Abstract
Background
Energy intake is a key determinant of weight.
Objective
Our objective was to examine trends in energy intake in adults in the United States from 1971–1975 to 2009–2010.
Design
The study was a trend analysis of 9 national surveys in the United States that included data from 63,761 adults aged 20–74 y.
Results
Adjusted mean energy intake increased from 1955 kcal/d during 1971–1975 to 2269 kcal/d during 2003–2004 and then declined to 2195 kcal/d during 2009–2010 (P-linear trend < 0.001, P-nonlinear trend < 0.001). During the period from 1999–2000 to 2009–2010, no significant linear trend in energy intake was observed (P = 0.058), but a significant nonlinear trend was noted (P = 0.042), indicating a downward trend in energy intake. Significant decreases in energy intake from 1999–2000 to 2009–2010 were noted for participants aged 20–39 y, men, women, and participants with a BMI (in kg/m2) of 18.5 to <25 and ≥30.
Conclusion
After decades of increases, mean energy intake has decreased significantly since 2003–2004.
INTRODUCTION
The relative contributions of excess energy intake and reduced energy expenditure to the growth in the prevalence of obesity in the United States remain poorly defined. Energy intake is generally thought to have increased (1, 2), but the lack of accurate long-term measures and consistent surveillance systems has precluded a definitive analysis of energy expenditure, although the percentage of adults meeting 2008 physical activity guidelines is increasing (3).
Because recent data suggested that the prevalence of obesity may be starting to level off, particularly in women (4), an examination of energy intake as one of the principal drivers of the obesity epidemic may shed light on one of the potential contributing factors. Therefore, the objective of the present study was to examine the trends in energy intake among adults in the United States from the early 1970s to the present.
SUBJECTS AND METHODS
Data from 9 NHANESs were used: NHANES I (1971–1975), NHANES II (1976–1980), NHANES III (1988–1994), NHANES 1999–2000, NHANES 2001–2002, NHANES 2003–2004, NHANES 2005–2006, NHANES 2007–2008, and NHANES 2009–2010. All NHANESs share a complex multistage complex sampling design resulting in the selection of representative samples of the noninstitutionalized civilian population. Typically, respondents are interviewed in their homes and are invited to participate in additional survey activities that include various examinations, providing biological specimens, and answering additional questionnaires in the mobile examination center. Details about the plans and operations of these surveys may be found elsewhere (5). Response rates for all surveys exceed 70%. NHANES I and II received internal review at the National Center for Health Statistics. NHANES III and subsequent NHANESs received institutional review board approval.
In the mobile examination center, study participants were asked to complete a 24-h recall. Details about the procedures and changes in the procedures used to administer the 24-h recalls and the processing of the data may be found elsewhere (6–14).
A total of 13,106, 11,864, 14,645, 3905, 4402, 4038, 4217, 5003, and 5391 adults aged 20–74 y participating in the consecutive NHANESs attended the mobile examination center. Estimates of energy intake were available for 13,106, 11,797, 14,167, 3735, 4173, 3790, 4021, 4761, and 5135 adults, respectively. The exclusion of participants with missing values for some of the covariates resulted in some attrition of sample size for analyses involving these variables.
Covariates included age, sex, race or ethnicity, educational status, and BMI. Because early NHANESs limited race or ethnicity to white, African American, and other, we used these categories for all surveys. The following 3 levels of educational status were defined: did not receive a high school diploma or equivalent, received a high school diploma or equivalent, and received education beyond high school. BMI (in kg/m2) was calculated from measured height and weight and grouped as 18.5 to <25, 25 to <30, and ≥30.
Analyses were limited to 63,761 participants aged 20–74 y because 74 y was the upper age limit in the earlier surveys. We calculated unadjusted mean energy intake and mean energy intake adjusted for age, sex, race or ethnicity, educational status, and BMI by using ANCOVA. We examined trends in energy intake by using linear regression with time specified as the midpoint of the surveys. We also examined nonlinear trend for time by adding a squared term to the models. In addition to examining trends from 1971–1975 to 2009–2010, we also examined the statistical significance of the trend from 1999–2000 to 2009–2010. Data management was conducted in SAS (version 9.2; SAS Institute), and final estimates were generated by using SUDAAN (version 10.0.1; RTI International) to account for the complex sampling design. Sampling weights were used to generate percentages and means that are representative of the noninstitutionalized civilian population.
