Abstract
Background:
The main goals in treating burns are to accelerate tissue renovation and prevent infection. Topical antibiotics are used in the treatment of burns, but they can cause side effects. Recently, a traditional ointment (Olea) has been used in Iran in the treatment of burns. This study examines the effect of topical honey ointment in healing of burn patients.
Materials and Methods:
In this randomized controlled trial (RCT), 30 hospitalized patients selected by conventional sampling (10 in Olea group and 20 in Acetate Mafenide ointment group) were evaluated. Inclusion criteria were: having second-degree burns and body surface area equal to or < 40%. One group was treated using topical Olea ointment and the other with Acetate Mafenide ointment (8.5%). Chi-square, Fisher exact test, and Kaplan–Meier were used. Significance level was considered as P < 0.05.
Results:
None of the patients in the Olea group needed surgery for debridement, while in the second group, 13 patients (65%) needed debridement (P = 0.001). In the Olea group, 1 patient (10%) and in the second group, 19 patients (95%) had positive cultures after 7 days (P < 0.001). The mean time of granulation tissue formation in the Olea group was 12 days (10.3–13.6) and in the other group, it was 17 days (13.3–20.6) (P < 0.001).
Conclusions:
Olea ointment is a useful treatment for burns, and it can prevent infections, accelerate tissue repair, and facilitate debridement. Therefore, using this ointment is recommended for the treatment of burns.
Keywords: Burns, re-epithelialization, wounds and injuries, wound healing
INTRODUCTION
The main goals of managing burns are to accelerate tissue repair and to prevent infection.[1] Infection is the most serious and fatal side effect of acute burns, which is produced by various microorganisms; however, correct and on-time treatment is effective in curing the patient.[2] Topical antibiotic creams such as acetate mafenide and silver sulfadiazine are among the most common medicines used for the treatment of burns. This ointment has a combination of silver nitrate and sodium sulfadiazine. Silver destroys the cell wall of bacteria and allows sulfadiazine to act as an antibacterial agent,[3] but wound healing can be affected by using this compound.[4] Acetate mafenide is a bacteriostatic drug which has bactericidal effect in high doses; it is effective against approximately all pathogens colonized in burn wounds.[5,6,7] However, these drugs may also have cytotoxic properties;[8] therefore, finding drugs with fewer side effects can be very helpful in treating this kind of patients.
Recently, some studies have investigated the use of honey to prevent infection and treat burns; they used honey as a remedy for the prevention of infection in bedsores and burns.[5,9,10,11,12] It has been reported that honey can facilitate removing necrotic tissues, increase the granulation and epithelialization speed, and reduce scars.[12,13,14] The antimicrobial power of honey prevents the growth of bacteria on the moist environment of skin surface. The factors that make honey a useful remedy for burns are: Acidic environment (pH= 3.4–6.1), high osmotic properties, avoids dressing from sticking to the wound, and decreases the dislodgement of granulation tissues at the time of dressing.[10] Since honey dressing reduces scar formation, it minimizes the need to graft.[13] A number of enzymes such as invertase, amylase, and glucose oxidase and hydroxide peroxide are found in honey. In addition, the antibacterial and antifungal effects of honey have also been reported. The antibacterial quality of honey is attributed to the presence of oligosaccharides, glycopeptides, and peptides.[15]
Sesame oil is also one among the agents that are currently used to treat burns; it has shown different effects on wound healing.[16] Sesame oil was reported to be effective in reduction of cholesterol and blood glucose[17] and it has antioxidant effect.[18] Olive oil was studied for its antioxidant effect and was found to have beneficial effects in cardiovascular diseases and cancers.[19] In traditional medicine, olive oil has been considered to be effective in skin healing; however, this issue has not been studied in advanced medicine. Unfortunately, very few studies has been done on sesame oil, olive oil, and their effects in healing wounds, while some studies have shown their beneficial effects.[12,16,20,21,22] However, the effect of honey has been studied in animal and human subjects.[22,23] Combining honey with olive oil and sesame oil may increase their beneficial effects in healing wounds. Also, this combination may reduce bacterial wound colonization; however, no study has been conducted to examine this idea.
