Abstract
Background:
Chronic obstructive pulmonary disease (COPD) is currently the fourth cause of mortality worldwide. Patients with COPD experience periods of dyspnea, fatigue, and disability, which impact on their life. The objective of this study was to investigate the effect of short-term inspiratory muscle training on exercise capacity, exertional dyspnea, and pulmonary lung function.
Materials and Methods:
A randomized, controlled trial was performed. Thirty patients (27 males, 3 females) with mild to very severe COPD were randomly assigned to a training group (group T) or to a control group (group C). Patients in group T received training for 8 weeks (15 min/day for 6 days/week) with flow-volumetric inspiratory exerciser named (Respivol). Each patient was assessed before and after 8 weeks of training for the following clinical parameters: exercise capacity by 6-min walking test (6MWT), exertional dyspnea by Borg scale, and pulmonary lung function by spirometry. Patients used training together with medical treatment. The data were analyzed using paired t-test and independent t-test.
Results:
Results showed statistically significant increase in 6MWT at the end of the training from 445.6 ± 22.99 to 491.06 ± 17.67 meters? (P < 0.001) and statistically significant decrease in dyspnea from 3.76 ± 0.64 to 1.13 ± 0.36 (P = 0.0001) in the training group but not in the control group. The values for exercise capacity and dyspnea improved after 8 weeks in group T in comparison with group C (P = 0.001 and P = 0.0001, respectively). No changes were observed in any measure of pulmonary function in both groups.
Conclusions:
Short-term inspiratory muscle training has beneficial effects on exercise capacity and exertional dyspnea in COPD patients.
Keywords: 6-min walking test, chronic obstructive pulmonary disease, exercise capacity, exertional dyspnea, inspiratory muscle training, pulmonary function
INTRODUCTION
Chronic obstructive pulmonary disease (COPD) is a disease characterized by airflow limitation and small airways, which is an irreversible process.[1] According to a report by the World Health Organization (WHO), there are 80 million people with COPD worldwide[2] and more than 6.3% of the population over 30 years in the Asia-Pacific countries suffer from this condition, which ranges from moderate to severe.[3] In 2001, the number of COPD patients per 100,000 people, who were mostly men living in cities, was estimated to be 105 patients aged 15-49 years and 1057 patients aged 50 years and over in 18 provinces of Iran, respectively.[4] Many economic and social costs are imposed on the society by this disease, and we also saw a trend toward increased financial burden in the past decade.[5]
According to the Australasian Rehabilitation Nurses’ Association (ARNA), rehabilitation nursing aims to maximize self determination, restore the function, and optimize patients’ lifestyles.[6] In order to restore function, pulmonary rehabilitation is one of the most important aspects of treatment in patients with COPD,[7] and inspiratory muscle training (IMT) is a relatively accessible method in respiratory rehabilitation programs[8] because inspiratory muscle function is inappropriate in COPD patients.[9] Inspiratory muscle dysfunction is caused by increased residual volume, severe inflammation, and decreased range of motion of the diaphragm, which is also exacerbated by factors such as eating disorders, hypercapnia, hypoxemia, and the use of corticosteroids. This leads to the increased dyspnea, reduced exercise capacity, and impairment in patients’ quality of life.[10] Patients with COPD suffer from dyspnea and disability, regardless of the severity of the disease.[11] Dyspnea is among the most common causes that limit activities in these patients.[12] Jones et al. demonstrated that 70% with mild intensity and 74% with moderate intensity experience limitations in daily living activities such as shopping or walking with a group of peers.[13] It seems that such problems make it essential to find a simple approach to improve the situation of patients. In this regard, the American College of Chest Physicians and the American Association of Cardiovascular and Pulmonary Rehabilitation Committee (ACCP/AACVPR) have stated that further randomized controlled trials are needed to determine the role of IMT in patients with COPD.[14] In a meta-analysis by Smith et al., it was shown that there is little clinical evidence on the benefits of respiratory muscle training in patients with COPD,[15] while the meta-analysis study by Crow et al. showed that IMT, with all three types of threshold, resistive, and normocapnic devices, has beneficial effects on quality of life, exercise tolerance, and dyspnea in patients with COPD; but in the same study, it was noted that the clinical significance of the findings is unclear and further studies are needed with different protocols (in terms of intensity, frequency, and monitoring of training).[16] As rehabilitation programs are extensive due to the diversity in implementation, and most of the studies in this area have been performed in the long-term periods of 6-24 months[17,18,19] and the role of short-term periods of IMT (periods of 4 weeks to 3 months) has not been well established in previous studies,[3,20] the researchers intended to perform a study to determine the effect of short-term period of home-based IMT on dyspnea, exercise tolerance, and pulmonary function in patients with COPD.