RESULTS
Mean age, the percentage of participants who were not white, the percentage who had at least graduated from high school, and mean BMI increased during the study period. The percentage of men remained relatively stable (data not shown).
Mean energy intake adjusted for age, sex, race or ethnicity, educational status, and BMI increased by 314 kcal (95% CI: 259, 368 kcal) from 1971–1975 through 2003–2004 and then decreased by 74 kcal (95% CI: 21, 126 kcal) in subsequent years (Table 1). For the unadjusted and adjusted means, the signs (both for the period 1971–1975 to 2009–2010 and for 1999–2000 to 2009–2010) for the regression coefficients of the quadratic term for time were negative (data not shown) and the P values were significant, suggesting that the upward trend in energy intake before ~2003–2004 had changed course and was decreasing in recent years.
TABLE 1.
Unadjusted and adjusted energy intake among US adults aged 20–74 y by NHANES study period1
| Energy intake
|
1971–1975 to 2009–2010 |
1999–2000 to 2009–2010 |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1971–1975 | 1976–1980 | 1988–1994 | 1999–2000 | 2001–2002 | 2003–2004 | 2005–2006 | 2007–2008 | 2009–2010 |
P-linear trend2 |
P-quadratic trend3 |
P-linear trend2 |
P-quadratic trend3 |
|
| Unadjusted means | |||||||||||||
| Total n | 12,891 | 11,515 | 14,050 | 3690 | 4037 | 3739 | 3975 | 4716 | 5093 | ||||
| Energy intake (kcal/d) | 1971.8 ± 17.54 | 1974.5 ± 17.1 | 2233.9 ± 20.1 | 2220.6 ± 30.0 | 2256.9 ± 28.1 | 2267.0 ± 20.0 | 2242.9 ± 32.1 | 2163.6 ± 29.3 | 2172.7 ± 18.8 | <0.001 | <0.001 | 0.010 | 0.041 |
| Age | |||||||||||||
| 20–39 y (n) | 5549 | 4410 | 6584 | 1472 | 1684 | 1518 | 1734 | 1741 | 1918 | ||||
| Energy intake (kcal/d) | 2185.8 ± 23.6 | 2184.1 ± 25.1 | 2451.8 ± 25.3 | 2396.3 ± 45.4 | 2450.0 ± 39.0 | 2475.1 ± 26.3 | 2429.9 ± 41.9 | 2268.2 ± 37.2 | 2292.5 ± 26.5 | <0.001 | <0.001 | 0.001 | 0.008 |
| 40–59 y (n) | 3390 | 2865 | 4265 | 1207 | 1450 | 1233 | 1361 | 1706 | 1921 | ||||
| Energy intake (kcal/d) | 1891.0 ± 25.1 | 1873.5 ± 23.6 | 2140.5 ± 24.6 | 2176.1 ± 36.0 | 2200.7 ± 31.1 | 2235.0 ± 39.9 | 2228.5 ± 34.7 | 2203.5 ± 42.9 | 2176.2 ± 31.2 | <0.001 | 0.001 | 0.906 | 0.123 |
| 60–74 y (n) | 3952 | 4240 | 3201 | 1011 | 903 | 988 | 880 | 1269 | 1254 | ||||
| Energy intake (kcal/d) | 1583.0 ± 22.8 | 1592.0 ± 11.8 | 1786.5 ± 20.0 | 1840.1 ± 24.3 | 1855.0 ± 44.1 | 1851.3 ± 32.9 | 1852.3 ± 51.7 | 1818.9 ± 46.9 | 1908.3 ± 24.7 | <0.001 | 0.049 | 0.320 | 0.387 |
| Sex | |||||||||||||
