Abstract
Pulmonary ground-glass opacity (GGO) nodules, which do not grow remarkably, are often observed without treatment. Lung tumors coexisting with inflammation and infection are difficult to diagnose. In this paper, we describe a very rare case of a pulmonary mixed GGO nodule with pleural dissemination. In 67-year-old female, chest computed tomography (CT) showed a mixed GGO nodule that had not grown remarkably in the right lung. For 6 years, the mixed GGO had been treated as nontuberculous mycobacterial infection. She was referred to our department for further investigation of the mixed GGO. We suspected lung cancer and performed lung segmentectomy. The tissue showed pleural dissemination. Coexisting nontuberculous mycobacteria (NTM) delayed the clinical diagnosis. Peripheral lung nodules should be resected or diagnosed as soon as possible, despite manifesting as a slow growth.
Keywords: Consolidation/maximum tumor diameter ratio, dissemination, ground-glass opacity (GGO), nontuberculous mycobacteria (NTM)
Introduction
Ground-glass opacity (GGO) detected by computed tomography (CT) includes malignancy, benign changes, and inflammatory changes. A GGO lesion is a less aggressive and slow-growing tumor; therefore, immediate resection at the time of detection may be unnecessary (1). If patients have inflammation or infection with lung cancer, it is difficult to diagnose the cancer accurately at an early stage. However, a mixed GGO nodule, despite being an extremely slow-growing tumor, can have pleural dissemination. In this paper, we report a case of a mixed GGO that was treated as a nontuberculous mycobacterial infection and was not recognized as progressive lung cancer, which appeared as pleural dissemination.
Case report
A 67-year-old woman visited the hospital with a complaint of cough and dyspnea. The CT scan of her chest showed several peripheral lung nodules in the right lower lobe (S6) and other lobes. The symptoms improved without any medication. For 2 years, the patient was followed up by CT scans. At the 3rd year, the lung nodule had spread to right middle lobe and left upper lobe. Based on transbronchial biopsy, she was diagnosed as having nontuberculous mycobacteria (NTM) of the lung. Antituberculous drugs were administered for 2 years, and nearly all peripheral lung nodules disappeared. However, the right lower lobe (S6) continued to have a mixed GGO nodule, which was detected because it was considered NTM or inflammatory change.
At the 5th year, an enhanced CT scan showed that the nodule was not growing but its solid component had shrunk slightly, and the consolidation/maximum tumor diameter (C/T) ratio was 0.35. At the 6th year, the nodule had not grown remarkably; however, solid component and the C/T ratio had increased (from 0.35 to 0.42). Figure 1 shows the clinical course of the nodule. The tumor doubling time (TDT), described by Schwartz, was estimated at 4,553 days. We suspected the nodule was a malignant tumor.
Figure 1.
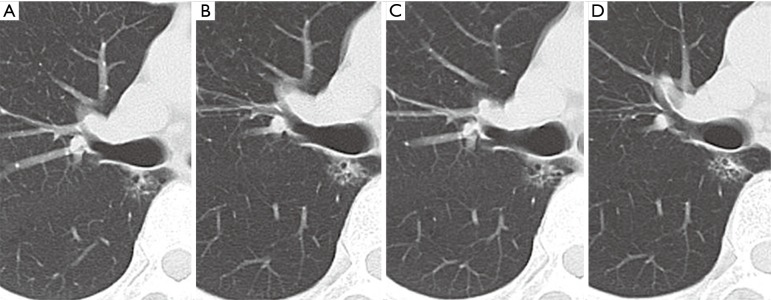
Mixed ground-glass opacity (GGO) in the right S6, detected by computed tomography (CT). (A) 6 years ago: the tumor size is 17 mm and C/T ratio is 0.35; (B) 2 years ago: the tumor size is 18 mm and the C/T ratio is 0.40; (C) 1 year ago: the tumor size is 18 mm and the C/T ratio is 0.35; (D) before the operation: the tumor size is 19 mm and the C/T ratio is 0.42. C/T, consolidation/maximum tumor diameter.
Video-assisted right lower S6 segmentectomy was performed as a limited operation because her pulmonary function would not have allowed her to tolerate a lobectomy. When we inserted the thoracoscope in the thoracic cavity, many small nodules were spread in the visceral pleura of the upper lobe and middle lobe; however, we determined during the operation that the nodules showed inflammatory or infectious changes rather than pleural dissemination. The pathological finding was adenocarcinoma and the small nodules were pleural dissemination (Figure 2). We ultimately diagnosed primary lung adenocarcinoma at pathological T1aN0M1a stage IV. Two months later, CDDP plus pemetrexed chemotherapy was initiated. Recurrence or a new lesion was not detected for 20 months.
Figure 2.