Nowadays, an ointment named Olea, which is a combination of honey, olive oil, and sesame, is being used in Iran for treatment of burns. This study aimed to examine the effect of this ointment on tissue repair and development of granulation tissues in patients with burns wounds.
MATERIALS AND METHODS
This is a randomized controlled trial. This study was approved by the ethical committee of Kurdistan University of Medical Sciences (Project No.: 84/42) and was registered in Iran Registry of Clinical Trial (RCT registration code: IRCT2014020516490N1). The inclusion criteria for patients enrolled in the study were: Having second-degree burns (burn depth of 0.2–5.0 mm); burns covering 40% or less of their body surface area; aged between 15 and 55 years; gave consent to participate in the study; referred durng the first 24 h of injury; and had negative ulcer culture on admission. Patients with underlying conditions such as diabetes, chronic renal or hepatic diseases, and those with simultaneous burns, trauma, and skin lacerations were excluded.
The sample included 30 available patients in Tohid hospital (in Sanandaj) who were divided into two groups using simple randomized method and table of random numbers; the chance of entering the control group was twice as that of the case group. The first group consisted of 10 patients who were treated using Olea ointment (manufactured in Farateb, Yazd, Iran). Olea ointment contains 33.4% honey, 33.3% olive oil, and 33.3% sesame oil. After washing the wound with normal saline solution, 3–5 mm thick layer of Olea ointment was applied over the wound and closed dressing was performed every day until the patients were discharged, by one of the researchers. The second group consisted of 20 patients; they were treated using about 1.5-mm-thick layer of Acetate Mafenide ointment (8.5%; manufactured by Sina Daro Pharmaceutical Company, Tehran, Iran) every 12 h, which is a broad-spectrum bacteriostatic ointment against gram-negative bacteria and is easily accessible. Patients and researchers were aware about the treatment groups, but the microbiologist and pathologist were blinded to the treatment groups.
To assess the outcomes, the burn wounds were evaluated daily after a week of intervention by a pathologist and a microbiologist for the formation of granulation tissues, debridement (using scalpel), and wound culture results. If they had positive culture, they were excluded from the study and treated by routine treatment for bacterial strains. However, the excluded patients were entered in the analysis.
Using Fisher exact test, the collected data were analyzed with SPSS 16 software to compare the qualitative variables between the two groups. The Kaplan–Meier survival curve was also used to compare granulation tissue formation time. The average time of granulation tissue formation was compared between the two groups using log-rank test.
RESULTS
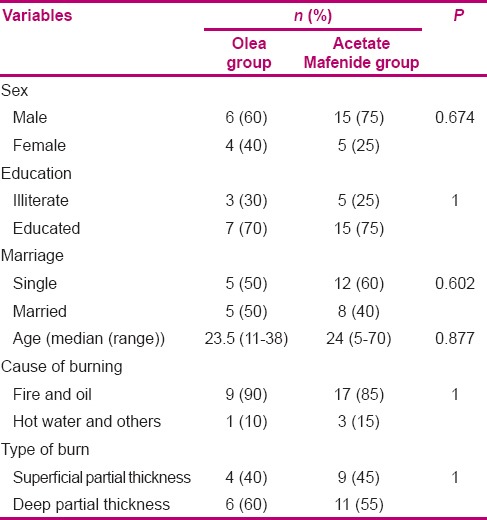
The mean age of participants was 24.8 (±11.9) years. Of the total number of participants, 21 (70%) were male, 17 (56.7%) were single, and 8 patients (26.7%) were illiterate. Concerning the cause of burn, the most common cause was direct fire or oil burns, which was observed in 26 patients (85%). Six patients (60%) in Olea group and 11 patients (55%) in Acetate Mafenide group had deep partial thickness (second-degree) burns. No statistically significant difference was observed between the two study groups regarding these variables [Table 1].
Table 1.