| Men (n) | 4903 | 5439 | 6572 | 1711 | 1911 | 1804 | 1876 | 2315 | 2456 | ||||
| Energy intake (kcal/d) | 2453.4 ± 28.4 | 2466.6 ± 26.7 | 2695.5 ± 28.1 | 2606.3 ± 37.6 | 2651.3 ± 41.7 | 2668.2 ± 29.4 | 2690.5 ± 40.3 | 2562.4 ± 36.4 | 2564.5 ± 31.2 | <0.001 | <0.001 | 0.109 | 0.014 |
| Women (n) | 7988 | 6076 | 7478 | 1979 | 2126 | 1935 | 2099 | 2401 | 2637 | ||||
| Energy intake (kcal/d) | 1539.9 ± 13.9 | 1526.5 ± 13.7 | 1804.8 ± 15.9 | 1859.4 ± 26.8 | 1880.0 ± 21.2 | 1884.1 ± 21.8 | 1820.7 ± 29.0 | 1799.3 ± 24.7 | 1803.1 ± 14.4 | <0.001 | <0.001 | 0.001 | 0.409 |
| Race or ethnicity | |||||||||||||
| White (n) | 10,518 | 10,042 | 5203 | 1547 | 1993 | 1891 | 1867 | 2062 | 2303 | ||||
| Energy intake (kcal/d) | 1992.3 ± 18.6 | 1994.3 ± 17.9 | 2253.1 ± 22.3 | 2266.7 ± 36.4 | 2287.9 ± 38.3 | 2282.5 ± 24.7 | 2276.5 ± 33.7 | 2200.7 ± 32.9 | 2199.3 ± 20.6 | <0.001 | <0.001 | 0.018 | 0.148 |
| African American (n) | 2220 | 1265 | 4175 | 707 | 801 | 782 | 931 | 1046 | 941 | ||||
| Energy intake (kcal/d) | 1780.1 ± 41.8 | 1821.4 ± 44.2 | 2169.6 ± 28.5 | 2151.5 ± 40.5 | 2258.5 ± 61.2 | 2169.2 ± 60.4 | 2179.0 ± 44.6 | 2127.8 ± 63.6 | 2134.0 ± 50.7 | <0.001 | <0.001 | 0.271 | 0.479 |
| Other (n) | 153 | 208 | 4672 | 1436 | 1243 | 1066 | 1177 | 1608 | 1849 | ||||
| Energy intake (kcal/d) | 2025.8 ± 158.8 | 1897.2 ± 59.5 | 2177.7 ± 36.9 | 2094.1 ± 54.3 | 2127.7 ± 36.0 | 2266.4 ± 49.5 | 2144.5 ± 48.8 | 2053.6 ± 41.9 | 2108.4 ± 32.9 | 0.950 | 0.023 | 0.447 | 0.090 |
| BMI | |||||||||||||
| 18.5 to <25 kg/m2 (n) | 6872 | 5934 | 5461 | 1160 | 1263 | 1146 | 1162 | 1340 | 1391 | ||||
| Energy intake (kcal/d) | 2015.0 ± 21.3 | 2013.4 ± 19.6 | 2257.8 ± 32.0 | 2271.5 ± 54.1 | 2285.5 ± 58.3 | 2261.7 ± 44.8 | 2247.0 ± 40.2 | 2220.2 ± 59.2 | 2111.1 ± 41.0 | <0.001 | <0.001 | 0.017 | 0.160 |
| 25 to <30 kg/m2 (n) | 3980 | 3768 | 4821 | 1268 | 1473 | 1269 | 1360 | 1588 | 1690 | ||||
| Energy intake (kcal/d) | 1994.7 ± 24.1 | 2008.0 ± 27.2 | 2291.4 ± 25.0 | 2197.1 ± 53.1 | 2296.1 ± 30.7 | 2298.4 ± 48.1 | 2281.2 ± 36.5 | 2144.8 ± 30.6 | 2280.9 ± 33.0 | <0.001 | <0.001 | 0.848 | 0.392 |
| ≥30 kg/m2 (n) | 2039 | 1813 | 3768 | 1262 | 1301 | 1324 | 1453 | 1788 | 2012 | ||||
| Energy intake (kcal/d) | 1758.4 ± 37.7 | 1754.5 ± 31.3 | 2104.3 ± 36.1 | 2187.0 ± 46.7 | 2183.5 ± 38.1 | 2241.1 ± 54.3 | 2201.9 ± 38.6 | 2130.0 ± 32.4 | 2127.1 ± 27.5 | <0.001 | <0.001 | 0.080 | 0.180 |
| Adjusted means5 (kcal/d) | |||||||||||||
