysis with latent variables. 6th. Los Angeles, CA: Authors; 1998–2010. [Google Scholar]
- Needham BL. Reciprocal relationships between symptoms of depression and parental support during the transition from adolescence to young adulthood. Journal of Youth and Adolescence. 2008;37:893–905. [Google Scholar]
- Nolen-Hoeksema S, Hilt LM. Gender differences in depression. In: Gotlib IH, Hammen CL, editors. Handbook of depression. 2nd. New York: Guilford; 2009. pp. 386–404. [Google Scholar]
- O’Connell ME, Boat T, Warner KE, editors. Preventing mental, emotional, and behavioral disorders among young people: Progress and possibilities Committee on the prevention of mental disorders and substance abuse among children, youth, and young adults: Research advance and promising interventions. Washington, DC: National Academies Press; 2009. [PubMed] [Google Scholar]
- O’Neil KA, Conner BT, Kendall PC. Internalizing disorders and substance use disorders in youth: comorbidity, risk, temporal order, and implications for intervention. Clinical Psychology Review. 2011;31:104–112. doi: 10.1016/j.cpr.2010.08.002. [DOI] [PubMed] [Google Scholar]
- Peen J, Schoevers RA, Beckman AT, Dekker J. The current status of urban–rural differences in psychiatric disorders. Acta Psychaitrica Scandinavica. 2010;121:84–93. doi: 10.1111/j.1600-0447.2009.01438.x. [DOI] [PubMed] [Google Scholar]
- Probst JC, Laditka S, Moore CG, Harun N, Powell MP. Depression in rural populations: Prevalence, effects on life quality, and treatment-seeking behavior. Columbia: South Carolina Rural Health Research Center; 2005. [Google Scholar]
- Rao U, Daley SE, Hammen C. Relationship between depression and substance use disorders in adolescent women during the transition to adulthood. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:215–222. doi: 10.1097/00004583-200002000-00022. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. 2nd. Newbury Park: Sage; 2002. [Google Scholar]
- Redmond C, Spoth RL, Shin C, Schainker L, Greenberg M, Feinberg M. Long-term protective factor outcomes of evidence-based interventions implemented by community teams through a community-university partnership. Journal of Primary Prevention. 2009;30:513–530. doi: 10.1007/s10935-009-0189-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudolph KD. Gender differences in emotional responses to interpersonal stress during adolescence. Journal of Adolescent Health. 2002;30S:3–13. doi: 10.1016/s1054-139x(01)00383-4. [DOI] [PubMed] [Google Scholar]
- Rudolph KD, Hammen C, Daley SE. Mood disorders. In: Wolfe DA, Mash EJ, editors. Behavioral and emotional disorders in adolescents: Nature, assessment, and treatment. New York: The Guilford Press; 2006. pp. 300–342. [Google Scholar]
- Sandler IN, Schoenfelder EN, Wolchik SA, MacKinnon DP. Long-term impact of prevention programs to promote effective parenting: lasting effects but uncertain processes. Annual Review of Psychology. 2011;62:299–329. doi: 10.1146/annurev.psych.121208.131619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychological Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- Schulenberg JE, Maggs JL. A developmental perspective on alcohol use and heavy drinking during adolescence and the transition to young adulthood. Journal of Studies on Alcohol. 2002;(Suppl. 14):54–70. doi: 10.15288/jsas.2002.s14.54. [DOI] [PubMed] [Google Scholar]
- Schulenberg JE, Zarrett NR. Mental health during emerging adulthood: Continuity and discontinuity in courses, causes, and functions. In: Arnett JJ, Tanner JL, editors. Emerging adults in America: Coming of age in the 21st century. Washington, DC: American Psychological Association; 2006. pp. 135–172. [Google Scholar]
- Shamblen SR, Derzon JH. A preliminary study of the population-adjusted effectiveness of substance abuse prevention programming: toward making IOM program types comparable. Journal of Primary Prevention. 2009;30:89–107. doi: 10.1007/s10935-009-0168-x. [DOI] [PubMed] [Google Scholar]
- Spoth R, Redmond C, Shin C. Direct and indirect latent-variable parenting outcomes of two universal family-focused preventive interventions: extending a public health-oriented research base. Journal of Consulting and Clinical Psychology. 1998;66:385–399. doi: 10.1037//0022-006x.66.2.385. [DOI] [PubMed] [Google Scholar]
- Spoth R, Guyll M, Trudeau L, Goldberg-Lillehoj C. Two studies of proximal outcomes and implementation quality of universal preventive interventions in a community-university collaboration context. Journal of Community Psychology. 2002a;30:499–518. [Google Scholar]
- Spoth R, Redmond C, Trudeau L, Shin C. Longitudinal substance initiation outcomes for a universal preventive intervention combining family and school programs. Psychology of Addictive Behavior. 2002b;16:129–134. [PubMed] [Google Scholar]