Comparison of the basic characteristics of the participants in Olea and Acetate Mafenide groups
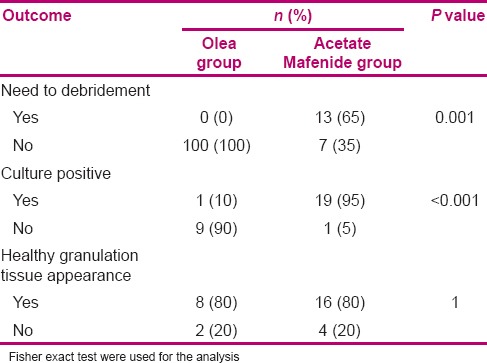
Results of the study showed that none of the patients in the Olea group needed to use a scalpel for debridement and debridement was performed by simple showers; however, 13 patients (65%) in the Acetate Mafenide group needed debridement, and the difference was statistically significant (P = 0.001). One patient (10%) in the Olea group and 19 patients (95%) in the Acetate Mafenide group had positive cultures 7 days after intervention; the difference was statistically significant (P < 0.001). The most common strains found in cultures were Pseudomonas, Staphylococcus aerogenes, Enterobacter, and Escherichia coli.
As shown in Figure 1, the median time of formation of granulation tissue in the Olea and Acetate Mafenide groups was 12 days (range: 10.3–13.6) and 17 days (range: 13.3–20.6), respectively (P < 0.001). Eight patients (80%) from Olea group and 16 patients (80%) from Acetate Mafenide had formed granulation tissue by the end of the study, and no statistically significant differences was observed between the two groups (P = 1) [Table 2].
Figure 1.
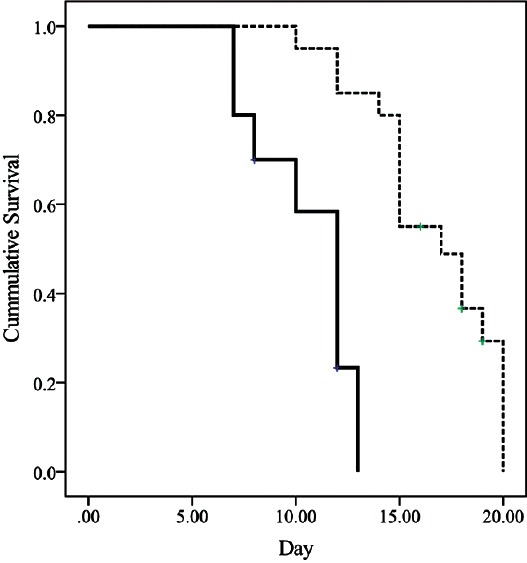
Comparing the duration of granulation tissue formation in both groups during the study period. Uninterrupted lines shows Olea group and broken lines indicate Acetate Mafenide group. The mean time of granulation tissue formation in the Olea and Acetate Mafenide groups was 12 days (10.3–13.6) and 17 days (13.3–20.6), respectively (P < 0.001)
Table 2.
Comparison of frequency (percent) of main outcomes between Olea and Acetate Mafenide groups
DISCUSSION
Results of this study showed that Olea ointment was effective in facilitating debridement and preventing wound infection; besides, treatment with topical Olea ointment accelerated tissue repair.
In our study, treatment with Olea led to easy debridement. A study found that when honey is used in the process of dressing, necrotic tissue is easily detached from the wound, the wet environment generated by honey prevents the dressing from sticking to the wound, and consequently, the patient experiences less tissue damage, pain, and bleeding during dressing changes.[24] When dressing does not stick to the wound, the newly formed tissue will not detach, and therefore, healing is accelerated and there is less pain. Furthermore, using substances such as olive oil, which contains Hypafix, can prevent damages caused by dressing and can facilitate washing wounds.[20]
Several clinical researches have shown that using honey ointment for dressing burn is more effective than topical antibiotic ointments used in healing wounds and can reduce inflammation and swelling.[24,25] Also, honey ointment is effective in the formation of granulation tissue and in epithelialization.[2,26] In our study, treatment with Olea led to prevention of infection. The antibacterial quality of honey is attributed to its moist and dense environment that prevents bacterial growth; besides, honey contains some enzymes which can prevent the growth of bacteria and fungi.[15] Based on the results of a study, during the first week of treatment, 85% of patients treated with Olea had sterile wounds while only 30% of patients treated with other methods had sterile wounds.[27] Such results were also observed in Baghel et al.'s study;[26] they showed that honey was more effective than silver sulfadiazine ointment. Honey prevents contamination and infection through covering the surface of the wound. Also, due to its high acidity attributed to the high levels of enzymes, honey can also directly affect bacteria.[15,28] However, unlike other antibacterial drugs, it does not cause tissue damage and does not have any side effects.