| Total | 1955.1 ± 18.7 | 1946.2 ± 16.8 | 2214.7 ± 16.9 | 2220.7 ± 25.8 | 2248.2 ± 20.7 | 2268.7 ± 20.6 | 2251.2 ± 26.8 | 2183.1 ± 29.2 | 2195.1 ± 17.3 | <0.001 | <0.001 | 0.058 | 0.042 |
| Age | |||||||||||||
| 20–39 y | 2153.4 ± 22.8 | 2147.6 ± 25.0 | 2438.2 ± 23.9 | 2405.3 ± 39.6 | 2471.0 ± 32.1 | 2478.8 ± 32.7 | 2429.0 ± 39.6 | 2287.0 ± 34.6 | 2304.9 ± 30.2 | <0.001 | <0.001 | <0.001 | 0.009 |
| 40–59 y | 1893.4 ± 25.6 | 1883.6 ± 23.9 | 2141.4 ± 24.4 | 2185.3 ± 30.0 | 2174.1 ± 29.6 | 2225.5 ± 38.6 | 2224.1 ± 31.0 | 2215.7 ± 40.0 | 2186.0 ± 30.6 | <0.001 | 0.001 | 0.697 | 0.233 |
| 60–74 y | 1616.7 ± 23.2 | 1604.3 ± 12.1 | 1794.8 ± 19.0 | 1846.5 ± 25.7 | 1852.0 ± 39.9 | 1835.9 ± 31.4 | 1844.9 ± 41.0 | 1812.3 ± 41.1 | 1899.5 ± 19.8 | <0.001 | 0.035 | 0.470 | 0.187 |
| Sex | |||||||||||||
| Men | 2395.8 ± 29.0 | 2401.1 ± 27.0 | 2661.6 ± 25.1 | 2609.7 ± 40.6 | 2654.5 ± 37.7 | 2678.5 ± 32.1 | 2709.5 ± 37.1 | 2592.5 ± 38.1 | 2603.5 ± 33.4 | <0.001 | <0.001 | 0.467 | 0.026 |
| Women | 1544.5 ± 16.5 | 1521.4 ± 14.1 | 1796.9 ± 14.6 | 1857.2 ± 29.2 | 1870.8 ± 19.8 | 1884.7 ± 20.6 | 1822.6 ± 24.8 | 1803.1 ± 25.0 | 1813.9 ± 14.2 | <0.001 | <0.001 | 0.009 | 0.512 |
| Race or ethnicity | |||||||||||||
| White | 1985.4 ± 19.9 | 1975.9 ± 18.0 | 2234.6 ± 18.0 | 2257.4 ± 28.6 | 2275.7 ± 30.0 | 2284.1 ± 20.9 | 2288.6 ± 28.7 | 2224.2 ± 33.1 | 2219.5 ± 20.0 | <0.001 | <0.001 | 0.100 | 0.076 |
| African American | 1786.4 ± 32.2 | 1801.7 ± 38.2 | 2138.8 ± 24.0 | 2140.6 ± 29.2 | 2246.5 ± 49.8 | 2165.7 ± 45.7 | 2193.8 ± 35.0 | 2143.6 ± 48.0 | 2157.6 ± 46.9 | <0.001 | <0.001 | 0.602 | 0.387 |
| Other | 1994.8 ± 158.8 | 1899.6 ± 52.5 | 2183.9 ± 40.0 | 2110.5 ± 58.9 | 2123.7 ± 32.6 | 2270.5 ± 49.7 | 2134.0 ± 46.8 | 2043.9 ± 40.9 | 2109.4 ± 33.0 | 0.784 | 0.010 | 0.311 | 0.171 |
| BMI | |||||||||||||
| 18.5 to <25 kg/m2 | 1998.3 ± 23.8 | 1972.6 ± 18.8 | 2234.7 ± 28.5 | 2254.2 ± 41.4 | 2278.2 ± 45.9 | 2276.0 ± 36.4 | 2291.3 ± 27.0 | 2244.6 ± 56.4 | 2143.5 ± 27.6 | <0.001 | <0.001 | 0.049 | 0.008 |
| 25 to <30 kg/m2 | 1957.5 ± 23.4 | 1982.4 ± 28.0 | 2262.7 ± 22.6 | 2206.3 ± 40.4 | 2286.5 ± 24.0 | 2311.4 ± 41.1 | 2264.5 ± 30.3 | 2169.9 ± 26.0 | 2320.4 ± 32.4 | <0.001 | <0.001 | 0.605 | 0.782 |
| ≥30 kg/m2 | 1826.6 ± 32.9 | 1806.3 ± 28.6 | 2123.3 ± 29.8 | 2195.8 ± 44.8 | 2174.2 ± 30.3 | 2215.4 ± 51.1 | 2194.8 ± 35.6 | 2131.1 ± 29.3 | 2116.9 ± 20.5 | <0.001 | <0.001 | 0.039 | 0.261 |
Sample sizes (n) for adjusted results are the same as those for unadjusted results. P values are derived from t tests of regression coefficients from linear regression analyses.