MATERIALS AND METHODS
This study is a single-blind, randomized clinical trial that was performed on COPD patients who referred to the Specialized Pulmonary Clinic of Ahvaz in 2011. Patients eligible for the study were divided using simple random method into two groups - IMT (18 males and 2 females) and control (19 males and 1 female). Inclusion criteria were: Patients with spirometric evidence of significant chronic airflow limitation (FEV1/FVC < 70% predicted) with mild to very severe COPD diagnosis according to the GOLD criteria, an age range of 45-65 years, no history of pulmonary rehabilitation, and having an established treatment plan 1 month prior to the study. Exclusion criteria included: body mass index (BMI) >35; having comorbid conditions such as diabetes, musculoskeletal disorders, cardiovascular diseases, and neurological diseases that can affect the results of 6-min walk distance test (6MWT);[21] having exacerbation for 1 month prior to the study; a history of long-term oxygen therapy; and a history of spontaneous pneumothorax and rib fracture.[22] Sampling lasted 5 months, and 40 patients who met the inclusion criteria were selected from 72 patients.
After obtaining consent from the patients, who were randomly divided into two groups, basic data were collected from all subjects in each group, who were invited separately. The data, which included exercise capacity, exertional dyspnea, and pulmonary function test, were collected from both groups at baseline and the end of 8 weeks of IMT. IMT was given using Respivol ( Medinet, Milano, Italy), which is one of the types of incentive exerciser, as a personal device. It has been specifically designed to train the inspiratory muscles so that it can provide the conditions for evaluating the inspiratory flow and volume of a patient. The device consists of two chamber-like piston cylinders, within each of which a movable indicator is located. The indicator in the measured cylinder shows the total inspiratory volume, while the indicator in the flow cylinder shows the patient when sufficient inspiratory flow is established. The chambers are connected between themselves and to the patient by a mouthpiece. A filter is placed at the beginning of each cylinder. A hydrodynamic damping of the indicators causes natural breathing. More precisely, because the cylinders of Respivol have no air leak and loss of air occurs very less between the cylinders and indicators, the device remains stable, even when the cylinders are polluted with dust. In addition, the indicators are heavy enough to cause slower reaction time of patients and delayed shortness of breath.[9,23]
In the first session, patients were taught to use the device, and the amount of their inspiratory volume was marked on the device. Patients were advised to consider a volume more than the marked amount as a target and try to achieve a higher level of inspiratory volume in each training session. Training was performed for 8 weeks (15 min/day for 6 days/week) at home; and at the end of the first week, it was repeated under the supervision of the researcher so that the accuracy of the performed training could be proven for the researcher. Although home-based training was performed without the supervision of researchers, they were informed of the training sessions through phone calls during the 8 weeks. A checklist, which was designed to be completed on weekdays, was prepared for the patients so that they could mark the relevant day after a training session. This study did not statistically analyze the patients who did not perform more than 20% of training (five or more sessions).
Tools for data collection in the study included the following. Spirometer: Lung volumes, including FEV1 and FEV1/FVC, were calculated by using Spirolab II (Italy). 6MWT: This test was performed according to the protocol provided by the American Thoracic Society (ATS) (21). The patients were encouraged to walk as far as they could in 6 min. The test was performed under the supervision of a therapist (the researcher) along a flat straight corridor with 30 m length. The length of corridor was marked every 3 m. At the beginning and end of the test, the researcher measured the heart rate and SPO2 by the pulse oximeter (NONIN, Ganshorn, Minnesota, USA) and the blood pressure by the sphygmomanometer (Richter, Germany). Borg dyspnea test: Dyspnea was evaluated base on Borg scale, which is a visual tool ranging from 0 (not noticeable) to 10 (maximum dyspnea).[24] Dyspnea was assessed at the beginning and end of the 6MWT.
Finally, the data were statistically analyzed using SPSS17 software. Baseline measurements were compared between groups using independent t-test and Fisher's exact test. Pre- and post-training differences within IMT and control groups were analyzed using paired t-tests. Pre- and post-training differences between IMT and control groups were analyzed using independent t-test. P <0.05 was considered significant.