According to a study, the average duration of tissue repair was 10.4 days in the honey group and was 16.2 days in the group treated with potatoes; in another study, the average duration of tissue repair in two groups treated with honey and silver sulfadiazine was 15.4 and 17.2 days, respectively.[27] Based on the results of another research, the duration of tissue repair in the group treated with honey was half of that in the group treated with silver sulfadiazine (18.1 vs 32.7 days).[26] Kogan et al. showed in their study that sesame oil alone has no beneficial effects on healing burn wounds in animal samples.[29] In another study, sesame oil accelerated wound epithelialization up to a week. Using this oil has also led to better contraction of the wound.[16] Honey also has anti-inflammatory effects; therefore, it can accelerate the tissue repair process as inflammation can prevent tissue repair.[30]
Another research found sesame oil to be effective in tissue repair.[21] Sesame seeds contain antioxidants and other substances that can prevent cellular damage and facilitate tissue repair. These effects can be induced by both topical application and systemic consumption.[16] A systematic review also indicated that honey can accelerate the process and duration of tissue repair.[10] In another study, 80% of patients treated with honey had tissue repair after 7 days, while it was only 52% in Mafenide Acetate groups.[31] It seems that dressing with honey has advantages such as early wound epithelialization, reduced time taken for the wounds to test culture negative, and earlier pain relief.[32]
In our study, epithelialization of wounds was more quickly initiated in the group treated with Olea. It seems that using honey ointment can reduce the costs of debridement surgeries and can even reduce the need to do graft, because the increased speed of granulation and epithelialization can increase the speed of healing and, consequently, will lead to minimal scarring.[13]
Sesame and olive contain substances that can inhibit lipid peroxidation process, improve the supply of blood to collagen tissues, increase the fibril collagen longevity, and reduce cell damages.[33,34] Olea ointment is a combination of honey, sesame oil, and olive oil. So, it possesses the useful effects of each of these factors. All these materials have special compounds that can be helpful to improve scar formation by burns; however, in Gurfinkel et al.'s study, olive oil was not able to improve healing of wound.
One of our study limitations was its small sample size. However, Olea ointment was effective in this sample size. Also, we could not evaluate all forms of burn wounds and did not evaluate the scar of wound after healing. We suggest other studies to be conducted with larger sample size to evaluate the other effects of Olea ointment. Future studies should address the effectiveness of the Olea on all forms of burn wounds.
CONCLUSION
Topical Olea ointment is useful for treating burns, and it can prevent infections, accelerate tissue repair, and facilitate debridement. Therefore, using this ointment is recommended for the treatment of grade II burns.
ACKNOWLEDGMENTS
This article is extracted from the project supported by Kurdistan University of Medical Sciences. The authors would like to thank to participants. Project number 8712, Kurdistan University of Medical Sciences, Sanandaj, Iran.
Footnotes
Source of Support: Kurdistan University of Medical Sciences
Conflict of Interest: None declared.