Model includes time only as a single continuous term.
Model includes time as a continuous and quadratic term. Only the P value for the quadratic term is shown.
Mean ± SE (all such values).
Adjusted for age, sex, race or ethnicity, educational status, and BMI, where applicable.
For most subgroups, adjusted energy intake peaked during 2003–2004. Mean energy intake peaked during 2001–2002 for African Americans and during 2005–2006 for men, whites, and participants with a BMI of <25. For participants aged 60–74 y and participants with a BMI of 25 to <30, maximal energy intake occurred during 2009–2010.
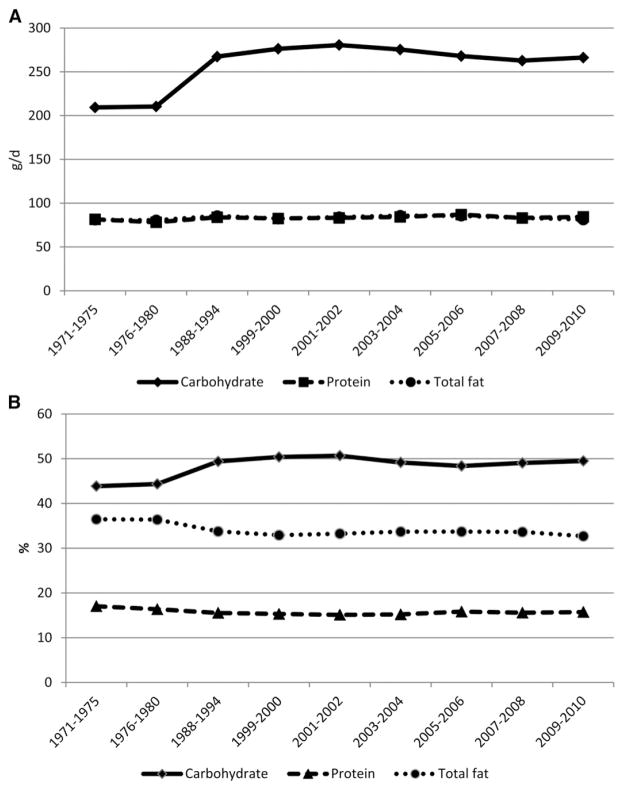
The adjusted mean intake of carbohydrates increased substantially between 1971–1975 and 2001–2002, with most of the increase occurring between 1976–1980 and 1988–1994 (Figure 1; see Supplemental Table 1 under “Supplemental data” in the online issue). From 1999–2000 to 2009–2010, adjusted mean intake decreased linearly. Although protein intake ranged between 78 and 87 g/d, regression analysis indicated a significant small increase in protein intake when viewed over the entire study period but not the period from 1999 to 2010. Adjusted mean intake of total fat varied between 80 and 86 g/d, peaked during 2003–2004, and subsequently declined.
FIGURE 1.
Mean adjusted intakes of macronutrients among adults aged 20–74 y by NHANES study period. A: Results shown as absolute intake in grams per day. B: Results shown as percentage of energy intake. Results were adjusted for age, sex, race or ethnicity, educational status, and BMI.
DISCUSSION
Our analysis of dietary data from NHANES suggests that mean energy intake peaked during 2003–2004 and has decreased during the subsequent 4 y. If energy intake is indeed trending down, this development would mark a major milestone in the history of the obesity epidemic and have implications for projections concerning the trajectory of the obesity epidemic.
Previous analyses of NHANES data had described increases in energy intake in the US population (1, 2). Our analyses provide a new perspective on recent developments concerning the trend in energy intake among US adults. Because of increased energy requirements among the obese, the increase in the prevalence of obesity since the 1970s sustained increased energy intake. The reasons for the apparent decrease in energy intake are uncertain. The attention drawn to the obesity epidemic and its attendant determinants by government and prominent organizations amplified by the many messages in the media about obesity and the need to limit energy intake may have had a salutary effect (15, 16).