Ethical consideration
This study was conducted after obtaining the confirmation of the Ahvaz Jundishapur Ethics Committee and the informed consent from all subjects participating in the study (ruling number: U89295).
RESULTS
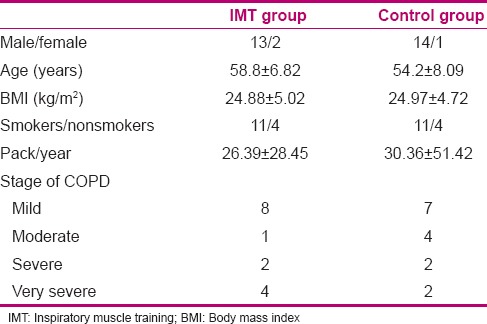
There were no statistically significant differences between the two groups in baseline measures of age, sex, BMI, pack/year, the number of smokers and non-smokers, and disease severity [Table 1]. Finally, 30 of 40 patients entering the study completed the trial (15 in the IMT group and 15 in the control group). Eight patients withdrew from the study due to the transportation problems and 2 patients were excluded from the study because of failure to complete the training period.
Table 1.
Characteristics of the enrolled patients (N=40)
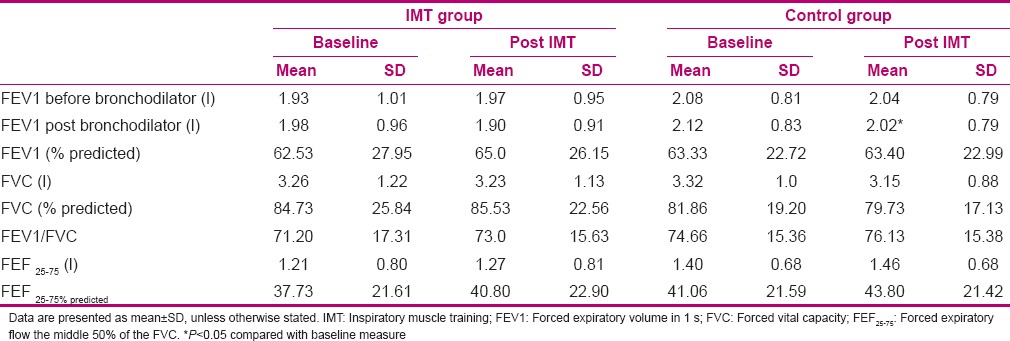
Spirometry
There was no statistically significant difference between the two groups in terms of pulmonary function tests FEV1 and FEV1/FVC [Table 2].
Table 2.
The effects of training on resting lung function
6-min walk distance test
At baseline, no statistically significant differences were observed between the two groups, while at the end of the 8-week intervention, an increase of 45 m (from 445.6 ± 89.05 to 491.06 ± 68.44 m, P = 0.0001) was observed in the training group but not in the control group (from 464.0 ± 66.39 to 464.4 ± 57.81 m, P = 0.957). At the end of the study, statistically significant difference was observed between the two groups (P = 0.001) [Table 3].
Table 3.
The effect of training on exercise capacity and dyspnea
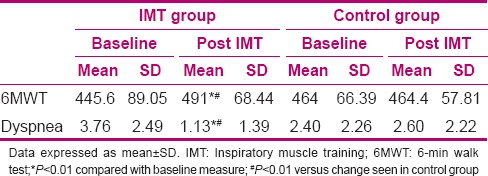
Dyspnea (Borg scale)
There was no difference in dyspnea between the two groups before training; following the training period, there was statistically significant decrease in dyspnea in the IMT group (from 3.76 ± 2.49 to 1.39 ± 1.13, P = 0.0001) but not in the control group. There was a significant difference between the two groups at the end of the study (P = 0.0001) [Table 3].
DISCUSSION
This study shows that home-based IMT using Respivol is suitable to improve symptoms of patients with mild to very severe COPD. A significant increase in exercise tolerance was observed after 8 weeks training, which is consistent with the findings of similar studies,[9,25,26] whereas in the studies by Newall[27] and Larson,[28] no additional benefits were observed in the IMT added to other rehabilitation methods because in their studies, the subjects had no or mild weakness in inspiratory muscle at the beginning of the study. In a systematic review conducted by Shoemaker et al., an increase of 54 m in the 6MWT was considered to be clinically significant.[29] In a critical review performed by Morgan on Kopper's paper, it was proposed that although there is a statistically significant increase in the 6MWT, this increase (23 m) is not clinically significant.[30,31] Increase observed in this study is equal to 45.46 m, which cannot be said to be clinically significant, as described above. However, since in the study by Beckerman,[20] an increase of 56 and 68 m was observed in the 6MWT after 3 and 9 months, respectively, it can be said that perhaps a significant increase in exercise capacity can also be seen clinically with increasing duration of training.