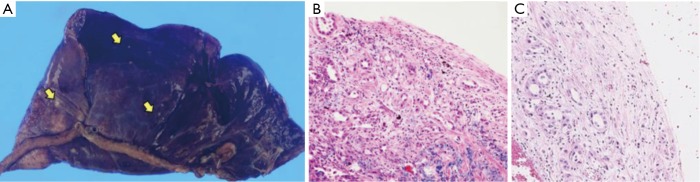
Pathology. (A) The surgical specimen: the small nodules (yellow arrows) are pleural dissemination in the right S6; (B) the primary tumor: the solid component shows a moderate differentiated adenocarcinoma, acinar type (hematoxylin and eosin stain; magnification, ×100); (C) pleural dissemination: small lung nodules in the visceral pleura show moderate differentiated adenocarcinoma, which is similar to the finding in the solid component (hematoxylin and eosin stain; magnification, ×100).
Discussion
We discovered an important clinical issue. A mixed GGO nodule has a malignant potential for pleural dissemination, even if the tumor is small and not growing remarkably. Infection by NTM delayed an accurate diagnosis of the small nodule, and resulted in a progressive state. We propose that small peripheral nodules such as mixed GGO nodules require early surgical resection for diagnosis and treatment.
This is the first patient in whom pleural dissemination was caused by mixed GGO nodule that did not grow remarkably and had a C/T ratio of less than 0.5. Mixed GGO nodules can certainly cause pleural invasion and lymph node metastasis if the C/T ratio is more than 0.25Jeny (2).
Even though pleural invasion in our patient was predictable, pleural dissemination was surprising because both the tumor size and the C/T ratio did not increase remarkably for 6 years and the TDT, which is related to malignancy (3), was quite long at 4,335 days. Therefore, it was very difficult to predict pleural dissemination.
Observing the mixed GGO nodule, which was treated as NTM, for a very long time affected the clinical course of pleural dissemination. Furthermore, observation for a long period is unusual. Two papers reported mixed GGO nodules of 3 cm or smaller and a C/T ratio of less than 0.5 that were observed for longer than 2 years and showed no pleural dissemination (4,5). The investigators further reported that all resected tumors were in an early stage pathologically and the patients had a good prognosis.
In our patient, the reason mixed GGO showed pleural dissemination was that the solid component, which was pathologically a moderate differentiated adenocarcinoma, was faced on visceral pleura for a long time (Figure 2B). We believe that the location of the mixed GGO nodule resulted in pleural dissemination because the pathological feature of the primary tumor was coincidental with the pleural dissemination (Figures 2C).
Lung cancer coexisting with NTM is unusual. The rate of patients who harbor concomitant lung cancer and NTM is 1.8-8.6% (6,7). A characteristic of lung cancer coexisting with NTM is that it arises from the peripheral lung (7). However, the incidence of pleural dissemination is not increased, based on previous reports. We propose that a mixed GGO nodule that is being treated as NTM and remains for a long time should be diagnosed as early as possible by CT-guided biopsy, transbronchial lung biopsy, or surgical resection.
In conclusion, a mixed GGO nodule showed pleural dissemination, despite being small and stable with a C/T ratio less than 0.5; the tumor size did not increase for 6 years. Physicians should be aware that a peripheral lung nodule that is a low grade malignancy can cause pleural dissemination, and physicians should consider the possibility of a coexisting malignant tumor when treating patients for NTM. Physicians should make the effort to diagnose accurately and perform a biopsy or resect peripheral lung nodule as soon as possible, even though the nodule is not growing.
Acknowledgements
None.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Kobayashi Y, Mitsudomi T. Management of ground-glass opacities: should all pulmonary lesions with ground-glass opacity be surgically resected? Transl Lung Cancer Res 2013;2:354-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Suzuki K, Kusumoto M, Watanabe S, et al. Radiologic classification of small adenocarcinoma of the lung: radiologic-pathologic correlation and its prognostic impact. Ann Thorac Surg 2006;81:413-9. [DOI] [PubMed] [Google Scholar]
- 3.Lillington GA. Management of solitary pulmonary nodules. How to decide when resection is required. Postgrad Med 1997;101:145-50. [DOI] [PubMed] [Google Scholar]
- 4.Kobayashi Y, Fukui T, Ito S, et al. How long should small lung lesions of ground-glass opacity be followed? J Thorac Oncol 2013;8:309-14. [DOI] [PubMed] [Google Scholar]
- 5.Matsuguma H, Mori K, Nakahara R, et al. Characteristics of subsolid pulmonary nodules showing growth during follow-up with CT scanning. Chest 2013;143:436-443. [DOI] [PubMed] [Google Scholar]
- 6.Tamura A, Hebisawa A, Masuda K, et al. Coexisting lung cancer and active pulmonary mycobacteriosis. Nihon Kokyuki Gakkai Zasshi 2007;45:382-93. [PubMed] [Google Scholar]
- 7.Lande L, Peterson DD, Gogoi R, et al. Association between pulmonary mycobacterium avium complex infection and lung cancer. J Thorac Oncol 2012;7:1345-51. [DOI] [PubMed] [Google Scholar]