Analyses of data from NHANES suggest that the prevalence of obesity may be leveling off among women, particularly white women, but continues to increase among men (4). The result of the present study showing a significant decline in energy intake in women is consistent with the trend in the prevalence of obesity among women. In contrast, energy intake among men decreased similarly in relative terms as energy intake among women despite a continuing increase in the prevalence of obesity among men.
The results of the present study should be considered in light of the changes in the methodology used to conduct the 24-h dietary recalls. The most recent change occurred during the 2001–2002 survey when the US Department of Health and Human Services and the USDA implemented a unified approach to collecting dietary data using NHANES (10). Dietary information was collected with a computer-assisted dietary interview system, a multiple pass system that involved interviewers recording foods during 1999–2001, and with the Automated Multiple Pass Method, a fully computerized system, from 2002 on. A second 24-h recall via telephone was released during the 2003–2004 cycle, but we only used the recall from the first day in the mobile examination center to maintain consistency across NHANES cycles. The impact of the changes to dietary recall methodology on the trends in energy intake is unclear. Since 2003–2004, however, the 24-h recall methods have remained largely consistent. A comparison of the ratio of energy intake to estimated basal metabolic rate in NHANES I and NHANES II showed approximately similar ratios (17). However, a similar analysis applied to data from phase I of NHANES III showed higher ratios of energy intake to estimated basal metabolic rate than in preceding surveys, suggesting that some part of the increase in energy intake seen in NHANES III was attributable to methodologic changes (18).
An important limitation of this study is the reliance on self-reported energy intakes, shown by the finding in Table 1, in which both the unadjusted and adjusted energy intakes for those with a BMI ≥30 were lower than energy intakes for overweight or healthy-weight subjects. Decreased reporting of energy intake and increased reporting of energy expenditure among the obese relative to actual levels has been well documented (19). In a more recent demonstration of underreporting of energy intake, self-reported energy intake in 524 participants aged 30–69 y was compared with total energy expenditure measured with doubly labeled water (20). Overall, self-reported energy intake was ~11% below total energy expenditure. When the data were stratified by BMI, self-reported energy intake was <3% below total energy expenditure among participants with a BMI <25, 14–15% below total energy expenditure among overweight men and women, and 20–21% below total energy expenditure among obese men and women.
During the time span covered in the present study, the sociodemographic profile of the United States changed substantially: the population aged, the percentage of whites decreased, and educational achievement increased. To the extent that these factors are related to energy intake, changes in sociodemographic factors could have influenced the trend in energy intake. By incorporating these factors in our adjusted analyses, we attempted to control for the effects of changes in sociodemographic factors.
The average yearly change in energy intake between any 2 consecutive surveys ranged from approximately −34 kcal/y from 2005–2006 to 2007–2008 to approximately +22 kcal/y from 1976–1980 to 1988–1994. The average yearly increase in energy intake from 1971–1975 to 2003–2004, when mean energy intake peaked, was almost +11 kcal/y. From 2003–2004 to 2007–2008, average yearly energy decreased by approximately −21 kcal/y. The increase of 12 kcal during the most recent 2-y period (6 kcal/y) should be considered in the context of these annual changes, and future monitoring of the trend in energy intake is critical to determine whether this most recent estimate may have been due to sampling variation or represented a renewed increase in energy intake.
An analysis of data from NHANES 2005–2006 showed that the top 10 sources of calories among adults were grain-based desserts, yeast breads, chicken and chicken mixed dishes, soda/energy/sports drinks, alcoholic beverages, pizza, tortillas, burritos, tacos, pasta and pasta dishes, beef and beef mixed dishes, and dairy desserts (21). However, little is known about the trends in the consumption of these foods.
The impact of sugar-sweetened beverage consumption on obesity has come under intense scrutiny in recent years (22). From 1988–1994 to 1999–2004, the consumption of these beverages increased (23). Since 1999–2000, however, the consumption of added sugars to beverages and foods has decreased (24). From 1970 to the late 1990s, the per capita alcohol consumption in the United States declined (25). Among persons ≥15 y of age, the per capita consumption of ethanol was 2.52 gallons in 1970, increased to 2.76 gallons during 1980 and 1981, decreased to 2.14 gallons during 1997 and 1998, and then increased again to 2.32 gallons in 2008 and 2.30 gallons in 2009. These data suggest that changes in per capita alcohol intake were unlikely to explain the trend in energy intake.