REFERENCES
- 1.Salas Campos L, Fernandes Mansilla M, Martinez de la Chica AM. Topical chemotherapy for the treatment of burns. Rev Enferm. 2005;28:67–70. [PubMed] [Google Scholar]
- 2.Wijesinghe M, Weatherall M, Perrin K, Beasley R. Honey in the treatment of burns: A systematic review and meta-analysis of its efficacy. N Z Med J. 2009;122:47–60. [PubMed] [Google Scholar]
- 3.Atiyeh BS, Costagliola M, Hayek SN, Dibo SA. Effect of silver on burn wound infection control and healing: Review of the literature. Burns. 2007;33:139–48. doi: 10.1016/j.burns.2006.06.010. [DOI] [PubMed] [Google Scholar]
- 4.Poon VK, Burd A. In vitro cytotoxity of silver: Implication for clinical wound care. Burns. 2004;30:140–7. doi: 10.1016/j.burns.2003.09.030. [DOI] [PubMed] [Google Scholar]
- 5.Song JJ, Salcido R. Use of Honey in Wound Care: An Update. Advances in Skin and Wound Care. 2011;24:40–4. doi: 10.1097/01.ASW.0000392731.34723.06. [DOI] [PubMed] [Google Scholar]
- 6.Church D, Elsayed S, Reid O, Winston B, Lindsay R. Burn wound infections. Clin Microbiol Rev. 2006;19:403–34. doi: 10.1128/CMR.19.2.403-434.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Molan PC, Betts JA. Clinical usage of honey as a wound dressing: An update. J Wound Care. 2004;13:353–6. doi: 10.12968/jowc.2004.13.9.26708. [DOI] [PubMed] [Google Scholar]
- 8.Fraser JF, Cuttle L, Kempf M, Kimble RM. Cytotoxicity of topical antimicrobial agents used in burn wounds in Australasia. ANZ J Surg. 2004;74:139–42. doi: 10.1046/j.1445-2197.2004.02916.x. [DOI] [PubMed] [Google Scholar]
- 9.Hamouda HM, Marzouk DS. Antibacterial Activity of Egyptian Honey from Different Sources. Int J Microbiol Res. 2011;2:149–55. [Google Scholar]
- 10.Vandamme L, Heyneman A, Hoeksema H, Verbelen J, Monstrey S. Honey in modern wound care: A systematic review. Burns. 2013;39:1514–25. doi: 10.1016/j.burns.2013.06.014. [DOI] [PubMed] [Google Scholar]
- 11.Manyi-Loh CE, Clarke AM, Ndip RN. An overview of honey: Therapeutic properties and contribution in nutrition and human hea. Afr J Microbiol Res. 2011;5:844–52. [Google Scholar]
- 12.Al-Waili N, Salom K, Al-Ghamdi AA. Honey for Wound Healing, Ulcers, and Burns; Data Supporting Its Use in Clinical Practice. Scientific World J. 2011;11:766–87. doi: 10.1100/tsw.2011.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vermeulen H, Ubbink DT, Goossens A, de Vos R, Legemate DA. Systematic review of dressings and topical agents for surgical wounds healing by secondary intention. Br J Surg. 2005;92:665–72. doi: 10.1002/bjs.5055. [DOI] [PubMed] [Google Scholar]
- 14.Oladejo OW, Imosemi IO, Osuagwu FC, Oyedele OO, Oluwadara OO, Ekpo OE, et al. A comparative study of the wound healing properties of honey and Ageratum conyzoides. Afr J Med Med Sci. 2003;32:193–6. [PubMed] [Google Scholar]
- 15.Aurongzeb M, Azim K. Antimicrobial properties of natural honey: A review of literature. Pak J Biochem Mol Biol. 2011;44:118–24. [Google Scholar]
- 16.Kiran K, Asad M. Wound healing activity of Sesamum indicum L seed and oil in rats. Indian J Exp Biol. 2008;46:777–82. [PubMed] [Google Scholar]
- 17.Sankar D, Ali A, Sambandam G, Rao R. Sesame oil exhibits synergistic effect with anti-diabetic medication in patients with type 2 diabetes mellitus. Clin Nutr. 2011;30:351–8. doi: 10.1016/j.clnu.2010.11.005. [DOI] [PubMed] [Google Scholar]
- 18.Jeyarani N, Rakshitha D. Isolation and antioxidant efficacy of nutraceutical concentrates from sesame and flax seed oils. J Food Sci Technol (Mysore) 2009;46:66–9. [Google Scholar]