In this study, exertional dyspnea showed a significant decrease, which is consistent with previous studies,[32,33] while in the study of Hill et al., no improvement was seen in dyspnea after high-intensity IMT, because training with a maximum inspiratory pressure of 101% seems to cause faster fatigue of the diaphragm and respiratory muscles and to reduce the effectiveness of this method.[25]
This study and similar studies indicate that inspiratory training cannot cause changes in lung volumes,[17,20] while in the study of Ahmad et al., an increase in lung volume was observed after 4 weeks of intervention.[3] The subjects examined in his study were patients admitted to hospital. As hospitalized patients are generally under corticosteroid therapy without an established treatment plan, changes in lung volumes seem to occur as a result of the treatment, because this disease is defined as an irreversible lung problem.
Training period in this study was considered to be 8 weeks, which seems to be the least amount of time in which inspiratory muscles can be strengthened. This issue was mentioned in a guideline study presented by Hill et al.[22] In this study, the types of a flow-volumetric inspiratory exerciser called Respivol were used. Battagilla et al. reported appropriate effects by using the same device in a period of 6 months and 12 months.[9,23] The present study also indicates that the short-term period of training with the types of flow-volumetric exerciser also has positive effects on the problems caused by COPD. Most studies have already been performed by different threshold, resistive, and normocapnic types.[16] In the threshold type, when patients breathe in through the device, they must generate a preset threshold load to open the valve and allow inspiratory flow. As soon as the pressure generated drops below the threshold load, the valve closes and airflow stops. In the resistive type, the degree of resistance (inspiratory load) is related to the speed of the airflow. Thus, individuals who slowly inhale through the device experience less resistance than those who quickly inhale. As a result, to use the device, it is necessary to train the patient to learn the respiratory pattern;[28] while in Respivol, the intensity level of IMT is characterized by daily practice (i.e. the intensity is determined by the patient rather than the device) and increases with increasing levels of inspiratory volume during each training, which can be considered as a positive point.
Some limitations of this study are: (1) the lack of a double-blind design; (2) the number of female subjects (it is for cultural reasons that the prevalence of smoking is very low among women; and (3) lack of patients’ follow-up after completion of the study, and therefore, lack of information on the longevity of the effects of rehabilitation, which requires further studies in this area to evaluate the patients even in terms of the number of admissions.
CONCLUSION
In general, home-based IMT using types of flow-volumetric exerciser with low levels of supervision can also be said to have good effects on the major problems in COPD patients, including dyspnea and exercise tolerance. Therefore, this rehabilitation method can be useful for the patients with a reduced exercise tolerance who suffer from exertional dyspnea. However, since no changes are made in lung volumes after rehabilitation, the disease can cause structural changes, and besides the common treatment methods, rehabilitation methods should be used to improve the quality of life of these patients.
ACKNOWLEDGMENT
We thankfully acknowledge the Deputy of Research Affairs at the Ahvaz Jundishapur University of Medical Sciences for the financial and technical support received for this research, Project number U89295.
Footnotes
Source of Support: The manuscript was derived from a MS thesis that was approved by Ahvaz Jndishapur University of Medical sciences as the dissertation course of first author, Maryam Bakhshandeh Bavarsad
Conflict of Interest: None declared.