In 2009 the CDC released a set of recommendations pertaining to community strategies to prevent obesity in the United States (26). Among these strategies were a number of recommendations to promote the availability of affordable healthy food and beverages and to support healthy food and beverage choices. Implementing these strategies may be key to sustaining future decreases in energy intake. The current dietary guidelines released in 2010 recommend balancing caloric needs to achieve a healthy weight and caloric decreases for people with excess weight (21). A recent complex modeling effort showed the prolonged duration in energy deficit needed to reverse current levels of obesity (27). That model made clear that returning to obesity levels that prevailed during the 1960s and 1970s will take considerably longer than previously thought.
Future research into behaviors that guide energy intake may help to clarify the underlying dynamics of the observed trend in energy intake. Research into factors such as the frequency of eating out, changes in portion sizes, changes in dietary patterns, changes in the intake of energy-dense foods of low nutritional value, and numerous other factors may shed light on the observed trend. Furthermore, continued surveillance of energy intake in the US population is critical to monitoring this component of energy balance and its influence on the obesity epidemic.
Supplementary Material
Footnotes
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the CDC.
The authors’ responsibilities were as follows—ESF: designed the study, analyzed the data, had primary responsibility for the final content of the manuscript; and ESF and WHD: interpreted the data and drafted the manuscript. Both authors read and approved the final manuscript.
Neither of the authors declared a conflict of interest.
References
- 1.Centers for Disease Control and Prevention. Trends in intake of energy and macronutrients–United States, 1971–2000. MMWR Morb Mortal Wkly Rep. 2004;53:80–2. [PubMed] [Google Scholar]
- 2.Briefel RR, Johnson CL. Secular trends in dietary intake in the United States. Annu Rev Nutr. 2004;24:401–31. doi: 10.1146/annurev.nutr.23.011702.073349. [DOI] [PubMed] [Google Scholar]
- 3.US Department of Health and Human Services. Health, United States, 2011: with special feature on socioeconomic status and health. Washington, DC: US Government Printing Office; 2012. [Google Scholar]
- 4.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307:491–7. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. About the National Health and Nutrition Examination Survey. Available from: http://www.cdc.gov/nchs/nhanes/about_nhanes.htm (cited 18 March 2011)
- 6.US Department of Health, Education, and Welfare, Public Health Service, Office of Health Research, Statistics, and Technology, National Center for Health Statistics. . Plan and operation of the Health and Nutrition Examination Survey: United States—1971–1973. Vital Health Stat. 1973;1:10a. [PubMed] [Google Scholar]
- 7.US Department of Health and Human Services, Public Health Service, Office of Health Research, Statistics, and Technology, National Center for Health Statistics. . Plan and operation of the Second National Health and Nutrition Examination Survey 1976–80. Vital Health Stat. 1981;1:15. DHHS Publication No. (PHS) 81-I317. [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. Plan and operation of the Third National Health and Nutrition Examination Survey, 1988–94. Vital Health Stat. 1994;1:32. DHHS Publication No. (PHS) 94-1308. [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. NHANES 1999–2000 dietary files. Available from: http://www.cdc.gov/nchs/nhanes/nhanes1999-2000/diet99_00.htm (cited 15 February 2012)
- 10.Centers for Disease Control and Prevention. NHANES 2001–2002 dietary files. Available from: http://www.cdc.gov/nchs/nhanes/nhanes2001-2002/diet01_02.htm (cited 12 December 2012)
- 11.Centers for Disease Control and Prevention. NHANES 2003–2004 dietary files. Available from: http://www.cdc.gov/nchs/nhanes/nhanes2003-2004/diet03_04.htm (cited 12 December 2012)