- 19.Waterman E, Lockwood B. Active components and clinical applications of olive oil. Altern Med Rev. 2007;12:331–42. [PubMed] [Google Scholar]
- 20.Papini R. Management of burn injuries of various depths. BMJ. 2004;329:158–60. doi: 10.1136/bmj.329.7458.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Valacchi G, Lim Y, Belmonte G, Miracco C, Zanardi I, Bocci V, et al. Ozonated sesame oil enhances cutaneous wound healing in SKH1 mice. Wound Repair Regen. 2011;19:107–15. doi: 10.1111/j.1524-475X.2010.00649.x. [DOI] [PubMed] [Google Scholar]
- 22.Lotfi A. Use of honey as a medical product in wound dressing (Human and Animal studies): A review. Res J Biol Sci. 2008;3:136–40. [Google Scholar]
- 23.Al-Waili N, Salom K, Al-Ghamdi AA. Honey for wound healing, ulcers, and burns; data supporting its use in clinical practice. Scientific World J. 2011;11:766–87. doi: 10.1100/tsw.2011.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gupta SS, Singh O, Bhagel PS, Moses S, Shukla S, Mathur RK. Honey dressing versus silver sulfadiazene dressing for wound healing in burn patients: A retrospective study. J Cutan Aesthet Surg. 2011;4:183–7. doi: 10.4103/0974-2077.91249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mohd Zohdi R, Abu Bakar Zakaria Z, Yusof N, Mohamed Mustapha N, Abdullah MN. Gelam (Melaleuca spp.) Honey-Based Hydrogel as Burn Wound Dressing. Evid Based Complement Alternat Med. 2012;2012:843025. doi: 10.1155/2012/843025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Baghel PS, Shukla S, Mathur RK, Randa R. A comparative study to evaluate the effect of honey dressing and silver sulfadiazene dressing on wound healing in burn patients. Indian J Plast Surg. 2009;42:176–81. doi: 10.4103/0970-0358.59276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Moore OA, Smith LA, Campbell F, Seers K, McQuay HJ, Moore RA. Systematic review of the use of honey as a wound dressing. BMC Complement Altern Med. 2001;1:2. doi: 10.1186/1472-6882-1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dudhamal TS, Gupta SK, Bhuyan C. Role of honey (Madhu) in the management of wounds (Dushta Vrana) Int J Ayurveda Res. 2010;1:271–3. doi: 10.4103/0974-7788.76793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kogan L, Lebenthal A, Breiterman S, Eldad A. A Chinese Sesame-oil-based ointment for burns compared with bacitracin ointment-An animal trial. Ann Burns Fire Disasters. 2001;14:85–9. [Google Scholar]
- 30.Molan P. Mode of action. In: White R, Cooper R, Honey MP, editors. A Modern Wound Management Product. Aberdeen: Wounds UK Publications; 2005. [Google Scholar]
- 31.Maghsoudi H, Salehi F, Khosrowshahi MK, Baghaei M, Nasirzadeh M, Shams R. Comparison between topical honey and mafenide acetate in treatment of burn wounds. Ann Burns Fire Disasters. 2011;24:132–7. [PMC free article] [PubMed] [Google Scholar]
- 32.Sami AN, Mehmood N, Qureshi MA. Honey Compared with Silver sulphadiazine as Burn Wound Dressing. Ann Pak Inst Med Sci. 2011;7:22–5. [Google Scholar]
- 33.Edraki M, Akbarzadeh A, Hosseinzadeh M, Tanideh N, Salehi A, Koohi-Hosseinabadi O. Healing effect of sea buckthorn, olive oil, and their mixture on full-thickness burn wounds. Adv Skin Wound Care. 2014;27:317–23. doi: 10.1097/01.ASW.0000451061.85540.f9. [DOI] [PubMed] [Google Scholar]
- 34.Senel O, Cetinkale O, Ozbay G, Ahcioglu F, Bulan R. Oxygen free radicals impair wound healing in ischemic rat skin. Ann Plast Surg. 1997;39:516–23. doi: 10.1097/00000637-199711000-00012. [DOI] [PubMed] [Google Scholar]