- Spoth R, Randall GK, Shin C, Redmond C. Randomized study of combined universal family and school preventive interventions: patterns of long-term effects on initiation, regular use, and weekly drunkenness. Psychology of Addictive Behaviors. 2005;19:372–381. doi: 10.1037/0893-164X.19.4.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth R, Clair S, Greenberg M, Redmond C, Shin C. Toward dissemination of evidence-based family interventions: maintenance of community-based partnership recruitment results and associated factors. Journal of Family Psychology. 2007;21:137–146. doi: 10.1037/0893-3200.21.2.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth R, Randall GK, Trudeau L, Shin C, Redmond C. Substance use outcomes 5½years past baseline for partnership-based, family-school preventive interventions. Drug and Alcohol Dependence. 2008a;96:57–68. doi: 10.1016/j.drugalcdep.2008.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth R, Trudeau L, Shin C, Redmond C. Long-term effects of universal preventive interventions on prescription drug misuse. Addiction. 2008b;103:1160–1168. doi: 10.1111/j.1360-0443.2008.02160.x. [DOI] [PubMed] [Google Scholar]
- Spoth R, Trudeau L, Guyll M, Shin C, Redmond C. Universal intervention effects on substance use among young adults mediated by delayed adolescent substance initiation. Journal of Consulting and Clinical Psychology. 2009;77:620–632. doi: 10.1037/a0016029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth R, Trudeau L, Redmond C, Shin C. Replication RCT of early universal prevention effects on young adult substance misuse. Journal of Consulting and Clinical Psychology. 2014;82:949–963. doi: 10.1037/a0036840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steering Committee of the Physicians’ Health Study Research Group. Final report on the aspirin component of the ongoing Physicians’ Health Study. New England Journal of Medicine. 1989;321:129–135. doi: 10.1056/NEJM198907203210301. [DOI] [PubMed] [Google Scholar]
- Stice E, Shaw H, Bohon C, Marti CN, Rohde P. A meta-analytic review of depression prevention programs for children and adolescents: factors that predict magnitude of intervention effects. Journal of Consulting and Clinical Psychology. 2009;77:486–503. doi: 10.1037/a0015168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Rohde P, Seeley JR, Gau JM. Testing mediators of intervention effects in randomized controlled trials: an evaluation of three depression prevention programs. Journal of Consulting and Clinical Psychology. 2010;78:273–280. doi: 10.1037/a0018396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Streiner DL. Being inconsistent about consistency: when coefficient alpha does and doesn’t matter. Journal of Personality Assessment. 2003;80:217–222. doi: 10.1207/S15327752JPA8003_01. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2009 National Survey on Drug Use and Health: Mental Health Findings. Rockville, MD: 2010a. (Office of Applied Studies, NSDUH Series H-39, HHS Publication No SMA 10-4609). [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2009 National Survey on Drug Use and Health: Volume I Summary of National Findings. Rockville, MD: 2010b. (Office of Applied Studies, NSDUH Series H-38A, HHS Publication No. SMA 10-4586 Findings). [Google Scholar]
- Trudeau L, Spoth R, Lillehoj C, Redmond C, Wickrama KAS. Effects of a preventive intervention on adolescent substance use initiation, expectancies, and refusal intentions. Prevention Science. 2003;4:109–122. doi: 10.1023/a:1022926332514. [DOI] [PubMed] [Google Scholar]
- Trudeau L, Spoth R, Randall GK, Azevedo K. Longitudinal effects of a universal family-focused intervention on growth patterns of adolescent internalizing symptoms and polysubstance use: gender comparisons. Journal of Youth and Adolescence. 2007;36(6):740–745. [Google Scholar]
- Trudeau L, Spoth R, Randall GK, Mason WA, Shin C. Internalizing symptoms: effects of a preventive intervention on developmental pathways from early adolescence to young adulthood. Journal of Youth and Adolescence. 2012;41:788–801. doi: 10.1007/s10964-011-9735-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wade AG, Häring J. A review of the costs associated with depression and treatment noncompliance: the potential benefits of online support. International Clinical Psychopharmacology. 2010;25:288–296. doi: 10.1097/yic.0b013e328339fbcf. [DOI] [PubMed] [Google Scholar]
- Whisman MA. The association between depression and marital dissatisfaction. In: Beach SRH, editor. Marital and family processes in depression: A scientific foundation for clinical practice. Washington, DC: American Psychological Association; 2001. pp. 3–24. [Google Scholar]