REFERENCES
- 1.Geddes EL, O’Brien K, Reid WD, Brooks D, Crowe J. Inspiratory muscle training in adults with chronic obstructive pulmonary disease: An update of a systematic review. Respir Med. 2008;102:1715–29. doi: 10.1016/j.rmed.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 2.Voll-Aanerud M, Eagan TM, Wentzel-Larsen T, Gulsvik A, Bakke PS. Respiratory symptoms, COPD severity, and health related quality of life in a general population sample. Respir Med. 2008;102:399–406. doi: 10.1016/j.rmed.2007.10.012. [DOI] [PubMed] [Google Scholar]
- 3.Ahmad H, Justine M, Othman Z, Mohan V, Mirza FT. The Outcomes of Short Term Inspiratory Muscle Training (IMT) Combined with Chest Physiotherapy in Hospitalized COPD Patients. Bangladesh J Med Sci. 2013;12:398–404. [Google Scholar]
- 4.Zakerimoghadam M, Tavasoli K, Nejad AK, Khoshkesht S. The effect of breathing exercises on the fatigue levels of patients with chronic obstructive pulmonary disease. Acta Med Indones. 2011;43:29–33. [PubMed] [Google Scholar]
- 5.von Leupoldt A, Taube K, Henkhus M, Dahme B, Magnussen H. The impact of affective states on the perception of dyspnea in patients with chronic obstructive pulmonary disease. Biol Psychol. 1016;84:129–34. doi: 10.1016/j.biopsycho.2009.07.010. [DOI] [PubMed] [Google Scholar]
- 6.Pryor J, Smith C. A framework for the role of Registered Nurses in the specialty practice of rehabilitation nursing in Australia. J Adv Nurs. 2002;39:249–57. doi: 10.1046/j.1365-2648.2002.02271.x. [DOI] [PubMed] [Google Scholar]
- 7.Vijayan VK. Chronic obstructive pulmonary disease. Indian J Med Res. 2013;137:251–69. [PMC free article] [PubMed] [Google Scholar]
- 8.McConnell AK. The role of inspiratory muscle function and training in the genesis of dyspnoea in asthma and COPD. Prim Care Respir J. 2005;14:186–94. doi: 10.1016/j.pcrj.2005.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Battaglia E, Fulgenzi A, Bernucci S, Giardini ME, Ferrero ME. Home respiratory muscle training in patients with chronic obstructive pulmonary disease. Respirology. 2006;11:799–804. doi: 10.1111/j.1440-1843.2006.00951.x. [DOI] [PubMed] [Google Scholar]
- 10.O’Brien K, Geddes EL, Reid WD, Brooks D, Crowe J. Inspiratory muscle training compared with other rehabilitation interventions in chronic obstructive pulmonary disease: A systematic review update. J Cardiopulm Rehabil Prev. 2008;28:128–41. doi: 10.1097/01.HCR.0000314208.40170.00. [DOI] [PubMed] [Google Scholar]
- 11.Rennard S, Decramer M, Calverley PM, Pride NB, Soriano JB, Vermeire PA, et al. Impact of COPD in North America and Europe in 2000: Subjects’ perspective of Confronting COPD International Survey. Eur Respir J. 2002;20:799–805. doi: 10.1183/09031936.02.03242002. [DOI] [PubMed] [Google Scholar]
- 12.O’Donnell DE, Travers J, Webb KA, He Z, Lam YM, Hamilton A, et al. Reliability of ventilatory parameters during cycle ergometry in multicentre trials in COPD. Eur Respir J. 2009;34:866–74. doi: 10.1183/09031936.00168708. [DOI] [PubMed] [Google Scholar]
- 13.Jones PW, Brusselle G, Dal Negro RW, Ferrer M, Kardos P, Levy ML, et al. Health-related quality of life in patients by COPD severity within primary care in Europe. Respir Med. 2010;105:57–66. doi: 10.1016/j.rmed.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 14.Ambrosino N, Palmiero G, Strambi SK. New approaches in pulmonary rehabilitation. Clin Chest Med. 2007;28:629–38. doi: 10.1016/j.ccm.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 15.Smith K, Cook D, Guyatt GH, Madhavan J, Oxman AD. Respiratory muscle training in chronic airflow limitation: A meta-analysis. Am Rev Respir Dis. 1992;145:533–9. doi: 10.1164/ajrccm/145.3.533. [DOI] [PubMed] [Google Scholar]
- 16.Crowe J, Reid WD, Geddes EL, O’Brien K, Brooks D. Inspiratory muscle training compared with other rehabilitation interventions in adults with chronic obstructive pulmonary disease: A systematic literature review and meta-analysis. Copd. 2005;2:319–29. doi: 10.1080/15412550500218072. [DOI] [PubMed] [Google Scholar]