- 12.Centers for Disease Control and Prevention. NHANES 2005–2006 dietary files. Available from: http://www.cdc.gov/nchs/nhanes/nhanes2005-2006/diet05_06.htm (cited 12 December 2012)
- 13.Centers for Disease Control and Prevention. NHANES 2007–2008 dietary files. Available from: http://www.cdc.gov/nchs/nhanes/nhanes2007-2008/diet07_08.htm (cited 12 December 2012)
- 14.Centers for Disease Control and Prevention. NHANES 2009–2010 dietary files. Available from: http://www.cdc.gov/nchs/nhanes/nhanes2009-2010/diet09_10.htm (cited 12 December 2012)
- 15.US Department of Health and Human Services; Public Health Service; Office of the Surgeon General. The Surgeon General’s call to action to prevent and decrease overweight and obesity. Available from: http://www.surgeongeneral.gov/library/calls/obesity/CalltoAction.pdf.pdf (cited 12 December 2012)
- 16.Koplan JP, Liverman CT, Kraak VI, editors. Committee on Prevention of Obesity in Children and Youth, Food and Nutrition Board, Board on Health Promotion and Disease Prevention. Preventing childhood obesity: health in the balance. Washington, DC: The National Academies Press; 2005. [PubMed] [Google Scholar]
- 17.Black AE, Goldberg GR, Jebb SA, Livingstone MB, Cole TJ, Prentice AM. Critical evaluation of energy intake data using fundamental principles of energy physiology: 2. Evaluating the results of published surveys. Eur J Clin Nutr. 1991;45:583–99. [PubMed] [Google Scholar]
- 18.Briefel RR, Sempos CT, McDowell MA, Chien S, Alaimo K. Dietary methods research in the third National Health and Nutrition Examination Survey: underreporting of energy intake. Am J Clin Nutr. 1997;65:1203S–9S. doi: 10.1093/ajcn/65.4.1203S. [DOI] [PubMed] [Google Scholar]
- 19.Lichtman SW, Pisarska K, Berman ER, Pestone M, Dowling H, Offenbacher E, Weisel H, Heshka S, Matthews DE, Heymsfield SB. Discrepancy between self-reported and actual caloric intake and exercise in obese subjects. N Engl J Med. 1992;327:1893–8. doi: 10.1056/NEJM199212313272701. [DOI] [PubMed] [Google Scholar]
- 20.Moshfegh AJ, Rhodes DG, Baer DJ, Murayi T, Clemens JC, Rumpler WV, Paul DR, Sebastian RS, Kuczynski KJ, Ingwersen LA, et al. The US Department of Agriculture Automated Multiple-Pass Method reduces bias in the collection of energy intakes. Am J Clin Nutr. 2008;88:324–32. doi: 10.1093/ajcn/88.2.324. [DOI] [PubMed] [Google Scholar]
- 21.US Department of Agriculture; US Department of Health and Human Services. Dietary guidelines for Americans, 2010. 7. Washington, DC: US Government Printing Office; 2010. [Google Scholar]
- 22.Malik VS, Popkin BM, Bray GA, Despres JP, Hu FB. Sugar-sweetened beverages, obesity, type 2 diabetes mellitus, and cardiovascular disease risk. Circulation. 2010;121:1356–64. doi: 10.1161/CIRCULATIONAHA.109.876185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bleich SN, Wang YC, Wang Y, Gortmaker SL. Increasing consumption of sugar-sweetened beverages among US adults: 1988–1994 to 1999–2004. Am J Clin Nutr. 2009;89:372–81. doi: 10.3945/ajcn.2008.26883. [DOI] [PubMed] [Google Scholar]
- 24.Welsh JA, Sharma AJ, Grellinger L, Vos MB. Consumption of added sugars is decreasing in the United States. Am J Clin Nutr. 2011;94:726–34. doi: 10.3945/ajcn.111.018366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.LaVallee RA, Yi H. Apparent per capita alcohol consumption: national, state, and regional trends, 1977–2009. Available from: http://pubs.niaaa.nih.gov/publications/Surveillance92/CONS09.pdf (cited 15 February 2012)
- 26.Khan LK, Sobush K, Keener D, Goodman K, Lowry A, Kakietek J, Zaro S. Recommended community strategies and measurements to prevent obesity in the United States. MMWR Recomm Rep. 2009;58:1–26. [PubMed] [Google Scholar]
- 27.Hall KD, Sacks G, Chandramohan D, Chow CC, Wang YC, Gortmaker SL, Swinburn BA. Quantification of the effect of energy imbalance on bodyweight. Lancet. 2011;378:826–37. doi: 10.1016/S0140-6736(11)60812-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.