- 17.Covey MK, Larson JL, Wirtz SE, Berry JK, Pogue NJ, Alex CG, et al. High-intensity inspiratory muscle training in patients with chronic obstructive pulmonary disease and severely reduced function. J Cardiopulm Rehabil. 2001;21:231–40. doi: 10.1097/00008483-200107000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Madariaga VB, Iturri JB, Manterola AG, Buey JC, Sebastian NT, Pena VS. Comparison of 2 methods for inspiratory muscle training in patients with chronic obstructive pulmonary disease. Arch Bronconeumol. 2007;43:431–8. doi: 10.1016/s1579-2129(07)60099-8. [DOI] [PubMed] [Google Scholar]
- 19.Beauchamp MK, Janaudis-Ferreira T, Goldstein RS, Brooks D. Optimal duration of pulmonary rehabilitation for individuals with chronic obstructive pulmonary disease-a systematic review. Chron Respir Dis. 2011;8:129–40. doi: 10.1177/1479972311404256. [DOI] [PubMed] [Google Scholar]
- 20.Beckerman M, Magadle R, Weiner M, Weiner P. The effects of 1 year of specific inspiratory muscle training in patients with COPD. Chest. 2005;128:3177–82. doi: 10.1378/chest.128.5.3177. [DOI] [PubMed] [Google Scholar]
- 21.ATS statement: Guidelines for the six-minute walk. Am J Respir Crit Care Med. 2002;166:111–7. doi: 10.1164/ajrccm.166.1.at1102. [DOI] [PubMed] [Google Scholar]
- 22.Hill K, Cecins NM, Eastwood PR, Jenkins SC. Inspiratory muscle training for patients with chronic obstructive pulmonary disease: A practical guide for clinicians. Arch Phys Med Rehabil. 2010;91:1466–70. doi: 10.1016/j.apmr.2010.06.010. [DOI] [PubMed] [Google Scholar]
- 23.Battaglia E, Fulgenzi A, Ferrero ME. Rationale of the combined use of inspiratory and expiratory devices in improving maximal inspiratory pressure and maximal expiratory pressure of patients with chronic obstructive pulmonary disease. Arch Phys Med Rehabil. 2009;90:913–8. doi: 10.1016/j.apmr.2008.12.019. [DOI] [PubMed] [Google Scholar]
- 24.Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14:377–81. [PubMed] [Google Scholar]
- 25.Hill K, Jenkins SC, Philippe DL, Cecins N, Shepherd KL, Green DJ, et al. High-intensity inspiratory muscle training in COPD. Eur Respir J. 2006;27:1119–28. doi: 10.1183/09031936.06.00105205. [DOI] [PubMed] [Google Scholar]
- 26.Shahin B, Germain M, Kazem A, Annat G. Benefits of short inspiratory muscle training on exercise capacity, dyspnea, and inspiratory fraction in COPD patients. Int J Chron Obstruct Pulmon Dis. 2008;3:423–7. doi: 10.2147/copd.s1822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Newall C, Stockley RA, Hill SL. Exercise training and inspiratory muscle training in patients with bronchiectasis. Thorax. 2005;60:943–8. doi: 10.1136/thx.2004.028928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Larson JL, Kim MJ, Sharp JT, Larson DA. Inspiratory muscle training with a pressure threshold breathing device in patients with chronic obstructive pulmonary disease. Am Rev Respir Dis. 1988;138:689–96. doi: 10.1164/ajrccm/138.3.689. [DOI] [PubMed] [Google Scholar]
- 29.Shoemaker MJ, Donker S, Lapoe A. Inspiratory muscle training in patients with chronic obstructive pulmonary disease: The state of the evidence. Cardiopulm Phys Ther J. 2009;20:5–15. [PMC free article] [PubMed] [Google Scholar]
- 30.Koppers RJ, Vos PJ, Boot CR, Folgering HT. Exercise performance improves in patients with COPD due to respiratory muscle endurance training. Chest. 2006;129:886–92. doi: 10.1378/chest.129.4.886. [DOI] [PubMed] [Google Scholar]
- 31.Can respiratory muscle endurance training alone improve exercise tolerance in COPD? Respir Med: COPD Update. 2007;2:153–4. [Google Scholar]
- 32.Chawla S, Narwa lR, Rawat J. Comparison of Inspiratory Muscle Training and Rib Raising Technique in Pulmonary Diseases Subjects. Indian J Physiother Occup Ther. 2013;7:145–50. [Google Scholar]
- 33.Magadle R, McConnell AK, Beckerman M, Weiner P. Inspiratory muscle training in pulmonary rehabilitation program in COPD patients. Respir Med. 2007;101:1500–5. doi: 10.1016/j.rmed.2007.01.010. [DOI] [PubMed] [Google Scholar]


